To the Editor,
The pandemic of the COVID-19 started in China in December 2019 with a rapid spread to the whole world. The COVID 19 is associated with different degrees of severe respiratory illness and might lead to a severe acute respiratory syndrome, which ends in many cases with death. The spread of the infection between humans occurs via droplets, contaminated hands or surfaces, with an incubation time of two to fourteen days.
Most countries went through the lockdown to try to flatten the contagion curve quickly. In these countries, hospitals suspended normal activities to reallocate healthcare professionals to cope with the pandemic. Furthermore, the paralysis period of the planned health activity is generating a waiting list of visits and procedures that must be incorporated into the health process. Although we are experiencing a health emergency never seen before, we must not forget that it is our ethical and moral obligation to continue taking care of our patients, not only patients infected with SARS-CoV-2, because every patient has the right to be cared for their demands and needs.
Patients with chronic pain, such as those with musculoskeletal, neuromuscular or oncological conditions, have been mostly deprived of the necessary resources to alleviate their symptoms and make their lives somewhat more bearable. In most countries during lockdown, patients have been allowed to use only telemedicine services, with the aim of reducing the risk of contagion. Unfortunately, in the management of these conditions, many of the treatments are interventional and therefore not accessible. Not performing or postponing a procedure may lead to morbidity and other chronic sequelae, including irreparable functional impairment.
Muscle spasticity, chronic musculoskeletal pain as rotator cuff pathologies or chronic tendinopathies and fasciitis, hip and knee osteoarthritis, entrapment neuropathies, polyneuropathy (diabetic etc.) or nerve injuries are disabling and have a great impact on daily activities performance and quality of life.
Adding to the chronic pain and physical disability these patients experience the fear, anxiety and loneliness due to the restrictive measures adopted to limit outbreaks, seriously undermining the mental health.
For this reason, it is essential to progressively reactivate health services and ensure our complete medical support to the population, which obviously include interventional and ultrasound-guided treatments, such as intra-articular and tendon injections, regenerative medicine, botulinum toxin for pain and especially for spasticity treatment, etc.
Although there are no references or experiences on how to resume healthcare in a pandemic, and whether the previously established processes are equally valid and safe for patients and healthcare professionals, we can still integrate those protocols with higher safety standards. It would be good to remember that the criteria and protocols for assigning and defining priorities for access to hospital care (elective, urgent, etc) must be applied individually and respecting professional ethics.
In the countries that are, albeit partially, exiting lockdown, we suggest the following recommendations to maintain a high safety standard. Patients infected with SARS-CoV-2 will follow a dedicated path, being preferably treated at COVID-19 blocks/dedicated COVID-19 hospitals or clinics. Consider establishing triage stations outside or at least at the facility entrance to screen individuals. The non-COVID service must be reorganized, reducing the number of patients that can be normally attended, minimizing gatherings of people and waiting time in wards, consultations or procedural rooms and to allow time for sanitation between patients.
Patients should be contacted in advance to investigate their clinical conditions and prioritize, to evaluate any possible exposure to coronavirus, in case to prescribe diagnostic test (serological or rtPCR), and to inform that they must wear at least a facemask upon arrival, at the scheduled time, to the facility. Of note, N95/FFP2/KN95 masks with an exhaust valve might not provide infection control, so health care personnel must change to or cover with a surgical mask.
Although these are not aerosol-generating procedures, many of them take time, so we recommend the health personnel present in the procedural rooms to always wear non-valve N95 masks. Health care personnel should always wear personal protective equipment. A practical guide on how to safely conduct interventional procedures is shown in Figure 1.
Figure 1.
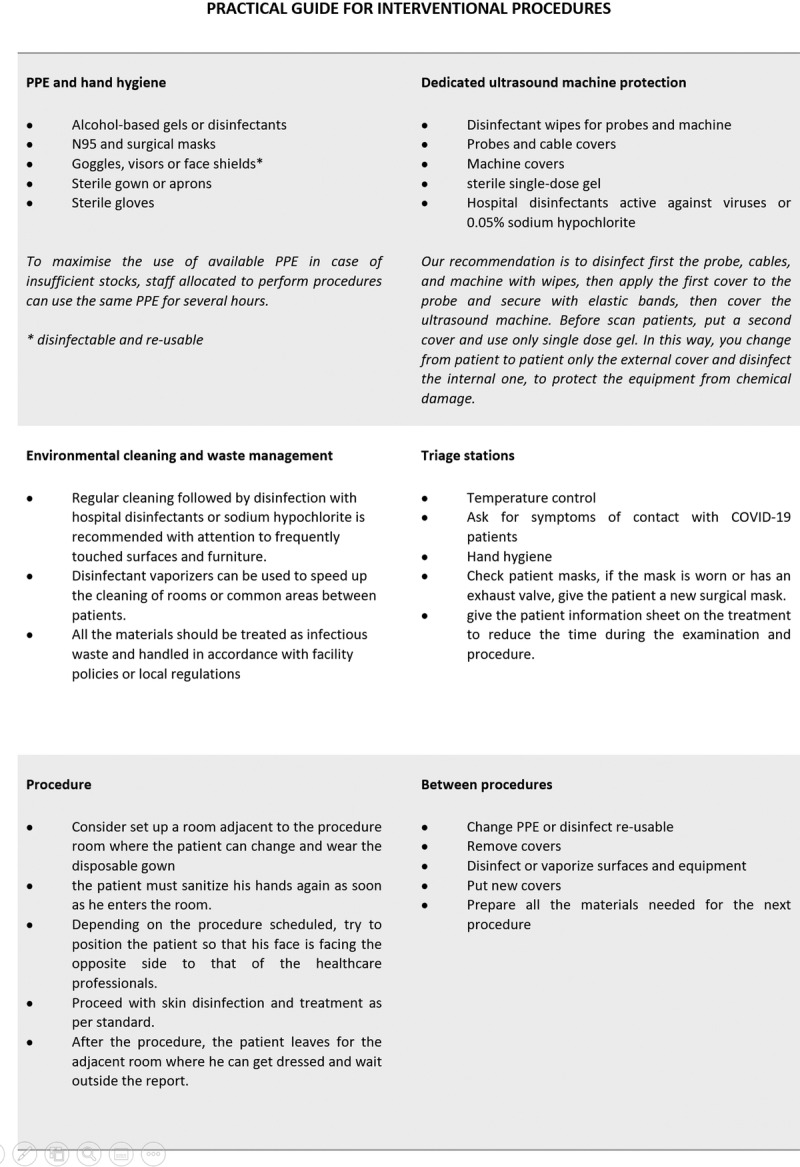
Practical guide on how to safely conduct interventional procedures.
Although there are no specific studies on the possible interference of drugs or treatments for the management of chronic pain in COVID-19 patients, it is important to elucidate some doubts, especially regarding the use of anti-inflammatory and corticosteroids, which are currently under discussion. Despite some controversy, there is no evidence that the use of nonsteroidal anti-inflammatory drugs can increase the severity of COVID-19, therefore they can be used when needed1.
Although the use of corticosteroids predisposes to a higher risk of infection, the immunosuppressive effect is dose and time dependent. Low doses of corticosteroids rarely increase the risk of infections and are not contraindicated for the treatment of rheumatic diseases, even during this pandemic2,3. Likewise, there is no absolute contraindication to the use of corticosteroids for the Herpes Zoster associated pain. Therefore, low doses oral corticosteroids as adjunctive therapy, or for local injection of depot formulations, can be used evaluating the risk and benefits. Every clinician should be alert on appearance of future new recommendations.
In conclusion, safe practice to protect patients and health care personnel is crucial to prevent the spread of COVID19 and to maintain chronic pain services to provide effective treatment for patients during this pandemic.
Footnotes
Disclosure: For all authors nothing to declare.
References
- 1.EMA gives advice on the use of non-steroidal anti-inflammatories for COVID-19 | European Medicines Agency. https://www.ema.europa.eu/en/news/ema-gives-advice-use-non-steroidal-anti-inflammatories-covid-19. Accessed May 4, 2020.
- 2.Liu D, Ahmet A, Ward L, et al. :. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy, Asthma Clin Immunol. 2013;9:30. doi: 10.1186/1710-1492-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mikuls TR, Johnson SR, Fraenkel L, et al. :. American College of Rheumatology Guidance for the Management of Adult Patients with Rheumatic Disease During the COVID-19 Pandemic. Arthritis Rheumatol. April2020:art.41301. doi: 10.1002/art.41301 [DOI] [PubMed] [Google Scholar]


