Abstract
Aims
Smaller hippocampal volumes are among the most consistently reported neuroimaging findings in schizophrenia. However, little is known about hippocampal volumes in people who report psychotic experiences. This study investigated differences in hippocampal volume between young people without formal diagnoses who report psychotic experiences (PEs) and those who do not report such experiences. This study also investigated if any differences persisted over two years.
Methods
A nested case-control study of 25 adolescents (mean age 13.5 years) with reported PEs and 25 matched controls (mean age 13.36 years) without PEs were drawn from a sample of 100 local schoolchildren. High-resolution T1-weighted anatomical imaging and subsequent automated cortical segmentation (Freesurfer 6.0) was undertaken to determine total hippocampal volumes. Comprehensive semi-structured clinical interviews were also performed including information on PEs, mental diagnoses and early life stress (bullying). Participants were invited for a second scan at two years.
Results
19 adolescents with PEs and 19 controls completed both scans. Hippocampal volumes were bilaterally lower in the PE group compared to the controls with moderate effects sizes both at baseline [left hippocampus p = 0.024 d = 0.736, right hippocampus p = 0.018, d = 0.738] and at 2 year follow up [left hippocampus p = 0.027 d = 0.702, right = 0.048 d = 0.659] throughout. These differences survived adjustment for co-morbid mental disorders and early life stress.
Conclusions
Psychotic experiences are associated with total hippocampal volume loss in young people and this volume loss appears to be independent of possible confounders such as co-morbid disorders and early life stress.
Introduction
One of the most consistent structural neuroimaging findings across all brain areas in schizophrenia research is that of smaller hippocampal volumes in patients with the disorder [1–3]. Meta-analyses of patients with schizophrenia also reveal that the hippocampus shows the largest volumetric difference when compared to other brain structures [4]. Interestingly, smaller hippocampal volumes are similarly reported in patients with first-episode psychosis and also patients in the At-Risk Mental State (a preclinical state indicating a likely conversion to a formal diagnosis of a psychotic disorder) [5]. These findings suggest a potential etiological role for this key temporal lobe structure in schizophrenia and other psychotic disorders.
The hippocampus is of particular interest in psychosis due to its location deep within the temporal lobe and its role as a key limbic hub. This complex structure processes important memory and spatial information and then transmits this encoded information throughout the brain, in particular to regions involved with emotional, behavioral and cognitive processing [6–8]. These regions, such as the cingulate and frontal cortices, hypothalamic areas and adjacent temporal structures are also known to be involved in psychosis. Changes in the expression and transmission of neurotransmitters such as GABA (γ-aminobutyric acid) and glutamate in the hippocampus have also been proposed as potential etiological disruptions in psychosis [9–12]. Such hippocampal abnormalities found in patients with psychosis are most likely multifactorial in origin, involving a complex combination of genetic predisposition [13], perinatal brain development [14] dose and duration of antipsychotic treatment, [15, 16] co-morbid mental disorders [17,18] and in particular exposure to early life stressors [19, 20].
Recent research has proposed the existence of an extended psychosis phenotype in the general population [21, 22]. Rather than psychotic disorders existing as discrete independent entities, it is suggested that psychosis may exist as a continuum of reality testing with varying levels of severity of psychotic experience blending along the continuum [23]. Between 8–17% of children and adolescents [21] and 7% of adults [22] in the general population report psychotic experiences (PEs) such as hallucinations and delusions but only a small proportion ever meet the stringent criteria for a diagnosable psychotic disorder. This extended psychosis phenotype model proposes that schizophrenia lies at the extreme end of a psychosis continuum with the majority of individuals experiencing less severe hallucinatory and delusional experiences with varying degrees of intact reality testing [24]. However, it is reported that individuals who describe PEs in early life are at increased risk of being diagnosed with a psychotic disorder such as schizophrenia [25, 26]. Interestingly, recent research has shown that individuals who report psychotic experiences are at risk of a wide range of mental disorders. Such disorders are just not limited to psychosis, however, and include other diagnosable psychiatric conditions such as depression and anxiety [27–29], as well as other poor mental health outcomes including suicidal behavior [30], poorer socio-occupational function [28, 31], and neurocognitive deficits [32, 33]. Although PEs appear common in the general population and are associated with serious sequelae, little is known about the brain changes, if any, in individuals with PEs. In particular, there has been no research regarding hippocampal volumes in young individuals who report PEs but do not meet the criteria for an identified psychotic disorder such as schizophrenia.
Psychotic disorders have consistently been associated with early life stressors such as neglect, sexual, physical and emotional abuse [34, 35]. Recent studies have also shown an association between childhood maltreatment or bullying and the extended psychosis phenotype [36, 37]. Although the majority of psychotic symptoms do not persist over time (longitudinal studies typically demonstrate persistence rates of between 15% to 25% [38, 39], research has shown that ongoing exposure to trauma increases the odds that psychotic symptoms will persist [40]. Of note, young people with persistent psychotic symptoms have been shown to have poorer clinical and functional outcomes [41].
To our knowledge, there has been no published longitudinal research to date examining hippocampal volumes and early life stress in young people with psychotic experiences. We hypothesize that adolescents with PEs will show reduced global hippocampal volume both at baseline and at follow-up compared to adolescents without PEs. We further hypothesize that a proportion of this hippocampal volume loss may be accounted for by a history of early life stress and/or by the presence of co-morbid mental disorders. To these ends, in this study, we investigated 1) if hippocampal volume differences exist between young people who report PEs and those who do not; 2) if these differences, if any, persist for 2 years through adolescence and 3) if these differences could be associated with co-morbid mental disorders and early adversity.
Methods
Participants
Between July 2007 and September 2010, 212 young people aged between 11–13 years were recruited from primary schools in Dublin and Kildare, Ireland [42]. All 212 participants were white and native English-speaking and attended for a semi-structured clinical interview and neurocognitive testing. For further details on the recruitment and interview assessments see Kelleher et al. [42]. A subsample of 100 of the original study participants also agreed to take part in a neuroimaging study. 25 of these adolescents reported psychotic experiences and constituted the Psychotic Experiences (PEs) group. From the remaining participants with brain imaging, 25 adolescents without psychotic symptoms were selected to match the PE group for age (at the time of scanning), gender and handedness to create the control group. All participants were naïve for both psychotropic medication and illicit substance use. Participants were followed up two years after the baseline neuroimaging scans and interviews.
Clinical interviews
The Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) is a well-validated, semi-structured research diagnostic interview for the assessment of current and lifetime DSM-IV mental disorders in children and adolescents [43]. Interviews with both the young person and a parent were carried out at baseline and repeated with the young person at 2-year follow-up. All interviews were carried out by trained interviewers with a background in mental health.
Psychotic experiences
The psychosis section of the K-SADS contains screening questions designed to assess hallucinations and delusions [42]. If one of the screening questions elicited a positive response, further details were ascertained using the SOCRATES template. This allowed perceptual abnormalities and unusual thought content to be explored and documented in a systematic and comprehensive manner. The SOCRATES template is available for download at https://epubs.rcsi.ie/psychart/19/. The history was transcribed and discussed at a consensus meeting involving three investigators (MC, IK, and MH who are mental health professionals with expertise in psychosis). At this meeting a decision was also reached on whether the young person had reported a “definite” psychotic symptom.
Mental disorders
Diagnoses of any Axis 1 mental disorders at baseline interview were made using DSM-IV criteria. This was coded as a yes/no variable.
Early life stress (bullying)
Information on any history of bullying up to the time of the baseline interview was obtained during the clinical interview. Bullying by our definition constituted either/and physical or psychosocial intimidation, harm, or coercion. This was coded as a binary yes/no variable depending on whether the participant endorsed being a victim of bullying at any time in their life.
Ethical approval was obtained from the Medical Research Ethics Committee, Beaumont Hospital, Dublin, and the School of Psychology, Trinity College Dublin. Written parental consent and participant assent were obtained prior to the study.
High-resolution anatomy imaging
180 axial high-resolution T1-weighted anatomical images (TE = 3.8 ms, TR = 8.4 ms, FOV 230 x 230 mm2, 0.898 x 0.898 mm2 in-plane resolution, slice thickness 0.9 mm, flip angle alpha = 8°) were acquired. The acquisition time was approximately 6.5 minutes. All scanning was conducted on the same scanner (Philips Intera Achieva 3.0 Tesla) at the Trinity College Institute of Neuroscience, Dublin.
Imaging analysis
Cortical reconstruction and volumetric segmentation was performed with the Freesurfer 5.3 image analysis suite (http://surfer.nmr.mgh.harvard.edu/) [44, 45]. The technical details of these procedures are described in prior publications [46–51]. In particular, the hippocampal analysis tool from the developmental version of FreeSurfer (v6.0 2017) was utilized to calculate hippocampal subfield volumes. This features novel algorithms using Bayesian inference [52] and high-resolution ex-vivo MRI atlas data offering improved accuracy and reliability [53]. Total hippocampal volume estimates where calculated by combining all individual subfield measures to yield a global hippocampal measure. An estimated measure for total intracranial volume (eTIV) was obtained from the routine output of Freesurfer using the MRI-seg- stats tool [54]. This procedure applies a one-parameter scaling factor calculated during the normalization transformation to the standard MNI305 brain.
Statistical analysis
Statistical analysis was performed with SPSS software (version 21) [55]. All hippocampal volume measures were initially investigated using the “Explore” function within SPSS to assess data normality and outlier identification. Systematic inspection of the data was then performed. Outliers were defined as volumes greater than 1.5 x interquartile (IQ) range and extremes as 3 x IQ range as per the standard SPSS boxplot summary output. The normality of the quantitative variables was studied through the Kolmogorov-Smirnov test [56], to determine the appropriate use of either parametric or non-parametric hypothesis tests. Since the data did meet the assumption of normal distribution, parametric tests were used in their analysis. All comparisons were performed for each hemisphere independently.
In our primary analysis: mixed-model repeated measures (MMRM) was used in order to explore the effects of Group x Time interaction between the Control and PE group for hippocampal volumes during the 2-year follow-up controlled for estimated Total Intracranial Volume (eTIV), Axis-1 disorders and Early Life Stress (Bullying). Within this analysis we also studied the inter- and intra-group differences during the 2-year follow-up.
Forward stepwise forced entry linear regression was performed to determine whether differences in hippocampal volume could be accounted for by co-morbid mental disorders or early adversity. The variable ‘Hippocampus’ (left and right at baseline and two years follow up) was used as a dependent variable and, as independent factors, we included the “group” variable (PE and Control) and eTIV in the first step and bullying and other diagnosis in the second step.
Effect sizes were determined to quantify the differences between groups. The effect size was calculated within each treatment condition and then subtracting the control group from the experimental group effect size. The effect size for each treatment condition is defined as the pre to post test change divided by the pre-test standard deviation. The magnitude of effect sizes can be described as small (d = 0.2), medium (d = 0.5) and large (d = 0.8) [57]. In addition, the effect size of the regression analyses were based on Cohen’s (1988) guidelines with f2≥ 0.02, f2≥ 0.15, and f2 ≥ 0.35 representing small, medium, and large effect sizes, respectively.
Results
Demographics
There were no significant differences between the PE group and the control group for age, gender or handedness (Table 1). At baseline the presence of mental disorders and early life stress were common in the PE group (Table 1). 60% of adolescents with PEs had been bullied compared with 24% in the control group. Similarly, 60% of adolescents with PEs had been diagnosed with an Axis 1 mental disorder at baseline compared with 28% in the control group.
Table 1. Sociodemographic and clinical data at baseline.
All values are expressed as percentages (%) unless otherwise indicated.
| PE, n = 25 | Controls, n = 25 | p-value | |
|---|---|---|---|
| Mean age (years), mean (SD) | 13.5 (1.26) | 13.36 (1.15) | 0.642 |
| Gender (Male) | 8(32) | 10(40) | 0.765 |
| Handedness (Right) | 23(92) | 24(96) | 0.552 |
| Co-morbid Axis 1 mental disorders | 15(60) | 7(28) | 0.023 |
| History of Bullying | 15(60) | 6(24) | 0.009 |
SD, standard deviation; PE, adolescents reporting psychotic experiences.
76% percent of the sample returned for follow-up after two years. PE group (n = 19) and the Control group (n = 19).
Hippocampal volumes
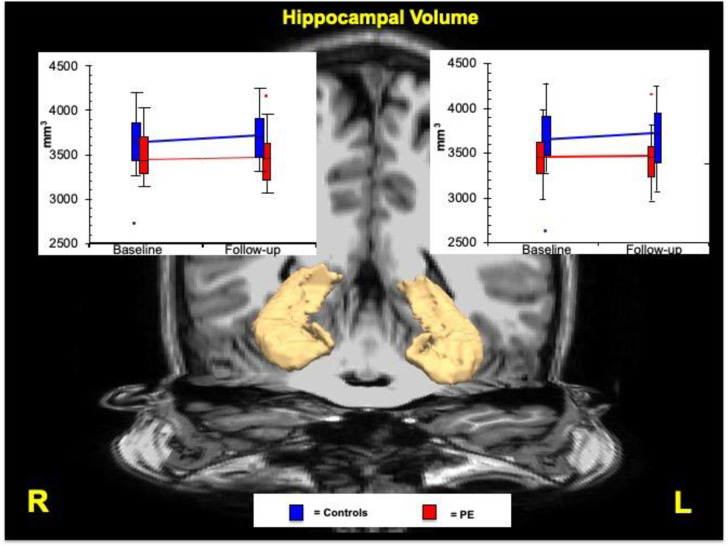
A total of four outliers were removed; one from each group at both timepoints (see Fig 1). At baseline there was a main effect for Group on the left [F(1,76) = 10,182 (p = 0.002)] and right [F(1,76) = 9,488 (p = 0.003)] whole hippocampal volumes. No Group x Time interaction was found in either in the left (p = 0.944) or right (p = 0.735) whole hippocampal volumes.
Fig 1. Patterns of change of hippocampal volume over 2 years follow-up between the PE and control group.
Graphs show volumetric measures at baseline and follow-up in left and right whole hippocampus. Trendlines provide rates of volume change during the two time points between the PE and control group. Blue represents the control group and red represents the PE group. Outliers are shown as dots in both graphs. Volumes are shown in millimeters cubed. PE, adolescents reporting psychotic experiences.
In the inter-group analysis, significant differences were found between the PE and Control group at baseline in the left and right hippocampal volumes and these differences persisted at two-year follow-up (Table 2). The PE group had significantly smaller hippocampal volumes throughout the sample with a large effect size for both left (d = 1.266) and right (d = 0.768) hippocampus. Specifically, moderate effect sizes were seen between the groups at baseline for the left (d = 0,736) and right (d = 0,738) hippocampus, and similarly between the groups at two years for the left (d = -0,702) and right (d = -0,659) hippocampus.
Table 2. Mixed model analysis: Whole hippocampal volumes.
Whole hippomcampal volumes were calculated throught the summation of all hippocampal outputs from using Freesurfer 6.0 and shown in millimeters cubed.
| PE hippocampal volumes (mm3)/(SEM) | Controls hippocampal volumes (mm3)/(SEM) | p-value (effect size) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structure | Baseline (n = 25) | 95% CI | Follow-up (n = 19) | 95% CI | Baseline (n = 25) | 95% CI | Follow-up (n = 19) | 95% CI | Baseline: time 1 | Follow up: time 2 | Overall effect size |
| Left | 3462(55) | 3346,964–3577.591 | 3466(59) | 3311.197–3590.874 | 3652(56) | 3534.530–3769.913 | 3727(62) | 3532.229–3840.417 | 0.024 (0.736) | 0.027 (0.702) | d = 1.266 |
| Right | 3448(57) | 3330,873–3565.251 | 3475(61) | 3307.085–3591.311 | 3651(58) | 3532.264–3771.476 | 3723(64) | 3505.952–3819.154 | 0.018 (0.738) | 0.048 (0.659) | d = 0.768 |
CI, confidence interval; SEM, standard error of the mean.
In the intra-group analysis, no significant differences in hippocampal volumes were found within either the PE or group between baseline and two-year follow up.
In the fully adjusted model, significant differences were found in the left and right hippocampus between PE and Control group at baseline and these differences persisted at two-year follow up. The percentages of changes over time were different between the 2 groups (see Fig 1)
Forward stepwise forced entry linear regression
Following linear regression, left and right hippocampal volumes at baseline and two years follow up were used as the dependent variables. The Group variable (PE and Control) and eTIV were included in the first step and Bullying and Axis-1 diagnosis as independent factors were included in the second step.
Left hippocampal volume linear regression
At baseline, Group and eTIV accounted for 30.1% of the variance in left hippocampal volume (F = 9.472, p = 0.0004, effect size f2 = 0.431 = large). Adding Bullying and Axis-1 diagnosis to the model did not significantly account for an additional proportion of the variance (Adjusted R2 changed: 2.5%, F = 0.774, p = .468, effect size f2 = 0.026 = small). In the second step, the beta co-efficients indicated that eTIV (Beta = 0.421, p = 0.002) and Group (Beta = -0.337, p = 0.023) contributed significantly to the model and were independently associated with left hippocampal volume but Bullying (Beta = 0.173, p = 0.227) and Axis-1 diagnosis (Beta = -0.067, p = 0.635) were not.
At two years follow up, Group and eTIV accounted for 50.9% of the variance in left hippocampal volume (F = 13.466, p = 0.0001, effect size f2 = 1.036 = large). Adding Bullying and Axis -1 diagnosis to the model significantly accounted for an additional proportion of the variance (Adjusted R2 changed: 17.2%, F = 6.464 p = 0.006, effect size f2 = 0.208 = medium). In the second step, the beta co-efficients indicated that eTIV (Beta = -0.618 p = 0.00002), Bullying (Beta = 0.458 p = 0.002) and Group (B = -0.38 p = 0.008), all contributed significantly and were independently associated as ordered with left hippocampal volume but Axis-1 diagnosis (Beta = -0.146 p = 0.260) was not.
Right hippocampal volume linear regression
At baseline, Group and eTIV accounted for 36.8% of the variance in right hippocampal volume (F = 12.790, p = 0.001, effect size f2 = 0.582 = large). Adding Bullying and Axis-1 diagnosis to the model did not significantly account for an additional proportion of the variance (Adjusted R2 changed: 4.5%, F = 3.27 p = 0.078, effect size f2 = 0.066 = small). In the second step, the co-efficients indicated that eTIV (Beta = 0.498, p = 0.001), Group (Beta = -0.336, p = 0.014), and Bullying (Beta = 0.261, p = 0.050) were independently associated with right hippocampal volume but Axis -1 diagnosis (Beta = -0.144, p = 0.265) was not.
In addition, at two years follow up, Group and eTIV accounted for 33.0% of the variance in right hippocampal volume (F = 6.416, p = 0.005, effect size f2 = 0.493 = large). Adding bullying and Axis-1diagnosis to the model did not significantly accounted for an additional proportion of the variance (Adjusted R2 changed: 8.0%, F = 1.622 p = 0.218, effect size f2 = 0.087 = small). In the second step, the co-efficients indicated that eTIV (B = 0.468, p = 0.008) was significantly independently associated with right hippocampal volume but Group (B = -0.348, p = 0.062), Bullying (B = 0.313, p = 0.085) and Axis -1 diagnosis (B = -0.084, p = 0.631) were not.
Discussion
This study investigated hippocampal volumes in adolescents with psychotic experiences (PEs) and hippocampal volumes in adolescents without PEs at two time-points, two years apart. Hippocampal volumes were found to be smaller bilaterally in the young adults who reported PEs at both timepoints. These differences were not accounted for by differences in the rate of co-morbid mental disorders or early life stress between the groups.
While significant brain variations have been found to exist in individuals with diagnosable psychotic disorders, there has been limited research on the neurobiology of the extended psychosis phenotype. Our group has previously reported structural and functional differences in frontotemporal regions [58] and bilateral white matter differences in both frontotemporal and striatal regions in adolescents with PEs [58, 59]. Other recent population-based studies identified both global reduced gray matter volume and increased white matter volume, and, more specifically decreased hippocampal and amygdala volumes with structural and functional dysconnectivity in young adults with psychotic symptoms [60–63].
Adolescents with PEs have a four-fold increased risk of developing a psychotic disorder [25]. Smaller hippocampal volumes are one of the most replicated neuroimaging findings in patients with psychosis [64–66], implying an important role for this highly integrated limbic structure in the disorder. Our finding of bilateral smaller hippocampal volumes at baseline scan and also at two-year follow up in adolescents with PEs suggests that hippocampal volume may have a role as an early vulnerability marker for psychosis. The mean age of 13 years in our PE group at baseline scan suggests that smaller bilateral hippocampal volumes may already be present in late childhood in those at risk for psychosis.
A recent study reported that childhood trauma is associated with hippocampal and amygdala volume in first-episode psychosis and suggests that childhood traumatic experiences may contribute to the different brain morphology in individuals diagnosed with psychosis [67]. Previous studies found that environmental factors including early life stress may also be implicated in reduced hippocampal volume as has been shown in depression [68, 69]. Adverse early life environmental factors are thought to interact with an inherent genetic vulnerability to produce hippocampal change [69]. Similarly, another recent study suggests that the effect of childhood trauma on the risk of psychosis may be mediated through changes in hippocampal function [70].
In this study, we accounted for the possible moderating effect of a commonly reported early life stress, bullying. Studies vary, but between 11–21% of children relate being bullied in early life [71, 72]. Adolescents in our study reported marginally higher rates of bullying in controls (24%) and particularly higher rates in those who experienced psychotic symptoms (60%). The higher reported rates in controls may be due to local factors or potentially as a result of recent destigmatization campaigns run by the local health and social services in Ireland. These campaigns encourage young adolescents to report and talk about bullying and other experiences. The increased reported bullying in our cohort of adolescents who experienced psychotic symptoms is consistent with higher rates of bullying found in other studies of individuals in the extended psychosis phenotype. Although this study found that bullying may be associated with smaller hippocampal volumes, the association between PEs and hippocampal volume appears to be independent of the effects of bullying. Similarly, this study did not find an effect of Axis-1 disorders diagnosis on hippocampal volumes, over and above the experience of PEs. All participants were free of any psychotropic medication, including antipsychotics, negating a role for these medications in the smaller hippocampal volumes found in this study [14].
Strengths and limitations
The strengths of this study include a well-described and well-matched sample of treatment and substance-naive adolescents. The use of a community-based sample rather than a hospital or clinic-based sample increases the generalizability of these results to other adolescent groups. 75% of the sample returned for repeat scanning on the same scanner two years later. Our analysis accounted for potential confounding by comorbid mental disorders and early life stress. In terms of limitations, we acknowledge that our sample is relatively small, localized to an Irish context and that our findings require replication in a larger and broader international sample. Also, this study only investigated bullying as a source of early life stress. It is entirely possible that other forms of abuse and neglect may reveal different relationships between hippocampal size and PEs in adolescents.
In conclusion, our findings of lower global bilateral hippocampal volumes in young people who report PEs suggest that smaller hippocampi at age 13 may be indicative of a broad psychosis phenotype. This study also found that young people who report PEs in early adolescence do not appear to recover hippocampal volumes to control levels after two years. These findings suggest a role for hippocampal volumes as potential biomarkers for psychosis later in life and hint at the benefits of early identification and treatment of young people who report PEs to alleviate hippocampal volume loss. This study also highlights the need for further neuroimaging and other biological research to elucidate the mechanism and relationship between smaller hippocampi in early adolescents with PEs and psychosis in later life.
Acknowledgments
We acknowledge the use of the facilities of the Clinical Research Centre in the RCSI Education and Research Centre and Trinity College High-Performance Computing support and infrastructure funded by Science Foundation Ireland. We thank Mr. Ciaran Conneely, Administrator, Trinity College Institute of Neuroscience (TCIN) and Mr. Sojo Joseph, TCIN MRI Radiographer. We would particularly like to thank all the young participants and their parents for giving their time to this study.
A Calvo, E O’Hanlon, D Roddy and M Cannon had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Data Availability
Data are not publicly available because of ethics and data protection consideration. This data contains potentially sensitive and identifying material as determined by Beaumont Hospital Medical Ethics Committee. Data can be requested via email from Beaumontethics@rcsi.ie.
Funding Statement
This study was funded by a European Research Council Consolidator Award [724809 iHEAR] to MCannon and by the Health Research Board Ireland [HRA/PHS/2-012/28 (EO’H)]. AC was supported through Alicia Koplowitz grant for Short-Term Placements from the Alicia Koplowitz Foundation. HC was supported by an Interdisciplinary Capacity Enhancement Award from the Health Research Board (ICE/2012/11) to M Cannon and M Clarke. The research of AL. is supported by VIDI Grant 639.072.411 from the Netherlands Organization for Scientific Research (NWO). IK is funded by a STaR lectureship from the Royal College of Surgeons in Ireland.
References
- 1.Heckers S, Konradi C. Hippocampal pathology in schizophrenia. Curr Top Behav Neurosci. 2010;4:529–53. 10.1007/7854_2010_43 [DOI] [PubMed] [Google Scholar]
- 2.van Erp TG, Hibar DP, Rasmussen JM, Glahn DC, Pearlson GD, Andreassen OA, et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry. 2016;21(4):585 10.1038/mp.2015.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brugger SP, Howes OD. Heterogeneity and Homogeneity of Regional Brain Structure in Schizophrenia: A Meta-analysis. JAMA Psychiatry. 2017;74(11):1104–11. 10.1001/jamapsychiatry.2017.2663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright IC, Rabe-Hesketh S, Woodruff PW, David AS, Murray RM, Bullmore ET. Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry. 2000;157(1):16–25. 10.1176/ajp.157.1.16 [DOI] [PubMed] [Google Scholar]
- 5.Nenadic I, Dietzek M, Schönfeld N, Lorenz C, Gussew A, Reichenchab Jr, et al. Brain structure in people at ultra-high risk of psychosis, patients with first-episode schizophrenia, and healthy contorls: a VBM study. Schizophr Res. 2015. February;161(2–3):169–76. 10.1016/j.schres.2014.10.041 [DOI] [PubMed] [Google Scholar]
- 6.Bird C, Burgess N. The hippocampus and memory: insights from apatial processing. Nat Rev Neurosci 2008, 9, 182–194, 10.1038/nrn2335 [DOI] [PubMed] [Google Scholar]
- 7.Roddy D, O’Keane V. Cornu Ammonis Changes Are at the Core of Hippocampal Pathology in Depression. Chronic Stress. 2019;3:2470547019849376 10.1177/2470547019849376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weininger JK, Roman E, Tierney P, Barry D, Gallagher H, Levins KJ, et al. Papez’s forgotten tract: 80 years of unreconciled findings concerning the thalamocingulate tract. Frontiers in neuroanatomy. 2019;13:14 10.3389/fnana.2019.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baumann PS, Griffa A, Fournier M, Golay P, Ferrari C, Alameda L, et al. Impaired fornix-hippocampus integrity is linked to peripheral glutathione peroxidase in early psychosis. Transl Psychiatry. 2016. July 26;6(7): e859 10.1038/tp.2016.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubovyk V, Manahan-Vaughan D. Distinct Time-Course of Alterations of Groups I and II Metabotropic Glutamate Receptor and GABAergic Receptor Expression Along the Dorsoventral Hippocampal Axis in an Animal Model of Psychosis. Front Behav Neurosci. 2019. May 8;13:98 10.3389/fnbeh.2019.00098 eCollection 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen P, Chaddock CA, Egerton A, Howes OD, Bonoldi I, Zelaya F, et al. Resting Hyperperfusion of the Hippocampus, Midbrain, and Basal Ganglia in People at High Risk for Psychosis. Am J Psychiatry. 2016. April 1;173(4):392–9. 10.1176/appi.ajp.2015.15040485 Epub 2015 Dec 18. [DOI] [PubMed] [Google Scholar]
- 12.Wood SJ, Kennedy D, Phillips LJ, Seal ML, Yucel M, Nelson B, et al. Hippocampal pathology in individuals at ultra-high risk for psychosis: a multi-modal magnetic resonance study. Neuroimage. 2010;52(1):62–8. 10.1016/j.neuroimage.2010.04.012 [DOI] [PubMed] [Google Scholar]
- 13.Harrisberger F, Smieskova R, Vogler C, Egli T, Schmidt A, Lenz C, et al. Impact of polygenic schizophrenia-related risk and hippocampal volumes on the onset of psychosis. Translational psychiatry. 2016;6(8):e868–e. 10.1038/tp.2016.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen P, Moore H, Corcoran CM, Gilleen J, Kozhuharova P, Reichenberg A, et al. Emerging Temporal Lobe Dysfunction in People at Clinical High Risk for Psychosis. Frontiers in Psychiatry. 2019;10(298). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamah D, Harms MP, Barch D, Styner M, Lieberman JA, Wang L. Hippocampal shape and volume changes with antipsychotics in early stage psychotic illness. Front Psychiatry. 2012;3:96 10.3389/fpsyt.2012.00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V. Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia. Arch Gen Psychiatry. 2011;68(2):128–37. 10.1001/archgenpsychiatry.2010.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roddy DW, Farrell C, Doolin K, Roman E, Tozzi L, Frodl T, et al. The Hippocampus in Depression: More Than the Sum of Its Parts? Advanced Hippocampal Substructure Segmentation in Depression. Biol Psychiatry. 2019;85(6):487–97. 10.1016/j.biopsych.2018.08.021 [DOI] [PubMed] [Google Scholar]
- 18.Sheline YI, Liston C, McEwen BS. Parsing the Hippocampus in Depression: Chronic Stress, Hippocampal Volume, and Major Depressive Disorder. Biol Psychiatry. 2019;85(6):436–8. 10.1016/j.biopsych.2019.01.011 [DOI] [PubMed] [Google Scholar]
- 19.Anacker C, Scholz J, O'Donnell KJ, Allemang-Grand R, Diorio J, Bagot RC, et al. Neuroanatomic Differences Associated With Stress Susceptibility and Resilience. Biol Psychiatry. 2016;79(10):840–9. 10.1016/j.biopsych.2015.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, et al. Childhood adversity impacts on brain subcortical structures relevant to depression. J Psychiatr Res. 2017;86:58–65. 10.1016/j.jpsychires.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42(9):1857–63. 10.1017/S0033291711002960 [DOI] [PubMed] [Google Scholar]
- 22.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–49. 10.1017/S0033291712001626 [DOI] [PubMed] [Google Scholar]
- 23.Kaymaz N, Van Os J. Extended psychosis phenotype–yes: single continuum–unlikely: a commentary on ‘Why we need more debate on whether psychotic symptoms lie on a continuum with normality’by David (2010). Psychological medicine. 2010;40(12):1963–6. 10.1017/S0033291710000358 [DOI] [PubMed] [Google Scholar]
- 24.Smeets F, Lataster T, van Winkel R, de Graaf R, Ten Have M, van Os J. Testing the hypothesis that psychotic illness begins when subthreshold hallucinations combine with [DOI] [PubMed]
- 25.Welham J, Scott J, Williams G, Najman J, Bor W, O'Callaghan M, et al. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychol Med. 2009;39(4):625–34. Hippocampal volume loss and psychotic experiences 10.1017/S0033291708003760 [DOI] [PubMed] [Google Scholar]
- 26.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children's self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57(11):1053–8. 10.1001/archpsyc.57.11.1053 [DOI] [PubMed] [Google Scholar]
- 27.Werbeloff N, Drukker M, Dohrenwend BP, Levav I, Yoffe R, van Os J, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. 2012;69(5):467–75. 10.1001/archgenpsychiatry.2011.1580 [DOI] [PubMed] [Google Scholar]
- 28.Wigman JT, van Nierop M, Vollebergh WA, Lieb R, Beesdo-Baum K, Wittchen HU, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra-high risk research. Schizophr Bull. 2012;38(2):247–57. Hippocampal volume loss and psychotic experiences 10.1093/schbul/sbr196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGrath JJ, Saha S, Al-Hamzawi A, Andrade L, Benjet C, Bromet EJ, et al. The Bidirectional Associations Between Psychotic Experiences and DSM-IV Mental Disorders. The American journal of psychiatry. 2016:appiajp201615101293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelleher I, Corcoran P, Keeley H, Wigman JT, Devlin N, Ramsay H, et al. Psychotic symptoms and population risk for suicide attempt: a prospective cohort study. JAMA Psychiatry. 2013;70(9):940–8. 10.1001/jamapsychiatry.2013.140 [DOI] [PubMed] [Google Scholar]
- 31.Armando M, Nelson B, Yung AR, Ross M, Birchwood M, Girardi P, et al. Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr Res. 2010;119(1–3):258–65. 10.1016/j.schres.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 32.Blanchard MM, Jacobson S, Clarke MC, Connor D, Kelleher I, Garavan H, et al. Language, motor and speed of processing deficits in adolescents with subclinical psychotic symptoms. Schizophr Res. 2010;123(1):71–6. 10.1016/j.schres.2010.05.028 [DOI] [PubMed] [Google Scholar]
- 33.Kelleher I, Clarke MC, Rawdon C, Murphy J, Cannon M. Neurocognition in the extended psychosis phenotype: performance of a community sample of adolescents with psychotic symptoms on the MATRICS neurocognitive battery. Schizophr Bull. 2013;39(5):1018–26. 10.1093/schbul/sbs086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34(3):568–79. 10.1093/schbul/sbm121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schalinski I, Fischer Y, Rockstroh B. Impact of childhood adversities on the short-term course of illness in psychotic spectrum disorders. Psychiatry Res. 2015;228(3):633–40. 10.1016/j.psychres.2015.04.052 [DOI] [PubMed] [Google Scholar]
- 36.Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children's emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168(1):65–72. 10.1176/appi.ajp.2010.10040567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cristobal-Narvaez P, Sheinbaum T, Ballespi S, Mitjavila M, Myin-Germeys I, Kwapil TR, et al. Impact of Adverse Childhood Experiences on Psychotic-Like Symptoms and Stress Reactivity in Daily Life in Nonclinical Young Adults. PLoS One. 2016;11(4):e0153557 10.1371/journal.pone.0153557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zammit S, Kounali D, Cannon M, David AS, Gunnell D, Heron J, et al. Psychotic experiences and psychotic disorders at age 18 in relation to psychotic experiences at age 12 in a longitudinal population-based cohort study. Am J Psychiatry. 2013;170(7):742–50. 10.1176/appi.ajp.2013.12060768 [DOI] [PubMed] [Google Scholar]
- 39.Spauwen J, Van Os J. The psychosis proneness: psychosis persistence model as an explanation for the association between urbanicity and psychosis. Epidemiol Psichiatr Soc. 2006;15(4):252 [PubMed] [Google Scholar]
- 40.Kelleher I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170(7):734–41. 10.1176/appi.ajp.2012.12091169 [DOI] [PubMed] [Google Scholar]
- 41.Rutigliano G, Valmaggia L, Landi P, Frascarelli M, Cappucciati M, Sear V, et al. Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra high risk for psychosis. J Affect Disord. 2016;203:101–10. 10.1016/j.jad.2016.05.053 [DOI] [PubMed] [Google Scholar]
- 42.Kelleher I, Murtagh A, Molloy C, Roddy S, Clarke MC, Harley M, et al. Identification and characterization of prodromal risk syndromes in young adolescents in the community: a population-based clinical interview study. Schizophr Bull. 2012;38(2):239–46. 10.1093/schbul/sbr164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–8. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 44.Fischl B. FreeSurfer. Neuroimage. 2012;62(2):774–81. 10.1016/j.neuroimage.2012.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci U S A. 2000;97(20):11050–5. 10.1073/pnas.200033797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999;9(2):179–94. 10.1006/nimg.1998.0395 [DOI] [PubMed] [Google Scholar]
- 47.Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31(3):968–80. 10.1016/j.neuroimage.2006.01.021 [DOI] [PubMed] [Google Scholar]
- 48.Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33(3):341–55. 10.1016/s0896-6273(02)00569-x [DOI] [PubMed] [Google Scholar]
- 49.Fischl B, Sereno MI, Dale AM. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage. 1999;9(2):195–207. 10.1006/nimg.1998.0396 [DOI] [PubMed] [Google Scholar]
- 50.Fischl B, van der Kouwe A, Destrieux C, Halgren E, Segonne F, Salat DH, et al. Automatically parcellating the human cerebral cortex. Cereb Cortex. 2004;14(1):11–22. 10.1093/cercor/bhg087 [DOI] [PubMed] [Google Scholar]
- 51.Reuter M, Schmansky NJ, Rosas HD, Fischl B. Within-subject template estimation for unbiased longitudinal image analysis. Neuroimage. 2012;61(4):1402–18. 10.1016/j.neuroimage.2012.02.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Leemput K. Encoding probabilistic brain atlases using Bayesian inference. IEEE Transactions on Medical Imaging. 2009;28(6):822 10.1109/TMI.2008.2010434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Iglesias JE, Augustinack JC, Nguyen K, Player CM, Player A, Wright M, et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: Application to adaptive segmentation of in vivo MRI. Neuroimage. 2015;115:117–37. 10.1016/j.neuroimage.2015.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buckner RL, Head D, Parker J, Fotenos AF, Marcus D, Morris JC, et al. A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: reliability and validation against manual measurement of total intracranial volume. Neuroimage. 2004;23(2):724–38. 10.1016/j.neuroimage.2004.06.018 [DOI] [PubMed] [Google Scholar]
- 55.Corp I. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; Released 2012. [Google Scholar]
- 56.Simard R, L’Ecuyer P. Computing the two-sided Kolmogorov-Smirnov distribution. Journal of Statistical Software. 2011;39(11):1–18. [Google Scholar]
- 57.Cohen J. Statistical power analysis for the behavioral sciences (2nd ed). Hillsdale, NJ: Lawrence Earlbaum Associates; 1998. [Google Scholar]
- 58.Jacobson S, Kelleher I, Harley M, Murtagh A, Clarke M, Blanchard M, et al. Structural and functional brain correlates of subclinical psychotic symptoms in 11–13 year old schoolchildren. NeuroImage. 2010;49(2):1875–85. 10.1016/j.neuroimage.2009.09.015 [DOI] [PubMed] [Google Scholar]
- 59.O'Hanlon E, Leemans A, Kelleher I, Clarke MC, Roddy S, Coughlan H, et al. White Matter Differences Among Adolescents Reporting Psychotic Experiences: A Population Based Diffusion Magnetic Resonance Imaging Study. JAMA Psychiatry. 2015;72(7):668–77. 10.1001/jamapsychiatry.2015.0137 [DOI] [PubMed] [Google Scholar]
- 60.Drakesmith M, Caeyenberghs K, Dutt A, Zammit S, Evans CJ, Reichenberg A, et al. Schizophrenia-like topological changes in the structural connectome of individuals with subclinical psychotic experiences. Hum Brain Mapp. 2015;36(7):2629–43. 10.1002/hbm.22796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Satterthwaite TD, Vandekar SN, Wolf DH, Bassett DS, Ruparel K, Shehzad Z, et al. Connectome-wide network analysis of youth with Psychosis-Spectrum symptoms. Mol Psychiatry. 2015;20(12):1508–15. 10.1038/mp.2015.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Satterthwaite TD, Wolf DH, Calkins ME, Vandekar SN, Erus G, Ruparel K, et al. Structural Brain Abnormalities in Youth With Psychosis Spectrum Symptoms. JAMA psychiatry. 2016;73(5):515–24. 10.1001/jamapsychiatry.2015.3463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wolf DH, Satterthwaite TD, Calkins ME, Ruparel K, Elliott MA, Hopson RD, et al. Functional neuroimaging abnormalities in youth with psychosis spectrum symptoms. JAMA Psychiatry. 2015;72(5):456–65. 10.1001/jamapsychiatry.2014.3169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Watson DR, Bai F, Barrett SL, Turkington A, Rushe TM, Mulholland CC, et al. Structural changes in the hippocampus and amygdala at first episode of psychosis. Brain Imaging Behav. 2012;6(1):49–60. 10.1007/s11682-011-9141-4 [DOI] [PubMed] [Google Scholar]
- 65.Qiu A, Gan SC, Wang Y, Sim K. Amygdala-hippocampal shape and cortical thickness abnormalities in first-episode schizophrenia and mania. Psychol Med. 2013;43(7):1353–63. 10.1017/S0033291712002218 [DOI] [PubMed] [Google Scholar]
- 66.Calvo A, Delvecchio G, Altamura AC, Soares JC, Brambilla P. Gray matter differences between affective and non-affective first episode psychosis: A review of Magnetic Resonance Imaging studies. J Affect Disord. 2018. [DOI] [PubMed] [Google Scholar]
- 67.Hoy K, Barrett S, Shannon C, Campbell C, Watson D, Rushe T, et al. Childhoo trauma and hippocampal and amygdalar volumes in first-episode psychosis. Schizophr Bull. 2012;38(6):1162–9. 10.1093/schbul/sbr085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Frodl T, O'Keane V. How does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humans. Neurobiol Dis. 2013;52:24–37. 10.1016/j.nbd.2012.03.012 [DOI] [PubMed] [Google Scholar]
- 69.Rao U, Chen LA, Bidesi AS, Shad MU, Thomas MA, Hammen CL. Hippocampal changes associated with early-life adversity and vulnerability to depression. Biol Psychiatry. 2010;67(4):357–64. 10.1016/j.biopsych.2009.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kaufman J, Plotsky PM, Nemeroff CB, Charney DS. Effects of early advers experiences on brain structure and function: clinical implications. Biol Psychiatry. 2000;48(8):778–90. 10.1016/s0006-3223(00)00998-7 [DOI] [PubMed] [Google Scholar]
- 71.Wolke D, Woods S, Stanford K, Schulz H. Bullying and victimization of primary school children in England and Germany: Prevalence and school factors. British journal of psychology. 2001;92(4):673–96. [DOI] [PubMed] [Google Scholar]
- 72.Nansel TR, Overpeck M, Pilla RS, Ruan WJ, Simons-Morton B, Scheidt P. Bullying behaviors among US youth: Prevalence and association with psychosocial adjustment. Jama. 2001;285 (16):2094–100. 10.1001/jama.285.16.2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not publicly available because of ethics and data protection consideration. This data contains potentially sensitive and identifying material as determined by Beaumont Hospital Medical Ethics Committee. Data can be requested via email from Beaumontethics@rcsi.ie.