Abstract
Medicare Part D has no cap on beneficiaries’ out-of-pocket spending on outpatient prescription drugs, and, unlike Medicare Parts A and B, beneficiaries are prohibited from purchasing supplemental insurance that could provide such a cap. Historically, most beneficiaries whose annual Part D spending reached the catastrophic level were protected from unlimited personal liability by the Low-Income Subsidy (LIS). However, we found that the proportion of beneficiaries whose spending reached that level but did not qualify for the subsidy—and therefore remained liable for coinsurance—increased rapidly, from 18 percent in 2007 to 28 percent in 2015. Moreover, average total per person per year spending grew much more rapidly for those who did not qualify for the LIS than for those who did, primarily because of differences in price and utilization trends for the drugs that represented disproportionately large shares of their spending. We estimated that a cap for all Part D enrollees in 2015 would have raised monthly premiums by only $0.40–$1.31 per member. Policy makers could provide true insurance protection under Part D by implementing this approach.
The Medicare Part D program has made prescription drugs more affordable for seniors since its inception in 2006. However, growing concern about the role of high-cost drugs—including their impact on both out-of-pocket spending for beneficiaries and the fiscal sustainability of the program—has led to recent proposals to reform Part D. For example, both President Donald Trump’s budget for fiscal year 20191 and recommendations from the Medicare Payment Advisory Commission (MedPAC)2 propose significant changes to the Part D program.
One important component of these proposals is modification of the Part D benefit design to provide beneficiaries with an out-of-pocket spending cap, thereby providing important financial protection (one of the primary goals of insurance) by limiting a beneficiary’s total financial liability in a given year. The Affordable Care Act (ACA)made such caps more common in the commercial health insurance market by requiring all nongrandfathered individual and group health insurance plans to include an annual out-of-pocket maximum for all essential health benefits, including prescription drugs. However, no such statutory requirement applies to all Medicare beneficiaries for all of their Medicare-covered benefits, and beneficiaries are particularly vulnerable for their prescription drug spending.
The traditional Medicare program does not cap out-of-pocket spending for hospital and physician services covered under Medicare Parts A and B, but seniors can limit their total out-of-pocket liability for these services by enrolling in either a Medicare Advantage plan (all of which are required to have an out-of-pocket spending cap of no more than $6,700 in 2018) or a supplemental policy (such as a Medigap or retiree plan) with an out-of-pocket spending cap. However, there is no elective way for beneficiaries to cap their out-of-pocket spending for prescription drugs in Medicare Part D, even if they get this coverage in conjunction with a Medicare Advantage plan. While beneficiaries who qualify for and enroll in the Low-Income Subsidy (LIS) program do have protection against high out-of-pocket spending, because the federal government pays all or most of their cost sharing, beneficiaries not in the program are subject to potentially high out-of-pocket spending on prescription drugs, with no possible way to cap their financial liability.
Part D beneficiaries’ out-of-pocket spending varies depending on their plan, benefit phase, and LIS status. Under the 2018 standard benefit design, non-LIS beneficiaries face a $405 deductible, followed by an initial coverage period with 25 percent coinsurance up to $3,750 in total drug spending, followed in turn by a coverage gap phase (or “doughnut hole”). While beneficiaries used to pay the full cost of prescription drugs in the coverage gap, the ACA initiated the “filling in” of this doughnut hole, and in 2018 beneficiaries pay coinsurance of 35 percent for brand-name drugs and 44 percent for generic drugs in this phase.3 These coinsurance rates will be further reduced to 25 percent for both brand-name and generic drugs. The reduction would have taken place by 2020 under the ACA, but it was accelerated to 2019 under the Bipartisan Budget Act of 2018, which reduced plan liability for brand-name drugs in this phase from 25 percent to 5 percent by increasing manufacturer-financed discounts from 50 percent to 70 percent—although it did not further reduce beneficiaries’ out-of-pocket liability.
Once a beneficiary reaches the catastrophic coverage threshold, or about $8,418 in total drug spending (or $5,000 in out-of-pocket spending),4 they face 5 percent coinsurance for all prescription drug spending for the remainder of the year. Plans are responsible for 15 percent of beneficiaries’ drug spending occurring in catastrophic coverage, while the federal government finances the remaining 80 percent through the federal reinsurance program.
Historically, most beneficiaries who reached catastrophic coverage were receiving either partial or full low-income subsidies and thus were protected from high financial liability.2 However, the number of high-spending nonsubsidized beneficiaries has increased significantly in recent years, with more than one million non-LIS beneficiaries reaching catastrophic coverage in 2015.5 Moreover, spending among beneficiaries who reach catastrophic coverage has accounted for a growing share of total Part D program spending over time.2
While the ACA’s provisions to fill in the doughnut hole have reduced out-of-pocket spending in that coverage phase, rapidly rising list prices (particularly for high-cost specialty drugs) have accelerated the growth in out-of-pocket spending in the catastrophic phase.2 Moreover, high prescription drug spending is generally more persistent than high medical spending, though this persistence varies across conditions.6,7 Thus, in the absence of a cap, many beneficiaries are likely to face high and growing out-of-pocket spending on prescription drugs year after year—particularly people with chronic conditions that are often treated by persistent use of high-cost prescription drugs, such as rheumatoid arthritis and multiple sclerosis.
In this article we evaluate trends in prescription drug spending among LIS and non-LIS beneficiaries who reach catastrophic coverage. Because the former are already protected from high financial liability whereas the latter are not, we highlight differential trends in beneficiaries who reach catastrophic coverage by LIS status and discuss the potential impact of introducing a cap on out-of-pocket spending in Medicare Part D.
Study Data And Methods
Data
We evaluated data from master beneficiary summary files and prescription drug event files from a 100 percent sample of Medicare beneficiaries through a data use agreement with the Virtual Research Data Center of the Centers for Medicare and Medicaid Services (CMS). We restricted our sample to Medicare beneficiaries enrolled in Part D plans, including both stand-alone prescription drug plans and Medicare Advantage plans with prescription drug benefits, from 2007 through 2015. Beneficiaries were categorized as LIS if they qualified for extra help with premiums and cost sharing (either full or partial LIS subsidies). We included any beneficiaries who were ever enrolled at any point in the year in our sample, and we defined beneficiaries as LIS or non-LIS according to their LIS enrollment status in the last month of enrollment in each year.8
Spending Trends
We first analyzed trends in total enrollment and the number of beneficiaries who reached catastrophic coverage, by LIS status. We then evaluated the proportion of total prescription drug expenditures that occurred in the catastrophic coverage phase, by LIS status. We categorized expenditures as occurring above or below the catastrophic coverage threshold using the beneficiaries’ cumulative true out-of-pocket (TrOOP) spending for each claim and comparing this to the year-specific out-of-pocket spending threshold for crossing into catastrophic coverage.9
Next, we assessed trends in average total spending for beneficiaries who reached catastrophic coverage, by LIS status. To do so, we computed mean per beneficiary measures of total annual prescription drug spending by summing total prescription drug expenditures (across all benefit phases) for all beneficiaries who reached catastrophic coverage and dividing that by the number of beneficiaries who reached that phase in each year.
Because we found faster growth in per beneficiary spending among non-LIS than among LIS beneficiaries who reached catastrophic coverage, we analyzed differences in the drug classes that accounted for the majority of spending for the two groups. Specifically, we determined the proportion of spending that occurred in the catastrophic coverage phase by drug class, separately for LIS and non-LIS beneficiaries. To do so, we summed total spending occurring in catastrophic coverage by drug class and divided that by total spending occurring in catastrophic coverage. We defined drug classes by grouping therapeutic classes specified by First Databank into the condition they treat. We present results for the top nine drug classes in 2015 that accounted for the majority of spending in catastrophic coverage, grouped by those that represent disproportionate shares of catastrophic spending for non-LIS and LIS beneficiaries, respectively. Additionally, for these top nine drug classes, we computed average thirty-day prices by summing total expenditures that occurred in the catastrophic coverage phase in each class across all beneficiaries, divided by total days supplied in that phase and class, and multiplied by thirty.
Limitations
Our analyses were limited by the fact that claims data for 2015 were the most recent available to us. Thus, to the extent that trends have changed in more recent years, we were unable to capture these dynamics in our analyses and estimates of the impact of potential reforms to the Medicare Part D program. Additionally, we did not adjust our data on trends to account for potential changes in health status or other demographic characteristics of enrollees that could affect drug spending over time.
Study Results
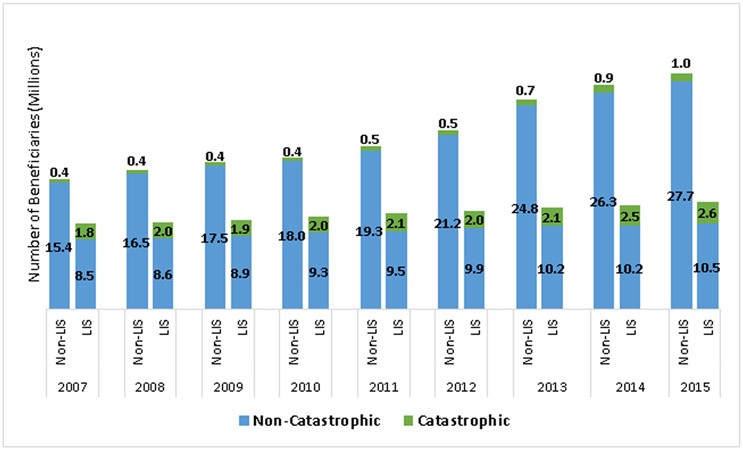
From 2007 to 2015, the total number of Part D beneficiaries increased from twenty-six million to forty-two million, but the proportion of LIS beneficiaries fell from 40 percent to 31 percent (exhibit 1, online appendix exhibit 1). The likelihood of reaching catastrophic coverage was much higher for LIS than for non-LIS beneficiaries: About 17–20 percent of LIS beneficiaries reached catastrophic coverage in each year of the study period, compared to about 2–3.5 percent of non-LIS beneficiaries (online appendix exhibit 1).10 The share of LIS and non-LIS beneficiaries who reached catastrophic coverage was higher in 2014 and 2015 than in earlier years of the study period (an unweighted average of 3.4 percent of non-LIS and 19.7 percent of LIS beneficiaries in the period 2014–15, compared with an unweighted average of 2.4 percent of non-LIS and 17.8 percent of LIS beneficiaries in 2007–13) (online appendix exhibit 1). Additionally, non-LIS beneficiaries represented a growing share of those reaching catastrophic coverage, increasing from 18 percent in 2007 to 28 percent in 2015 (online appendix exhibit 1). This increase likely reflects a combination of the fact that non-LIS beneficiaries grew disproportionately as a share of overall Part D beneficiaries, and the fact that the ACA’s manufacturer-financed discounts for brand-name drugs taken by non-LIS beneficiaries while in the doughnut hole counted toward beneficiaries’ true out-of-pocket spending accumulation, which is the metric that moves beneficiaries through benefit phases. Thus, the change to counting manufacturer-financed discounts toward this spending has likely also contributed to the disproportionate growth in the share of non-LIS beneficiaries among those reaching catastrophic coverage by reducing the actual out-of-pocket spending required for them to do so.
Exhibit 1 (Figure). Trends in Part D Enrollment (in Millions), by LIS Status and Reaching Catastrophic Coverage.
Source: Authors’ analysis of Centers for Medicare and Medicaid Services beneficiary summary file and prescription drug event files from a 100 percent sample of Medicare beneficiaries, 2007-2015.
Notes: The sample includes beneficiaries enrolled in stand-alone prescription drug plans or in Medicare Advantage plans that had prescription drug coverage. Low Income Subsidy (LIS) beneficiaries include those receiving both partial and full benefits; beneficiary LIS status was assigned according to their LIS eligibility status in the last month of enrollment in each year. Beneficiaries were categorized as reaching catastrophic coverage if they had one or more prescription drug claims that included spending in the catastrophic coverage benefit phase.
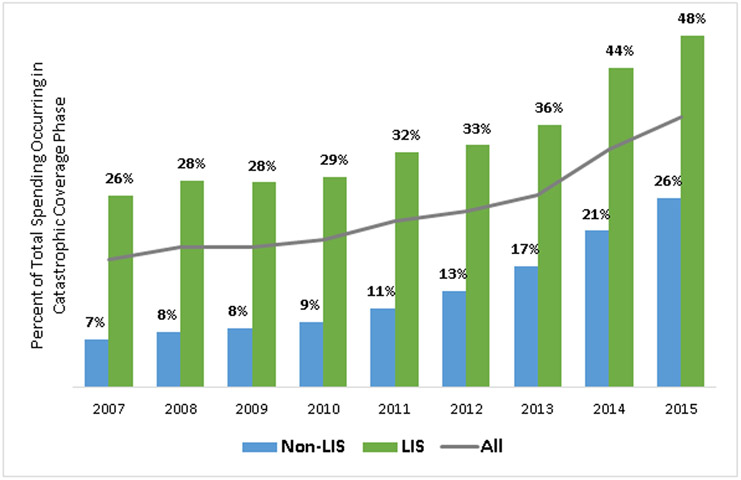
Despite the fact that the share of overall beneficiaries reaching catastrophic coverage was relatively stable over the study period, the proportion of total Part D expenditures occurring in catastrophic coverage increased considerably, from 18 percent in 2007 to 37 percent in 2015 (exhibit 2). The proportion of expenditures occurring in catastrophic coverage was higher for LIS than non-LIS beneficiaries (in 2015, 48 percent versus 26 percent), in part because a much higher share of LIS beneficiaries reached catastrophic coverage. However, the proportion of spending that occurred in catastrophic coverage grew much more rapidly for non-LIS beneficiaries from 2007 to 2015 (a 292 percent increase versus an 84 percent increase).
Exhibit 2 (Figure). Percent of Total Spending Occurring in the Catastrophic Coverage Phase, by LIS Status and Year.
Source: Authors’ analysis of Centers for Medicare and Medicaid Services beneficiary summary file and prescription drug event files from a 100 percent sample of Medicare beneficiaries, 2007-2015.
Notes: The sample includes beneficiaries enrolled in stand-alone prescription drug plans or in Medicare Advantage plans that had prescription drug coverage. Low Income Subsidy (LIS) beneficiaries include those receiving both partial and full benefits; beneficiary LIS status was assigned according to their LIS eligibility status in the last month of enrollment in each year. Beneficiaries were categorized as reaching catastrophic coverage if they had one or more prescription drug claims that included spending in the catastrophic coverage benefit phase. Spending represents list (i.e., pre-rebate) prices.
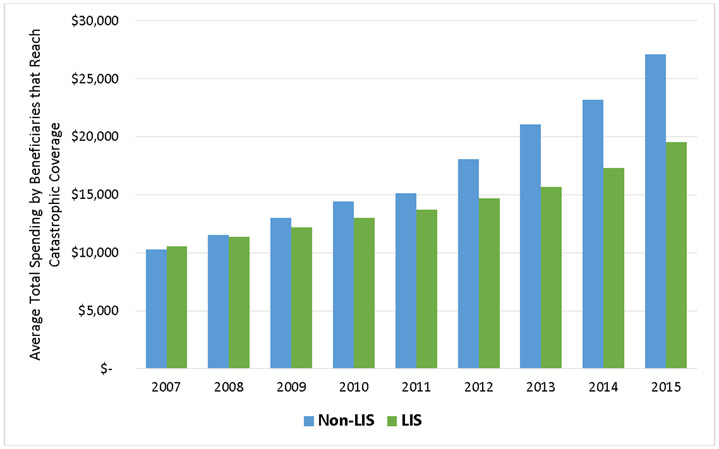
This higher growth rate for non-LIS beneficiaries was primarily driven by faster spending growth per beneficiary who reached catastrophic coverage (exhibit 3). For non-LIS beneficiaries, average total annual spending (across all benefit phases) per beneficiary who reached catastrophic coverage increased 163 percent, from $10,300 in 2007 to $27,095 in 2015. In comparison, for LIS beneficiaries, average total annual spending per beneficiary who reached catastrophic coverage increased 85 percent, from $10,570 in 2007 to $19,554 in 2015. Thus, whereas LIS and non-LIS beneficiaries who reached catastrophic coverage had similar spending levels in the early years of our study period, by 2015 non-LIS beneficiaries reaching catastrophic coverage had spending that was 39 percent higher than that of LIS beneficiaries.
Exhibit 3 (Figure). Average Total Annual Spending by Beneficiaries that Reach Catastrophic Coverage, by LIS Status and Year.
Source: Authors’ analysis of Centers for Medicare and Medicaid Services beneficiary summary file and prescription drug event files from a 100 percent sample of Medicare beneficiaries, 2007-2015.
Notes: The sample includes beneficiaries enrolled in stand-alone prescription drug plans or in Medicare Advantage plans that had prescription drug coverage. Low Income Subsidy (LIS) beneficiaries include those receiving both partial and full benefits; beneficiary LIS status was assigned according to their LIS eligibility status in the last month of enrollment in each year. Beneficiaries were categorized as reaching catastrophic coverage if they had one or more prescription drug claims that included spending in the catastrophic coverage benefit phase. Totals include all spending (across all benefit phases) by beneficiaries that reach catastrophic coverage. All spending is reported in nominal amounts and represent list (i.e., pre-rebate) prices.
These differences in per beneficiary spending between LIS and non-LIS beneficiaries who reached catastrophic coverage were largely attributable to differences in the drug classes used by the two groups of beneficiaries (and the differences in prices and price growth across these classes). While spending on drugs used to treat hepatitis C represented a considerable portion of drug spending among both LIS and non-LIS beneficiaries who reached catastrophic coverage in 2014 and 2015 (due to the introduction of Sovaldi, Harvoni, and Viekira Pak), spending on other drug classes tended to be more concentrated among one of the two groups over the study period. Non-LIS beneficiaries were more likely to use drugs for treating cancer, multiple sclerosis, rheumatoid arthritis, and pulmonary hypertension than subsidized beneficiaries were, whereas the LIS population was more likely to use medications for mental health, diabetes, HIV/AIDS, and pain (exhibit 4 and appendix exhibit 2).10 More specifically, spending on cancer drugs accounted for 30 percent of all catastrophic spending by non-LIS beneficiaries who reached that benefit phase in 2015, compared to 7 percent for LIS beneficiaries. In contrast, LIS spending was highest on drugs used to treat mental health conditions (other than hepatitis C drugs)—accounting for 12 percent of all catastrophic spending by LIS beneficiaries who reached that benefit phase in in 2015, compared to 2 percent for non-LIS beneficiaries.
Exhibit 4:
Shares of average annual spending in the catastrophic coverage benefit phase and average 30-day price in 2015 and price change from 2007, by drug class and enrollment in the Low-Income Subsidy (LIS) program
| Share of 2015 spending in catastrophic coverage |
Average 2015 30-day price |
Average annual price change, 2007– 15 |
||
|---|---|---|---|---|
| Drug class | Non-LIS | LIS | ||
| Higher share of non-LIS than LIS catastrophic spending | ||||
| Cancer | 30% | 7% | $5,154 | 20% |
| Multiple sclerosis | 9 | 6 | 5,698 | 16 |
| Rheumatoid arthritis | 5 | 4 | 3,870 | 11 |
| Pulmonary hypertension | 4 | 2 | 5,099 | 7 |
| Total or weighted average | 48 | 19 | 5,018 | 16 |
| Higher share of LIS than non-LIS catastrophic spending | ||||
| Mental healtha | 2 | 12 | 178 | −1 |
| Diabetes | 7 | 10 | 327 | 16 |
| HIV/AIDS | 4 | 8 | 1,184 | 8 |
| Pain | 2 | 3 | 180 | 1 |
| Total or weighted average | 14 | 33 | 278 | 5 |
| High share of both non-LIS and LIS catastrophic spending | ||||
| Hepatitis C | 14 | 16 | 27,620 | 47 |
SOURCE Authors’ analysis of data for 2007–15 from the Centers for Medicare and Medicaid Services’ master beneficiary summary files and prescription drug event files for a 100 percent sample of Medicare beneficiaries. NOTES The sample, LIS beneficiaries, and catastrophic coverage status are explained in the notes to exhibit 1. Prices are reported in nominal amounts and represent list prices—that is, before any rebates. Weighted average 30-day prices were computed by dividing total spending that occurred in the catastrophic coverage phase across all beneficiaries (by LIS status) across each of the top four classes, divided by total days supplied in that phase across those top four classes, and multiplying by thirty; essentially weighting the average price of each class by its days supplied. Price increases over time could be due to multiple factors, such as the introduction of new, higher-price products in the drug class; increasing prices of existing products; substitution of higher-price products for lower-price products in the class; or some combination of the three.
Includes antidepressants, antipsychotics, and anticonvulsants.
Differences in prices and price growth across drugs used to treat these different conditions played an important role in explaining the differences in the growth of per beneficiary total spending between LIS and non-LIS beneficiaries reaching catastrophic coverage (as seen in exhibit 3). In 2015 the weighted average thirty-day price among the top four drug classes used more heavily by the non-LIS population reaching catastrophic coverage was $5,018 (exhibit 4). Moreover, the weighted average annual price increase for these drug classes from 2007 to 2015 was 16 percent. In contrast, the weighted average thirty-day price among the top four drug classes used more heavily by the LIS population reaching catastrophic coverage was $278, with a 5 percent weighted average annual price increase from 2007 to 2015. That is, drug classes used more heavily by the non-LIS population reaching catastrophic coverage had much higher prices and faster price growth than those used more heavily by the LIS population reaching catastrophic coverage. However, we note that these increases could be due to multiple factors, such as the introduction of new, higher-price products in a class; increasing prices of existing medications; substitution of higher-price drugs for lower-price ones in the class; or some combination of the three.
Discussion
Though many Part D beneficiaries who reach catastrophic coverage are protected from high financial liability because of the presence of low-income subsidies, we found considerable increases in both the number and proportion of non–Low-Income Subsidy beneficiaries reaching catastrophic coverage. Moreover, we found that average total per person spending has grown much more rapidly for non-LIS beneficiaries who reach catastrophic coverage, compared to LIS beneficiaries—primarily because of differences in the price and utilization trends of cancer and mental health drugs, which represent disproportionately large shares of spending among non-LIS and LIS beneficiaries, respectively. Thus, the population most susceptible to high and unlimited financial liability as a result of the lack of an out-of-pocket spending cap in Medicare Part D—that is, non-LIS beneficiaries who reach catastrophic coverage—has grown the most in terms of both the number of beneficiaries and the magnitude of their spending.
As a result, we believe that policy makers should consider implementing an out-of-pocket spending cap in Medicare Part D. Such a policy would be consistent with other recent changes in the ACA that require all commercial plans to cap out-of-pocket spending on essential health benefits, including prescription drugs. A proposal to cap Part D out-of-pocket spending has been put forth by Sen. Ron Wyden (D-OR)—the Reducing Existing Costs Associated with Pharmaceuticals for Seniors Act (or the RxCAP Act) of 2016—which would eliminate beneficiary cost sharing in the catastrophic coverage phase, but the proposal has not been taken up by the full Senate. Moreover, such a cap has also been proposed, in conjunction with broader Part D reforms, by MedPAC2 and the Trump administration.1
Premium Impact
Capping beneficiary cost sharing at the catastrophic coverage threshold would necessarily increase Part D plans’ spending, assuming no changes to the generosity of the federal reinsurance program. Plans would likely increase premiums to offset this increased liability. Using our data on 2015 enrollment and catastrophic spending, we estimated that implementing a cap on beneficiary out-of-pocket spending would result in a premium increase of $0.40–$1.31 per member per month, depending on whether such a policy change shifted the liability for beneficiary cost sharing in catastrophic coverage to plans for all beneficiaries (both non-LIS and LIS) or only to plans for non-LIS beneficiaries (where the low-income cost-sharing subsidy program would continue to finance this liability for LIS beneficiaries) (see appendix for details).10 This represents about a 1–4 percent premium increase, based on the $30 monthly average beneficiary-paid premium for a basic Part D plan in 2015.11
Insurance Is About Risk Protection
While such a premium increase would be minimal when spread across a large population of beneficiaries, the impact of the financial protection it would bestow would be considerable for the small fraction of non-LIS beneficiaries with very high drug spending. Moreover, it would confer added value in the form of financial protection from the uncertain risk of potentially very high out-of-pocket spending on prescription drugs to all Part D beneficiaries.
This point of insurance protection for all beneficiaries is particularly compelling due to the fact that 16 percent of non-LIS beneficiaries who reached catastrophic coverage in 2015 had a single claim whose total price paid was more than $7,062 (the catastrophic total spending threshold in 2015)—meaning that that single claim would have resulted in the beneficiary’s reaching catastrophic coverage. In other words, it is not simply that beneficiaries must take numerous prescription drugs to reach catastrophic coverage, but rather that all beneficiaries would benefit from insurance against the possibility of needing a single very costly drug.
The Cost Of A Cap In Perspective
To put this in perspective with other recent policy changes, the ACA’s provisions to fill in the doughnut hole gradually increased plan liability to 25 percent and 75 percent of spending on brand-name and generic drugs, respectively, for all non-LIS beneficiaries in the doughnut hole by 2020—though, as noted above, the Bipartisan Budget Act of 2018 reduced plan liability to 5 percent of spending for brand-name drugs by increasing manufacturer-financed discounts from 50 percent to 70 percent, beginning in 2019. We computed what the additional plan liability would have been for our sample, had either of these policies been fully implemented in 2015. We estimated that the increased plan liability attributable to closing the doughnut hole would have resulted in a premium increase of $1.52–$2.71 per member per month, under the Bipartisan Budget Act and the ACA, respectively (see appendix for details).10
These results underscore the fact that there has clearly been political will in the past to make changes to Part D that led to higher premiums and Medicare spending to pursue the goal of reducing cost sharing for a much broader population reaching the doughnut hole. While the political benefit of a change that positively affects a larger share of beneficiaries by subsidizing their doughnut-hole cost sharing is clear, protecting all beneficiaries from high and unlimited financial liability would arguably be more consistent with the risk-protecting goals of insurance.
Potential Unintended Consequences
Though introducing an out-of-pocket spending cap would protect beneficiaries from high financial liability, doing so could result in increased utilization or prices due to lower cost sharing, which could increase the potential premium impact. However, evidence suggests that demand for high-cost drugs is relatively inelastic.12,13 Moreover, it is not clear that the 2018 policy of 5 percent coinsurance after a beneficiary has already accrued over $8,000 in total drug expenditures is imposing a significant demand restraint in such a way that capping out-of-pocket spending liability would result in sizable utilization increases. Furthermore, the potential impact on utilization or prices of eliminating 5 percent coinsurance in catastrophic coverage is likely less than the potential impact of the ACA’s and Bipartisan Budget Act’s provisions to fill in the doughnut hole. Nonetheless, if policy makers are concerned about potential adverse consequences from the lack of a demand restraint under an out-of-pocket spending cap, a policy proposal that would be less burdensome to enrollees—such as nominal copayments rather than the current open-ended coinsurance, similar to what partial LIS enrollees currently pay above the catastrophic threshold—could be considered.
The potential premium impact also could increase if the trends we observed continue and the share of non-LIS catastrophic spending continues to grow, due to proportionally larger numbers of non-LIS beneficiaries reaching catastrophic coverage, higher spending per beneficiary reaching catastrophic coverage, or both. However, while the potential premium impact may be understated if these trends continue, we note that not capping out-of-pocket spending in that case would lead to even higher financial burden for a larger number of beneficiaries, and thus redistributing that financial liability over the broader Part D population would likely still be a preferable policy trade-off.
Broader Part D Reforms
While capping out-of-pocket spending would limit beneficiaries’ financial liability, it would not address the broader issue of high and increasing catastrophic spending and the resulting impact on federal spending on Part D. In fact, federal spending on the reinsurance program, which finances 80 percent of total catastrophic spending, was the fastest-growing component of federal Part D expenditures during our study period, and as of 2014 it overtook the LIS program to become the largest component of federal spending on Part D.14 There is some concern that the structure of the reinsurance program may lack adequate financial incentives for plans to rigorously control spending, since they face liability for only 15 percent of catastrophic expenditures.15
However, other institutional features of the Part D market may also have had an effect on the growth in catastrophic expenditures. For example, beneficiary cost sharing (and, thus, a beneficiary’s progression through the Part D benefit phases) is based on the negotiated list price of a drug, despite the fact that plans often receive rebates that ultimately lower the overall net cost. Because of the presence of the federal reinsurance program, plans have an incentive to move high-cost beneficiaries to catastrophic coverage more rapidly, so that they reduce their liability to 15 percent of spending—which thus generates an incentive for plans to prefer higher list prices with higher rebates as opposed to negotiating lower list prices.11,16 This ultimately harms beneficiaries because they pay 5 percent coinsurance in catastrophic coverage that is based on an inflated list price rather than on the final net price. Moreover, nearly all plans charge coinsurance (rather than flat copayments) for all specialty and nonpreferred brand-name drugs, and an increasing share also use coinsurance even for preferred brand-name drugs—which means that beneficiaries pay cost sharing based on these inflated list prices throughout all benefit phases, not just in catastrophic coverage.17 Because these rebates are primarily used by plans to lower premiums, this in turn means that beneficiaries taking these high-cost drugs are actually subsidizing the premiums of their lower-spending counterparts as a result of paying coinsurance on inflated list prices. Though plans are ultimately required to share these rebates with CMS in the sense that federal reinsurance payments to plans are based on plans’ catastrophic spending net of these rebates, there is no such reconciliation with the beneficiaries who have paid coinsurance based on these inflated list prices. In fact, average Part D rebates have also increased considerably in recent years, which suggests that increases in out-of-pocket spending among beneficiaries who reach catastrophic coverage may be partly due to increasing list prices.18,19
Reforms to the Part D program in addition to capping out-of-pocket spending have been proposed. For example, in an effort to address concerns about beneficiaries who take high-cost drugs and pay cost sharing based on list rather than net prices, CMS released a request for information in November 2017 about how the agency might require plans to pass a substantial portion of these rebates through to beneficiaries at the point of sale,20 and this was also included in President Trump’s budget.1 Additionally, to address concerns about increasing federal reinsurance spending and perverse incentives for plans, in June 2016 MedPAC proposed reforms (also included in the president’s budget) to the structure of the reinsurance program, including transitioning Medicare’s reinsurance subsidy from 80 percent to 20 percent (while maintaining Medicare’s overall 74.5 percent subsidy of basic Part D benefits by increasing capitated payments to plans) and no longer counting manufacturer-financed discounts toward true out-of-pocket spending accumulation.2, 21 Such a proposal could reduce the number of beneficiaries reaching catastrophic coverage and increase plans’ financial incentives to control spending. It could also limit plans’ incentives to underbid on their expected catastrophic spending—which has resulted in excess payments from the federal government to plans in recent years, since reinsurance payments to plans are ultimately based on actual rather than expected catastrophic spending, whereas overbidding on precatastrophic spending results in federal premium subsidies paid to plans that are not reconciled after the fact.15(ch6) Thus, such reforms to the structure of Part D financing could reduce perverse plan incentives that currently work to encourage the growth of catastrophic spending, which would benefit high-cost beneficiaries. However, further analysis is needed to estimate the reforms’ likely impact on both beneficiaries and federal spending.
Conclusion
Despite recent legislative efforts to broadly expand the presence of out-of-pocket spending caps in the commercial insurance market, Medicare beneficiaries that are not receiving the Low-Income Subsidy have no way to limit their financial liability for prescription drug spending. Policy makers should consider implementing an out-of-pocket spending cap in the Part D program to provide true insurance protection for beneficiaries. However, while imposing such a cap would protect beneficiaries, it would not address the broader concerns about increasing federal spending on the Part D reinsurance program or the underlying concerns about increasing drug prices. Future work is needed to evaluate the potential impact of broader changes to ensure the sustainability of federal financing for the Part D program.
Supplementary Material
Acknowledgment
An earlier version of this article was presented at the National Health Policy Conference, Washington, D.C., February 6, 2018 and at the AcademyHealth Annual Research Meeting, Seattle, WA, June 24, 2018. Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health (Award Nos. P01AG033559 and P30AG024968). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Research reported here was also generously supported by the Leonard D. Schaeffer Center for Health Policy and Economics of the University of Southern California, through the Centers for Medicare and Medicaid Services’ data use agreement number 51738 (“The Past, Present, and Future of Medicare Policy”). The authors thank Laura Gascue and Patty St. Clair for excellent programming assistance, Rachel Schmidt for helpful discussions, and the Health Affairs editors and two anonymous reviewers for helpful suggestions.
Contributor Information
E Trish, department of health policy and management at the Price School of Public Policy, Leonard D. Schaeffer Center for Health Policy and Economics, University of Southern California, in Los Angeles..
J Xu, Price School of Public Policy and the Leonard D. Schaeffer Center for Health Policy and Economics, University of Southern California..
G. Joyce, department of pharmaceutical and health economics at the School of Pharmacy, Leonard D. Schaeffer Center for Health Policy and Economics, University of Southern California..
Notes
- 1.Office of Management and Budget. An American budget, fiscal year 2019 [Internet] Washington (DC): Government Publishing Office; [cited 2018 Apr 30]. Available from: https://www.whitehouse.gov/wp-content/uploads/2018/02/budget-fy2019.pdf [Google Scholar]
- 2.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System [Internet] Washington (DC): MedPAC; 2016. June Chapter 6, Improving Medicare Part D; [cited 2018 May 31]. Available from: http://www.medpac.gov/docs/default-source/reports/chapter-6-improving-medicare-part-d-june-2016-report-.pdf [Google Scholar]
- 3.Cost sharing can vary from this standard benefit design, but “basic alternative” plans must be actuarially equivalent to this standard plan. “Enhanced alternative” plans may reduce beneficiary cost sharing but generally charge higher premiums and still do not have an out-of-pocket spending cap. [Google Scholar]
- 4.The $5,000 limit includes the 50 percent manufacturer-financed doughnut-hole discounts for brand-name drugs, even though they are not actually incurred as out-of-pocket spending.
- 5.Cubanski J, Newman T, Orgera K, Damico A. No limit: Medicare Part D enrollees exposed to high out-of-pocket drug costs without a hard cap on spending [Internet]. San Francisco (CA): Henry J Kaiser Family Foundation; 2017. November [cited 2018 Apr 30]. (Issue Brief). Available from: http://files.kff.org/attachment/Issue-Brief-No-Limit-Medicare-Part-D-Enrollees-Exposed-to-High-Out-of-Pocket-Drug-Costs-Without-a-Hard-Cap-on-Spending [Google Scholar]
- 6.Garber AM, MaCurdy TE, McClellan MB. Persistence of Medicare expenditures among elderly beneficiaries. In: Garber AM, editor. Frontiers in health policy research. Vol. 1 Cambridge (MA): MIT Press; 1998. p. 153–80. [Google Scholar]
- 7.Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood). 2007;26(3):808–16 PubMed. [DOI] [PubMed] [Google Scholar]
- 8.CMS.gov. Defining Medicare-Medicaid Enrollees in CMS data sources (a.k.a. defining duals) [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2013. January 9 [cited 2018 Apr 30]. Available from: https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/Downloads/MMCO_Definition_of_Dual_Eligible.pdf [Google Scholar]
- 9.For “straddle claims” (those that included expenditures both below and above the catastrophic coverage threshold), we used our estimates of true out-of-pocket spending accumulation to proportionally attribute spending across phases. [Google Scholar]
- 10.To access the appendix, click on the Details tab of the article online.
- 11.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy [Internet] Washington (DC): MedPAC; 2017. March Chapter 14, Status report on the Medicare prescription drug program (Part D); [cited 2018 Apr 30]. Available from: http://www.medpac.gov/docs/default-source/reports/mar17_medpac_ch14.pdf [Google Scholar]
- 12.Goldman DP, Joyce GF, Lawless G, Crown WH, Willey V. Benefit design and specialty drug use. Health Aff (Millwood). 2006;25(5):1319–31 PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung J, Xu WY, Cheong C. In-gap discounts in Medicare Part D and specialty drug use. Am J Manag Care. 2017;23(9):553–9 PubMed. [PMC free article] [PubMed] [Google Scholar]
- 14.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy [Internet] Washington (DC): MedPAC; 2016. March Chapter 13, Status report on Part D; [cited 2018 Apr 30]. Available from: http://www.medpac.gov/docs/default-source/reports/chapter-13-status-report-on-part-d-march-2016-report-.pdf [Google Scholar]
- 15.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the health care delivery system [Internet]. Washington (DC): MedPAC; 2015. June [cited 2018 Apr 30]. Available from: http://www.medpac.gov/docs/default-source/reports/june-2015-report-to-the-congress-medicare-and-the-health-care-delivery-system.pdf?sfvrsn=0 [Google Scholar]
- 16.Dusetzina SB, Conti RM, Yu NL, Bach PB. Association of prescription drug price rebates in Medicare Part D with patient out-of-pocket and federal spending. JAMA Intern Med. 2017;177(8):1185–8 PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cubanski J, Damico A, Hoadley J, Orgera K, Neuman T. Medicare Part D: a first look at prescription drug plans in 2018 [Internet]. San Francisco (CA): Henry J Kaiser Family Foundation; 2017. October [cited 2018 Apr 30]. (Issue Brief). Available from: http://files.kff.org/attachment/Issue-Brief-Medicare-Part-D-A-First-Look-at-Prescription-Drug-Plans-in-2018 [Google Scholar]
- 18.CMS.gov. Medicare Part D—direct and indirect remuneration (DIR) [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2017. January 19 [cited 2018 Apr 30]. (Fact Sheet). Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017–01–19–2.html [Google Scholar]
- 19.Boards of Trustees. 2017 annual report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2017. July 13 [cited 2018 Apr 30]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2017.pdf [Google Scholar]
- 20.Centers for Medicare and Medicaid Services. Medicare Program; contract year 2019 policy and technical changes to the Medicare Advantage, Medicare Cost Plan, Medicare fee-for-service, the Medicare prescription drug benefit programs, and the PACE program: proposed rule. Federal Register [serial on the Internet]. 2017. November 28 [cited 2018 Apr 30]. Available from: https://www.federalregister.gov/documents/2017/11/28/2017-25068/medicare-program-contract-year-2019-policy-and-technical-changes-to-the-medicare-advantage-medicare [PubMed] [Google Scholar]
- 21.The recommendations also would permit plans to introduce modest cost sharing for LIS beneficiaries to encourage them to use lower-cost alternatives.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.