Abstract
Introduction:
New paediatric cardiology trainees are required to rapidly assimilate knowledge and gain clinical skills to which they have limited or no exposure during residency. The Pediatric Cardiology Fellowship Boot Camp (PCBC) at Boston Children’s Hospital was designed to provide incoming fellows with an intensive exposure to congenital cardiac pathology and a broad overview of major areas of paediatric cardiology practice.
Methods:
The PCBC curriculum was designed by core faculty in cardiac pathology, echocardiography, electrophysiology, interventional cardiology, exercise physiology, and cardiac intensive care. Individual faculty contributed learning objectives, which were refined by fellowship directors and used to build a programme of didactics, hands-on/simulation-based activities, and self-guided learning opportunities.
Results:
A total of 16 incoming fellows participated in the 4-week boot camp, with no concurrent clinical responsibilities, over 2 years. On the basis of pre- and post-PCBC surveys, 80% of trainees strongly agreed that they felt more prepared for clinical responsibilities, and a similar percentage felt that PCBC should be offered to future incoming fellows. Fellows showed significant increase in their confidence in all specific knowledge and skills related to the learning objectives. Fellows rated hands-on learning experiences and simulation-based exercises most highly.
Conclusions:
We describe a novel 4-week-long boot camp designed to expose incoming paediatric cardiology fellows to the broad spectrum of knowledge and skills required for the practice of paediatric cardiology. The experience increased trainee confidence and sense of preparedness to begin fellowship-related responsibilities. Given that highly interactive activities were rated most highly, boot camps in paediatric cardiology should strongly emphasise these elements.
Keywords: Fellowship training, boot camp, medical education, simulation, paediatric cardiology
THE PRACTICE OF PAEDIATRIC CARDIOLOGY REQUIRES a unique knowledge base as well as procedural and diagnostic skills to which paediatric residents traditionally have limited exposure during residency training. In particular, most paediatric residents have little or no hands-on exposure to echocardiography, invasive/interventional cardiology, and electrophysiology. Similarly, exposure to complex cardiac pathology and pathophysiology is typically limited; yet, entering fellows are often expected to rapidly integrate into these highly technical clinical environments caring for patients with complex anatomy and physiology despite little formal training. In the era of work-hour restrictions, acquisition of core skills may be delayed when introduction of these concepts relies on “time and chance” exposure in the clinical environment. Other highly technical fields such as paediatric critical care medicine as well as general, orthopaedic, otolaryngology, and cardiothoracic surgery have utilised dedicated instructional time early in training, so-called “boot camps”, to rapidly introduce key knowledge and skills in order that trainees can become rapidly functional and safe in the clinical setting.1–6 A meta-analysis of such boot camps has shown that these programmes lead to significant improvements in clinical skills, knowledge, and confidence.7 Some of the objectives of these boot camps include introduction of core clinical content, acquisition of fundamental procedural skills, orientation to hospital policy and procedure, and team building. Such dedicated instructional time has also been advocated as a way to mitigate the “July effect”, a decrease in efficiency and increase in morbidity and mortality seen in some hospital settings at the onset of the academic year.8,9 Historically, fellows at the Boston Children’s Hospital Pediatric Cardiology Fellowship Program are introduced to subspecialty areas of cardiology on a rotation basis, such that some fellows may not have significant intensive exposure to some areas until the second half of the first year of fellowship. Orientation has been previously limited to introduction to hospital computing systems, brief welcome lectures from faculty representatives from each of the major divisions of paediatric cardiology, and introduction of standardised hospital infection control practices, and has been characterised by a paucity of both clinical instructional time and hands-on activities.
The Pediatric Cardiology Fellowship Boot Camp (PCBC) project was conceived following a comprehensive fellowship programme evaluation in order to address perceived weaknesses in orientation, didactic curriculum, and changes in educational processes related to the implementation of work-hour restrictions. The objectives of boot camp were as follows: to provide a comprehensive overview of congenital cardiovascular pathology early in the fellowship experience that would form the foundation for the integration of complex pathophysiological principles during patient care experiences; introduce key procedural skills in a simulation environment free of risk to patients; ensure a uniform introduction to key clinical topics in paediatric cardiology for fellows coming from residency training backgrounds with varied exposure to paediatric cardiology, “levelling the playing field”; reduce the programmatic burden of orienting fellows to a new clinical or procedural environment – that is, catheterisation laboratory, inpatient ward, cardiac ICU – on a repeated basis; introduce fellows to the flow of patients and providers through the programme, including the role of fellows in this flow; and foster team building.
Methods
All entering paediatric cardiology fellows participated in a 4-week-long “boot camp” experience designed to introduce key knowledge, skills, and attitudes related to the practice of paediatric cardiology across the inpatient, diagnostic, and procedural settings. The work of Kolb describes different ways in which adult learners interact with new knowledge. Learners may acquire knowledge through concrete – for example, lecture – or abstract – for example, experiential – processes, and process this new knowledge either through reflection or through active experimentation; therefore, four styles of adult learners are described on the basis of which of these mechanisms they use to acquire and process new knowledge.10 Optimal adult learning experiences incorporate strategies that appeal to all styles of adult learners.10,11 On the basis of these fundamental principles of adult learning theory, the PCBC elements included didactic sessions, hands-on, mentored interactive sessions such as simulation and table-top electrophysiology exercises, self-directed learning exercises such as creation of catheterisation and exercise physiology reports from raw data, and group problem-based exercises such as ECG reading. The PCBC experience introduced fellows to five major areas of paediatric cardiology including echocardiography, electrophysiology, cardiac catheterisation, exercise testing, and cardiac intensive care. The boot camp experience was anchored by a comprehensive series of small-group interactive sessions on congenital and paediatric cardiac pathology that reviewed all major cardiac lesions (Table 1). Pathology sessions included didactic descriptions of congenital cardiac pathology and hands-on exploration of preserved heart specimens from the extensive collection at Boston Children’s Hospital Cardiac Registry. The experience emphasised early acquisition of basic skills that would enhance their ability to function in the various paediatric cardiology clinical environments.
Table 1.
Cardiac pathology lecture series topics.
| Normal cardiac anatomy and nomenclature |
|---|
| Cardiac development |
| Veins |
| Systemic venous anomalies |
| Pulmonary venous anomalies |
| Atria |
| Communications |
| Appendages |
| AV canal |
| AV canal defects |
| AV valve atresia |
| AV valve stenosis/regurgitation |
| Straddling AV valve |
| Ventricles |
| Septal defects |
| Double/common inlet |
| Hypoplasia |
| Cavity obstruction |
| Conotruncus |
| Semilunar valve abnormalities (AS, PS, bicuspid Ao valve) |
| Abnormal ventriculo-arterial alignment/connection (TGA,DOV, other) |
| Abnormal outflow division (TOF, TA, IAA) |
| Great arteries |
| Ao obstruction (coarctation, IAA) |
| Pulmonary artery obstruction |
| Abnormal AP connections (hemitruncus, AP window,PDA) |
| Vascular ring |
| Coronary artery anomalies |
| Origin from pulmonary trunk |
| Abnormal origin from aorta |
| Variants associated with other CHD |
| Heterotaxy syndrome |
| Asplenia |
| Polysplenia |
| Endocardium, myocardium, pericardium |
| Endocardial fibroelastosis |
| Infective endocarditis |
| Myocarditis |
| Cardiomyopathy |
| Absent pericardium |
| Pericarditis |
Ao=aortic; AP=aortopulmonary; AS =aortic stenosis; AV=atrioventricular; DOV=double-outlet ventricle; IAA=interrupted aortic arch; PDA=patent ductus arteriosus; PS = pulmonary stenosis; TA=truncus arteriosus; TGA=transposition of the great arteries; TOF=tetralogy of Fallot
To guide boot camp design, core faculty from each of the five areas mentioned above were asked to create a set of specific learning objectives for new trainees related to their area of expertise. Learning objectives were reviewed and modified for appropriateness for level of trainees by the Fellowship Program Directors (D.W.B., C.K.A.). Small-group didactic, hands-on interactive, or self-guided learning opportunities were then created to address each of these learning objectives (Table 2). A learning passport was created on the basis of these learning objectives that allowed fellows to track completion of activities during the 4-week period (Table 3). Fellowship directors reviewed the passports at the conclusion of the PCBC. The didactic sessions covering the core paediatric cardiology curriculum as well as skills-based simulation sessions were all taught by experienced paediatric cardiology faculty. Orientation sessions aimed at introducing fellows to the “nuts and bolts” of daily responsibilities of paediatric cardiology fellowship – for example, how to prepare for a catheterisation case and how to write a catheterisation report – were taught by third-year paediatric cardiology fellows.
Table 2.
Pediatric Cardiology Fellowship Boot Camp curriculum.
| Didactics | Hands-on | Self-directed learning | |
|---|---|---|---|
| Echocardiography | • Segmental anatomy | • Faculty-guided echo simulation - obtaining the basic echo views | • Practice on echo simulator |
| • Basic ultrasound physics | |||
| • Normal echo views, basic machine functionality | |||
| • Emergency echocardiography | |||
| • Evaluation of ventricular function | |||
| Electrophysiology | • Basic ECG interpretation | • Use of temporary epicardial pacemakers | • ECG interpretation - teaching cases |
| • Approach to supraventricular tachycardias | • Interpretation of Holter monitors | ||
| Cardiac catheterisation | • Introduction to haemodynamic tracings | • Use of basic catheterisation equipment | • Case preparation and haemodynamic interpretation for an actual case |
| • Introduction to haemodynamic calculations | • Setting up for a catheterisation | ||
| • Introduction to angiography | |||
| Cardiac intensive care | • Cardiopulmonary interactions | • Airway management simulation | • Observe OR to ICU hand-off |
| • Central venous access simulation | |||
| • Haemodynamic monitoring | • Crisis resource management simulation | ||
| • Single-ventricle physiology | • PALS | ||
| • Bidirectional Glenn and Fontan physiology | |||
| Exercise physiology | • Basics of exercise physiology | • Observe exercise test | • Write-up exercise test |
| • Interpretation of exercise testing | |||
Activities included didactics, hands-on, mentored activities, and self-directed learning exercises in five major clinical areas to capture all types of adult learners
Table 3.
Learning Passport is used to guide and document fellow’s activities during PCBC.
| LEARNING OBJECTIVES | CHECKLIST |
| ELECTROPHYSIOLOGY | |
| • Establish organised approach to ECG analysis | □ ECG packet |
| • Analyse/write a report for a normal 24-hour Holter monitor | □ Read 25 ECGs in EKG reader |
| • Understand basic pacemaker timing cycles; be able to programme a bedside pacemaker | □ Read 5 Holters |
| □ Perform EP consents for | |
| • Provide differential diagnosis for narrow and wide complex arrhythmia | □ SVT ablation |
| □ Pacemaker/ICD procedure | |
| • Consent a patient for a standard EP study and ablation, understanding the risk and benefits for performing the procedure | □ Set up temporary pacemaker for: |
| □ AAI, VVI, and DDD pacing | |
| • Consent a patient for a pacemaker or defibrillator procedure, understanding the risks and benefits of performing the procedure | □ Perform capture threshold |
| □ Perform sensing threshold | |
| • Use and review the 8E/8S telemetry machines | □ Observe one SVT ablation |
| ECHOCARDIOGRAPHY | |
| • Understand basic ultrasound physics: transducer technology, imaging physics, spectral and color Doppler, Nyquist limit, and the importance of frame rate to imaging | □ Participate in normal anatomy review/intro to simulator |
| □ Complete 3 hours independent work on simulator | |
| □ Read intro chapters on ventricular function and basic echo (to be handed out at first lecture) | |
| • Understand the concepts of systolic and diastolic function and the difference between them | □ Demonstrate full cardiac sweeps from all 4 standard imaging windows |
| • Recognise basic ultrasound views | |
| • Understand how to use the modified Bernoulli’s equation during Doppler evaluation to estimate intracardiac gradients | Demonstrate recognition of basic normal anatomy |
| □ Demonstrate calculation of gradients from Doppler velocity measurements | |
| • Understand the environmental factors that affect echocardiographic and MRI effectiveness | |
| CARDIAC ICU | |
| • Describe factors that influence systemic perfusion in infants with single-ventricle physiology | □ Demonstrate aseptic technique, identification of appropriate landmarks, and use of Seldinger technique during central line placement |
| • Describe the relationship between pulmonary and cardiovascular function under normal conditions | □ Demonstrate effective bag mask ventilation |
| • Describe how pathological cardiovascular and pulmonary states alter cardiopulmonary interactions | □ Demonstrate correct size and placement of oral airway |
| • Explain the effects of positive and negative pressure ventilation on cardiovascular physiology | □ Discuss haemodynamic considerations during intubation of patient with myocardial dysfunction |
| □ Participate in 3 CRM scenarios and debriefing | |
| • Describe common modes of routine bedside monitoring in the cardiac ICU | □ Demonstrate use of CRM principles |
| EXERCISE PHYSIOLOGY | |
| • Understand different modalities used in exercise lab, including advantages and disadvantages, when to use | □ Attend 2 exercise tests |
| □ Interpret and write up 2 exercise tests, including reviewing findings with faculty member | |
| • Interpret exercise test, including understanding factors that limit patient’s exercise capacity | |
| • Understand how a patient’s exercise performance compares with normal subjects and those with similar diagnosis | |
| CATHETERISATION | |
| • Understand normal intracardiac pressures and identify normal pressure tracings | □ Observe 1 cath consent |
| □ Perform 1 supervised cath consent | |
| • Recognise normal saturation data and where obtained | □ Second scrub on 2 cath cases |
| • Understand the relevant variables and be able to calculate basic catheterisation-derived indices (cardiac index, Qp:Qs, systemic and pulmonary vascular resistance) | □ Co-write report on 1 cath |
| Participate in patient sign-out/transfer to 8E/8S on 1 cath | |
| □ Observe 2 equipment set-ups | |
| • Recognise normal angiograms of the cardiac chambers and thoracic vasculature | □ Perform 1 equipment set-up |
| □ Demonstrate ability to move cameras | |
| • Identify the common equipment used in a paediatric catheterisation | □ Round on 1 post-cath patient before discharge |
| □ Interpret assigned unknown case and write preliminary report |
Fellows completed pre- and post-PCBC surveys distributed via SurveyMonkey. Survey questions addressed the perceived level of confidence to engage in clinical activities related to the PCBC learning objectives across five clinical domains – echocardiography, electrophysiology, interventional cardiology, exercise physiology, and cardiac intensive care – and included general questions related to the overall utility of the PCBC. Confidence was reported on a scale from 1 (“not all confident”) to 9 (“extremely confident”). Survey results were utilised to calculate a composite “confidence score” in each clinical domain by adding points for each question in a given clinical domain, out of nine possible points, divided by total possible points in that domain, 9× the number of questions in that domain. Open-ended questions were utilised to gain more specific feedback on the overall boot camp experience. Qualitative analysis was used to analyse and report results of open-ended questions.
Results
A total of 16 first-year fellows completed the 4-week PCBC experience, eight in each of two academic years. Pre-surveys were completed by all 16 fellows by the 1st day of PCBC, and post-surveys were completed by 15 of 16 fellows within 1 month of completing the PCBC experience. Overall, 12/15 fellows completing the post-survey strongly agreed (scale 1= “disagree strongly”, 3= “disagree somewhat”, 5= “neither agree nor disagree”, 7= “agree somewhat”, and 9= “agree strongly”) that they felt more ready to begin their fellowship clinical responsibilities following participation in PCBC, with the remaining three respondents rating this question 6 or 7. Similarly, 80% strongly agreed (rating 9) that PCBC should be offered in the future to incoming fellows, with other respondents rating this statement 7 or 8 (Fig 1).
Figure 1.
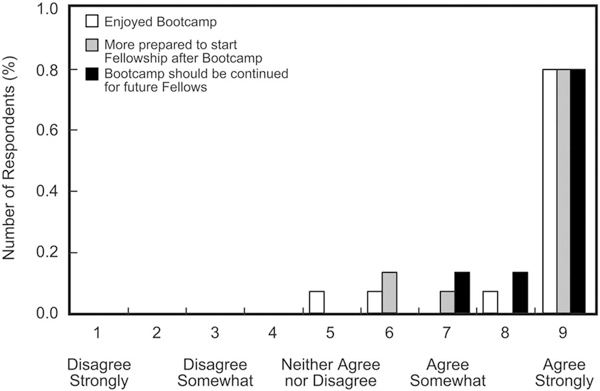
The boot camp leaves learners with greater sense of preparedness to begin paediatric cardiology fellowship.
Additional survey questions addressed participants’ perceived level of preparedness to undertake clinical responsibilities related to specific Bootcamp Learning Objectives. Figure 2 shows median pre- and post-confidence scores for the cohort as a whole for each major objective within each of the five clinical areas. Fellows rated their level of confidence in specific knowledge or skills on a nine-point scale (1, not at all confident; 3, a little confident; 5, somewhat confident; 7, very confident; and 9, extremely confident). The median confidence scores increased for each learning objective across all five areas targeted. Composite scores for each of the five clinical areas were calculated. Figure 3 demonstrates an increase in composite confidence scores in all five areas.
Figure 2.
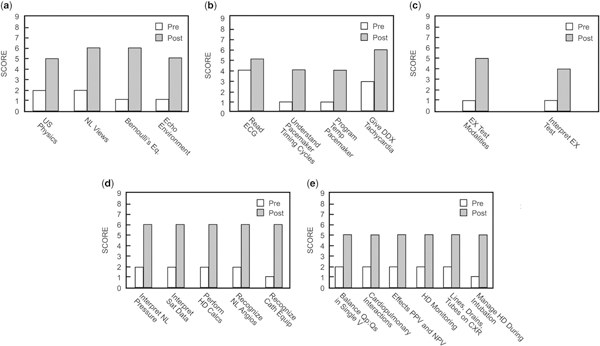
Increase in self-perceived level of preparedness related to all major learning objectives. (a) Echocardiography; (b) electrophysiology; (c) exercise physiology; (d) cardiac catheterisation; (e) cardiac intensive care. US = ultrasound; NL = normal; Eq = Equation; ECG = electrocardiogram; DDX = differential diagnosis; EX = exercise; Sat = saturation; HD = haemodynamic; Qp:Qs = ratio of pulmonary to systemic blood flow; V = ventricle; PPV = positive pressure ventilation; NPV = negative pressure ventilation; CXR = chest radiograph.
Figure 3.
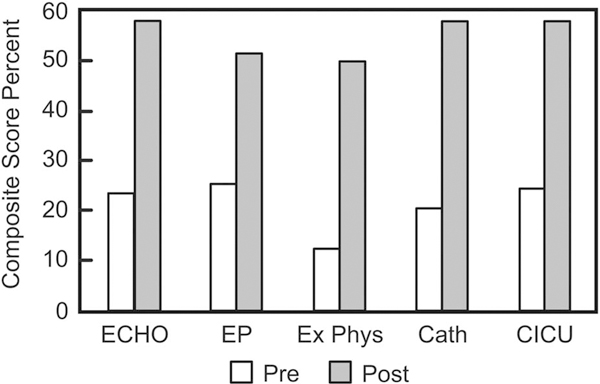
Increase in composite preparedness score across all major disciplines.
Fellows were asked to identify the most and least useful elements of boot camp. Notably, the majority of fellows found simulation-based or hands-on activities to be most useful. This included traditional simulation sessions directed at acquisition of fundamental clinical skills – central line placement and echocardiography – as well as table-top exercises – using a temporary pacemaker, recognition, and handling of catheterisation equipment. Lectures were perceived to be of variable utility, although pathology and electrophysiology lectures were noted to be particular strengths. Just as simulations and hands-on exercises were perceived to be strengths, areas in which these were perceived to be missing – hands-on instruction setting up catheterisation equipment table – were noted as deficiencies of the programme. Fellows cited specific deficiencies in interactive sessions on interpreting angiograms and the opportunity to interpret echocardiograms. In addition to faculty-led hands-on activities, fellows favoured “orientation-type” activities led by other fellows, citing greater sense of preparedness for daily fellowship responsibilities after these practically oriented sessions.
Discussion
Dedicated instructional periods – “boot camps” – have been widely used in surgical and other procedural fields to introduce novice trainees to fundamental procedural skills such as chest tube insertion, suturing, IV placement, and urinary catheter placement, to teach management of specific common clinical entities, and to provide orientation to hospital policy and procedure. In paediatric cardiology, previously reported experience with boot camps includes an echocardiography boot camp aimed at providing novice fellows with fundamental paediatric echocardiography skills through lectures and hands-on, mentored practice sessions.12 In addition, Ceresnak et al reported on a 2-day boot camp experience covering an array of topics in cardiovascular intensive care, catheterisation, electrophysiology, and echocardiography. They demonstrated both an increase in knowledge of participants and greater comfort level when entering fellowship.13 Our paediatric cardiology boot camp is unique, as the duration of dedicated instructional time is significantly greater than most published boot camps. The majority of boot camps provide 2–5 days of dedicated instructional time free of clinical responsibilities.1,8,14 Our boot camp provided 4 weeks of instructional time during which fellows had no other direct clinical responsibilities, allowing us to incorporate a greater breadth of materials and guaranteeing availability for full participation. An 8-week Surgical Internship Boot Camp has been previously described, but this programme required participants to complete concurrent clinical responsibilities, relying heavily on the use of web-based modules for presentation of boot camp material and suffering an 11% rate of absenteeism,15 whereas our curriculum allowed complete immersion in the course materials and experiences.
Another distinguishing feature of our boot camp was the use of multiple teaching modalities. Although many boot camps are strongly skewed towards simulation-based learning activities and lectures, our boot camp also incorporated reflection and experimentation with new concepts through self-guided and group learning activities in an effort to capture all types of adult learners. Many of these self-guided activities were hands-on in nature, such as interpreting catheterisation data and writing a catheterisation report or reading a prescribed set of ECGs. It is notable that in the evaluations, these activities, as well as simulation-based activities, were cited as significant strengths of the PCBC programme, whereas areas where such activities were absent were cited as weaknesses of the programme.
On pre-PCBC surveys, the majority of fellows rated themselves as “not at all confident” to undertake most clinical activities addressed in PCBC, with the notable exceptions of reading electrocardiograms and generating a differential diagnosis of tachycardias. This likely reflects the fact that few paediatric residents have significant exposure to some of the most fundamental knowledge and skills required to practise paediatric cardiology. These data suggest that the PCBC curriculum targeted areas of significant deficit in knowledge and skills as intended.
Notably, a significant increase in confidence to undertake clinical activities related to the PCBC curriculum was seen, with the greatest changes noted in areas that participants rated “not at all confident”. Following training, composite confidence scores ranged from 40 to 50% in each of the five disciplines, reflecting ratings of “somewhat confident”. Given the highly technical nature of the knowledge and skills addressed, it is not surprising that fellows did not achieve levels of very or extremely confident in these areas. The PCBC programme was not designed as a “train-to-competency” exercise, but rather as a foundational introduction to fundamental knowledge and skills on which fellows could build over the subsequent year of fellowship, and to provide them with a working vocabulary to interact with clinicians across the various sub-disciplines in the field of paediatric cardiology. In addition, the breadth of material introduced during the boot camp precluded a train-to-competency model.
Simulation-based activities were consistently rated highly by learners. This is consistent with findings of other boot camps in which simulation-based activities address high-risk procedures or clinical scenarios, which have been traditionally taught by the “see one, do one, teach one” approach. Improved patient outcomes have been linked to use of simulation-based education with deliberate practice compared with traditional educational approaches in central venous catheter placement and management of shoulder dystocia.16–19 Perception by learners of simulation as an effective learning methodology may be related to improved instructional behaviours in the simulated setting compared with during live procedures. Simulation-based teaching has been associated with positive instructional behaviours, particularly in procedural fields, where high acuity, time pressure, and task fixation in the live setting may impair instructional technique.20
Non-simulation-based hands-on and problem-oriented exercises were also consistently cited by learners as strong components of the PCBC. Knowles’21 theory of andragogy suggests that adult learners tend to be oriented towards problem solving and learn best when an educational activity addresses a self-perceived compelling need. Simulation-based activities in this session addressed either high risk – management of airways in haemodynamically unstable patients, code leadership in emergency events – or frequently required – vascular access – skills about which novice trainees often have significant anxiety. Similarly, hands-on exercises such as programming a temporary pacemaker, interpreting ECGs, and interpreting catheterisation data to generate a report reflected clinical activities that fellows would be expected to perform early in their clinical duties, often without direct attending-level supervision immediately available. Thus, incoming fellows would have perceived some urgency to gaining skills in these areas before beginning clinical duties.
Orientation sessions led by more experienced fellows were highly rated by our learners. Our fellows are asked to rapidly acclimate into a high-acuity, high-volume clinical environment within a complex hospital system. Practically oriented sessions related to completion of daily fellowship responsibilities were, thus, highly valued. Inclusion of these sessions is in keeping with a learner-centred educational approach, in which a learner’s past experience and immediate compelling educational needs – as defined by the learner – drive curriculum development. These sessions also served as an important team-building opportunity for fellows both within and across fellowship years. Orientation and team building were pre-defined objectives of the boot camp experience, and attention to clinical systems and collaborative work both have important roles in promoting patient safety. However, these were not the sole objectives of the boot camp experience. Indeed, informal feedback suggested that faculty perceived the primary role of boot camp as an opportunity for fellows to acquire clinical knowledge and skills. This highlights the challenge of creating a balanced curriculum that meets learners’ self-perceived needs and ensures transmission of foundational knowledge – for example, the extensive pathology curriculum from boot camp was a key foundational element that could not readily be provided to fellows outside the boot camp experience, as scheduling limitations during busy clinical months beyond boot camp preclude uniform attendance at pathology lectures.
We describe here a unique 4-week PCBC for incoming cardiology fellows. The curriculum draws strongly on principles of adult learning theory, utilising multiple educational modalities to capture all types of adult learners. Through a combination of small-group didactics, hands-on technical skills practice, self-directed exercises, and simulation training, the programme helps trainees develop a toolbox of knowledge and skills across the breadth of sub-disciplines in the field, and promotes team building as well. This boot camp was not designed with a train-to-competency model, given that one objective was to address a wide range of clinical topics and skills within a relatively limited time frame; however, participation led to a significant increase in confidence to begin the clinical responsibilities of fellowship, and the vast majority of participants felt that the PCBC had high educational value and should continue to be offered to incoming fellows in the future.
Footnotes
Presented at the Johns Hopkins All Children’s Heart Institute Andrews/Daicoff Cardiovascular Program International Symposium on Postgraduate Education in Pediatric and Congenital Cardiac Care, Saint Petersburg, Florida, United States of America, Thursday, 11 February, 2016 and Friday, 12 February, 2016.
References
- 1.Nishisaki A, Hales R, Biagas K, et al. A multi-institutional high-fidelity simulation “boot camp” orientation and training program for first year pediatric critical care fellows. Pediatr Crit Care Med 2009; 10: 157–162. [DOI] [PubMed] [Google Scholar]
- 2.Singh P, Aggarwal R, Pucher PH, Darzi A. Development, Organisation and Implementation of a Surgical Skills “Boot Camp”: SIMweek. World J Surg 2015; 39: 1649–1660. [DOI] [PubMed] [Google Scholar]
- 3.Sonnadara RR, Van Vliet A, Safir O, et al. Orthopedic boot camp: examining the effectiveness of an intensive surgical skills course. Surgery 2011; 149: 745–749. [DOI] [PubMed] [Google Scholar]
- 4.American Board of Surgery, American College of Surgeons, Association of Program Directors in Surgery, Association for Surgical Education. Statement on surgical pre-residency preparatory courses. World J Surg 2014; 38: 2743–2745. [DOI] [PubMed] [Google Scholar]
- 5.Fann JI, Feins RH, Hicks GL Jr, et al. Evaluation of simulation training in cardiothoracic surgery: the Senior Tour perspective. J Thorac Cardiovasc Surg 2012; 143: 264–272. [DOI] [PubMed] [Google Scholar]
- 6.Hicks GL Jr, Gangemi J, Angona RE Jr, Ramphal PS, Feins RH, Fann JI. Cardiopulmonary bypass simulation at the Boot Camp. J Thorac Cardiovasc Surg 2011; 141: 284–292. [DOI] [PubMed] [Google Scholar]
- 7.Blackmore C, Austin J, Lopushinsky SR, Donnon T. Effects of postgraduate medical education “boot camps” on clinical skills, knowledge, and confidence: a meta-analysis. J Grad Med Educ 2014; 6: 643–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen ER, Barsuk JH, Moazed F, et al. Making July safer: simulation-based mastery learning during intern boot camp. Acad Med 2013; 88: 233–239. [DOI] [PubMed] [Google Scholar]
- 9.Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD. “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. Ann Intern Med 2011; 155: 309–315. [DOI] [PubMed] [Google Scholar]
- 10.Kolb DA. Experience as the Source of Learning and Development. Prentice Hall, Englewood Cliffs, NJ, 1984. [Google Scholar]
- 11.Armstrong E, Parsa-Parsi R. How can physicians’ learning styles drive educational planning? Acad Med 2005; 80: 680–684. [DOI] [PubMed] [Google Scholar]
- 12.Maskatia SA, Altman CA, Morris SA, Cabrera AG. The echocardiography “boot camp”: a novel approach in pediatric cardiovascular imaging education. J Am Soc Echocardiogr 2013; 26: 1187–1192. [DOI] [PubMed] [Google Scholar]
- 13.Ceresnak SR, Axelrod DM, Motonaga KS, Johnson ER, Krawczeski CD. Pediatric cardiology boot camp: description and evaluation of a novel intensive training program for pediatric cardiology trainees. Pediatr Cardiol 2016; 37: 834–844. [DOI] [PubMed] [Google Scholar]
- 14.Bismuth J, Duran C, Donovan M, Davies MG, Lumsden AB. The Cardiovascular Fellows Bootcamp. J Vasc Surg 2012; 56: 1155–1161; e1. [DOI] [PubMed] [Google Scholar]
- 15.Krajewski A, Filippa D, Staff I, Singh R, Kirton OC. Implementation of an intern boot camp curriculum to address clinical competencies under the new Accreditation Council for Graduate Medical Education supervision requirements and duty hour restrictions. JAMA Surg 2013; 148: 727–732. [DOI] [PubMed] [Google Scholar]
- 16.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med 2009; 169: 1420–1423. [DOI] [PubMed] [Google Scholar]
- 17.Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med 2009; 37: 2697–2701. [PubMed] [Google Scholar]
- 18.Draycott T, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG. 2006; 113: 177–182. [DOI] [PubMed] [Google Scholar]
- 19.Draycott TJ, Crofts JF, Ash JP, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 2008; 112: 14–20. [DOI] [PubMed] [Google Scholar]
- 20.Fann JI, Sullivan ME, Skeff KM, et al. Teaching behaviors in thecardiac surgery simulation environment. J Thorac Cardiovasc Surg 2013; 145: 45–53. [DOI] [PubMed] [Google Scholar]
- 21.Knowles MS. Andragogy in Action. Jossey-Bass, San Francisco, CA, 1984. [Google Scholar]


