Severe acute respiratory syndrome coronavirus 2, the virus responsible for COVID-19, has placed unprecedented strain on the healthcare system in the United States and worldwide. The resultant surge of patients with COVID-19 has presented hospitals with unique challenges with respect to infrastructure, supply chain disruptions, capacity, staffing, and triage. Intensive care unit (ICU) teams have increased their surge capacity, often in unfamiliar and geographically distant locations, to ensure care for the critically ill COVID-19 patients requiring prolonged mechanical ventilation and hemodynamic support. Here, we share the design, creation, and preliminary outcomes of a streamlined multidisciplinary procedure team at our institution: the COVID-19 Bundled Response for Access (COBRA) team. The COBRA team has played a vital role in the management of the critical care surge at the Massachusetts General Hospital, and we believe that sharing our experience in a timely manner will assist other institutions worldwide in managing their COVID-19 critical care surge.
NEEDS ASSESSMENT
With the number of mechanically ventilated ICU patients rising exponentially in the first few weeks of the pandemic, several medical and surgical floors were converted into surge ICUs. The pool of residents, advanced practice providers, and intensivists taking care of these patients was quickly spread thin. Recognizing the need for innovative ways to meet the surge demands, a multidisciplinary team set out to design a new system to meet the demands of critically-ill patients in the context of ongoing personnel and resource constraints.
PURPOSE AND GOALS
COBRA was formed in early April 2020 to provide a multidisciplinary, safe, and streamlined approach to provide bundled vascular and enteral access in critically ill COVID-19 patients. The goals of the initiative were to: (1) improve the efficiency and safety of these procedures using a well-trained team of experts, (2) off-load busy ICU providers, (3) decrease healthcare worker exposure to the virus, and (4) preserve limited supplies of personal protective equipment (PPE).
MULTIDISCIPLINARY APPROACH
Due to the time-sensitive nature of the crisis, multiple emails, phone calls, and ZOOM meetings were conducted within 72 hours to establish the team. The multidisciplinary effort spanned the Departments of Surgery, Anesthesia, Interventional Radiology, Medicine, and Nursing. Approval was obtained from the Hospital Incident Command System. Feedback was obtained from hospital ICU leadership, including the established ICUs and the newly formed surge ICUs.
ACCESS AND COVERAGE
A dedicated COBRA pager was created with an easy search and find feature in the hospital telephone directory to facilitate consultation from the primary ICU team. The initial intent was to provide coverage from 6 am to 6 pm only; however, demand was so high in the first 24 hours that the decision was made to provide coverage 24 hours a day, 7 days a week.
BUNDLED PROCEDURES
The bundled procedures performed by the COBRA team included arterial lines, central venous catheters (CVC), nontunneled hemodialysis (HD) catheters, and orogastric/nasogastric tubes.
STRUCTURE
The COBRA team consisted of 4 surgical residents (post-graduate years 3–7), working 2 per team, with an in-house dedicated attending (surgeon, anesthesiologist or interventional radiologist) during the daytime. Overnight, the service was staffed by 2 surgical residents working alongside the in-house on-call trauma surgeon. Participation in COBRA at all levels was strictly voluntary. Notably, 65% of eligible surgical residents and 37% of surgical attendings at our institution volunteered to participate. The choice of attending coverage was made with special attention to specialty, expertise, and comfort with performance of vascular procedures.
SAFETY
A number of features of the service were explicitly designed to facilitate safe and efficient care by the team and to ensure participant safety. An in-depth checklist was established to facilitate communication between the ICU teams and the COBRA team. Procedure “go bags” were assembled with all essential contents for catheter placement and a dedicated hospital space was created to house necessary materials, including ultrasound machines. A bundled procedure checklist was created to guide team members through the necessary pre-procedural, procedural, and post-procedural steps. Discussions with the hospital infection control experts were held and the decision was made to provide the COBRA team members with full PPE (strict contact and airborne precautions with N95 respirator) to ensure their safety at all times. All participants completed a mandatory online and in-person PPE training, including N95 fit testing, that was supplemented with additional training on the specifics of donning and doffing PPE in a sterile environment.
VOLUME
Over a 2-week period, the COBRA team responded to a total of 158 consults on 102 patients for a total of 214 procedures. The maximum number of procedures performed during a single 24-hour period was 25 procedures on 20 patients. The majority of the procedures were arterial lines (55%), followed by CVC (25%), and HD catheters (13%). More procedures were conducted during the daytime (59%) than overnight (41%). Procedures were performed across all hospital ICUs, with more than half (54%) being performed on patients admitted to the new surge ICUs.
OUTCOMES
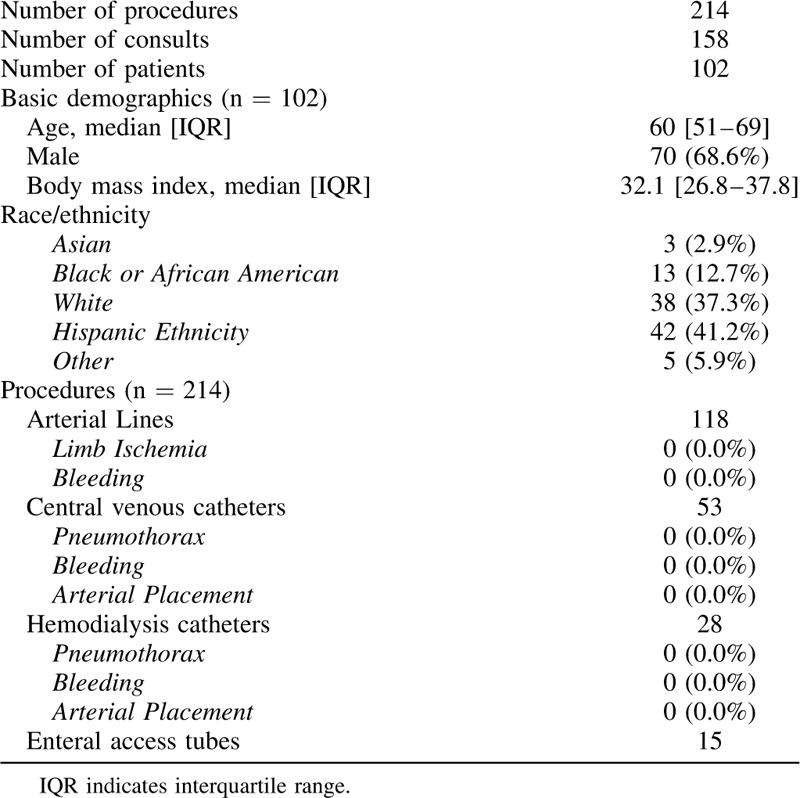
Table 1 describes the patient demographics and characteristics, and the nature and complications of the procedures performed. In total, 118 arterial lines, 53 CVC, 28 HD catheters, and 15 enteral access tubes were placed. During the 2-week interim study period there were no complications related to these procedures.
TABLE 1.
COBRA Demographics, Consults, and Procedures During the First 14 Days
CHALLENGES AND LESSONS LEARNED
The COBRA team was enthusiastically received across the hospital and effectively met procedural demands. Notably, several unique challenges arose with regards to vascular access in the COVID-19 patient population. The average body mass index of 32.1 kg/m2 presented challenges not only with patient positioning but also with procedural technique. Positioning is often a challenge given tenuous respiratory mechanics, and thus an open channel of communication between the proceduralist, ICU nurse, and respiratory therapist was key. Additional challenges were related to prone positioning, as many of these patients continued to have access needs, such as rewiring of existing catheters and placement of new lines. The COBRA team successfully placed arterial radial lines in prone patients and coordinated placement of CVC, HD catheters, and femoral arterial lines around the time of supination planned by the ICU team. Ultrasound guidance was essential for both arterial and venous catheter placement. The most frequent challenge encountered was arterial catheter-associated thrombosis requiring re-wiring or replacement of these catheters. Although the coagulopathy associated with COVID-19 syndrome remains under investigation, the COBRA team attempted to minimize risk factors for future thrombosis with the use of 3 specific strategies: (1) minimizing vascular access attempts before COBRA consultation, (2) ultrasound guidance for arterial line placement, and (3) use of longer arterial catheters to minimize accidental dislodgement. Ongoing investigations for prophylaxis of line-associated thrombosis include pilots initiatives of the use of intracatheter heparinized saline solution and systemic anticoagulation. Finally, by coordinating and bundling consults with the experienced providers on the COBRA team, we were able to optimize the use of PPE and minimize waste of procedural supplies in a time supply chain disruptions and equipment shortages.
SUMMARY
Here we describe our experience in a large academic quaternary care center in establishing a streamlined, high reliability, and multidisciplinary procedural team during the COVID-19 pandemic. This team has proved to be integral to our hospital's response to the overwhelming number of critically ill COVID-19 patients. We hope that the timely sharing of this experience will help prepare other hospitals to meet present and future COVID-19 or other disaster needs.
Footnotes
Katherine Albutt and Casey M. Luckhurst are co-first authors.
The authors declare no conflict of interest.


