Introduction
We received a call at 9:00 pm on Friday evening, February 28th that our patient had died of coronavirus disease 2019 (COVID-19) disease. This would be the first reported death from COVID-19 in the nation. After suspending disbelief, we began our approach following three guiding principles: provide outpatient dialysis; follow the science; and provide leadership to our community through assurance, transparency, communication, and support. Our patient—whom we will refer to as Patient #1—had last received hemodialysis in the outpatient setting on February 21st. The Centers for Disease Control and Prevention (CDC) lifted testing restrictions on the 28th, at which time our patient was both tested in the intensive care unit and died.
Facing the Pandemic
From there, we immediately stood up our emergency operating center. In coordination with our local public health department, we assembled a list of patients who dialyzed adjacent to Patient #1 both the day that he had a cough and the treatment prior to respiratory symptoms. We traced staff members who had direct patient contact and our hospital services staff who cared for this patient in the hospital. The exposed staff were placed on furlough for a 14-day quarantine with symptoms monitoring, a recommendation that has already changed as described below.
Fortunately, this outpatient facility operated from Sunday to Friday, and therefore, we performed a full disinfection on Saturday. During this time, we developed our symptoms screening tool, which would ultimately apply to all patients and staff, and we developed modifications to personal protective equipment (PPE) aligned with infection prevention and control principles.
We wrote the first of three letters directed to our patients to explain what had happened and what we planned to do. We—our Chief Nursing Officer (CNO), Chief Medical Officer, and local Clinical Director—arrived on site at 0445 hours Sunday morning. We felt that it was critical to communicate directly, chair side, with patients before they heard this information from other sources.
That Sunday night, after we had addressed the most urgent weekend demands, our second patient died. Both Patients #1 and #2 dialyzed at the same dialysis facility on different shifts and days. The latter was a nursing facility resident where there had been an outbreak of COVID-19, but the former had no obvious route of acquisition. The CDC team arrived on site Monday, reviewed data with us, and then, traveled to our facility where the patients who were COVID-19 positive had dialyzed. We had contact with them two to three times per day, with their cell numbers ringing frequently on our CNO’s cell phone.
During the weekend, we contacted all exposed patients who had dialyzed adjacent to Patients #1 and #2, recommending 14-day home quarantine from the day of contact with one critical exception: patients were urged to dialyze at their outpatient facility. Our public health colleagues partnered closely with us, agreeing to this approach.
Although three patients and some staff members developed respiratory symptoms, all tested negative for severe acute respiratory syndrome coronavirus 2, the virus that causes COVID-19 disease. During this time, we developed specific guidance to screen all patients and staff alongside algorithms for staff who became ill, including considerations for returning to work. These were on the basis of the principles listed above and described below (Table 1).
Table 1.
Our guiding principles for the coronavirus disease 2019 outbreak
| Guiding Principles |
|---|
| Provide dialysis |
| Dialyze in the outpatient setting if patient is stable |
| Develop algorithms to screen and dialyze patients |
| Develop algorithms to screen and protect staff |
| Develop algorithms for removal of precautions for patients and staff |
| Create an environment where patients feel safe |
| Follow the science |
| Follow droplet precautions |
| Use PPE judiciously, particularly if supply is allocated |
| Educate staff and patients |
| Work with local and national public health officials |
| Provide leadership |
| Assurances: ensure that staff and patients know that we have their best interest in mind, have a visible presence |
| Transparency: share current-state information with patients and staff |
| Communication: hold frequent calls, disseminate written information, address questions and discussion, give patients and staff opportunity to have input |
| Support: provide patient and employee assistance, demonstrate best practices |
PPE, personal protective equipment.
Providing Dialysis
With our obligation to provide dialysis in the safest and most effective way possible, we developed policies and procedures over the following days. Any patients who were stable to dialyze in the outpatient setting did so. This avoided additional strain to overburdened emergency departments and hospitals. We rolled this out for all of our 19 facilities because we expected COVID-19 to roll out in other regions too.
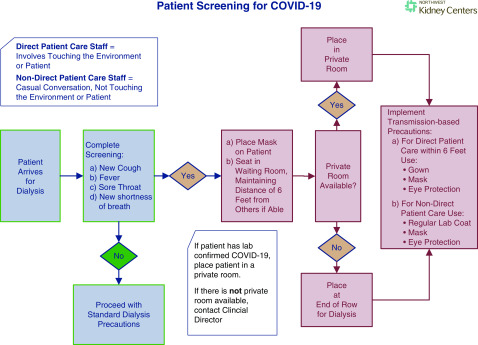
Our current practice is evolving. Now, patients are screened as they enter the facility for fever, new shortness of breath, new cough, and sore throat. Their temperatures are taken as they enter the clinic rather than at bedside (Figure 1). New signage has clear, consistent messages. Any patients with symptoms immediately don a mask and if necessary, sit in the waiting area at least 6 feet from others. Those with positive screens are dialyzed in private rooms if available or cohorted at the end of a row. We considered but have not created a separate location for patients with COVID-19. For provision of dialysis to these patients, staff members were taught to don and doff PPE for modified droplet-contact precautions, which included mask, face shield, gloves, and disposable gown. We created a video to facilitate consistent teaching.
Figure 1.
Patient screening and disposition for coronavirus disease 2019 (COVID-19) symptoms.
Clinical staff underwent the same screening as patients. If staff members have symptoms, they cease work and put on a mask. If they have a diagnosis other than COVID-19, they can return to work when afebrile for 24 hours with waning symptoms. If they have no diagnosis or test positive for COVID-19, they can return per our local guidance—which may evolve—7 days after diagnosis or 72 hours after symptoms mitigate, whichever is longer; they will wear a mask until symptoms resolve or 14 days after diagnosis, also whichever is longer. We have not fully followed current CDC recommendations to allow staff back to work with two tests negative for COVID-19 24 hours apart due to limited testing capacity. However, we encourage testing for clinical staff because a negative test shortens the time until a health care worker can return to work. In a time of staff shortage, this may prove critical. We are fortunate in Washington state to have four current testing locations and turnaround time of 1 day at the local university virology laboratory.
Following the Science
COVID-19 is a droplet disease, not airborne (1). Initially, guidelines recommended use of N95 masks and negative pressure rooms, which did not align with droplet disease recommendations. In conjunction with CDC staff, we instituted the “modified droplet-contact precautions” described above. We emphasized that such PPE should be used when appropriate, not uniformly for all patients and staff, given the known science behind the recommendations. Noting that supplies were and are on allocation, we did our best to be good stewards of our available resources. With concern for lack of supplies, such as the mysterious disappearance of two trunks of hand sanitizer, we set up a cart system to allocate daily supply needs to each location. Then, we contracted with a company to compound hand gel and had to find 55-gallon drums of isopropyl alcohol to supply them. Even with this in place, we had concerns that some supplies would not last until the next shipment. We went to extremes to buy bandanas in case we ran out of masks (2).
At our dialysis facilities, we implemented disinfection procedures for areas that were not routinely addressed, such as rails on scales, doorknobs to bathrooms, seats in the waiting rooms, and hand rests on wheelchairs. We now have checklists to sanitize these and other items at appropriate intervals.
Providing Leadership
We have done our best to show strong leadership presence. We hope to provide assurances to patients, staff, and family that the appropriate attention and resources are being used to address this dire situation not only at the affected facility but throughout the organization.
We felt that it was essential for our patients and staff to feel safe. We tried to achieve this with timely, transparent communication. From onset, we provided direct communication to patients—preferably face to face. We continue to update our patient letter, explaining events and providing precautions. In fact, with multiple new strategies in place, several patients commented that they felt safer at dialysis than other places around town, such as the grocery store or doctors’ appointments.
We craft daily communications to staff. We hold conference calls every weekday for medical directors and medical staff members, with information via email including contacts to address concerns. We held conference calls for each dialysis facility and our hospital services staff so that frontline employees had the opportunity to hear from leadership and ask questions. We began weekday calls for all clinical and nonclinical staff.
We held executive group “huddles” at least daily to review ongoing events and follow-up items. Critical to optimize communication, our Chief Executive Officer designated a point person to lead this charge. With our CNO and Vice President of Patient Care Services in this role, we established clear lines of reporting and communication, which served to keep our leaders well organized and on task.
Community Perspective and Future State
Now, COVID-19 is present in our broader community. As of today, it has affected every state in our nation (3). Other communities will encounter similar situations to ours, and therefore, we hope to share what we have learned, providing support for each other. At Northwest Kidney Centers, we have experienced several “firsts.” Founded in 1962, we were the first dialysis organization in the world (4). Now, it seems that we have the dubious distinction as first in the nation to address the COVID-19 virus. This was not the plan; nonetheless, we hope to continue our mission, promoting the optimal health, quality of life, and independence of people with kidney disease through patient care, education, and research. Hopefully, this perspective can provide some guidance to others who are affected or who are preparing to address COVID-19.
Disclosures
Dr. Watnick and Ms. McNamara have nothing to disclose.
Funding
None.
Acknowledgments
This information is current as of March 17th, 2020. Practices and guidance may have substantially evolved from the current state. The content of this article does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN. Responsibility for the information and views expressed therein lies entirely with the author(s).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 55: 105924, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention: Strategies for optimizing the supply of facemasks, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html. Accessed March 17, 2020
- 3.Centers for Disease Control and Prevention: Coronavirus in the US: Map, case counts and news, 2020. Available at: https://www.livescience.com/coronavirus-updates-united-states.html. Accessed March 18, 2020
- 4.Blagg CR: 50th Anniversary of the opening of the world’s first out-of-hospital dialysis unit, January 8, 1962. Hemodial Int 16: 122–127, 2012 [DOI] [PubMed] [Google Scholar]