Novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) lies behind the ongoing outbreak of coronavirus disease 2019 (COVID-19). There is a growing understanding of SARS-CoV-2 in virology, epidemiology, and clinical management strategies. However, no anti-SARS-CoV-2 drug or vaccine has been officially approved due to the absence of adequate evidence. Scientists are racing to develop a treatment for COVID-19. Recent studies have revealed many attractive therapeutic options, even if some of them remain to be further confirmed in rigorous preclinical models and clinical trials.
KEYWORDS: COVID-19, SARS-CoV-2, antiviral drugs, treatment, vaccines
ABSTRACT
Novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) lies behind the ongoing outbreak of coronavirus disease 2019 (COVID-19). There is a growing understanding of SARS-CoV-2 in virology, epidemiology, and clinical management strategies. However, no anti-SARS-CoV-2 drug or vaccine has been officially approved due to the absence of adequate evidence. Scientists are racing to develop a treatment for COVID-19. Recent studies have revealed many attractive therapeutic options, even if some of them remain to be further confirmed in rigorous preclinical models and clinical trials. In this minireview, we aim to summarize the updated potential approaches against SARS-CoV-2. We emphasize that further efforts are warranted to develop the safest and most effective approach.
INTRODUCTION
Since December 2019, coronavirus disease 2019 (COVID-19) has been spreading around the world, with over 130,000 confirmed cases (as of 13 March 2020) (1, 2). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel betacoronavirus, is the causative agent of this global health threat (3). Like other coronavirus strains, SARS-CoV-2 is characterized by a spherical morphology with spike projections on the surface. It was demonstrated that SARS-CoV-2 shared high sequence identity with SARS-CoV and bat SARS-like coronavirus (SL-CoV) (4). Notably, SARS-CoV-2 has lower pathogenicity than SARS-CoV but higher transmissibility from human to human (5). Cell entry is the first step of cross-species transmission. SARS-CoV-2 is more likely to infect lung type II alveolar cells, which may explain the severe alveolar damage after infection (6).
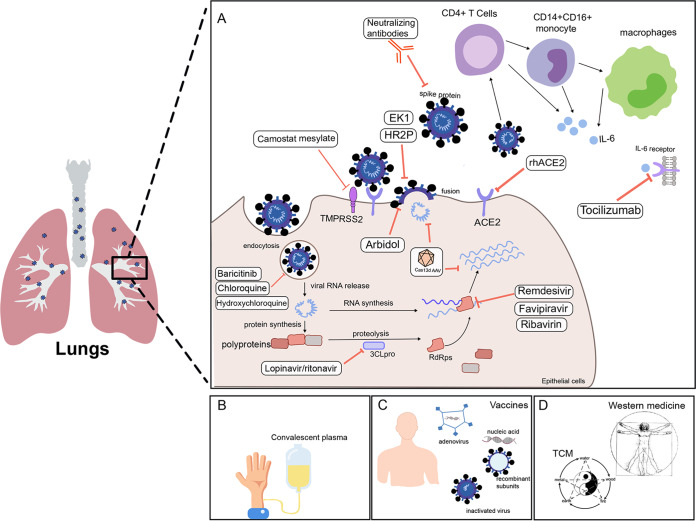
The rapid spread of COVID-19 has resulted in an urgent requirement for effective therapeutic strategies against SARS-CoV-2. Initially, without licensed vaccines or approved antiviral drugs, COVID-19 treatment was mainly based on the experience of clinicians. The newest guideline published by National Health Commission (NHC) of the People's Republic of China recommends alpha interferon (IFN-α), lopinavir/ritonavir, ribavirin, chloroquine phosphate, and arbidol as antiviral therapy (7). To date, many potential approaches have been revealed based on the progress of SARS-CoV-2 research, including inhibition of SARS-CoV-2 fusion/entry, disruption of SARS-CoV-2 replication, suppression of excessive inflammatory response, convalescent plasma (CP) treatment, and the use of vaccines as well as the combination of traditional Chinese medicine (TCM) and Western medicine (as summarized in Fig. 1). Additionally, a number of clinical trials are in progress to test the safety and effectiveness of candidate drugs. In this review, we summarize the current knowledge on the potential treatment against SARS-CoV-2 based on the emerging basic and clinical data.
FIG 1.
Updated potential approaches against SARS-CoV-2. (A) Dampening of SARS-CoV-2 fusion/entry; disruption of SARS-CoV-2 replication; inhibition of excessive inflammatory response. (B) Convalescent plasma treatment. (C) Vaccines. (D) Combinations of traditional Chinese and Western medicine. ACE2, angiotensin-converting enzyme 2; rhACE2, recombinant human ACE2; HR2P, heptad repeat 2-derived peptides; EK1, a modified OC43-HR2P peptide; 3CLpro, 3C-like protease; RdRps, RNA-dependent RNA polymerases; AAV, adeno-associated virus; IL-6, interleukin-6; TCM, traditional Chinese medicine.
UPDATED ATTRACTIVE APPROACHES AGAINST SARS-CoV-2
Inhibition of SARS-CoV-2 fusion/entry.
Similarly to SARS-CoV, SARS-CoV-2 uses spike (S) protein to gain entry into host cells (8). It was shown that the S protein on the surface of SARS-CoV-2 cell bound the entry receptor angiotensin-converting enzyme 2 (ACE2) on infected cells (9). SARS-CoV-2 was predicted to recognize human ACE2 more efficiently than SARS-CoV (10). Thus, targeting the interactions between ACE2 and S protein may be a potential approach. Specifically, a receptor binding domain (RBD) within the S protein is the critical target for neutralizing antibodies. Since SARS-CoV-2 S protein displayed high homology to that of SARS-CoV, the available neutralizing antibody of SARS-CoV CR3022 was found to bind potently with SARS-CoV-2 RBD (4). Nevertheless, Zheng and Song recently reported that more than 85% of the RBD antibody epitopes in SARS-CoV-2 showed remarkable alterations compared with SARS-CoV, indicating the necessity to develop new monoclonal antibodies for SARS-CoV-2 (11). In addition, the rationale for the choice of the ACE2 receptor as a specific target has been reviewed elsewhere (12, 13). Notably, an open-label, randomized, controlled, pilot clinical trial is in progress, further investigating the effect of recombinant human ACE2 (rhACE2; GSK2586881) in patients with severe COVID-19 (ClinicalTrials registration no. NCT04287686). It was suggested that S protein-derived cell entry depended on not only ACE2 but also on the host cellular serine protease TMPRSS2 (14). Camostat mesylate, a clinically proven inhibitor of TMPRSS2, significantly reduced lung cell line infection with SARS-CoV-2 and could be considered for COVID-19 treatment (14). In addition, heptad repeat 1 (HR1) and heptad repeat 2 (HR2) on SARS-CoV-2 involved viral and cell membrane fusion (15). Xia et al. reported that HR2-derived peptides (HR2P) and EK1 (a modified OC43-HR2P peptide) exhibited effective fusion inhibitory activity toward SARS-CoV-2 and would act as fusion/entry inhibitors to treat SARS-CoV-2 infection. Further studies are warranted to substantiate these concepts.
Moreover, it was suggested that coronavirus entry also involved pH- and receptor-dependent endocytosis (16, 17). Targeting endocytosis may be another option for fighting SARS-CoV-2. AP-2-associated protein kinase 1 (AAK1) is a host kinase that regulates clathrin-mediated endocytosis (18). A group of approved drugs targeting AAK1 were searched out based on artificial intelligence (AI) technology (19). Among them, the Janus kinase inhibitor baricitinib, an AAK1-binding drug, was expected to be a suitable candidate drug for COVID-19 because the standard treatment doses of baricitinib were sufficient to inhibit AAK1 (19).
Arbidol and chloroquine phosphate have been added to the list of potential treatment options in the NHC guideline for COVID-19 treatment (7). Arbidol was shown to inhibit multiple enveloped viruses by inhibiting virus entry/fusion of viral membranes with cellular membranes (20). Chloroquine, a traditional antimalarial drug, was shown to be effective against SARS-CoV-2 infection in vitro (21). Several clinical trials are in progress to test the efficacy and safety of chloroquine phosphate against COVID-19 (22). Results from more than 100 patients provided the first evidence that chloroquine phosphate was more effective in inhibiting the exacerbation of pneumonia than control treatment (22). Additionally, Yao et al. found that hydroxychloroquine (50% effective concentration [EC50] = 0.72 μM) was more potent with respect to inhibiting SARS-CoV-2 than chloroquine (EC50 = 5.47 μM) in vitro (23). Most importantly, the molecular mechanism of chloroquine phosphate in the treatment of COVID-19 remains elusive. It has been reported that chloroquine could impair endosome-mediated viral entry or the late stages of viral replication (24). More efforts are needed to pin down the exact mechanism.
Disruption of SARS-CoV-2 replication.
Many antiviral agents have been developed against viral proteases, polymerases, MTases, and entry proteins. Clinical trials are currently in progress to test a number of antiviral drugs, such as remdesivir (ClinicalTrials registration no. NCT04252664 and NCT04257656), favipiravir (Chinese Clinical Trial registration no. ChiCTR2000029600 and ChiCTR2000029544), ASC09 (ChiCTR2000029603), lopinavir/ritonavir (ChiCTR2000029387, ChiCTR2000029468, and ChiCTR2000029539), and arbidol (ChiCTR2000029621). Martinez reported that the most promising antiviral for fighting SARS-CoV-2 was remdesivir (25). Remdesivir is a monophosphoramidate prodrug of an adenosine analog. Its active form can incorporate into nascent viral RNA by the activity of RNA-dependent RNA polymerases (RdRps), which then causes RNA synthesis arrest (26). Wang et al. demonstrated that remdesivir effectively inhibited SARS-CoV-2 in vitro (21). The clinical condition of the patient with the first case of COVID-19 confirmed in the United States improved following intravenous remdesivir administration (27). Similarly, favipiravir and ribavirin are monophosphoramidate prodrugs of guanine analogues and have been approved for treatment of infections by some other viruses (28). However, their antiviral effect in patients with COVID-19 needs rigorous data to support their use. Lopinavir and ritonavir are protease inhibitors targeting the coronavirus main proteinase (3C-like protease; 3CLpro). 3CLpro is responsible for processing the polypeptide translation product from the genomic RNA into the protein components (29). High-throughput screening was also used to screen small-molecule drugs targeting the viral main protease in clinical drug libraries (30). Four molecules, including prulifloxacin, tegobuvir, bictegravir, and nelfinavir, showed reasonable binding conformations with the viral main protease (30).
Targeting the RNA genome of SARS-CoV-2 may be another approach. Nguyen et al. showed the application of the novel CRISPR/Cas13 RNA knockdown system in cleaving the SARS-CoV-2 RNA genome (31). This CRISPR/Cas13d system was composed of a Cas13d protein and guide RNA-containing spacer sequences specifically complementary to the virus RNA genome. It was suggested that the Cas13d effector could be delivered via an adeno-associated virus (AAV) to the lung infected with SARS-CoV-2 (31).
Suppression of excessive inflammatory response.
A coordinated cytokine response is essential for the host immune response. However, a dysregulated response leads to a hyperinflammatory condition in some patients infected with SARS-CoV-2. It was reported that patients in intensive care units (ICUs) had higher concentration of cytokines in plasma than non-ICU patients with COVID-19, suggesting that the cytokine storm was associated with disease severity (32). Besides, higher percentages of granulocyte-macrophage colony-stimulating factor-positive (GM-CSF+) and interleukin-6-positive (IL-6+) CD4+ T cells were isolated from ICU patients infected with SARS-CoV-2 than from non-ICU patients (33). In view of this, inhibition of excessive inflammatory response may represent an adjunct therapy for COVID-19. Nevertheless, the therapeutic use of corticosteroids, which has shown excellent pharmacological effects with respect to suppressing exuberant and dysfunctional systematic inflammation, is still controversial (25, 32). The current NHC guideline emphasizes that the routine use of systematic corticosteroids is not recommended unless indicated for another reason. In line, there were no available data showing that patients benefited from corticosteroid treatment in SARS-CoV or Middle East respiratory syndrome coronavirus (MERS-CoV) infection, which might be attributable to the suppression of immune response against virus (34). Notably, a recent retrospective study showed the potential benefits accruing from low-dose corticosteroid treatment in a subset of critically ill patients with SARS-CoV-2 (35). More studies are needed to find out how and when to use corticosteroids properly.
At the cellular level, Zhou et al. demonstrated that CD4+ T cells were rapidly activated to produce GM-CSF and other inflammatory cytokines after SARS-CoV-2 infection, which further induced CD14+ CD16+ monocyte activation with high levels of expression of interleukin 6 (IL-6) (33). Thus, blocking GM-CSF or IL-6 receptor would potentially reduce immunopathology caused by SARS-CoV-2. In line, a multicenter, randomized, controlled clinical trial is under way to examine the efficacy and safety of tocilizumab (an IL-6 receptor-specific antibody) in patients with COVID-19 (Chinese Clinical Trial registration no. ChiCTR2000029765). Moreover, Fu et al. mentioned possible mechanisms of SARS-CoV-2-mediated inflammatory responses in which the neutralizing antibodies triggered Fc receptor (FcR)-mediated inflammatory responses and acute lung injury (36). Various options to block FcR activation might reduce SARS-CoV-2-induced inflammatory responses (36).
Convalescent plasma treatment.
With infections for which there is no specific therapy available, therapy with convalescent plasma (CP) has been proposed as a principal treatment (37). The CP is obtained from a donor who has recovered from infection by developing humoral immunity against the SARS-CoV-2 (38). The protective and therapeutic benefit of CP was attributed to the possible source of specific antibodies of human origin (39). However, evaluation of the efficacy of CP treatment is still difficult because of the lack of high-quality randomized clinical trials and of knowledge of the precise mechanism of action of plasma therapy. According to the NHC guideline, the CP of recovered patients is mainly used for patients in rapid disease progression or in a severe or critical condition (40). Several clinical trials investigating the efficacy and safety of convalescent plasma transfusion in patients with COVID-19 are in progress (Chinese Clinical Trial registration no. ChiCTR2000030010, ChiCTR2000030179, and ChiCTR2000030381).
Vaccines.
With the global spread of SARS-CoV-2, vaccination must be the most efficient and cost-effective means to prevent and control COVID-19 (41). Robust research efforts are under way to facilitate the development of vaccines against SARS-CoV-2. Specifically, the S protein of SARS-CoV-2 remains a key target for vaccine development. Recently, Wrapp et al. reported and shared the cryo-electron microscopy (cryo-EM) structure of SARS-CoV-2 S trimer, which enabled additional protein engineering efforts and speeded up the process of vaccine development (42). In addition, Lucchese searched the pentapeptides unique to SARS-CoV-2 by comparing the viral and the human proteomes and found that 107 human-foreign pentapeptides were embedded in S protein (43). Further, these S protein pentapeptides yielded 66 candidate epitopes for vaccine development (43). Moreover, since there were few available immunological studies related to SARS-CoV-2, Ahmed et al. screened the SARS-CoV-derived epitopes due to its high level of genetic similarity with SARS-CoV-2 (44). A screened set of SARS-CoV-derived B cell and T cell epitopes that mapped identically to SARS-CoV-2 proteins were identified, which would help the initial phase of vaccine development (44).
More than 15 potential vaccine candidates for treatment of COVID-19 infection are being developed around the world, including inactivated vaccine, recombinant subunits vaccine, nucleic acid-based vaccine, adenoviral vector vaccine, recombinant influenza viral vector vaccine, etc. (45). On 23 January 2020, the Coalition for Epidemic Preparedness Innovations (CEPI) announced the finding on DNA, mRNA, and “molecular clamp” vaccine platforms (46). There was no existing literature on SARS-CoV-2 vaccine trials as of 13 March 2020. The safety of vaccine remains a top priority for vaccine development.
Combination of traditional Chinese and Western medicine.
It was reported that the Chinese medicine products that were used to treat respiratory tract infectious diseases might be helpful for SARS-CoV-2 treatment (47, 48). Among these products, Lianhua Qingwen capsules and ShuFeng JieDu capsules were shown to exert independent antiviral effects and synergistic antiviral effects with Western medicine products on influenza viruses, respectively (49, 50). The latest treatment guideline in China added traditional Chinese medicine (TCM) as one of the treatment options for COVID-19. Wang et al. reported four cases with COVID-19 which showed improvement after the patients were given combined Chinese and Western medicine treatment (51). However, there are few published studies on Chinese medicine products in the treatment of COVID-19 and, in particular, a dearth of high-quality research. Additional prospective, rigorous population studies are urgently required to confirm the therapeutic effect of TCM. The mechanism of their antiviral action needs to be further illuminated.
CONCLUSIONS
The potential therapeutic strategies mentioned above are based on the updated research data for SARS-CoV-2. Among those options, we anticipate that the therapeutic drugs that directly target SARS-CoV-2 will be most effective. Besides, vaccines are critical for the prevention and limitation of COVID-19 transmission. Notably, the encouraging advances in deciphering SARS-Cov-2 will lead to additional potential therapeutic targets. Further, strong preclinical and clinical studies are needed to determine the safe and effective treatment for COVID-19.
ACKNOWLEDGMENTS
All of us declare that we have no conflict of interest.
The work was supported by the National Natural Science Foundation of China (J.L., no. 81472735) and by the National Basic Research Program of China (973 program, J.L., grant no. 2015CB932600).
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19 28 February 2020, posting date Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. 2020. Coronavirus disease 2019 (COVID-19) situation report—53. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200313-sitrep-53-covid-19.pdf?sfvrsn=adb3f72_2. Accessed 13 March 2020.
- 3.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team . 2020. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tian X, Li C, Huang A, Xia S, Lu S, Shi Z, Lu L, Jiang S, Yang Z, Wu Y, Ying T. 2020. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg Microbes Infect 9:382–385. doi: 10.1080/22221751.2020.1729069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Li M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JTK, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. 29 January 2020, posting date Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao YZZ, Wang Y, Zhou Y, Ma Y, Zuo W. 2020. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv doi: 10.1101/2020.01.26.919985. [DOI] [PMC free article] [PubMed]
- 7.National Health Commission of the People’s Republic of China. 2020. Notice on printing and distributing the diagnosis and treatment plan of pneumonia with new coronavirus infection (trial version 7). http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. Accessed 4 March 2020.
- 8.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. 6 March 2020, posting date Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wan Y, Shang J, Graham R, Baric RS, Li F. 29 January 2020, posting date Receptor recognition by novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS. J Virol doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng M, Song L. 4 March 2020, posting date Novel antibody epitopes dominate the antigenicity of spike glycoprotein in SARS-CoV-2 compared to SARS-CoV. Cell Mol Immunol doi: 10.1038/s41423-020-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. 3 March 2020, posting date Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruse RL. 2020. Therapeutic strategies in an outbreak scenario to treat the novel coronavirus originating in Wuhan, China. F1000Res 9:72. doi: 10.12688/f1000research.22211.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu N-H, Nitsche A, Müller MA, Drosten C, Pöhlmann S. 4 March 2020, posting date SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xia S, Zhu Y, Liu M, Lan Q, Xu W, Wu Y, Ying T, Liu S, Shi Z, Jiang S, Lu L. 11 February 2020, posting date Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cell Mol Immunol doi: 10.1038/s41423-020-0374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inoue Y, Tanaka N, Tanaka Y, Inoue S, Morita K, Zhuang M, Hattori T, Sugamura K. 2007. Clathrin-dependent entry of severe acute respiratory syndrome coronavirus into target cells expressing ACE2 with the cytoplasmic tail deleted. J Virol 81:8722–8729. doi: 10.1128/JVI.00253-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang H, Yang P, Liu K, Guo F, Zhang Y, Zhang G, Jiang C. 2008. SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Res 18:290–301. doi: 10.1038/cr.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neveu G, Ziv-Av A, Barouch-Bentov R, Berkerman E, Mulholland J, Einav S. 2015. AP-2-associated protein kinase 1 and cyclin G-associated kinase regulate hepatitis C virus entry and are potential drug targets. J Virol 89:4387–4404. doi: 10.1128/JVI.02705-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richardson P, Griffin I, Tucker C, Smith D, Oechsle O, Phelan A, Stebbing J. 2020. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet 395:e30–e31. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blaising J, Polyak SJ, Pecheur EI. 2014. Arbidol as a broad-spectrum antiviral: an update. Antiviral Res 107:84–94. doi: 10.1016/j.antiviral.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. 2020. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao J, Tian Z, Yang X. 19 February 2020, posting date Breakthrough: chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 23.Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, Liu X, Zhao L, Dong E, Song C, Zhan S, Lu R, Li H, Tan W, Liu D. 9 March 2020, posting date In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis doi: 10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. 2003. Effects of chloroquine on viral infections: an old drug against today’s diseases? Lancet Infect Dis 3:722–727. doi: 10.1016/S1473-3099(03)00806-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez MA. 9 March 2020, posting date Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob Agents Chemother doi: 10.1128/AAC.00399-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gordon CJ, Tchesnokov EP, Feng JY, Porter DP, Gotte M. 24 February 2020, posting date The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J Biol Chem doi: 10.1074/jbc.AC120.013056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK, Washington State 2019-nCoV Case Investigation Team . 2020. First case of 2019 novel coronavirus in the United States. N Engl J Med 382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li G, De Clercq E. 2020. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov 19:149–150. doi: 10.1038/d41573-020-00016-0. [DOI] [PubMed] [Google Scholar]
- 29.Morse JS, Lalonde T, Xu S, Liu WR. 2020. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem 21:730–738. doi: 10.1002/cbic.202000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li YZJ, Wang N, Li H, Shi Y, Guo G, Liu K, Zeng H, Zou Q. 2020. Therapeutic drugs targeting 2019-nCoV main protease by high-throughput screening. BioRxiv https://www.biorxiv.org/content/10.1101/2020.01.28.922922v2.
- 31.Nguyen TM, Zhang Y, Pandolfi PP. 2020. Virus against virus: a potential treatment for 2019-nCov (SARS-CoV-2) and other RNA viruses. Cell Res 30:189–190. doi: 10.1038/s41422-020-0290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou YF, Zheng X, Wang D, Zhao C, Qi Y, Sun R, Tian Z, Xu X, Wei H. 2020. Aberrant pathogenic GM-CSF+ T cells and inflammatory CD14+CD16+ monocytes in severe pulmonary syndrome patients of a new coronavirus. BioRxiv 10.1101/2020.02.12.945576. [DOI]
- 34.Russell CD, Millar JE, Baillie JK. 2020. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet 395:473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou W, Liu Y, Tian D, Wang C, Wang S, Cheng J, Hu M, Fang M, Gao Y. 2020. Potential benefits of precise corticosteroids therapy for severe 2019-nCoV pneumonia. Signal Transduct Target Ther 5:18. doi: 10.1038/s41392-020-0127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fu Y, Cheng Y, Wu Y. 3 March 2020, posting date Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin doi: 10.1007/s12250-020-00207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen L, Xiong J, Bao L, Shi Y. 27 February 2020, posting date Convalescent plasma as a potential therapy for COVID-19. Lancet Infect Dis doi: 10.1016/S1473-3099(20)30141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garraud O, Heshmati F, Pozzetto B, Lefrere F, Girot R, Saillol A, Laperche S. 2016. Plasma therapy against infectious pathogens, as of yesterday, today and tomorrow. Transfus Clin Biol 23:39–44. doi: 10.1016/j.tracli.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marano G, Vaglio S, Pupella S, Facco G, Catalano L, Liumbruno GM, Grazzini G. 2016. Convalescent plasma: new evidence for an old therapeutic tool? Blood Transfus 14:152–157. doi: 10.2450/2015.0131-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Health Commission of the People’s Republic of China. 2020. Notice on printing and distributing the convalescent plasma treatment for novel coronavirus pneumonia (trial version 2). http://www.nhc.gov.cn/yzygj/s7658/202003/61d608a7e8bf49fca418a6074c2bf5a2.shtml. Accessed 4 March 2020.
- 41.Lu S. 2020. Timely development of vaccines against SARS-CoV-2. Emerg Microbes Infect 9:542–544. doi: 10.1080/22221751.2020.1737580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. 2020. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lucchese G. 24 Februar Y 2020, posting date Epitopes for a 2019-nCoV vaccine. Cell Mol Immunol doi: 10.1038/s41423-020-0377-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmed SF, Quadeer AA, McKay MR. 2020. Preliminary identification of potential vaccine targets for the COVID-19 coronavirus (SARS-CoV-2) based on SARS-CoV immunological studies. Viruses 12:E254. doi: 10.3390/v12030254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JI, Gutierrez RA, Gwee SXW, Chua PEY, Yang Q, Ng XY, Yap RK, Tan HY, Teo YY, Tan CC, Cook AR, Yap JC, Hsu LY. 26 Februar Y 2020, posting date Potential rapid diagnostics, vaccine and therapeutics for 2019 novel coronavirus (2019-nCoV): a systematic review. J Clin Med doi: 10.3390/jcm9030623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.CEPI. 2020. CEPI to fund three programmes to develop vaccines against the novel coronavirus, ncov-2019. https://cepi.net/news_cepi/cepi-to-fund-three-programmes-to-develop-vaccines-against-the-novel-coronavirus-ncov-2019/. Accessed on 29 January 2020.
- 47.Lu H. 28 January 2020, posting date Drug treatment options for the 2019-new coronavirus (2019-nCoV). Biosci Trends doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- 48.Ren JL, Zhang AH, Wang XJ. 2020. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res 155:104743. doi: 10.1016/j.phrs.2020.104743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ding Y, Zeng L, Li R, Chen Q, Zhou B, Chen Q, Cheng PL, Yutao W, Zheng J, Yang Z, Zhang F. 2017. The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Complement Altern Med 17:130. doi: 10.1186/s12906-017-1585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ji S, Bai Q, Wu X, Zhang DW, Wang S, Shen JL, Fei GH. 2020. Unique synergistic antiviral effects of Shufeng Jiedu Capsule and oseltamivir in influenza A viral-induced acute exacerbation of chronic obstructive pulmonary disease. Biomed Pharmacother 121:109652. doi: 10.1016/j.biopha.2019.109652. [DOI] [PubMed] [Google Scholar]
- 51.Wang Z, Chen X, Lu Y, Chen F, Zhang W. 9 Februar Y 2020, posting date Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]