Abstract
Wegener's Granulomatosis (WG) is an immunologically mediated rare multisystem disease characterized by necrotizing granulomatous inflammation affecting the upper and lower respiratory tracts, disseminated vasculitis and glomerulonephritis. WG oral lesions are reported to occur in 6%–13% of patients; they were an initial presenting feature in only 2% of cases. A case of strawberry gingivitis as the first sign of WG presented with erythematous and painful localized gingival enlargement affecting the maxillary anterior region of jaw in a 17-year-old boy is reported here. Correlation of histopathology with routine hematoxylin and eosin and special stains such as Grocott-Gomori's methenamine-silver nitrate and periodic acid–Schiff, peripheral blood smear, chest radiographs, Mantoux test and clinical presentation were established in diagnosing this rare entity. By the above-mentioned procedures, we arrived at the diagnosis of WG. The aim of reporting this case was to emphasize that, the dental surgeon often being the first person to examine the oral cavity, should be familiar with the typical appearance of gingiva as “strawberry gingivitis,” its clinical course, diagnostic parameters and adequate management of WG.
Keywords: Granulomatosis, strawberry gingivitis, Wegener's granulomatosis
INTRODUCTION
Wegener's granulomatosis is an uncommon multi-organ disease first categorized as a distinct syndrome by Friedrich Wegener in 1936.[1,2,3] Wegener's granulomatosis (WG) is an immunologically mediated rare multisystem disease characterized by necrotizing granulomatous inflammation affecting the upper and lower respiratory tracts, disseminated vasculitis and glomerulonephritis.[3,4,5,6] The limited form of Wegener's granulomatosis runs an indolent course, whereas the disseminated disease has a rapidly progressive course leading to life-threatening multiorgan failure.[7,8,9,10] Detailed explanation of WG is given by Godman and Churg.[7] In 1990, the American College of Rheumatology (ACR) proposed the following specific criteria for the classification of WG: (1) oral ulcers or nasal discharge or inflammation, (2) the presence of nodules, fixed infiltrates or cavities on a chest radiograph, (3) abnormal urinary sediment (red cell casts or more than five red blood cells per high power field) and (4) granulomatous inflammation on biopsy. For the diagnosis of WG, a minimum of two criteria should be fulfilled from the above-mentioned criteria.[7,11] Because the dental surgeon is often the first person to examine the oral cavity, should be familiar with the classical picture of gingival WG as “strawberry gingivitis,” its clinical course as well as diagnostic parameters and adequate treatment.
CASE REPORT
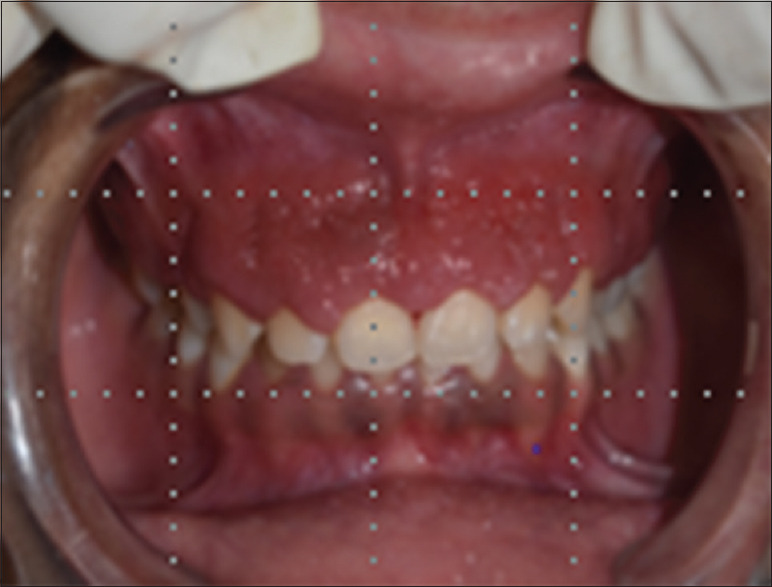
A 17-year-old male patient was referred to the Government Dental College, Aurangabad (Maharashtra), India in February 2018, with erythematous, painful and bleeding gums since last 8–9 months. Patient-reported to private dentist for painful and swollen gums 6 months back, they performed scaling and root planing, but signs did not get resolved; and hence, the patient reported to the institute. Clinical examination revealed localized gingival enlargement extending from the distal aspect of the right maxillary first premolar to the distal aspect of the left maxillary first premolar, with the appearance simulating “strawberry gingivitis” [Figure 1]. The gingiva was very friable and easily bled on touch. No other lesions were found elsewhere in the oral cavity. Panoramic radiographs did not show any evidence of underlying bony involvement and his medical history was otherwise unremarkable.
Figure 1.

Baseline
Histopathological findings
Follow-up after 1-month revealed only slight reduction in gingival enlargement [Figure 2] and hence, decision was made to perform incisional biopsy on gingival growth under local anesthesia [Figure 3]. The specimen obtained was submitted for routine tissue processing followed by routine staining with hematoxylin–eosin and special staining with periodic acid–Schiff (PAS), Grocott-Gomori methenamine-silver nitrate to rule out fungal infection.
Figure 2.
One-month after follow-up
Figure 3.

Incisional biopsy
Microscopic examination of the lesional tissue showed parakeratinized stratified squamous epithelium with pseudoepitheliomatous hyperplasia. In the underlying connective tissues, a granulomatous inflammatory response was observed. A diffuse mixed inflammatory cell infiltrate comprising mostly neutrophils and small numbers of eosinophils, plasma cells and lymphocytes were present. Scattered multinucleated giant cells with pronounced vasculitis were evident [Figures 4 and 5]. Special stains such as PAS, Grocott-Gomori methenamine-silver nitrate were negative for fungal infection.
Figure 4.
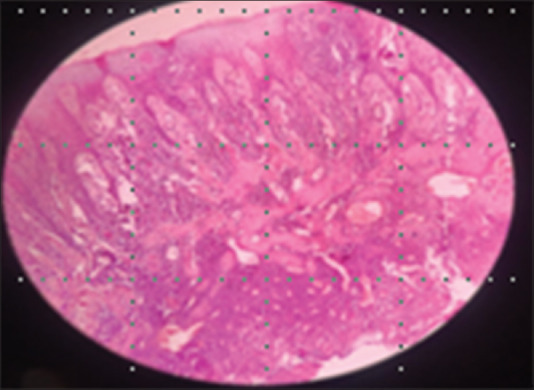
Histopathological picture showing pseudoepitheliomatous hyperplasia
Figure 5.
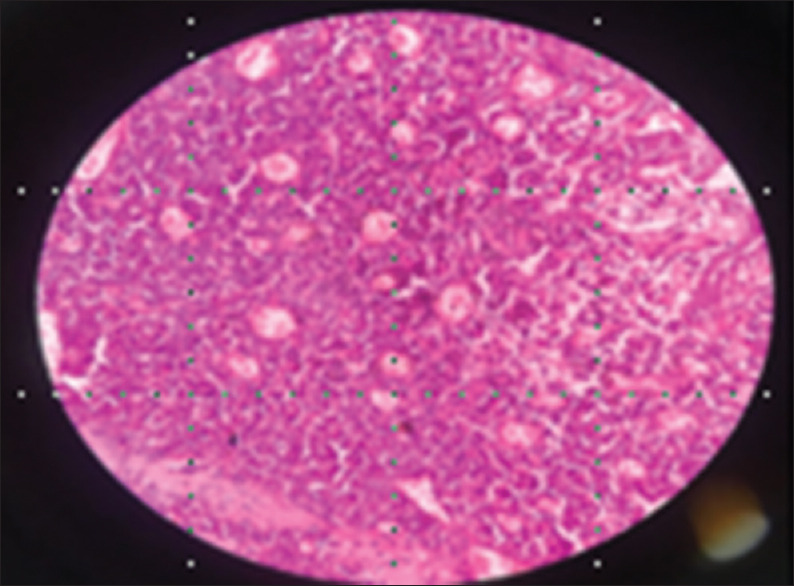
Histopathological picture showing vasculitis and granulomatous inflammation
Diagnosis
Based on the clinical presentation which simulating the appearance of “strawberry gingivitis,” histological examination revealing granulomatous inflammation in correlation with antineutrophil cytoplasmic autoantibody titer value, a diagnosis of WG was made.
Management
The patient was referred to the Medical Department for a systemic workout. Investigations yielded normal counts for hemoglobin, complete blood count, erythrocyte sedimentation rate and urine analysis. Chest radiographs were also normal, and Mantoux test was negative. Antineutrophil cytoplasmic autoantibody titer value 1:23 revealed positive results.
The treatment included prednisolone beginning at 20 mg/day that would be reduced rapidly over a set amount of time. The patient's gingival response was rapid, with improvement noted at 1 week and 3-week follow-up appointments [Figure 6]. The patient was followed for an additional 3 months and remained stable and free of lesions.
Figure 6.

Follow-up after 3 months
DISCUSSION
Wegener's granulomatosis is disease with multisystem involvement through oral presentation is very rare. Approximately 6%–13% of cases present with oral manifestations, that too in advanced stage of the disease and is rarely an indicator of the disease. Otorhinolaryngological involvement is more common with the destruction of nasal septum resulting in palatal perforation and progressive sensorineural hearing loss. Ophthalmic symptoms may manifest as epiphora due to involvement of nasolacrimal duct. Skin lesions manifests as purpura, nodules and ulcers and have been reported in 46% of affected patients in later course and 13% of affected patients at the onset of disease. However, limited forms of the disease have been reported in which only one or two organ systems have been involved.[7,11] The oral lesions may manifest either as mucosal ulcer on the tongue, buccal mucosa, gingiva and palate or as gingival hyperplasia with classical “strawberry gingivitis.” However, Cawson suggested that other lesions may also occur such as ulceration of the palate by extension from the nose, where destruction of the nasal septum may develop. It may also occur as small ulcers such as aphthae, diffuse ulcerative stomatitis and spontaneous exfoliation of the teeth.[7,11,12] Crohn's disease, sarcoidosis, deep fungal infection (candida, histoplasmosis and paracoccidioidomycosis), tuberculosis, other granulomatous infections such as midline lethal granuloma, midline natural killer/T-cell lymphomas, vasculitis, drug-induced gingival enlargement and rarely cicatricialpemphigoid or mucous membrane pemphigoid and leukemia should be included in the differential diagnosis of Wegener's granulomatosis.[7,11,12,13] In the reported case, a peripheral blood smear examination was performed, and leukemia was ruled out. The presence of multinucleated giant cells in the histopathology prompted for ruling out tuberculosis and deep fungal infection, hence Mantoux test was performed to rule out tuberculosis and special staining with Grocott-Gomori methenamine-silver nitrate and PAS were performed to rule out fungal infection.
In the case presented, the diagnosis of Wegener's granulomatosis was made according to criteria given by the American Association of Rheumatology, after careful exclusion of the above-mentioned lesions by appropriate systemic evaluation, laboratory investigation and referring the previous reported cases with similar clinical and histopathological reports. Our case also fulfilled two criteria of ACR 1990, including gingival ulceration which appeared such as “strawberry gingivitis” and granulomatous lesion in gingival biopsy. Most authors acknowledge that the clinicopathological complex of strawberry gingivitis and the accompanying histopathological features of pseudoepitheliomatous hyperplasia, microabscesses in connective tissue stroma, vasculitis and multinucleate giant cells are “highly suggestive” of Wegener's granulomatosis. It was also suggested that there was no association of the features of this complex with any other disease process and in an appropriate clinical setting they are so characteristic of gingival Wegener's granulomatosis.[10] The classical antineutrophil cytoplasmic antibodies titer, arguably the most useful investigation in cases of Wegener's granulomatosis was contributory in our case. Only few cases of Wegener's granulomatosis have been reported with classical presentation of “strawberry gingivitis” in literature.
WG has been treated unsuccessfully with antibiotics, chelating agents and local irradiation. Therapy with corticosteroids appears to have reduced inflammatory reactions and improved symptoms early in the disease but was of doubtful clinical significance when the disease progressed to significant renal and pulmonary involvement. In a study conducted at the National Institutes of Health, a regimen of cyclophosphamide (2 mg/kg body weight per day) with prednisone (1 mg/kg body weight) has been utilized to obtain complete remission in 93% of their patient population.
Histological evaluation of gingival biopsies from WG patients typically shows infiltrates of acute and chronic inflammatory cells, areas of microabscess, hemorrhage, multinucleated giant cells and pseudoepitheliomatous hyperplasia of the epithelium. Unfortunately, none of these findings are diagnostic for WG. However, the demonstration of neutrophil cytoplasmic autoantibodies in serum has shown great promise for the immunodiagnosis of WG.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Flethcher CDM, Unni K, Mertens K. Pathology and genetics of tumors of soft tissue and bone. Geneva: World Health Organization; 2002. [Google Scholar]
- 2.Lilly J, Juhlin T, Lew D, Vincent S, Lilly G. Wegener's granulomatosis presenting as oral lesions: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:153–7. doi: 10.1016/s1079-2104(98)90418-8. [DOI] [PubMed] [Google Scholar]
- 3.Ponniah I, Shaheen A, Shankar KA, Kumaran MG. Wegener's granulomatosis: The current understanding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:265–70. doi: 10.1016/j.tripleo.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt V, Hall TJ. Strawberry gingival enlargement as only manifestation of Wegener's granulomatosis. Br J Oral Maxillofac Surg. 2009;47:500. doi: 10.1016/j.bjoms.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Lourenço SV, Nico MM. Strawberry gingivitis: An isolated manifestation of Wegener's granulomatosis? Acta Derm Venereol. 2006;86:90–1. doi: 10.2340/00015555-0008. [DOI] [PubMed] [Google Scholar]
- 6.Ruokonen H, Helve T, Arola J, Hietanen J, Lindqvist C, Hagstrom J. “Strawberry like” gingivitis being the first sign of Wegener's granulomatosis. Eur J Intern Med. 2009;20:651–3. doi: 10.1016/j.ejim.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Godman GC, Churg J. Wegeners granulomatosis: pathology and review of the literature. AMA Arch Pathol. 1954;58:533–53. [PubMed] [Google Scholar]
- 8.Cohen RE, Cardoza TT, Drinnan AJ, Aguirre A, Neiders ME. Gingival manifestations of Wegener's granulomatosis. J Periodontol. 1990;61:705–9. doi: 10.1902/jop.1990.61.11.705. [DOI] [PubMed] [Google Scholar]
- 9.Eufinger H, Machtens E, Akuamoa-Boateng E. Oral manifestations of Wegener's granulomatosis. Review of the literature and report of a case. Int J Oral Maxillofac Surg. 1992;21:50–3. doi: 10.1016/s0901-5027(05)80454-0. [DOI] [PubMed] [Google Scholar]
- 10.Napier SS, Allen JA, Irwin CR, McCluskey DR. Strawberry gums: A clinicopathological manifestation diagnostic of Wegener's granulomatosis? J Clin Pathol. 1993;46:709–12. doi: 10.1136/jcp.46.8.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reboll-Ferrer RM, Zapater-Latorre E, Calabuig-Crespo C, Basterra-Alegría J. Wegener's granulomatosis: Description of a case with oral manifestation. Med Oral Patol Oral Cir Bucal. 2010;15:e601–4. doi: 10.4317/medoral.15.e601. [DOI] [PubMed] [Google Scholar]
- 12.Rajendran R, Sivapathsundharam B, editors. Shafer Textbook of Oral Pathology. 6th ed. Elsevier; 2009. pp. 670–1. [Google Scholar]
- 13.Kundu BK, Gadpayl AK. Gum hypertrophy a manifestation. J Indian Acad Clin Med. 2011;12:76–9. [Google Scholar]


