Abstract
Background:
African Americans have disproportionate rates of cardiovascular disease (CVD). Psychosocial stress may contribute to this disparity. Previous trials on stress reduction with the Transcendental Meditation (TM) program have reported improvements in CVD risk factors, surrogate endpoints and mortality in African Americans and other populations.
Methods and Results:
This was a randomized controlled trial of 201 African American men and women with coronary heart disease (CHD) who were randomized to the TM program or health education. The primary end point was the composite of all-cause mortality, myocardial infarction, or stroke. Secondary endpoints included the composite of cardiovascular mortality, revascularizations, and cardiovascular hospitalizations; blood pressure (BP); psychosocial stress factors; and lifestyle behaviors. Over an average follow-up of 5.4 years, there was a 48% risk reduction in the primary end point in the TM group (hazard ratio [HR], 0.52; 95% confidence interval[CI], 0.29-0.92)(P =.025). The TM group also showed a 24% risk reduction in the secondary end point (HR, 0.76; 95% CI, 0.51-0.1.13) (P =.17). There were reductions of 4.9 mm Hg in systolic BP (95% CI −8.3 to –1.5 mm Hg) (P =.01) and anger expression (P < .05 for all scales). Adherence was associated with survival.
Conclusion:
A selected mind-body intervention, the Transcendental Meditation program, significantly reduced risk for mortality, myocardial infarction and stroke in CHD patients. These changes were associated with lower BP and psychosocial stress factors. Therefore, this practice may be clinically useful in the secondary prevention of CVD.
Clinical Trial Registration:
www.clinicaltrials.gov; NCT01299935
Keywords: preventive cardiology, integrative cardiology, health disparities, stress reduction, meditation, coronary heart disease, cardiovascular disease, mind-body medicine
BACKGROUND
Cardiovascular disease (CVD) is the leading cause of death in the United States and the world. 1, 2 African Americans suffer from disproportionately high rates of CVD morbidity and mortality.1,3 Substantial evidence indicates that psychosocial stress contributes to the onset and progression of CVD.4-8 The attributable risk associated with psychosocial stress factors across diverse populations is similar to traditional CVD risk factors. 8 Psychological distress factors, including depression, anger, hostility and anxiety predict CVD clinical events.9-11 The disparity in CVD in African Americans may be related to disproportionate levels of psychosocial and environmental stress.12-16 Randomized controlled trials of stress reduction using the Transcendental Meditation (TM) program have reported decreases in CVD risk factors, surrogate end points, and mortality in African Americans and the general population.17-24 The overall objective of this trial was to evaluate the effects of practice of the TM program in the secondary prevention of CVD in African Americans.
METHODS
STUDY DESIGN
The trial was conducted between March 1998 and July 2007 in 2 phases. The first phase occurred from March 1998 to April 2003. After a hiatus in funding, the second phase was conducted from March 2004 to July 2007. All phase 1 subjects were invited to participate in phase 2. Subjects provided written informed consent separately for each of the 2 phases.
The clinical site was the Department of Medicine, Medical College of Wisconsin, Milwaukee and the administrative and data coordinating center was the Institute for Natural Medicine and Prevention, Maharishi University of Management, Fairfield, Iowa. The institutional review boards of both institutions approved the protocol. The trial was monitored by an independent data and safety monitoring board (DSMB).
PARTICIPANTS
Eligible patients were African American men and women with angiographic evidence of at least one coronary artery with ≥ 50% stenosis. Exclusion criteria were acute myocardial infarction (MI), stroke, or coronary revascularization within the previous 3 months; chronic heart failure with ejection fraction < 20%; cognitive impairment; and noncardiac life-threatening illness. Subjects continued usual medical care throughout the study.
Subjects were identified from the African American Heart Health Registry of the Medical College of Wisconsin and other databases of Milwaukee area hospitals. Each patient’s physician gave permission for study participation.
PROCEDURE
Subjects were randomly assigned to either the TM or health education (HE) arms using a stratified block design. The strata were gender (M/F), age (above and below median for each cohort), and lipid-lowering medication (yes/no). Stratification factors were based on previous literature indicating that these are strong predictors of cardiovascular clinical events-fatal and nonfatal 25, 26. Random allocation was performed by the study biostatistician who concealed the allocation schedule and conveyed the assignments to the study coordinator. Investigators, data collectors and data management staff were blinded to group assignment. Intervention groups met separately to minimize contamination. Since double blinding in behavioral trials is generally not feasible, this was a single-blinded trial. 27
Subjects were assessed at baseline, month 3 and every 6 months thereafter for clinical events, blood pressure (BP), body mass index (BMI) and adherence. Lifestyle behaviors (diet, exercise and substance use) and psychosocial distress factors were assessed annually.
OUTCOMES
The primary end point was the time to first event of the composite of all-cause mortality, nonfatal MI or nonfatal stroke. The secondary clinical end point was time to first event for the composite of cardiovascular mortality, nonfatal MI, nonfatal stroke, coronary revascularization or hospitalization for ischemic heart disease-non-MI or heart failure. Additional secondary, intermediate end points included BP, smoking, alcohol, body mass index, diet, exercise and psychological distress.
Mortality and cause of death were determined from death certificates and the National Death Index.28, 29 At semiannual study visits, participants reported hospitalizations. Nonfatal events were confirmed from hospital discharge summaries. All clinical end points were adjudicated by a blinded, independent reviewer who applied standardized and validated criteria.30
Three successive BP measurements were taken with a mercury sphygmomanometer in the seated positon. BMI was calculated as weight/height2. Dietary patterns were assessed with the Block Dietary Food Consumption Questionnaire.31 Smoking and alcohol use were determined from weekly recall questionnaires.32 A modified Minnesota Leisure Time Physical Activity Questionnaire was used for exercise.33 Psychological distress factors were assessed with the Center for Epidemiological Studies Depression Scale (CES-D) for depression,34, 35 the Cook-Medley Hostility Inventory composite score (CMHI) for hostility36, 37 and the Anger Expression (AX) scale for anger-in, anger-out, anger-control and total anger.38
Expectation of treatment benefits was assessed by questionnaire at baseline in a subset of 71 subjects. Regularity of home practice for both groups was determined by questionnaire at each posttesting session. Practice of at least once a day was considered regular. Attendance at group instructional and follow-up meetings was recorded.
INTERVENTIONS
The TM program was used as a mind-body intervention for its effects on physiological correlates of stress and related CVD outcomes because of its standardization, reproducibility and validity.23, 24, 39-41 It is the principal mind-body technique of Maharishi Ayurveda, a comprehensive traditional system of natural medicine.42, 43 The TM technique is described as a simple, natural, effortless procedure that is practiced 20 minutes twice a day while sitting comfortably with the eyes closed.40, 44, 45 During the practice, it is reported that ordinary thinking processes settle down, and a distinctive “wakeful hypometabolic” state characterized by neural coherence and physiological rest is gained.46-48 Standard teaching materials and format were used.40 The TM technique was taught in a 7-step course of instruction consisting of six 1.5–2 hour individual and group meetings taught by an instructor certified by Maharishi Foundation-USA.40 Thereafter, follow-up and maintenance meetings were held weekly for the first month, biweekly for the next two months, and monthly thereafter for the remainder of phases 1 and 2.
The control intervention was a cardiovascular health education program designed to match the format of the experimental intervention for instructional time, instructor attention, participant expectancy, social support, and other nonspecific factors.27, 49 The content was based on standard, published materials.50, 51 The instructors were professional health educators. The HE subjects were advised to spend at least 20 minutes a day at home practicing heart-healthy behaviors, e.g., exercise, healthy meal preparation and nonspecific relaxation. Care was taken to separate both intervention groups to minimize contact and communication.
STATISTICAL ANALYSIS
Baseline comparisons of group data for continuous variables were assessed with t tests for independent variables. Dichotomous variables were compared using Fisher’s exact test.
Survival curves were estimated by the Kaplan-Meier product limit method using time-to-first event. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using the Cox proportional hazard model. Event data from phases 1 and 2 for all subjects were included in the survival analyses with time to event censored at the end of the subjects’ follow-up. That is, subjects who enrolled in phase 1 were followed through completion of phase 1. Subjects who reconsented and re-enrolled in phase 2 were followed through completion of phase 2, including the interim/hiatus period. Mortality data were collected from public records for all subjects regardless of re-enrollment status and confirmed with death certificates.28, 29 Multivariate models covaried for the stratification factors of age, sex, and lipid-lowering medication status since this is recommended to improve the precision and power of the analyses 52, 53
The primary survival analysis comprised the study periods during which subjects were consented and enrolled (either phase 1 only or phase 1 through 2). Re-enrollment in phase 2 of the study was examined as an additional grouping factor in the analyses of baseline characteristics and as a time-dependent covariate in the survival analyses. The validity of the proportional hazards assumption was tested by assessing the joint significance of the re-enrollment variable, the treatment variable, and their interaction. A second, independent analysis of the survival data was conducted by Dr. Bruce Barton, Department of Quantitative Health Sciences, University of Massechusetts Medical School.
Changes in intermediate outcomes were analyzed using a repeated measures mixed model. Subject differences were modeled as random effects. Other independent variables were fixed effects. Time was modeled as a continuous linear trend. Baseline level of the outcome, age, sex, and lipid-lowering medication were covariates. The model was fit over all available data points by restricted maximum likelihood estimation.
All primary and secondary outcomes were analyzed using the intention-to-treat principle. Power calculations were based on the approach of Proschan and Hunsberger for conditional power. 54 The power calculation for phase 1 estimated that with 374 subjects, there was 80% power to detect a 36% risk reduction in the composite of cardiovascular mortality, nonfatal MI, nonfatal stroke, coronary artery bypass graft surgery (CABG), percutaneous coronary intervention, and hospitalizations for heart failure and ischemic heart disease (non MI). At the completion of phase 1, 201 subjects were recruited (Figure 1). With review and approval of the DSMB, a single interim analysis determined that with 201 subjects and an additional 6 years of follow up to accrue the required number of events, the trial had 80% power to detect a 50% risk reduction in the DSMB-approved endpoint of all-cause mortality, nonfatal MI and nonfatal stroke.
Figure 1.
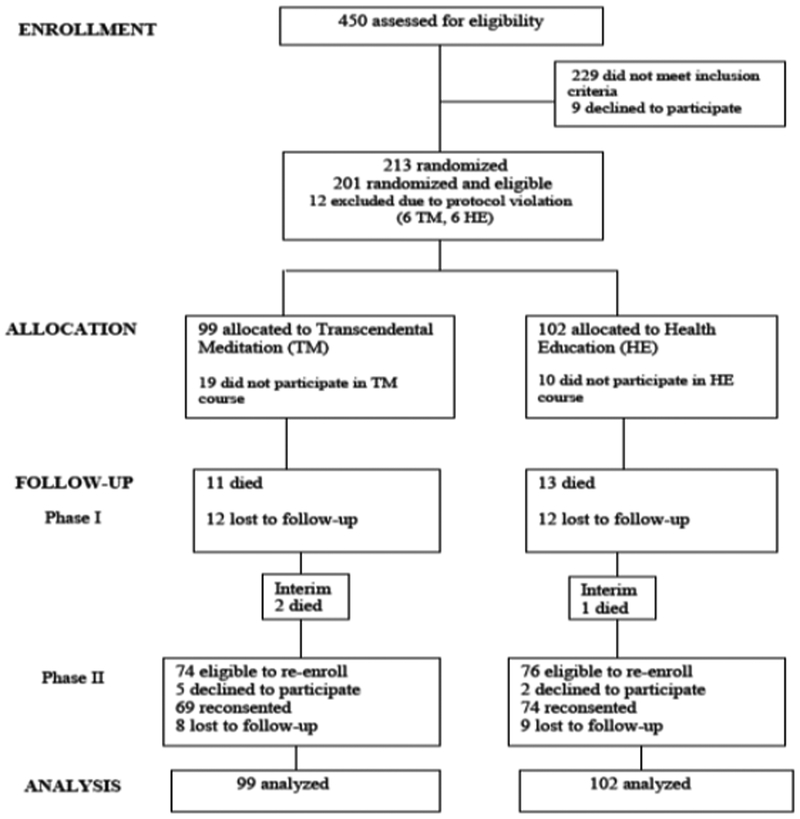
Participant Flow diagram
RESULTS
There were 201 participants who met eligibility criteria, provided informed consent, and were randomized to either TM (n = 99) or HE (n =102) in phase 1 (Figure 1). The rate of nonparticipation in the treatment groups was 19/99 or 19% in the TM group and 10/102 or 10% in the HE group, a nonsignificant difference (p=.07, Fishers’s exact test). At the beginning of phase 2, 143 subjects were re-enrolled in the second phase. Fifty-eight subjects from phase 1 did not participate in phase 2 because of death, attrition or lack of informed consent. Of these, 25 or nearly half, had primary outcome events during phase 1.
As shown in table 1, the groups were generally similar at baseline; 42% were women; mean age was 59 years; half of the participants reported incomes of less than $10,000/year. The only significant baseline differences were education level and CES-D score. No significant interactions were found on any of the baseline variables between treatment group and phase 2 re-enrollment.
Table 1.
Demographic and Baseline Characteristics by Treatment Groupa
| Characteristic | Mean (SD) | P Value | |
|---|---|---|---|
| TM (n = 99)a |
HE (n = 102)a |
||
| Female participants | 41.4 | 44.1 | .70 |
| Age, y | 59.9 (10.7) | 58.4 (10.5) | .30 |
| Lipid-lowering medication | 59.6 | 60.8 | .86 |
| ACE inhibitors | 43.4% | 45.1% | .81 |
| Angiotensin receptor agonists | 7.1% | 6.9% | .95 |
| Beta blockers | 2.0% | 2.0% | .98 |
| Calcium channel blockers | 34.3% | 36.3% | .77 |
| Diuretics | 43.4% | 46.1% | .71 |
| Aspirin | 41.4% | 31.4% | .14 |
| Married | 32.7 | 26.5 | .34 |
| Education, y | 11.3 (2.7) | 9.9 (3.6) | .003** |
| Household Income, $ | 16,979 (17,807) | 14,194 (15, 023) | .25 |
| Income below $10 000 | 48.5 | 47.1 | .84 |
| Weight, kg | 93.1 (19.4) | 92.6 (24.0) | .87 |
| BMI | 32.2 (6.8) | 32.7 (7.4) | .56 |
| Stenosed Arteries, No. | 1.8 (0.9) | 1.8 (0.9) | .91 |
| Systolic blood pressure, mm Hg | 133.0 (18.7) | 131.5 (18.0) | .57 |
| Diastolic blood pressure, mm Hg | 77.5 (12.3) | 76.8 (11.4) | .68 |
| Hypertensive (BP≥140/90 mm Hg) | 39.4 | 35.3 | .55 |
| Heart rate, bpm | 72.0 (10.1) | 72.2 (9.6) | .89 |
| Currently smoke | 38.4 | 43.1 | .49 |
| Consume alcohol | 30.3 | 28.4 | .77 |
| Use illicit drugs | 4.0 | 4.9 | .77 |
| Moderate or vigorous physical activity, hr/d | 4.4 (4.0) | 4.9 (4.0) | .41 |
| Anger expression | 26.0 (11.9) | 28.5 (11.3) | .14 |
| CMHI | 15.2 (5.1) | 15.9 (5.3) | .38 |
| CES-D | 18.2 | 30.7 | .04* |
| Treatment expectancy | 3.5 (0.9) | 3.7 (0.9) | .36 |
P-value column needs to be deleted and replaced by footnotes:
P<.05
P<.01
P<.001
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CES-D, Center for Epidemiological Studies Depression Scale35,36; CMHI, Cook-Medley Hostility Inventory composite score37,38; HE, health education control group; TM, Transcendental Meditation program.
For continuous variables, data are expressed as mean (SD) values; for dichotomous variables, data are expressed as percentage of patients.
Randomized subjects were observed for a maximum of 9.3 years and a mean of 5.4 ± 2.4 years (TM group = 5.3 ±2.3 years, HE group = 5.4 ± 2.5 years). There were 52 primary end point events. Of these, 20 events occurred in the TM group and 32 in the HE group (Table 2). Figure 2 shows the survival curves for the primary end point of mortality, MI and stroke. Table 3 presents the results of the survival analyses. In the primary analysis, the adjusted hazard ratio for the TM group compared to the HE group was 0.52 (95% CI,0.29–0.92) (P = .025). The stratification factors of age, gender, and lipid-lowering medications used as covariates were jointly significant as predictors of time to event (P=.0003. For the individual covariates: P = .0003, P = .057, and P = .03, respectively). The test for violation of the proportional hazards assumption was not significant.
Table 2.
Components of Primary and Secondary Clinical Event End points
| End Point | Number of Events | ||
|---|---|---|---|
| TM | HE | Both | |
| Primary end point a | |||
| All-cause mortality | 17 | 24 | 41 |
| Nonfatal MI | 1 | 4 | 5 |
| Nonfatal stroke | 2 | 4 | 6 |
| Total | 20 | 32 | 52 |
| Secondary end point a | |||
| CVD mortality | 4 | 5 | 9 |
| Nonfatal MI | 0 | 2 | 2 |
| Nonfatal stroke | 2 | 4 | 6 |
| Revascularization (CABG, PCI) | 17 | 15 | 32 |
| Hospitalization for CHD | 12 | 18 | 30 |
| Hospitalization for CHF | 9 | 10 | 19 |
| Total | 44 | 54 | 98 |
Abbreviations: CABG, coronary artery bypass graft surgery; CHD, coronary heart disease; CHF, congestive heart failure; CVD, cardiovascular disease; HE, health education control group; MI, myocardial infarction; PCI, percutaneous coronary intervention; TM, Transcendental Meditation program.
The counts of events refer to first events, and therefore the counts of primary and secondary events in each category may differ.
Figure 2.
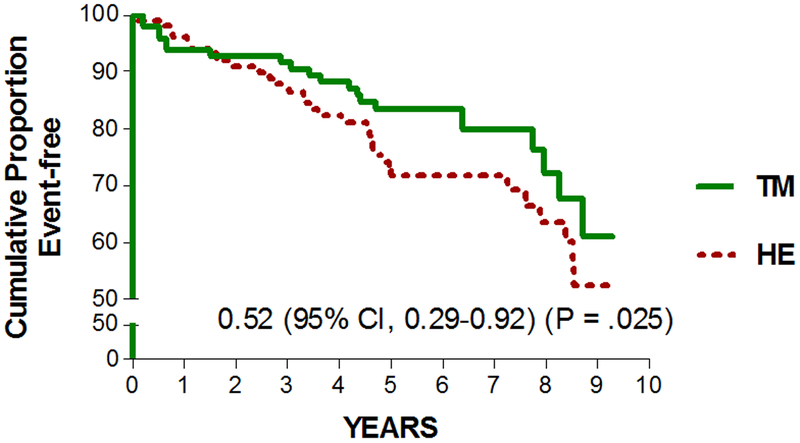
Kaplan-Meier survival curves of primary end point (all-cause mortality, non-fatal MI, or non-fatal stroke). HE indicates the health education intervention; TM the Transcendental Meditation program.
Table 3.
Results of Survival Analyses
| Hazard Ratio (95% CI) |
P-value | |
|---|---|---|
| Primary end point | ||
| Unadjusted | 0.64 (0.37-1.12) | 0.12 |
| Adjusted for stratification variables (age, gender, lipid lowering medications) – primary analysis | 0.52 (0.29-0.92) | 0.025 |
| Adjusted for stratification variables + education, baseline CESD | 0.54 (0.30-0.98) | 0.04 |
| Including events in non-reenrolled subjects during hiatus and phase 2, adjusted for stratification variables | 0.57 (0.34-0.96) | 0.03 |
| Secondary end point | ||
| Unadjusted | 0.77 (0.52-1.15) | 0.21 |
| Adjusted for stratification variables (age, gender, lipid lowering medications) | 0.76 (0.51-1.13) | 0.17 |
| Adjusted for stratification variables + education, baseline CESD | 0.82 (0.54-1.24) | 0.36 |
In secondary and sensitivity analyses, adjustment for baseline education and CES-D score in addition to the stratification factors showed a similar result (HR 0.54; 95% CI, 0.30–0.98) (P = .04). Eleven additional deaths occurred during the hiatus period and phase 2 in subjects whose enrollment terminated at the end of phase 1 (7 in TM group and 4 in HE group). Nonfatal events were not available for these subjects since their consent and enrollment had terminated although their fatal events were available from public records. 28, 29 Including these fatal events in non-reenrolled subjects, there were 27 primary end point events in the TM group and 36 in the HE group. The adjusted hazard ratio for the TM group compared to the HE group was 0.57 (95% CI, 0.34 to 0.96, P = .03).
There were 98 secondary end point events. Of these, 44 occurred in the TM group and 54 in the HE group (Table 2). As shown in Table 3, the adjusted hazard ratio for the TM group compared to the HE group was 0.76 (95% CI, 0.51–1.13) (P = .17). With additional adjustment for education and CES-D score, the hazard ratio was 0.82 (95% CI, 0.54–1.24) (P = .36).
Independent analysis of the primary and secondary survival data confirmed identical results (Dr. Bruce Barton, University of Massechusetts Medical School.)
Table 4 shows changes in the intermediate outcomes averaged during the trial. There was a significant net difference of −4.9 mm Hg in systolic BP in the TM group compared with HE group (95% CI, −8.3 to −1.5 mm Hg) (P = .01). For diastolic BP, there was a net difference of −1.6 mm Hg (95% CI, −3.4 to 0.3 mm Hg) (P = .27). There were no significant between group changes in BMI, physical activity, alcohol use, smoking or diet. There were significant improvements in anger-in, anger control, and total anger (P =.02, P =.02, and P =.03), respectively. There were no significant changes in anger-out, depression, or hostility for the TM vs HE groups. There were significant group by time interactions for anger-in (P = .002) and total anger (P = .01) although not for anger control or other intermediate outcomes.
Table 4.
Changes in Intermediate Outcomes During 5.4-Year Average Follow-up
| Outcome (TM/HE No.) |
TM Group Change, Mean (SE) |
HE Group Change, Mean (SE) |
Net Difference (TM–HE) |
P Value |
|---|---|---|---|---|
| Systolic BP, mm Hg (86/97) |
0.022 (1.264) | 4.883 (1.184) | −4.861 | .01 |
| Diastolic BP, mm Hg (86/97) |
−3.433 (0.683) | −1.877 (0.643) | −1.556 | .27 |
| HR, bpm (86/97) |
0.518 (0.541) | −0.145 (0.509) | 0.663 | .01 |
| BMI, wt/ht2 (86/97) |
−0.070 (0.274) | −0.144 (0.258) | 0.074 | .94 |
| Exercise, hr/d (81/88) |
0.454 (0.327) | 0.440 (0.316) | 0.014 | .13 |
| Alcohol, drinks/wk (80/90) |
−2.494 (0.424) | −3.109 (0.400) | 0.615 | .46 |
| Cigarettes, No./d (84/93) |
−0.637 (0.324) | −0.027 (0.309) | −0.610 | .16 |
| Anger-in (85/94) |
−1.826 (0.399) | −1.618 (0.378) | −0.209 | .02 |
| Anger-out (85/94) |
0.266 (0.338) | −0.156 (0.321) | 0.422 | .87 |
| Anger control (85/94) |
−0.267 (0.290) | −1.344 (0.277) | 1.077 | .02 |
| Total anger (85/94) |
−1.171 (0.750) | −0.531 (0.712) | −0.640 | .03 |
| Depression (85/93) |
−0.252 (0.713) | 0.686 (0.680) | −0.938 | .20 |
| Hostility (84/92) |
−0.703 (0.346) | −0.621 (0.330) | −0.082 | .53 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BP, blood pressure; HE, health education control group; HR, heart rate; TM, Transcendental Meditation program.
Experimental subjects practiced the TM technique an average of 8.5 times per week. Control subjects practiced healthy lifestyle activities an average of 8.6 times per week. Attendance at follow-up meetings averaged over 5.4 years was 48% for each group. There were no significant differences in home practice or meeting attendance for either group in phase 1 compared with phase 2.
In the high-adherence subgroup of subjects who were regular in home practice(n = 141), the hazard ratio was 0.34 [95% CI, 0.16–0.69]) (P = .003). The interaction between treatment and adherence (high vs. low) showed a statistical trend (P =.08). Cox regression analysis within the TM group indicated that frequency of home practice was inversely associated with primary clinical events (P = .04). On average, subjects attended 70% of all semiannual testing visits.
DISCUSSION
This randomized controlled trial on the secondary prevention of CVD in a high risk population extends previous trials reporting that mind-body intervention with the TM program reduced CVD risk factors, surrogate end points, and mortality.17-24, 39, 55, 56 In this trial, the TM program was associated with 48% risk reduction in the composite of mortality, nonfatal MI and nonfatal stroke in African American men and women with CHD over an average of 5.4 years follow-up. These results were confirmed by independent data analysis. Concurrently, there were improvements in BP and psychosocial distress factors, particularly anger. Regularity of TM practice was associated with increased survival.
The effects of active intervention appeared stable and reliable during the trial. The two treatment groups did not differ in characteristics between phases 1 and 2, indicating that there was no evidence of selective attrition. Adherence to the interventions was similar in both phases. Although there were between-group baseline differences on education and depression, adjusting for these differences did not substantially affect the primary outcome.
The average BP reduction of 5 mm Hg is similar to that found in meta-analyses of shorter-term trials of the TM progam.17, 18 Reduction in systolic BP may be one physiological mechanism for reduced clinical events in this trial since this magnitude of reduction has been associated with 15% reduction in cardiovascular clinical events.57 The improvements in anger expression and control may also have contributed to enhanced survival, since anger has been associated with CVD clinical events in CHD patients 10. There was a nonsignificant reduction in smoking in the TM group. It is possible that other mechanisms not evaluated in this study contributed to the reduced risk in the TM group. Previous studies have reported reductions in sympathetic nervous system tone, hypothalamic-pituitary-adrenal axis activation, insulin resistance, left ventricular mass, myocardial ischemia, carotid atherosclerosis and heart failure. 19-21, 58, 59,72 Central nervous system integration has been proposed as a neurophysiologic basis for these physiologic effects. 47, 60, 61
There was some evidence of a dose-response relationship between practice of the TM program and survival. There was a significant association between regularity of home practice and survival. Further, the subgroup of subjects who were regular in their TM practice had a 66% risk reduction compared with the overall sample risk reduction of 48%.
To our knowledge, this is the first randomized controlled trial to demonstrate a reduction in the risk for mortality, MI and stroke with the individual practice of a relatively simple mind-body intervention, particularly in a high-risk racial/ethnic population.62 Previous randomized trials of stress reduction methods in patients with CHD typically used group-based psychosocial counseling methods with complex multimodal interventions, lacked attention controls and resulted in heterogeneous outcomes. 62-67 This is also the first prospectively designed and conducted randomized controlled trial to evaluate effects on CVD clinical events of a nonpharmacologic, lifestyle modification approach for hypertension. 68
There were limitations to this study. The sample size did not allow for sufficiently powered analyses of single clinical end points. The 24% risk reduction in the secondary composite end point of CVD mortality, MI, stroke, coronary revascularization and CVD hospitalization did not reach statistical significance (P = .17). This may have been related to variability in the utilization of revascularization procedures and hospitalizations in the community. The reduction in depression in the meditation group was not significant, perhaps because depression was already low in this group at baseline. Hostility scores were relatively low in both groups at baseline. There were no significant differences between groups in change in BMI, exercise or alcohol consumption, although in both study groups there were apparent (within group) improvements in exercise and alcohol consumption. As noted above, there was a nonsignificant reduction in cigarette smoking in the stress reduction group. The sample was limited to a single racial/ethnic sample. However, previous studies have reported improvements in CVD outcomes with the TM program in general population samples, suggesting that this finding is generalizable.17-20, 39
Another limitation was the variable length of time of subject participation and the heterogeneity of outcome data for subjects who did not re-enroll in phase 2. However, when all available data, i.e., mortality from non-reenrolling subjects was in included in a sensitivity analysis of the primary end point, the results were similar to the main analysis in treatment effect and significance level. The unadjusted results of the primary end point analysis showed a nonsiginficant statistical trend (P =.12), However, the hazard ratio adjusted for covariates of age, gender and antihypertensive medications was significant (P=.025). According to Pocock et al and CONSORT recommendations, adjusted analyses frequently improve the precision of the estimate of the treatment effect 52, 69. Furthermore, since these factors were used in the stratified randomization procedure, it is recommended to adjust for stratification factors to achieve the most efficient treatment comparison 52, 53. This is particularly relevant when the adjustment factors predict the outcome, as they did in this trial 52.
The proportion of cardiovascular deaths in the present trial was lower than national averages.1 This may have been due to the relatively small sample size or method of collecting causes of death from death certificates. The accuracy of death certificate data for cause of death has been seriously questioned 70, 71. There was a nonsignificantly higher non-participation rate in the TM group compared to HE controls. Because the analysis was based on intention-to-treat, the higher non-participation rate in the TM group may have led to a more conservative estimate of the treatment effect.
This trial did not address the effects other mind-body, meditation-type interventions on clinical events. While several meta-analyses and comparative studies suggest a distinctive effect of the TM program,18, 48, 73 it remains for future comparative effectiveness trials to address differential effects of mind-body interventions on CVD clinical events.
In conclusion, this randomized controlled trial found that a selected mind-body, stress reduction intervention, the Transcendental Meditation program, significantly reduced risk for mortality, MI and stroke in African American men and women with CHD. These changes were associated with lower BP and psychosocial distress. Thus, the TM program may be a clinically useful behavioral intervention in the secondary prevention of CVD in this and perhaps other high-risk populations.
What is known
Psychosocial stress is associated with the onset and progression of cardiovascular disease in African Americans and the general population
Stress reduction with the Transcendental Meditation program has previously been shown to reduce cardiovascular risk factors e.g., hypertension, psychological stress, smoking, insulin resistance and myocardial ischemia.
What this article adds
This randomized controlled trial found that adding stress-reducing Transcendental Meditation to usual care in patients with coronary heart disease resulted in a 48% reduction in the risk for cardiovascular clinical events, i.e., mortality, myocardial infarction and stroke over more than five years of follow up.
Potential mechanisms for the observed outcomes differences included lower blood pressure and anger scores. There was evidence for dose-response effect between regularity of meditation practice and longer survival.
A transcendental meditation program may be useful in the secondary prevention of cardiovascular disease.
ACKNOWLEDGEMENTS
The authors are grateful to Linda Piller, MD, MPH, University to Texas Health Science Center-Houston for adjudication of clinical end points and to James Ware, PhD, Harvard School of Public Health for review of the statistical methods. William Sheppard, PhD, Jing Li, MD, Ahmed Dalmar, MD, Janice Peete, Laura Valls, Jean Symington Craig, MS, Laura Alcorn, Diane Prather-Huff, OD, MPH, Ragnhild Boes, PhD, Julie Stephens, PhD, Linda Heaton, Marilyn Ungaro and Carol Jarvis provided administrative and technical support. Andrea LaFave and Gina Orange taught the Transcendental Meditation program. Preliminary findings from this study were presented at the American Heart Association Annual Meeting, Orlando, FL, 2009 (Circulation. 2009;120:S461).
Funding: This study was funded by grant # RO1HL48107 from the National Institutes of Health-National Heart, Lung and Blood Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no relevant financial disclosures.
REFERENCES
- 1.American Heart Association, Roger V, Go A, Lloyd-Jones D Heart disease and stroke statistics−-2012 update: a report from the American Heart Association Circulation. 2012;125:e2–e220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mackay J, Mensah GA, Mendis S, Greenlund K. The Atlas of Heart Disease and Stroke, 2004, World Health Statistics. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 3.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241 [DOI] [PubMed] [Google Scholar]
- 4.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51:1237–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651 [DOI] [PubMed] [Google Scholar]
- 6.Brotman D, Golden S, Wittstein I. The cardiovascular toll of stress. Lancet. 2007;370:1089–1100 [DOI] [PubMed] [Google Scholar]
- 7.Bairey-Merz NC, Dwyer J, Nordstrom CK, Walton KG, Salerno JW, Schneider RH. Psychosocial stress and cardiovascular disease: Pathophysiological links. Behav Med. 2002;27:141–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952 [DOI] [PubMed] [Google Scholar]
- 9.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–813 [DOI] [PubMed] [Google Scholar]
- 10.Chida Y, Steptoe A. The association of anger, hostility with future coronary heart disease: meta-analytic review of prospective evidence. J Am Coll Cardiol. 2009;53:936–946 [DOI] [PubMed] [Google Scholar]
- 11.Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol. 2010;56:38–46 [DOI] [PubMed] [Google Scholar]
- 12.Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325:315–331 [DOI] [PubMed] [Google Scholar]
- 13.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A bio-psychosocial model. American Psychologist. 1999;54:805–816 [DOI] [PubMed] [Google Scholar]
- 14.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. Am J Epidemiol.. 2008;167:624–632 [DOI] [PubMed] [Google Scholar]
- 15.Whitfield K, Weidner G, Clark R, Anderson N. Sociodemographic diversity and behavioral medicine. J Consult Clin Psychol. 2002;70:463–481 [DOI] [PubMed] [Google Scholar]
- 16.Barnes VA, Schneider RH, Alexander CN, Staggers F. Stress, stress reduction and hypertension in African Americans: An updated review. J Natl Med Assoc. 1997;89:464–476 [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson J, Liu C, Kryscio R. Blood Pressure Response to Transcendental Meditation: a meta-analysis. Am J Hypertens. 2008;21:310–316 [DOI] [PubMed] [Google Scholar]
- 18.Rainforth M, Schneider R, Nidich S, King C, Salerno J, Anderson J. Stress Reduction Programs in Patients with Elevated Blood Pressure: A Systematic Review and Meta-analysis. Curr Hypertens Rep. 2007;9:520–528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paul-Labrador M, Polk D, Dwyer J, Velasquez I, Nidich S, Rainforth M, Schneider R, Bairey Merz C. Effects of a randomized controlled trial of Transcendental Meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med. 2006;166:1218–1224 [DOI] [PubMed] [Google Scholar]
- 20.Zamarra JW, Schneider RH, Besseghini I, Robinson DK, Salerno JW. Usefulness of the Transcendental Meditation program in the treatment of patients with coronary artery disease. Am J Cardiol. 1996;78:77–80 [DOI] [PubMed] [Google Scholar]
- 21.Castillo-Richmond A, Schneider R, Alexander C, Cook R, Myers H, Nidich S, Haney C, Rainforth M, Salerno J. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31:568–573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schneider RH, Alexander CN, Staggers F, Rainforth M, Salerno JW, Hartz A, Arndt S, Barnes V, Nidich S. Long-term effects of stress reduction on mortality in persons > 55 years of age with systemic hypertension. Am J Cardiol. 2005;95:1060–1064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walton K, Schneider R, Nidich S. Review of controlled research on the Transcendental Meditation program and cardiovascular disease - risk factors, morbidity and mortality. Cardiol Rev. 2004;12:262–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orme-Johnson DW, Barnes VA, Schneider R. Transcendental Meditation for primary and secondary prevention of coronary heart disease In: Allan R, Fisher J, eds. Heart & Mind: the Practice of Cardiac Psychology, second edition. Washington, DC: American Psychological Association; 2012:365–379. [Google Scholar]
- 25.D’Agostino RB Sr., Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753 [DOI] [PubMed] [Google Scholar]
- 26.National Cholesterol Education Program. Classification, Prevalence, Detection, Evaluation Second Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Washington, D.C.: National Institutes of Health National Heart, Lung, and Blood Institute; 1993:I-1–1-21. [Google Scholar]
- 27.Powell L, Calvin J, Mendes de Leon C, Richardson D, Grady K, Flynn K, Rucker-Whitaker C, Janssen I, Kravitz G, Eaton C. Heart Failure Adherence and Retention Trial Investigators. The Heart Failure Adherence and Retention Trial (HART): design and rationale. Am Heart J. 2008;156:452–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edlavitch SA, Baxter J. Comparability of mortality follow-up before and after the National Death Index. Am J Epidemiol. 1988;127:1164–1178 [DOI] [PubMed] [Google Scholar]
- 29.Stampfer MJ, Willett WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, Hennekens CH. Test of the National Death Index. Am J Epidemiol. 1984;119:837–839 [DOI] [PubMed] [Google Scholar]
- 30.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major Outcomes in High-Risk Hypertensive Patients Randomized to Angiotensin-Converting Enzyme Inhibitor or Calcium Channel Blocker vs. Diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–2997 [DOI] [PubMed] [Google Scholar]
- 31.Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G. Validity and reliability of the Block 98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9:84–93 [DOI] [PubMed] [Google Scholar]
- 32.Elmer PJ, Grimm R Jr., Laing B, Grandits G, Svendsen K, Van Heel N, Betz E, Raines J, Link M, Stamler J, et al. Lifestyle intervention: results of the Treatment of Mild Hypertension Study (TOMHS). Prev Med. 1995;24:378–388 [DOI] [PubMed] [Google Scholar]
- 33.Folsom AR, Caspersen CJ, Taylor HL, Jacobs DR Jr., Luepker RV, Gomez-Marin O, Gillum RF, Blackburn H Leisure time physical activity and its relationship to coronary risk factors in a population-based sample. The Minnesota Heart Survey. Am J Epidemiol. 1985;121:570–579. [DOI] [PubMed] [Google Scholar]
- 34.Radloff L The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;3:385–401 [Google Scholar]
- 35.Long Foley K, Reed PS, Mutran EJ, DeVellis RF Measurement adequacy of the CES-D among a sample of older African Americans. Psychiatry Res. 2002;109:61–69 [DOI] [PubMed] [Google Scholar]
- 36.Barefoot J, Dodge K, Peterson B. The Cook-Medley Hostility Scale: Item content and ability to predict survival. Psychosom Med. 1989;51:46–57 [DOI] [PubMed] [Google Scholar]
- 37.Nabi H, Singh-Manoux A, Ferrie JE, Marmot MG, Melchior M, Kivimaki M. Hostility and depressive mood: results from the Whitehall II prospective cohort study. Psychol Med. 2010;40:405–413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spielberger C, Sydeman S, Owen A, Marsh B. Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI) In: Maruish M, ed. The use of psychological testing for treatment planning and outcomes assessment. Mahwah, NJ: Lawrence Erlbaum Associates; 1999:1507. [Google Scholar]
- 39.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental Meditation, mindfulness, and longevity: an experimental study with the elderly. J Pers Soc Psychol. 1989;57:950–964 [DOI] [PubMed] [Google Scholar]
- 40.Roth R Maharishi Mahesh Yogi’s Transcendental Meditation. Washington, DC: Primus; 2002. [Google Scholar]
- 41.Walton K, Schneider R, Salerno J, Nidich S. Psychosocial Stress and Cardiovascular Disease 3: Cost Studies and Policy Implications of the Transcendental Meditation Program. Behav Med. 2005;30:173–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schneider RH, Alexander CN, Salerno J, Robinson D, Fields J, Nidich S. Disease prevention and health promotion in the aging with a traditional system of natural medicine: Maharishi Vedic Medicine. J Aging Health. 2002;14:57–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharma H, Clark C. Ayurvedic Healing: Contemporary Maharishi Ayurveda Medicine and Science. London, UK: Singing Dragon Publications, 2012 [Google Scholar]
- 44.Rosenthal N Transcendence: Healing and Transformation Through Transcendental Meditation. NYC, New York: Penguin-Tarcher; 2011. [Google Scholar]
- 45.Travis F Transcendental Meditation technique In: Craighead W, Nemeroff C, eds. The Corsini Encyclopedia of Psychology and Behavioral Science. New York: John Wiley and Sons; 2001:1705–1706. [Google Scholar]
- 46.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: A review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424 [DOI] [PubMed] [Google Scholar]
- 47.Travis F, Shear J. Focused attention, open monitoring and automatic self-transcending: Categories to organize meditations from Vedic, Buddhist and Chinese traditions. Conscious Cogn. 2010;19:1110–1118 [DOI] [PubMed] [Google Scholar]
- 48.Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, Bairey-Merz CN. Psychosocial stress and cardiovascular disease 2: Effectiveness of the Transcendental Meditation technique in treatment and prevention. Behav Med. 2002;28:106–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Windsor R, Baranowski T, Clark N, Cutter G. Evaluation of health promotion, health education and disease prevention programs. Mountainview, CA: Mayfield Publishing Co.; 1994. [Google Scholar]
- 50.Chobanian A, Bakris G, Black H, National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 51.Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, and treatment of high blood cholesterol in adults (Adult Treatment Panel III),. Final Report. Circulation. 2002;106:3143–3421 [PubMed] [Google Scholar]
- 52.Pocock S, Assman S, Enos L, Kasten L. Subgroup analysis, covariate adjustment and baseline comparisions in clinical trial reporting: current practice and problems. Statistics in Medicine. 2002;21:2917–2930 [DOI] [PubMed] [Google Scholar]
- 53.Committee for Proprietary Medicinal Products. Points to consider on adjustment for baseline covariates, The European Agency for the Evaluation of Medicinal Products. 2003:London, 2863/2899 [Google Scholar]
- 54.Proschan MA, Hunsberger SA. Designed extensions of studies based on conditional power. Biometrics 1995;51:1315–3124 [PubMed] [Google Scholar]
- 55.Alexander CN, Schneider R, Staggers F, Sheppard W, Clayborne M, Rainforth M, Salerno J, Kondwani K, Smith S, Walton K, Egan B. A trial of stress reduction for hypertension in older African Americans (Part II): Sex and risk factor subgroup analysis. Hypertension. 1996;28:228–237 [DOI] [PubMed] [Google Scholar]
- 56.Schneider R, Alexander C, Staggers F, Orme-Johnson D, Rainforth M, Salerno J, Sheppard W, Castillo-Richmond A, Barnes V, Nidich S. A randomized controlled trial of stress reduction in the treatment of hypertension in African Americans during one year. Am J Hypertens. 2005;18:88–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Law M, Morris J, Wald N. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mills PJ, Schneider RH, Hill D, Walton KG, Wallace RK. Beta-adrenergic receptor sensitivity in subjects practicing transcendental meditation. J Psychosom Res. 1990;34:29–33 [DOI] [PubMed] [Google Scholar]
- 59.Barnes VA, Kapuku GK, Treiber FA. Impact of Transcendental Meditation on left ventricular mass in African American adolescents. Evid Based Complement Alternat Med. 2012;2012:923153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Travis F, Wallace RK. Autonomic and EEG patterns during eyes-closed rest and transcendental meditation (TM) practice: the basis for a neural model of TM practice. Conscious Cogn. 1999;8:302–318. [DOI] [PubMed] [Google Scholar]
- 61.Travis F, Haaga DA, Hagelin J, Tanner M, Nidich S, Gaylord-King C, Grosswald S, Rainforth M, Schneider RH. Effects of Transcendental Meditation practice on brain functioning and stress reactivity in college students. Int J Psychophysiol. 2009;71:170–176 [DOI] [PubMed] [Google Scholar]
- 62.Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol. 2009;169:1158–1165 [DOI] [PubMed] [Google Scholar]
- 63.Friedman M, Thoresen C, Gill J, Ulmer D, Powell L, Price V, Brown B, Thompson L, Rabin D, Breall W, Bourg E, Levy R, Dixon T. Alteration of the Type A behaviour and reduction in cardiac recurrences in postmyocardial infarction patients: Summary results of the Reccurrent Coronary Prevention Project. Amer Heart J. 1986;112:653–665 [DOI] [PubMed] [Google Scholar]
- 64.Jones D, West R. Psychological rehabilitation after myocardial infarction: multicentre randomised controlled trial. BMJ. 1996;313:1517–1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Writing Committee for the ENRICHD investigators. Effects of treating depression and low level social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease (ENRICHD) patients randomized trial. JAMA. 2003;289:3106–3116 [DOI] [PubMed] [Google Scholar]
- 66.Gulliksson M, Burell G, Vessby B, Lundin L, Toss H, Svardsudd K. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease. Arch Intern Med. 2011;171:134–140 [DOI] [PubMed] [Google Scholar]
- 67.Orth-Gomer K, Schneiderman N, Wang HX, Walldin C, Blom M, Jernberg T. Stress reduction prolongs life in women with coronary disease: the Stockholm Women’s Intervention Trial for Coronary Heart Disease (SWITCHD). Circ Cardiovasc Qual Outcomes. 2009;2:25–32 [DOI] [PubMed] [Google Scholar]
- 68.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007;334:885–888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Keech A, Gebski V and Pike Rhana, eds. Interpreting and reporting clinical trials: a guide to the CONSORT statement and the principles of randomized controlled trials, 2007. Australasian Medical Publishing Co, Sydney, Australia, p. 27 [Google Scholar]
- 70.Smith Sehdev AE, Hutchins GM. Problems with proper completion and accuracy of the cause-of-death statement. Arch Intern Med. 2001;161:277–284 [DOI] [PubMed] [Google Scholar]
- 71.Ravakhah K Death certificates are not reliable: revivification of the autopsy. South Med J. 2006;99:728–733 [DOI] [PubMed] [Google Scholar]
- 72.Jayadevappa R, Johnson J, Bloom B, Nidich S, Desai S, Chhatre S, Raziano D, Schneider R. Effectiveness of Transcendental Meditation on Functional Capacity and Quality of Life of African Americans with Congestive Heart Failure: A Randomized Control Study. Ethnicity and Disease. 2007;17:72–77 [PMC free article] [PubMed] [Google Scholar]
- 73.Orme-Johnson D, Walton K. All approaches to preventing or reversing effects of stress are not the same. Am J Health Promot. 1998;12:297–299 [DOI] [PubMed] [Google Scholar]


