Amidst the SARS-CoV-2 or “COVID-19” pandemic, the need for trauma care remains a critical public health responsibility. Anticipating augmentation of social determinants of violence, “end stage” presentations of surgical pathologies from delayed care, and demands on surgeons and surgical intensivists, readiness, adaptability, and leadership in trauma centers are paramount. This Surgical Perspectives centers around an urban, Level-1 trauma center's experience in meeting the challenge to maintain trauma care access and capability during the COVID-19 pandemic.
INSTITUTIONAL CONTEXT
Denver Health Medical Center (DHMC) is a 555-bed hospital and an American College of Surgeons - and Colorado state-verified Level-1 trauma center. The Ernest E. Moore Shock Trauma Center at Denver Health is one of the world's leading trauma centers, providing care to 18,000 trauma patients annually. DHMC is dedicated to maintaining a state of readiness, including access to the operating room, intensive care unit (ICU), and the full complement of trauma center resources. Although surgical patient volume has decreased slightly in the past month with “shelter in place” ordinances, our demands remain high (Fig. 1).
FIGURE 1.
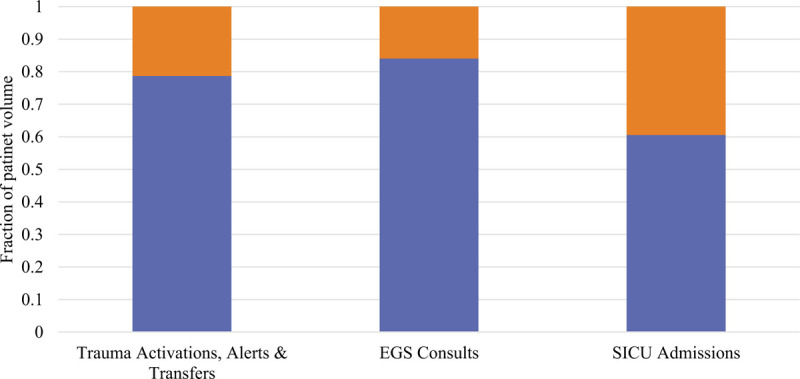
Ongoing trauma center demands during COVID-19 pandemic. Blue represents percent of volume compared with prepandemic monthly average.
HOSPITAL AND TRAUMA CENTER SURGE CAPABILITY AND CAPACITY
Know your capability and capacity, and reorganize patient housing accordingly. To best allocate resources, preparedness and proactive strategy are vital. This requires knowing surge capability and capacity and ensuring that trauma resources are protected and preserved. Anticipating maximum capacity during the pandemic and ensuring mitigation of “in-house” disease spread mandates precise attention to patient distribution within the hospital. As we increased our ICU capacity for COVID-19 patients, we dedicated the surgical ICU to be the “clean” ICU for all trauma and surgical patients and COVID-19 negative MICU patients. To accomplish this, we reorganized patients based on COVID-19 risk stratification: “baseline” community risk (absence of recent fever, cough, and shortness of breath and no clinical or radiographic concern for COVID-19), “intermediate” risk (evidence of respiratory illness as suggested clinically and/or radiographically or patient from a skilled nursing or long-term care facility), and “high” risk (fever, cough, shortness of breath, and/or other concerning clinical or radiographic findings). After stratifying risk, a patient is directed to an appropriate initial location in the hospital: baseline risk to “clean” ICU or floor, intermediate risk to MICU or “COVID-19 floor” for rule out, and high risk or confirmed COVID-19 to MICU or “COVID-19 floor.” Ultimately, this strategy of patient allocation ensures that at all times, there is an ICU free of known COVID-19 patients, and most importantly, we ensure capacity to always run a trauma center.
Have processes in place to augment and cohort personnel. After COVID-19 was identified in Colorado, DHMC promptly transitioned all clinic appointments to virtual telehealth, except for those which mandate in-person evaluation. This clinic is handled by advanced practice providers, overseen by a faculty surgeon, who work separately from the inpatient surgical team. To avoid the potential for COVID-19 spread decimating the workforce, we also expeditiously restructured our inpatient staff teams, at a faculty and resident level, to create 2 core cohorts of personnel with staggered shifts. Our current teams include trauma, emergency general surgery, and surgical ICU, with a staggered “home cohort” on call and available if any provider becomes ill or demand increases. During our morning report and ICU rounds, all providers connect via virtual meeting software.
Maintain a constant line of communication. Communication is the key as dynamic changes occur to meet ever-evolving demands. Daily email reports with consolidated information highlighting updates in key resources and practices keep surgeon staff updated and provide situational awareness on patient load and resource availability. Electronic medical record also facilitates timely data sharing, with “COVID-19” dashboards which collate the number of resulted and pending COVID-19 tests and the number of used and available ICU beds. These collated data inform implementation of each level of the surge plan, as well as trigger requests for additional resources.
Identify centralized leadership through existing national organizations. Urban, Level-1 trauma centers are uniquely poised to be “command centers” for trauma care. It is essential trauma centers reach out to regional institutions by way of Trauma Medical Directors and Trauma Program Managers to provide resources and expertise, ensuring regional trauma center capacity is preserved. This is best done by helping other trauma centers identify patients requiring transfer to high level of care and patients with potentially nonsurvivable injuries, as well as letting them know availability to receive transfers and/or consultations through telehealth platforms.
TRAUMA BAY AND TRAUMA CARE CAPABILITY AND MODIFICATIONS
Continue best practices of trauma care, with extra precautions. Operationally, for the safety of personnel, all trauma patients should be considered infected with COVID-19 until proven otherwise. As such, strict use of personal protective equipment (PPE) should be worn by all personnel for trauma activations. If a history or current symptoms of COVID-19 exist, a face mask should be placed on the patient immediately. Additionally, to identify potential COVID-19 infections and allocate patient placement, for all trauma patients who are to be admitted and we are unable to obtain history, we obtain a chest computed tomography and then test for COVID-19 accordingly.1
When it comes to personnel, less is more. It is the responsibility of the trauma team to minimize personnel in the trauma bay. Our current process is to have an emergency medicine provider present for airway and initial rapid assessment, a trauma surgery chief resident present for procedures and secondary exam, and a nurse for venipuncture and medications in the room; these personnel are overseen by the trauma surgeon attending. The remaining team remains behind closed glass doors (trauma bay becomes a negative pressure room) in a standing area. The trauma surgeon attending presence facilitates rapid assessment and activation of the remainder of the team. Additionally, immediate response of trauma attending surgeon at all levels of alerts has increased quick triage and assessment of the need for additional personnel and resources.
Develop policies and procedures for airway management and thoracic procedures. Given aerosolization of the COVID-19 by respiratory tract violation,2 it is crucial that trauma teams carefully consider emergency department thoracotomy (EDT), intubation, and tube thoracostomy. If a patient requires intubation or tube thoracostomy, only 1 provider is in the room and with appropriate PPE (assuming COVID-19 infection until proven otherwise). With respect to EDT, in the setting of blunt traumatic arrest, we maximize use of resuscitative endovascular balloon occlusion of the aorta when deemed clinically equivalent to EDT.
Recognize blood banks as a vital component of resource tracking and allocation. While our massive transfusion criteria remain unchanged, in anticipation of blood shortages, we have adopted restrictive transfusion strategies in the ICU, anticipating potential preferential resuscitation with crystalloid and lowering our threshold for vascular surgery or embolization. We also proactively stockpiled topical hemostatic agents and other resuscitative adjuncts (tranexamic acid, prothrombin complex concentrate, etc). Lastly, we are monitoring product supply at local blood banks and discussing a “walking blood bank.”
OPERATING ROOM CAPACITY AND MODIFICATIONS
Prepare for prolonged cancellation of elective cases and deferred surgery. In addition to cancelled elective surgery and transitioning clinic to telehealth, we developed a system to closely monitor surgical pathologies which may become urgent and to facilitate appropriate work up for suspected cancer diagnoses. For patients requiring surgery, a 3-point preoperative screening is undertaken: patients are screened for COVID-19 symptoms by telephone 3 days and 1 day preoperatively and then on the day of surgery. With patients who present urgently to the hospital, all those booked for laparoscopy are tested for COVID-19 preoperatively. If a patient tests positive, medical management and/or less invasive procedures are considered if possible.
Minimize personnel in the operating room during airway interrogation. Given the data which reports aerosolization of COVID-19 with intubation,3,4 our institutional policy is that personnel in the room during intubation must be wearing full PPE (N-95 masks, eye protection). Given the OR are negative pressure rooms, after intubation and extubation, all travel in and out of the room is ceased for 10 minutes.
Continue best practices of surgical care, with extra precautions. Due to concern for viral aerosolization with pneumoperitoneum,5 it is advisable to operate under the assumption that COVID-19 may be aerosolized with laparoscopy. As such, we promptly followed recommendations from the Society of American Gastrointestinal and Endoscopic Surgeons6 and the Canadian Association of General Surgeons,7 as advised by American College of Surgeons. Surgeons are supported in their discretion to preferentially perform open operations and for all laparoscopy, operative personnel don N-95 masks, high filtration systems are utilized, and cautery and energy use are minimized.
CONCLUSION
In the face of the COVID-19 pandemic, leadership, preparedness, and adaptability are paramount. It is our hope that the description of our multitiered strategic plan can serve as a model for other trauma centers. As disease spread continues and societal modifications evolve, our response must be dynamic. Intentionality, flexibility, and a little bit of grace have always been critical for optimal care of the trauma patient, as well as the well-being of those caring for patients, and this remains true now more so than ever.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Liu J, Yu H, Zhang S. The indispensable role of chest CT in the detection of coronavirus disease 2019 (COVID-19). Eur J Nucl Med Mol Imaging 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382:1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caputo KM, Byrick R, Chapman MG, et al. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anaesth 2006; 53:122–129. [DOI] [PubMed] [Google Scholar]
- 4.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wisniewski PM, Warhol MJ, Rando RF, et al. Studies on the transmission of viral disease via the CO2 laser plume and ejecta. J Reprod Med 1990; 35:1117–1123. [PubMed] [Google Scholar]
- 6. Society of American Gastrointestinal and Endoscopic Surgeons. Resources for Smoke & Gas Evacuation During Open, Laparoscopic, and Endoscopic Procedures. 2020 [cited April 6, 2020]. Available at: https://www.sages.org/resources-smoke-gas-evacuation-during-open-laparoscopic-endoscopic-procedures/. Accessed April 16, 20. [Google Scholar]
- 7. Canadian Association of General Surgeons. Statement from the CAGS MIS Committee re: Laparoscopy and the risk of aerosolization. 2020 [cited April 6, 2020]. Available at: https://cags-accg.ca/covid-19-update/resources/. Accessed April 16, 20. [Google Scholar]


