Abstract
Background:
A novel coronavirus (COVID-19) erupted in the latter part of 2019. The virus, SARS-CoV-2 can cause a range of symptoms ranging from mild through fulminant respiratory failure. Approximately 25% of hospitalized patients require admission to the intensive care unit, with the majority of those requiring mechanical ventilation. High density consolidations in the bronchial tree and in the pulmonary parenchyma have been described in the advanced phase of the disease. We noted a subset of patients who had a sudden, significant increase in peak airway, plateau and peak inspiratory pressures. Partial or complete ETT occlusion was noted to be the culprit in the majority of these patients.
Methods:
With institutional IRB approval, we examined a subset of our mechanically ventilated COVID-19 patients. All of the patients were admitted to one of our COVID-19 ICUs. Each was staffed by a board certified intensivist. During multidisciplinary rounds, all arterial blood gas (ABG) results, ventilator settings and ventilator measurements are discussed and addressed. ARDSNet Protocols are employed. In patients with confirmed acute occlusion of the endotracheal tube (ETT), acute elevation in peak airway and peak inspiratory pressures are noted in conjunction with desaturation. Data was collected retrospectively and demographics, ventilatory settings and ABG results were recorded.
Results:
Our team has observed impeded ventilation in intubated patients who are several days into the critical course. Pathologic evaluation of the removed endotracheal tube contents from one of our patients demonstrated a specimen consistent with sloughed tracheobronchial tissues and inflammatory cells in a background of dense mucin. Of 110 patients admitted to our adult COVID-19 ICUs, 28 patients required urgent exchange of their ETT.
Conclusion:
Caregivers need to be aware of this pathological finding, recognize, and to treat this aspect of the COVID-19 critical illness course, which is becoming more prevalent.
Keywords: coronavirus, COVID, COVID 19, critical care, endotracheal tube, inflammation, occlusion, tracheobronchial tree
A novel coronavirus (COVID-19) erupted in Wuhan, Hubei Province, China in November 2019. The subsequent pandemic has now affected millions of people as of March 2020. The virus, Severe acute respiratory syndrome coronavirus 2 can cause a range of symptoms from the mild (fevers, cough, and sore throat) through severe, culminating in acute respiratory distress syndrome (ARDS) and death.1 The number of affected individuals has been increasing daily in the United States, with more than 150,000 patients diagnosed in New York State as of April 8, 2020. Most patients develop only mild symptoms requiring supportive management without hospitalization. The vast majority of patients are able to convalesce without hospitalization; however, 20% of those infected have been hospitalized. Further, 25% of hospitalized patients require admission to the intensive care unit (ICU) and not infrequently prolonged mechanical ventilation.2 Patients that require mechanical ventilation usually present either with severe hypoxic respiratory failure initially or fail supplemental oxygen support during hospitalization. Mechanical ventilation typically portends a poor outcome, with a quoted mortality of 48% in 1 series.3
At our institution, more than 400 patients have been hospitalized thus far for the treatment of COVID-19. Of these more than 25% have required admission to the ICU; the vast majority of those required mechanical ventilation. Although this patient population has met the Berlin Criteria of ARDS,4 their presentation has not been classic. As noted by multiple sources, there can be dissociation between lung compliance and oxygenation in this patient population.5,6 Some patients are noted to have a low compliance picture consistent with classic ARDS, whereas others have high compliance with severely impaired oxygenation and pulmonary findings not typical for ARDS. During their hospitalization, all of the COVID-19 mechanically ventilated patients, whether with classic ARDS or preserved compliance, can have substantial variations in their required ventilatory support. Lei et al7 and others8,9 have described a computed tomography finding of higher density consolidations in the bronchial tree and in the pulmonary parenchyma in the advanced stage of the disease. These consolidations and ground-glass opacities decrease and are absorbed in dissipating stage of the disease.
Our first patient in this series, after mechanical ventilation for about 5 days, was noted to have an acute decline in his oxygenation and ventilation. It was felt initially that this was secondary to a pulmonary embolus due to the hypercoagulable nature of COVID-19. However, assessment of his ventilatory parameters raised concern for an acute airway obstruction. Exchange of the endotracheal tube (ETT) revealed that the tube was occluded by a thick plug. Thereafter, with IRB approval, we examined a subset of patients that appeared to have a similar clinical picture in that they appeared to be steadily improving in their required pulmonary support, with a sudden, significant increase in peak airway, plateau, and peak inspiratory pressures (PIPs) with inability to adequately oxygenate and ventilate. Partial or complete ETT occlusion was noted to be the culprit in the vast majority of these patients.
METHODS
All COVID-19 mechanically ventilated patients are admitted to one of our hospital's COVID-19 ICUs. Staffing of the COVID-19 ICUs is by a team of board-certified medical or surgical intensivists. Per current staffing and protocol, an intensivist completes rounds daily on each of these critically ill patients. As part of our multi-disciplinary rounds, all arterial blood gas (ABG) results, and ventilator settings and ventilator measurements (including plateau airway pressure depending on ventilator model, PIP, and exhaled tidal volume) are discussed and addressed. The pulmonary findings seen in this patient population are not classic. Indeed, these patients seem to have a component of ARDS and in many ways also mimic inhalational injury. To help prevent additional lung injury, ARDSNet Protocols4 are followed. All patients have central venous catheters and arterial lines placed for hemodynamic monitoring. Patients with impeded ventilatory status are also monitored with continuous end-tidal carbon dioxide (EtCO2) measurements, when available. Any episode of desaturation or abrupt change in EtCO2 is expeditiously assessed by the team. Initially, the mechanical aspects of the ventilatory circuit are assessed to ensure appropriate set-up. Additionally, suction catheters are passed to assess for plugging and manual ventilation is undertaken to assess resistance. In this subset of patients with confirmed acute occlusion of their ETT, acute elevation in peak airway and PIP are generally noted in conjunction with desaturation. When ABGs or PIPs were available pre- or post-ETT exchange they were noted to be congruent with this phenomenon, indicating both decreased oxygenation and impeded ventilation. Improvement in PIPs was noted in those patients with a confirmed occluded ETT, by anesthesia, at the time of exchange. Elevated PIPs, with abrupt change were felt to be more predictive of an acute ETT occlusion.
RESULTS
In a subset of our COVID-19 mechanically ventilated patients, acute obstruction of the ETT has led to an inability to oxygenate and ventilate. Remarkably, although this patient population meets Berlin Criteria for ARDS, compliance is maintained in many of our patients. In traditional ARDS, both oxygenation and ventilation are impeded with significantly elevated airway pressure with any large tidal volume. Per Berlin Criteria, the severity of ARDS is assessed by a relatively acute onset coupled with specific PaO2/FiO2 ratios. Any PaO2/FiO2 ratio less than 150 is considered severe ARDS.
On review of approximately 110 patients in our adult COVID-19 ICUs, 28 patients required an urgent change of their ETT due to a suspected acute occlusion of the ETT (Fig. 1). All of the cohort patients were on our normal complement of critical care ventilators which were Draeger Evita Series ventilators. Heated circuits were utilized on all ventilators. Pre-ETT and post-ETT change PIP values were captured in 19 of these patients. Fifteen of these 19 patients demonstrated improvement in PIP with ETT exchange. The median change in PIP after ETT change was 12 (interquartile range 2–17.5). Pre- and post-ETT exchange ABG values were available in 11 of these patients. Per chart review and documentation of the bedside clinician, ETT exchange resulted in improvement in oxygenation, ventilation or both with ETT exchange in the majority of patients. This acute obstruction of the ETT, leading to an inability to oxygenate and ventilate, was observed at a median of 7 (interquartile range 6–11.25) days of intubation. At the time of removal, the ETT was noted to be partially to nearly completely occluded. A pathologic examination of the removed ETT contents from one of the patients demonstrated a specimen consistent with sloughed tracheobronchial tissue and inflammatory cells in a background of dense mucin (Fig. 2).
FIGURE 1.

The photograph shows an occluded endotracheal tube that as removed after a tube exchange.
FIGURE 2.
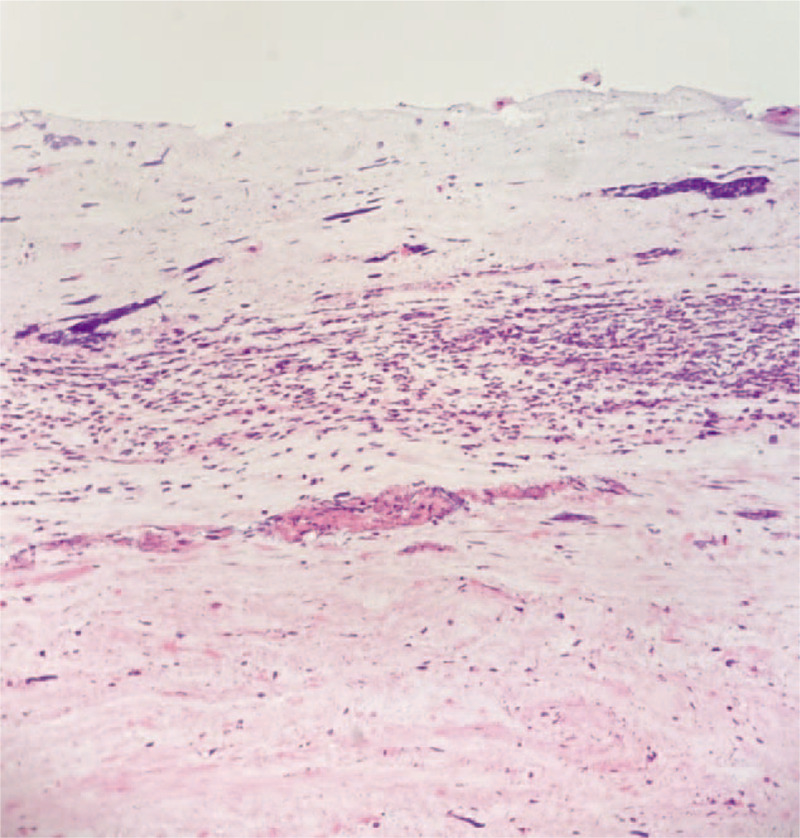
Demonstrated is a microscopic image (20× magnification) of a patient's ETT contents with a trilaminar appearance with a superficial layer of mucin, an underlying layer of degenerated inflammatory cells, and a deep collagenous layer with spindle cells suggestive for stroma. ETT indicates endotracheal tube.
DISCUSSION
Mechanically ventilated COVID-19 patients, at this time, are the primary inhabitants of the adult ICUs in our hospital. Although the patients initially present with an inability to oxygenate and a virally mediated ARDS, intrinsic lung disease is not the only reason for impaired oxygenation and ventilation. We noted at a median of 1 week after intubation, although oxygenation may have initially improved, approximately 25% (28/110) of patients had an acute deterioration with an inability to oxygenate and ventilate, which manifests as an abrupt increase in EtCO2 and PIP, suggesting an acute occlusion of the ETT.
Based upon the gross appearance, with some characteristics of bronchial casts in 1 specimen, as well assumptions made from the presence of severe viral pneumonia, we postulate that this is an inflammatory/proteinaceous exudate that results in part from diffuse alveolar damage and bronchial epithelial sloughing. We also anticipate there is likely a component of ischemia to the pulmonary endothelial cells from microthrombi yielding a sloughing of the endothelial cells. Given the tenacity of this exudate, it yields an acute occlusion of the ETT mandating an ETT exchange.
To mitigate this, a number of techniques can be utilized including close observation of ventilator measurements. Any acute change in PIP, decrease in minute ventilation and change in EtCO2 should alert the clinician to the possibility of an ETT occlusion. Routine assessment of the ETT should be performed, even with the use of common in-line suction. Any sign of obstruction, even partial, should prompt consideration for an ETT tube exchange. We have started to employ single-use ETT cleaners – devices similar to Fogarty embolectomy catheters – that allow extraction of inspissated secretions and the like from an ETT. These can be attached to the ETT via Y-connectors, allowing them to remain part of a closed circuit and hence protecting healthcare workers from aerosolization of the virus during tube cleaning. There is a theoretical risk of an ETT occlusion from the plugs and, hence, staff should be ready to re-intubate immediately. Bronchoscopy could also be considered to diagnose the problem but has limited ability to treat without advanced techniques and results in aerosolization. Traditional bronchoscopy would enable one to irrigate and suction out mucus secretions and/or hemorrhage. However, the tenacity of the occlusive material may be unable to be suctioned via a traditional bronchoscope and require further instrumentation for removal.
Routine ETT exchanges are being evaluated, as obstruction seems to occur typically around day 7 of intubation. Change of the occluded ETT has resulted in near immediate resolution of ventilation and oxygenation difficulties in a subset of patients, which has culminated in several successful extubations. Another contributing factor may be the use of heat and moisture exchangers (HME), as opposed to heated circuits in many of these patients. Although the role of HMEs in ETT obstruction is debated,10 it may be that HMEs in this particular circumstance are not sufficient.
CONCLUSIONS
A subset of mechanically ventilated COVID-19 patients had sudden pulmonary decompensation due to acute occlusion of the ETT. Clinicians need to be aware of the possibility of this devastating complication and aggressively treat this aspect of the COVID-19 illness.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bialek S, Boundy E, Bowen V, et al. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:343–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the seattle region––case series. N Engl J Med 2020; 10.1056/NEJMoa2004500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA - J Am Med Assoc 2012; 307:2526–2533. [DOI] [PubMed] [Google Scholar]
- 5.Gattinoni L, Marini JJ, Pesenti A, et al. The “baby lung” became an adult. Intensive Care Med 2016; 42:663–673. [DOI] [PubMed] [Google Scholar]
- 6.Cressoni M, Caironi P, Polli F, et al. Anatomical and functional intrapulmonary shunt in acute respiratory distress syndrome. Crit Care Med 2008; 36:669–675. [DOI] [PubMed] [Google Scholar]
- 7.Lei DP, Fan B, Mao J, Wei J, Wang P. The progression of computed tomographic (CT) images in patients with coronavirus disease (COVID-19) pneumonia. J Infect 2020; 10.1016/j.jinf.2020.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020; 10.1148/radiol.2020200370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20:425–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillies D, Todd DA, Foster JP, et al. Heat and moisture exchangers versus heated humidifiers for mechanically ventilated adults and children. Cochrane Database Syst Rev 2017; 9:CD004711. [DOI] [PMC free article] [PubMed] [Google Scholar]


