Abstract
Background:
Despite our sincere and serious efforts, oral cancer (particularly oral squamous cell carcinoma [OSCC]) is the major cause of morbidity and mortality in the Indian population. Oral precancerous lesions show quite high malignant transformation rate. Epidemiological data of oral epithelial dysplasia (OED) and OSCC could help in early diagnosis and thus may improve the prognosis. The current study aims to retrospectively analyze the epidemiological profile of patients with different grades of OED and OSCCs.
Materials and Methods:
The current study is a retrospective analysis of OED and OSCC reported in 5 years in our institution from 2014 to 2018. Data for the analysis were attained from the case sheets from the patients diagnosed with OED and OSCC.
Results:
The mean prevalence of OED and OSCC was 5.71% and 9.85%, respectively. Among the dysplastic lesions, severe dysplasia was more common, while well-differentiated squamous cell carcinoma was more common among the carcinomatous lesions. The peak age prevalence of both the lesions was third to fifth decade. Males were more frequently affected than females, with buccal mucosa being the most common site.
Conclusion:
The data attained from this study highlight the need for community-based screening and awareness programs for general population and thus obtain a healthier society.
Keywords: Age, gender, grades, location, oral epithelial dysplasia, oral squamous cell carcinoma
INTRODUCTION
Oral squamous cell carcinoma (OSCC) was defined by Pindborg et al., 1997 as “A malignant epithelial neoplasm exhibiting squamous differentiation as characterized by the formation of keratin and/or the presence of intercellular bridges.”[1] In Southeast Asia, OSCCs account for 40% of all cancers compared with approximately 4% in developed countries. Despite numerous advances in treatment, the 5-year survival has remained approximately 50% for the past 50 years.[2] This disappointing survival rate may be most probably attributable to diagnostic delay. The prevalence of oral cancer is highest in India as per the World Oral Health Report 2003. Oral cancer ranks number one among men and number three among women in India. Oral cancer constitutes 12% of all cancers in men and 8% of all cancers among women.[3]
Oral epithelial dysplasia (OED) is a potentially malignant lesion of the oral mucosa with an erratic sequence of succession,[4] where there is growth of immature cells, along with a simultaneous decrease in the number and location of mature cells.[4] The presence of epithelial dysplasia is generally considered as one of the most vital conjecturers of malignant transformation.[5] Warnakulasuriya conducted a meta-analysis and reported a malignant transformation rate of 10.5% among patients with histologically confirmed OED undergoing long-term follow-up.[6] The early and careful diagnosis is of extreme significance, which allows arresting the progression of OED to OSCC.
The current study is aimed to study the demographic variation and site predilection in patients reported with OED and OSCC in the North Indian population.
MATERIALS AND METHODS
All cases of OSCC and OED histopathologically diagnosed between 2014 and 2018 were reviewed from the archives of the Department of Oral and Maxillofacial Pathology of our institution. The following variables were recorded: gender, age and location and grades of OED and OSCC. The data were analyzed, and graphs were formulated, respectively. Grading of dysplasia was done according to the WHO 2005 classification, and grading of OSCC was done according to Broder et al.[7] The grading was re-evaluated by two pathologists independently, and the case of discrepancies was resolved by common consensus.
Inclusion and exclusion criteria
Patients with histopathologically confirmed cases of OED and OSCCs, which were reported in our institution from the period of 2014–2018, were included in the study. Patients who had a history of previous malignancy other than the oral cavity and recurrent cases of dysplasia and OSCCs were excluded from the study.
Data analysis
The overall prevalence in different grades of dysplasia and different grades of OSCCs was tabulated and recorded as mean percentage. Statistical evaluation was done for scale and ordinal variance using SPSS Version 21.0 Software (IBM Corporation, NY, United States). Age distribution, gender distribution and site predilection of different grades of dysplasia and OSCCs were statistically analyzed using the Chi-square test (P < 0.05).
RESULTS
Among 893 patients visiting the department between 2014 and 2018, 51 patients presented with OED and 88 patients presented with OSCC. The overall prevalence of OED was recorded as 5.71% and OSCC as 9.85%. In 2014, 22 patients were diagnosed with epithelial dysplasia and 55 were diagnosed with OSCC. In 2015, five patients were diagnosed with dysplasia and 18 were diagnosed with OSCC. In 2016, eight patients were diagnosed with epithelial dysplasia and 17 were diagnosed with OSCC. In 2017, eight patients were diagnosed with epithelial dysplasia and 19 were diagnosed with OSCC, whereas in 2018, 13 patients presented with dysplasia and 24 patients were diagnosed with OSCC. 27.5% of cases were graded as mild dysplasia, 21.6% of cases were graded as moderate dysplasia and 37.3% of cases were graded as severe dysplasia, whereas 13.6% of cases were graded as carcinoma in situ. Out of the total cases, 43.2% of cases were found to be welldifferentiated squamous cell carcinoma, 23.2% of cases were found to be moderately differentiated OSCC and 23.9% of cases were found to be poorly differentiated OSCC. A total of 6.8% of cases were diagnosed as early invasive squamous cell carcinoma. Figures 1 and 2 show the overall prevalence of different grades of OED and OSCC, respectively.
Figure 1.
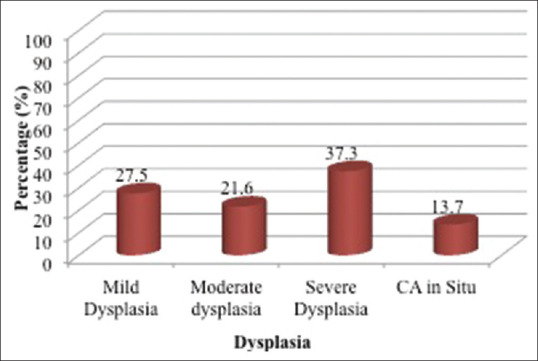
Overall prevalence of oral epithelial dysplasia
Figure 2.
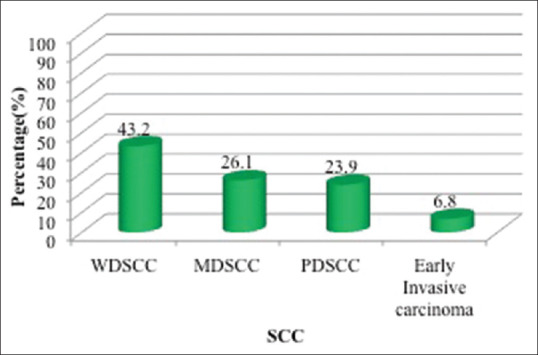
Overall prevalence of oral squamous cell carcinoma
Figure 3 illustrates the comparison of the types of OED according to the age. The peak prevalence was seen in the third to fifth decade in mild, moderate and severe dysplasia. The maximum number of cases of carcinoma in situ was seen in >56 years of age. The second most prevalent age group was fifth to sixth decade with four cases of severe dysplasia, three cases of moderate dysplasia and two cases of mild dysplasia. The younger age group (<30 years of age) had four cases of severe dysplasia, two cases of moderate dysplasia and one case of mild dysplasia and no cases of carcinoma in situ. However, there was no statistically significant difference among different age groups.
Figure 3.
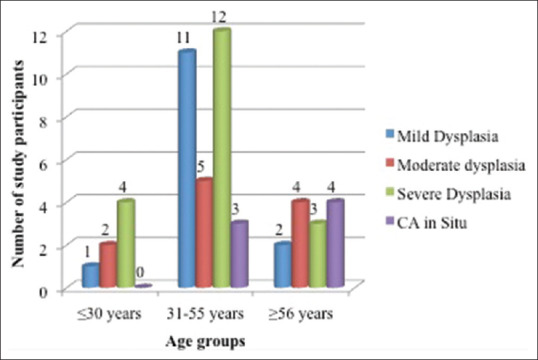
Distribution of oral epithelial dysplasia according to age
Figure 4 illustrates the comparison of the different grades of OED according to gender; male preponderance is seen in different grades of dysplasia and carcinoma in situ. There was no statistically significant difference between both genders.
Figure 4.
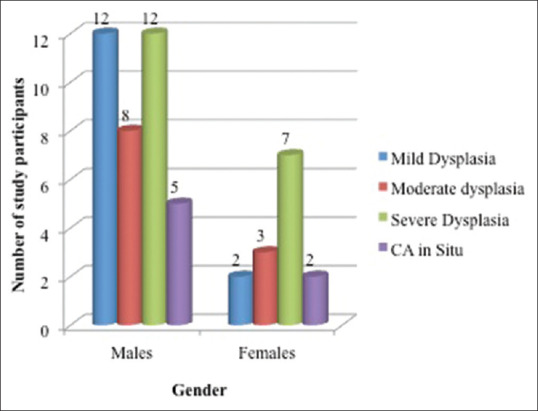
Comparison of the grades of oral epithelial dysplasia according to the gender
Figure 5 illustrates the comparison of the different grades of OSCC according to the age. Nineteen patients aged 31–55 years, 16 patients aged ≥56 years and 3 patients aged ≤30 years presented with well-differentiated squamous cell carcinoma. Ten patients in the middle age group (third to fifth decade), 11 cases aged ≥56 years and 2 cases aged ≤30 years presented with moderately differentiated squamous cell carcinoma. Eighteen cases in the range of third to fifth decade, 3 cases in the older age group (≥56 years) and no patients in the younger age group (≤30 years of age) presented with poorly differentiated squamous cell carcinoma. In case of early invasive squamous cell carcinoma, a maximum number of patients were seen in the age range of 31–55 years. Only one case was seen in the age range of ≥56 years, while no case was seen in ≤30 years of age. There was no statistically significant difference found among different age groups.
Figure 5.
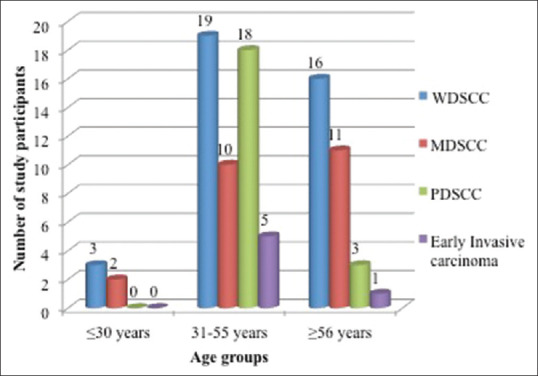
Comparison of the grades of oral squamous cell carcinoma according to age
Figure 6 illustrates the comparison of the different grades of OSCC according to gender; male predilection was noteworthy in all the different grades of OSCC. Thirty-three male patients and five female patients were diagnosed with well-differentiated OSCC. Nineteen male patients and four female patients were diagnosed with moderately differentiated OSCC. Sixteen male and five female patients were diagnosed with poorly differentiated OSCC, whereas five males and one female were diagnosed with early invasive squamous cell carcinoma. There was no statistically significant difference between both genders.
Figure 6.
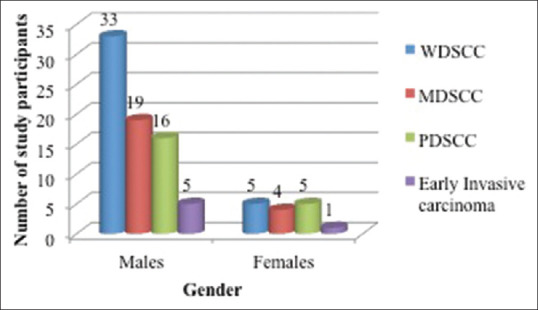
Comparison of the different grades of oral squamous cell carcinoma according to gender
Figure 7 illustrates the presentation of the different grades of dysplasia according to the location. Majority of the patients presented with lesion in the buccal mucosa, followed by alveobuccal complex, tongue and retromolar area retrospectively. One case each was presented in gingiva and labial mucosa.
Figure 7.
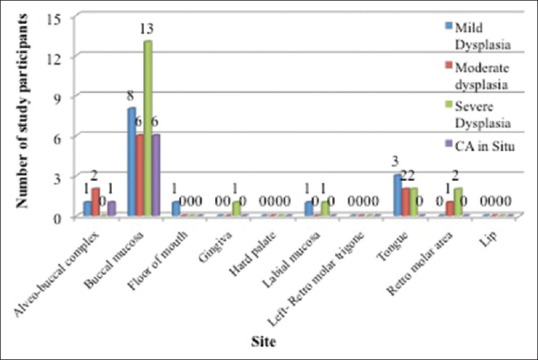
Presentation of grades of oral epithelial dysplasia according to the location
Figure 8 demonstrates the presentation of the different grades of OSCC according to the location. Buccal mucosa was the predominant site for all grades of OSCC, followed by alveobuccal complex. The floor of the mouth was the predominant site for poorly differentiated OSCC (two cases). A total of five cases were located on the tongue, two each of welldifferentiated OSCC and poorly differentiated OSCC and one case of moderately differentiated OSCC. One case of moderately differentiated OSCC each was presented in gingiva, hard palate, labial mucosa and retromolar trigone.
Figure 8.
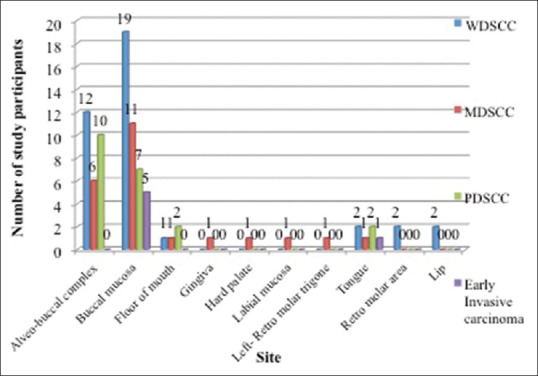
Presentation of grades of oral squamous cell carcinoma according to the location
DISCUSSION
Oral cancers have a multifaceted etiology.[6] A plethora of lifestyle and environmental factors has been identified as the risk factor for oral cancers. In view of the relatively common presentation, delay in diagnosis is also frequent which could be correlated to patient delay, professional delay or both. Thus, thorough information of the diverse presentation and an experienced eye can go a long way in preventing the high morbidity and mortality associated with oral cancers.[8] A pertinent issue for consideration is rich lymphatic supply of the oral cavity, which results in many cases being detected first in the advanced stage itself.[9]
The mean prevalence of OED in our study was 5.71%, which was consistent with the study done by Hsue et al.[10] (8.85%) and in contrast with Pereira Jdos et al.,[11] Hosagadde et al.[12] and Roy and Varshney.[13] The probable reason for this discrepancy could be attributed to geographical variation and the associated tobacco usage in the North Indian population.
The peak prevalence of age in all the grades of dysplasia was found to be in the third to fifth decade. Majority of the studies found a similar result except the study done by Mincer et al.[14] whose peak prevalence was a bit higher (sixth to seventh decade).
Male preponderance was seen in our study. Almost all the studies were consistent with our finding, whereas Pereira Jdos et al.[11] showed a female preponderance. The most common site in all the grades was buccal mucosa. Similar findings were seen by Hsue et al.[10] and Jaber et al.[15] Arduino et al.[16] revealed the lateral border of the tongue, Pereira Jdos et al.[11] revealed the alveolar ridge, Lumerman et al.[17] revealed the floor of the mouth and Mincer et al.[14] revealed the lower lip to be the most prevalent site.
Severe dysplasia (37.3%) was seen more than mild (27.5%) and moderate (21.6%) dysplasia in our study. Carcinoma in situ showed the least prevalence of 13.7%. Lumerman et al.[17] reported mild dysplasia as the more prevalent grade than severe and moderate dysplasia, with carcinoma in situ being the least (3.9%). All other studies showed more prevalence of mild dysplasia as compared to severe dysplasia.[10,11,15,16,17] The probable reason could be late presentation of the disease due to patients' unawareness of symptoms and lack of concern for the disease.
The prevalence of OSCC in the present study was 9.85%, whereas the lower prevalence was seen in previous studies.[18,19] Other studies have shown regional disparities in different regions of India, with West Bengal reporting the highest[20] incidence of OSCC whereas Kerala reporting the lowest.[21]
The peak age range of OSCC in our study was reported to be in the third to fifth decade. Majority of the studies are consistent with our finding.[9,22,23,24,25,26,27,28,29,30,31] Few of the studies have reported a slightly higher age predilection.[32] All the grades of OSCC showed male prevalence in our study, which was consistent with almost all the other database studies done in the past.[22,23,24,25,26,27,28,29,30,31,32]
The most prevalent site in all the grades of OSCC was buccal mucosa, which is similar to studies done by Singh et al.,[22] Abdulla et al.,[23] Tandon et al.,[25] Kumar et al.,[26] Sharma et al.[30] and Ajay et al.[19] Other studies showed gingivobuccal sulcus,[24] mandibular alveolus[9,32] and tongue[31] as the most common sites.
Well-differentiated OSCC being the most common grade of OSCC showed a mean percentage of 43.2%, which was in concordance with the studies done by Smitha et al.,[24] Shenoi et al.,[9] Kumar et al.[26] and Salian et al.[28] Moderately differentiated OSCC showed a mean prevalence of 26.1% with poorly differentiated OSCC and early invasive OSCC showing a prevalence rate of 23.9% and 6.8%, respectively. Only one study showed more prevalence of moderately differentiated OSCC.[23]
CONCLUSION
OSCC is a major social burden in our nation. We need more stringent policies to combat the exponential rise in the number of these patients. Early diagnosis paves way for a better prognosis, thus improving the lifestyle of these individuals. A collaborative attempt of a large database study will enable us to formulate better therapeutic strategies. Further, cross-sectional study with larger sample size with a multi-centric approach is required to detect and treat oral cancer in its initial stage and hence aid in reducing the morbidity and mortality associated with it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pindborg J, Reichart P, Smith C, Waal I. Histological Typing of Cancer and Precancer of the Oral Mucosa WHO International Histological Classification of Tumors. 2nd ed. Springer: 1997. doi: 101007/978-3-642-60592-5. [Google Scholar]
- 2.Oral Cancer 5-Year Survival Rate by Race, Gender, and Stage of Diagnosis. NIDCR. [Last accessed on 2020 Feb 28]. Available from: https://www.nidcr.nih.gov/research/data-statistics/oral-cancer/survival-rates .
- 3.Sankaranarayanan R. Oral cancer in India: An epidemiologic and clinical review. Oral Surg Oral Med Oral Pathol. 1990;69:325–30. doi: 10.1016/0030-4220(90)90294-3. [DOI] [PubMed] [Google Scholar]
- 4.Jack H, Lee K, Polonowita A. Dilemmas in managing oral dysplasia: A case report and literature review. N Z Med J. 2009;122:89–98. [PubMed] [Google Scholar]
- 5.Nagao T, Ikeda N, Fukano H, Hashimoto S, Shimozato H, Warnakulasuriya S. Incidence rates for oral leukoplakia and lichen planus in a Japanese population. J Oral Pathol Med. 2005;34:5329. doi: 10.1111/j.1600-0714.2005.00349.x. [DOI] [PubMed] [Google Scholar]
- 6.Warnakulasuriya S. Causes of oral cancer – An appraisal of controversies. Br Dent J. 2009;207:471–5. doi: 10.1038/sj.bdj.2009.1009. [DOI] [PubMed] [Google Scholar]
- 7.Broders AC. The microscopic grading of cancer. Surg Clin North Am. 1941;21:947–62. [Google Scholar]
- 8.Morelatto RA, Herrera MC, Fernández EN, Corball AG, López de Blanc SA. Diagnostic delay of oral squamous cell carcinoma in two diagnosis centers in Córdoba Argentina. J Oral Pathol Med. 2007;36:405–8. doi: 10.1111/j.1600-0714.2007.00547.x. [DOI] [PubMed] [Google Scholar]
- 9.Shenoi R, Devrukhkar V, Chaudhuri, Sharma BK, Sapre SB, Chikhale A. Demographic and clinical profile of Oral squamous cell carcinoma patients: A retrospective study. Indian J Cancer. 2012;49:21–6. doi: 10.4103/0019-509X.98910. [DOI] [PubMed] [Google Scholar]
- 10.Hsue SS, Wang WC, Chen CH, Lin CC, Chen YK, Lin LM. Malignant transformation in 1458 patients with potentially malignant oral mucosal disorders: A follow-up study based in a Taiwanese hospital. J Oral Pathol Med. 2007;36:25–9. doi: 10.1111/j.1600-0714.2006.00491.x. [DOI] [PubMed] [Google Scholar]
- 11.Pereira Jdos S, Carvalho Mde V, Henriques AC, de Queiroz Camara TH, Miguel MC, Freitas Rde A. Epidemiology and correlation of the clinicopathological features in oral epithelial dysplasia: analysis of 173 cases. Ann Diagn Pathol. 2011;15:98–102. doi: 10.1016/j.anndiagpath.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Hosagadde S, Dabholkar J, Virmani N. A clinicopathological study of oral potentially malignant disorders. J Head Neck Physicians Surg. 2016;4:29–34. [Google Scholar]
- 13.Roy S, Varshney S. Oral dermatological conditions: A clinical study. Indian J Otolaryngol Head Neck Surg. 2013;65:97–101. doi: 10.1007/s12070-011-0347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mincer HH, Coleman SA, Hopkins KP, Tenn M. Observations of the clinical characterstics showing histological epithelial dysplasia. Oral Surg. 1972;33:390–4. doi: 10.1016/0030-4220(72)90468-9. [DOI] [PubMed] [Google Scholar]
- 15.Jaber MA, Porter SR, Speight P, Eveson JW, Scully C. Oral epithelial dysplasia: Clinical characteristics of western European residents. Oral Oncol. 2003;39:589–96. doi: 10.1016/s1368-8375(03)00045-9. [DOI] [PubMed] [Google Scholar]
- 16.Arduino PG, Surace A, Carbone M, Elia A, Massolini G, Gandolfo S, et al. Outcome of oral dysplasia: A retrospective hospital-based study of 207 patients with a long follow-up. J Oral Pathol Med. 2009;38:540–4. doi: 10.1111/j.1600-0714.2009.00782.x. [DOI] [PubMed] [Google Scholar]
- 17.Lumerman H, Freedman P, Kerpel S. Oral epithelial dysplasia and the development of invasive squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:321–9. doi: 10.1016/s1079-2104(05)80226-4. [DOI] [PubMed] [Google Scholar]
- 18.Sawlani K, Kumari N, Mishra AK, Agrawal U. Oral cancer prevalence in a tertiary care hospital in India. J Fam Med Community Health 2014. 2014;1:1022. [Google Scholar]
- 19.Ajay PR, Ashwinirani SR, Nayak A, Suragimath G, Kamala KA, Sande A, et al. Oral cancer prevalence in Western population of Maharashtra, India, for a period of 5 years. J Oral Res Rev. 2018;10:11–4. [Google Scholar]
- 20.Karmakar R, Bandyopadhyay A, Barui G, Maiti PK, Bhattacharya A, Choudhuri MK. Pattern of cancer occurrence in rural population of West Bengal – A hospital-based study. J Indian Med Assoc. 2010;108:505–6, 508. [PubMed] [Google Scholar]
- 21.Elango JK, Gangadharan P, Sumithra S, Kuriakose MA. Trends of head and neck cancers in urban and rural India. Asian Pac J Cancer Prev. 2006;7:108–12. [PubMed] [Google Scholar]
- 22.Singh MP, Kumar V, Agarwal A, Kumar R, Bhatt ML, Misra S. Clinico-epidemiological study of oral squamous cell carcinoma: A tertiary care centre study in North India. J Oral Biol Craniofac Res. 2016;6:31–4. doi: 10.1016/j.jobcr.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdulla R, Adyanthaya S, Kini P, Mohanty V, D'Souza N, Subbannayya Y. Clinicopathological analysis of oral squamous cell carcinoma among the younger age group in coastal Karnataka, India: A retrospective study. J Oral Maxillofac Pathol. 2018;22:180–7. doi: 10.4103/jomfp.JOMFP_16_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smitha T, Mohan CV, Hemavathy S. Clinicopathological features of oral squamous cell carcinoma: A hospital based retrospective study. J NTR Univ Health Sci. 2017;6:29–34. [Google Scholar]
- 25.Tandon A, Bordoloi B, Jaiswal R, Srivastava A, Singh RB, Shafique U. Demographic and clinicopathological profile of oral squamous cell carcinoma patients of North India: A retrospective institutional study. SRM J Res Dent Sci. 2018;9:114–8. [Google Scholar]
- 26.Kumar GK, Abidullah M, Elbadawi L, Dakhil S, Mawardi H. Epidemiological profile and clinical characteristics of oral potentially malignant disorders and oral squamous cell carcinoma: A pilot study in Bidar and Gulbarga Districts, Karnataka, India. J Oral Maxillofac Pathol. 2019;23:90–6. doi: 10.4103/jomfp.JOMFP_116_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krishna A, Singh RK, Singh S, Verma P, Pal US, Tiwari S. Demographic risk factors, affected anatomical sites and clinicopathological profile for oral squamous cell carcinoma in a North Indian population. Asian Pac J Cancer Prev. 2014;15:6755–60. doi: 10.7314/apjcp.2014.15.16.6755. [DOI] [PubMed] [Google Scholar]
- 28.Salian V, Dinakar C, Shetty P, Ajila V. Etiological trends in oral squamous cell carcinoma: A retrospective institutional study. Cancer Transl Med. 2016;2:33–6. [Google Scholar]
- 29.Sharma RG, Bang B, Verma H, Mehta JM. Profile of oral squamous cell cancer in a tertiary level medical college hospital: A 10 yr study. Indian J Surg Oncol. 2012;3:250–4. doi: 10.1007/s13193-012-0165-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma P, Saxena S, Aggarwal P. Trends in the epidemiology of oral squamous cell carcinoma in Western UP: An institutional study. Indian J Dent Res. 2010;21:316–9. doi: 10.4103/0970-9290.70782. [DOI] [PubMed] [Google Scholar]
- 31.Addala L, Pentapati CK, Reddy Thavanati PK, Anjaneyulu V, Sadhnani MD. Risk factor profiles of head and neck cancer patients of Andhra Pradesh, India. Indian J Cancer. 2012;49:215–9. doi: 10.4103/0019-509X.102865. [DOI] [PubMed] [Google Scholar]
- 32.Rahman SS, Sarkar MK, Khan MH, Biswas SS, Saha MM. Clinical profile of oral squamous cell carcinoma patients attending a tertiary care hospital. Bang Med J Khulna. 2014;47:3–6. [Google Scholar]


