Abstract
Objectives:
The present study aimed to assess the levels of the cardiac biomarkers in smokers versus non-smokers chronic periodontitis (CP) patients and periodontally healthy subjects, also to correlate cardiac biomarkers level with the severity of CP.
Methods:
Eighty selected individuals were divided into three groups: Smokers CP (28), non-smokers CP (32), and healthy control subjects (20). The CP evaluated clinically by plaque index (PI), bleeding index (BI), clinical attachment loss (CAL), and pocket depth (PD). Serum levels of cardiac biomarkers were assayed for the following: Aspartate transaminase (AST), alanine transaminase (ALT), troponin-I (Tr-I), creatinine kinase (CK), and lactate dehydrogenase (LDH).
Results:
The statistical analysis of the investigated biomarkers showed that ALT and AST significantly increased in smokers versus non-smokers CP patients (P ≤ 0.05). In addition, the other biomarkers (Tr-I, CK, and LDH) showed a non-significant increase in smokers compared with non-smokers periodontitis patients (P ≥ 0.05). Furthermore, the mean values of all biomarkers, Tr-I, ALT, AST, LDH, and CK, expressed highly significant comparisons (P ≤ 0.01) in smokers and non-smokers CP patients against healthy subjects.
Conclusion:
The present study suggested that the cardiac biomarkers affected by CP and worse aggravated by the presence of smoking that could play a bidirectional effect on periodontitis and cardiovascular (CV) conditions. Further researches are needed to elucidate the efficacy of periodontal treatment and serum cardiac biomarkers in systemically healthy and diseased CV patients.
Keywords: Alanine transaminase, aspartate transaminase, creatinine kinase, lactate dehydrogenase, smoking, troponin-I
Introduction
Chronic periodontitis (CP) is a wide-spreading disease caused mainly by anaerobic Gram-negative bacteria in susceptible host. This interaction causes damage to periodontium including loss of attachment and alveolar bone resorption.[1,2]
Smoking has a negative effect on all human body systems and considered a common risk factor which precipitating many causative diseases of death. The impact of smoking on the cardiovascular (CV) system is mediated by several pathophysiological pathways, including vasomotor effects, irritation, smooth muscle expansion, and platelet dysfunction. Moreover, smoking alters oral microflora in the human being and harms periodontium by several immunological challenges. The complexity of the problem is the slowly increasing severity of periodontal disease and a long-term follow-up is needed to monitor the progression of the disease.[3]
There is a relationship between periodontal diseases and CV diseases where the treatment of periodontal diseases may be considered now as one of the preventive measures of CV diseases. A few studies have been done using cohort, cross-sectional, or case–control studies with fluctuating results regarding the quality of this relationship.[4] The pathogenesis of periodontal diseases could explain the relationship between CV disease and CP, where the later arise from bacteria that interact with the host immunity. This challenge releases different cytokines and inflammatory mediators that could lead to systemic inflammation.[5]
The linking between CP and coronary heart diseases (CHD) has not fully understood. However, this relation complicated by other factors. In light of the fact that not just the hereditary factor assumes a role, but ecological components and other risk factors are also included. In late decades, investigations have gone to concentrate on the relationship between CP and CHD.[6]
CV biomarkers can assess the heart work by distinguishing the blood elements which related to myocardial infarction. The following biomarkers (ALT, AST, LDH, CK, and Tr-I) and high-sensitive C-reactive protein were significantly increased in CP patients than healthy controls.[7,8] A study concluded that smoking could be harmful to the CV system, apparently by elevating ventricular wall stress and leading to subclinical myocardial injury. Furthermore, there is a significant relationship between high-sensitive troponins (hs-troponins) and CV disease.[9]
Although some studies did not affirm such relation between periodontal diseases and CV diseases,[10,11] a few investigators proposed that the danger of CHD might be improved by periodontal treatment.[12,13]
Regarding the previous knowledge, this study designed to clarify such a relationship between periodontal diseases and CV diseases by evaluating the cardiac biomarkers in smokers versus non-smokers CP patients and to correlate the level of biomarkers with the severity of CP.
Materials and Methods
Patients
The individuals of this study were recruited from the periodontology clinics at the Teaching Dental Hospital, Faculty of Dentistry, Umm Al-Qura University. The UQUDENT review board was gained (IRB number 111-18), and the consent forms were obtained from all participants before management.
All participants were interviewed to taken the medical and demographic information. A total of 80 patients ranged from 30–55 years old, and they were divided into three groups: Group 1 – smoker CP (28 patients), Group 2 – non-smoker CP (32 patients), and Group 3 – healthy non-smokers control group (20 subjects).
The inclusion criteria of the selected individuals were systemically healthy subjects, either smokers or non-smokers, and Stage II and Stage III (Grade B or C) periodontitis patients (CAL ≥ 3 mm).[14] The exclusion criteria were as follows: Patients have received periodontal treatment in the past 6 months, medically and immunocompromised patients, pregnant and lactating women.
Blood samples
Non-fasting venous blood samples were collected from all participants in teaching dental hospital, then centrifuged at room temperature at 2000×g for 10 min then stored at −80°C until used. The biochemical assay was processed in medical laboratory at Al-Noor Specialized Hospital, Makkah, Saudi Arabia.
Periodontal examination
The periodontal status of all patients was measured using of the following clinical parameters: PI and BI[15,16] and PD and CAL[17] for all smokers and non-smokers CP patients.
Laboratory investigations
The selected cardiac biomarkers were investigated according to the required methodology for each one biochemically, except using an enzyme-linked immunosorbent assay technique for measuring the serum levels of Tr-I according to the manufacturer’s directions, using Dimension analyzer (Siemens Healthcare, Erlangen, Germany).
The biochemical assaying of ALT, AST, LDH, and CK was determined in serum using of UV/Vis Spectrophotometer (Humastar 200, Automatic Biochemistry Analyzer, Wiesbaden, Germany). The levels of serum (AST and ALT) were determined by the method of Reitman,[18] LDH by the technique of Amador,[19] and CK by the method of Tanzer.[20]
Statistical analysis
The statistical investigation was done using of the SPSS (Statistical Package for the Social Sciences) program version-22. The collected data represented in the following descriptive statistics data mean, standard deviation, minimum, and maximum. The paired and unpaired t-test was used to compare the mean values between groups and intergroups; also, Pearson’s correlation was used to correlate periodontal parameters against to the evaluated biomarkers. The significance was determined when P ≤ 0.05. The statistical data were charted and graphed by Microsoft Word version 2016.
Results
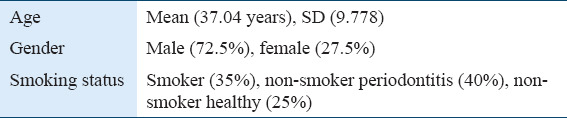
Eighty individuals were participated in this study, their mean age was 37.04 years (male 72.5% and female 27.5%). They were categorized into the following groups: Group 1 (smoker CP patients, 35%), Group 2 (non-smoker CP patients, 40%), and Group 3 (healthy subjects, 25%) (Table 1).
Table 1.
Demographic data of participants
Evaluation of clinical parameters
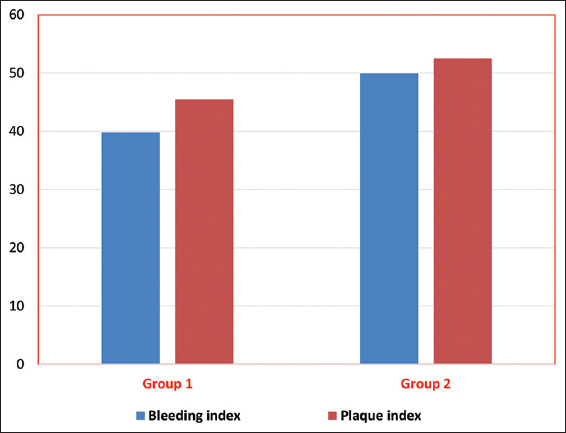
The descriptive statistics of clinical parameters (BI, PI, PD, and CAL) are demonstrated in Table 2. The data were expressed as follows: Mean ± SD, Group 1 – smoker periodontitis (39.81 ± 19.08, 45.49 ± 14.89, 2.76 ± 0.51, and 3.84 ± 1.09, respectively) and Group 2 – non-smoker (49.92 ± 17.46, 52.49 ± 14.30, 2.81 ± 0.47, and 4.07 ± 1.27, respectively). The statistical analysis showed a significant reduction in BI and PI in smokers compared to non-smokers CP periodontitis patient (P ≤ 0.05) (Figure 1), while there were no significant differences in PD and CAL (P ≥ 0.05) (Figures 1 and 2).
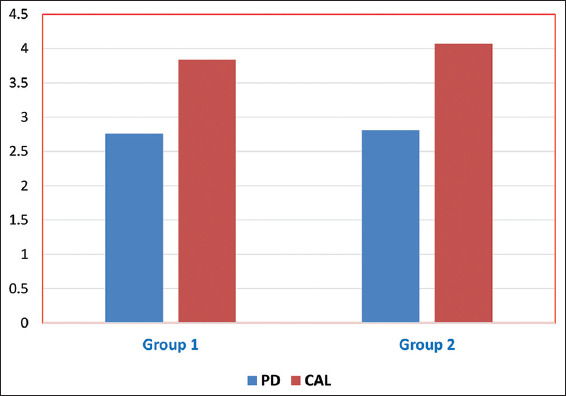
Table 2.
Statistical comparisons of t-test for all clinical parameters
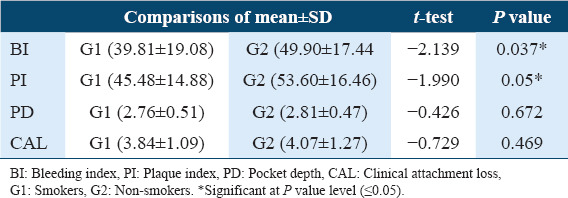
Figure 1.
The bleeding and plaque indices of smokers and non-smokers CP patients. G1: Smokers CP, G2: Non-smokers CP
Figure 2.
The pocket depth and clinical attachment loss of smokers and non smokers CP patients.
Evaluation of cardiac biomarkers
The descriptive statistical data, mean ± SD, are expressed in Table 3. The statistical comparisons for mean values of ALT and AST showed a significant increase in smokers versus non-smokers CP patients (P ≤ 0.05). Whereas, non-significant changes (P ≥ 0.05) when comparing the other cardiac biomarkers (Tr-I, CK, and LDH). Furthermore, the comparisons of smokers and non-smokers CP patients to healthy control subjects, the statistical analysis demonstrated a highly significant increase (P ≤ 0.01) for all examined cardiac biomarkers: Tr-I, ALT, AST, LDH, and CK (Table 3) (Figures 3 and 4).
Table 3.
Demonstrate statistical comparison of t-test for blood analyses
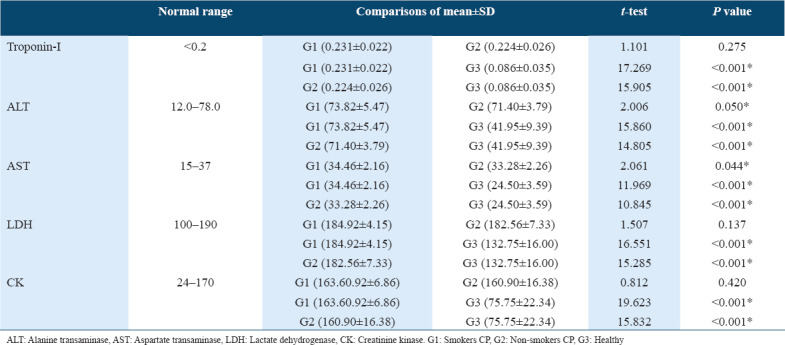
Figure 3.
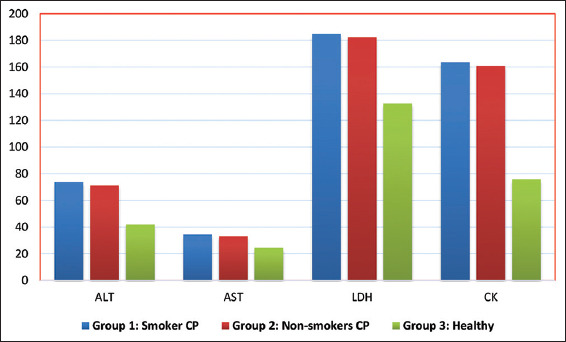
The cardiac biomarker in three studied groups.
Figure 4.
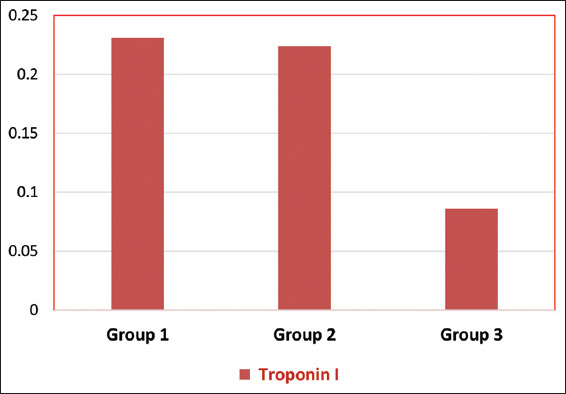
Mean values of troponin-I levels in three examined groups. G1: Smokers CP, G2: Non-smokers CP, G3: Healthy
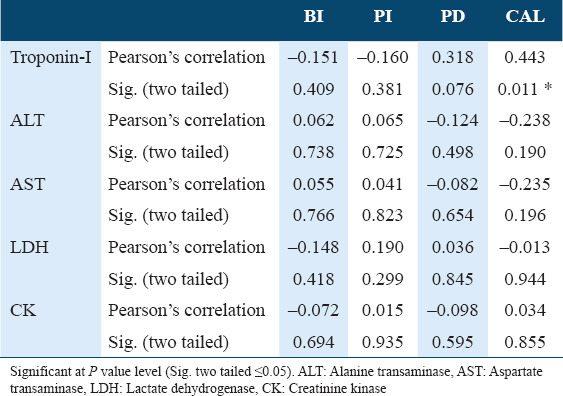
Correlation of cardiac biomarkers with clinical parameters
A correlation was significant in Tr-I test in relation to clinical attachment loss in non-smoker CP patients (P ≤ 0.05, Pearson’s correlation; r = 0.443), while there was no significant increase in other parameters. The correlation of blood analyses with clinical parameters in smokers and non-smokers CP patients presented in Tables 4 and 5.
Table 4.
Correlation of cardiac biomarkers levels with clinical parameters in smokers CP
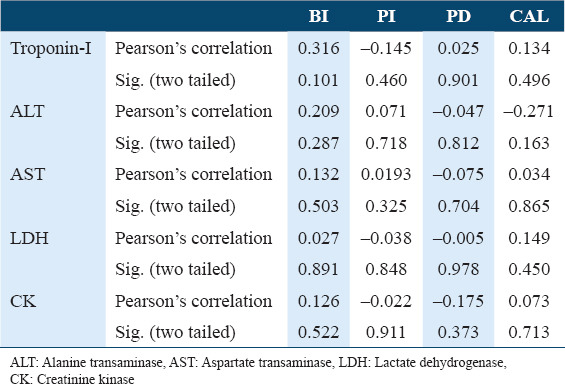
Table 5.
Correlation of cardiac biomarkers levels with clinical parameters in non-smokers CP.
Discussion
Periodontal disease shared with systemic or metabolic disorders is highly prevalent among the population. The association between them is the subject of periodontal medicine researches, and a variety of theories about the possible association between the two diseases have been proposed and hypothesized the intervention of an inflammatory responses.[21] This bidirectional effect between CP and systemic diseases as diabetes, autoimmune, and CV diseases, rheumatoid arthritis, was suggested by the fact that oral infection is a constant potential source for systemic infection and inflammation.[22]
Systemic infections are recognized to induce a hypercoagulable state and increase blood viscosity. Fibrinogen levels and white blood cell counts are often raised in patients with periodontal disease. Individuals with poor oral health may also have significant elevations in coagulation factor VIII/von Willebrand factor antigen, thereby increasing the risk of thrombus formation. Thus, the periodontal infection may also promote increased blood viscosity and thrombogenesis, which leads to an increased risk for central and peripheral vascular diseases.[23]
Cigarette smoking is considered a leading preventable cause of CV mortality and morbidity. Epidemiological studies suggested that former smokers, and current smokers, are at higher risk in developing of heart failure even after adjusting for coronary artery disease.[24] Experimental animal studies suggested that smoking of tobacco may exert direct toxic effects on the myocardium;[25] additionally, clinical studies showed association between smoking and alteration in cardiac function in subjects without obvious CV disease.[26] On the other hand, cigarette smoking is an independent risk factor for the initiation, progression, and severity of the periodontal disease. Besides that, smoking can impact the chances of successful periodontal therapy.[3]
The present study mainly aimed to evaluate the serum cardiac biomarkers level in smokers and non-smokers CP patients in comparison to the healthy control individuals. The periodontal parameters were evaluated clinically, and the cardiac biomarkers were measured biochemically to confirm the possible relationship.
The current study evaluated the clinical parameters of both examined groups through clinical evaluation of PI, BI, PD, and CAL. The PI was significantly increased in non-smokers CP patients, this finding is consistent with Lin et al., 2017,[27] but disagree with Feres et al., 2015.[28] The BI has significantly increased in non-smokers CP patients, this outcome inconsistent with Feres et al., 2015 and Lin et al., 2017.[27,28] For clarification, because the vasoconstriction effect of smoking on gingival blood vessels and increased keratinization of the gingival epithelium, these may reflect less inflammation in gingival tissues of smokers than non-smokers CP patients, this concept is supported by Preber and Bergstrom, 1986.[29]
Regarding the mean values of PD, the results demonstrated a non-significant comparison between smokers and non-smokers CP patients, this observation in agreement with Feres et al., 2015,[28] whereas inconsistent with some studies.[27,30] Concerning to CAL, the results expressed non-significant differences between smokers and non-smokers CP patients. This remark was consistent with some authors,[28,30] while against the results of Lin et al., 2017.[27] The insignificant comparisons of PD and CAL in smokers versus non-smokers CP may be referred to as the selected individuals are moderate-to-severe CP, and a large scale of the population may be required.
Troponin is considered a primary cardiac biomarker, notably increased with acute myocardial conditions.[31] They examined the relationship of acute myocardial infarct size with extension and severity of periodontitis and measured the Tr-I serum levels. They reported that the Tr-I level was highly significant correlated with the severity of periodontitis in acute myocardial infarcted periodontitis patients. According to the investigated levels of Tr-I in the present study, the level of Tr-I was significantly increased in both smokers and non-smokers CP patients in comparison to healthy control subjects. These findings are consistent with the research work of Loo et al., 2012,[8] they concluded that the increased level of Tr-I may consider a potential risk of CVD development and suggested to use the Tr-I as a monitor to CVD in CP patients. The Tr-I level was slightly increased in smokers than non-smokers CP patients, and this relationship is similar to the results of Loo et al., 2012.[8] According to the previous outcomes, smoking may increase the possibility of cardiac disorders in systemically healthy CP patients. On the other hand, another study by Vedin et al., 2017,[32] observed that there is no association between the high-sensitivity troponin-T (Tr-T) and the ratio of tooth loss in several patients with cardiac disease.
AST and ALT enzymes are most commonly associated with tissue damage. Measurement of AST level provides a suggestion of the progression of periodontitis. Therefore, AST could be a potential biomarker for differentiating between active and inactive disease sites.[33] The statistical comparisons for serum level of ALT and AST were demonstrated highly significant increase in smokers and non-smokers CP patients versus healthy individuals. This observation was supported by some authors.[34,7] On other side, Dabra et al., 2012, concluded that the salivary (AST and ALT) considered as biochemical markers for assessing the diagnosis and prognosis of the functional state of periodontal tissues in health and disease and in the evaluation of the periodontal therapy outcomes.[35]
In this study, the mean values of ALT and AST were increased in smokers than non-smokers CP patients, and a significant difference was obtained. This observation was in accordance with the results of two studies.[36,37] Based on the previous information, the present study suggested a significant effect of smoking and periodontitis as risks for elevating the serum levels of ALT and AST.
The LDH, CK, and AST biomarkers are intracellular cytoplasmic enzymes that become extracellular when cell death. Hence, the LDH, CK, and AST are used as diagnostic biomarkers of tissue breakdown in chronic liver diseases, acute myocardial infarction, the extent of brain injury following cerebrovascular disease, or infection. The extracellular appearance of LDH and the high level of LDH used to detect cell damages, disease progression, and cell death. This outcome is adapted with the result in the current study that represented a highly significant increase of LDH levels in smokers and non-smokers CP in comparison to healthy control that might support the use of LDH as a potential diagnostic biomarker for periodontal disease progression.[38,39]
The association between periodontal condition and serum CK levels among young soccer players was studied by Alshail et al., 2016,[40] they concluded that the increase in bleeding on probing (BOP) and PD was associated with high serum CK level in young soccer players and considered that serum CK level may be revealing compromised oral health. Similarly, we observed a highly significant increase in the levels of CK in smokers and non-smokers in contrast to healthy individuals. Furthermore, the serum levels of LDH and CK were increased in smokers in comparison to non-smokers CP patients and the differences were non-significant.[41] This notification may reveal the risk of smoking on systemically healthy CP patients.
The correlative analysis of the assayed biomarkers with clinical parameters in both smokers and non-smokers CP patients reflected a non-significant association for all parameters except for CAL and Tr-I in non-smokers CP. For elucidation, the non-significant correlation may be related to the patients who were in the range of moderate-to-severe CP and systemically healthy. For the previous reason, a future study on the association of cardiac biomarkers with periodontal parameters in CVD patients is recommended. Periodontitis and CVD are multifactorial diseases that are precipitated by common risk factors, and the association might be present. Moreover, smoking aggravated the severity of periodontitis and CVD. Hence, the resolution of periodontal infections and tobacco cessation are beneficial, as well as the communication between dentists and cardiologists is strongly recommended.
Conclusion
The present study concluded the following: (1) The serum levels of cardiac biomarkers were more affected in smokers, and non-smokers CP patients versus healthy individuals. (2) Periodontitis considered as one of the potential risk factors that lead to the development and progression of CVD. (3) Smoking played a bidirectional role in aggravating the periodontal and CVD. (4) More researches are needed to clarify the efficacy of periodontal treatment on cardiac biomarkers in the systemically healthy and in diseased CV patients.
Funding/Support
No fund.
Conflicts of Interest
None declared including specific, related, and/or affiliated financial interest.
References
- 1.D'aiuto F, Graziani F, Tete S, Gabriele M, Tonetti MS. Periodontitis:From local infection to systemic diseases. Int J Immunopathol Pharmacol. 2005;18(Suppl 3):1–11. [PubMed] [Google Scholar]
- 2.Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990-2010:A systematic analysis. J Dent Res. 2013;92:592–7. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borojevic T. Smoking and periodontal disease. Mater Sociomed. 2012;24:274. doi: 10.5455/msm.2012.24.274-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmstrup P, Poulsen AH, Andersen L, Skuldbøl T, Fiehn NE. Oral infections and systemic diseases. Dent Clin North Am. 2003;47:575–98. doi: 10.1016/s0011-8532(03)00023-5. [DOI] [PubMed] [Google Scholar]
- 5.de Oliveira C, Watt R, Hamer M. Toothbrushing, inflammation, and risk of cardiovascular disease:Results from Scottish health survey. BMJ. 2010;340:c2451. doi: 10.1136/bmj.c2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parkar SM, Modi GN, Jani J. Periodontitis as risk factor for acute myocardial infarction:A case control study. Heart Views. 2013;14:5–11. doi: 10.4103/1995-705X.107113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Furuta M, Ekuni D, Yamamoto T, Irie K, Koyama R, Sanbe T, et al. Relationship between periodontitis and hepatic abnormalities in young adults. Acta Odontol Scand. 2010;68:27–33. doi: 10.3109/00016350903291913. [DOI] [PubMed] [Google Scholar]
- 8.Loo WT, Yue Y, Fan CB, Bai LJ, Dou YD, Wang M, et al. Comparing serum levels of cardiac biomarkers in cancer patients receiving chemotherapy and subjects with chronic periodontitis. J Transl Med. 2012;10:S5. doi: 10.1186/1479-5876-10-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nadruz W, Jr, Gonçalves A, Claggett B, Roca GQ, Shah AM, Cheng S, et al. Influence of cigarette smoking on cardiac biomarkers:The atherosclerosis risk in communities (ARIC) study. Eur J Heart Fail. 2016;18:629–37. doi: 10.1002/ejhf.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hujoel PP, Drangsholt M, Spiekerman C, Derouen TA. Examining the link between coronary heart disease and the elimination of chronic dental infections. J Am Dent Assoc. 2001;132:883–9. doi: 10.14219/jada.archive.2001.0300. [DOI] [PubMed] [Google Scholar]
- 11.Tuominen R, Reunanen A, Paunio M, Paunio I, Aromaa A. Oral health indicators poorly predict coronary heart disease deaths. J Dent Res. 2003;82:713–8. doi: 10.1177/154405910308200911. [DOI] [PubMed] [Google Scholar]
- 12.Losche W. Periodontitis and cardiovascular disease:Periodontal treatment lowers plasma cholesterol. Southern Med J. 2007;100:663–5. doi: 10.1097/SMJ.0b013e318038fa4d. [DOI] [PubMed] [Google Scholar]
- 13.Tonetti MS, D'Aiuto F, Nibali L, Donald A, Storry C, Parkar M, et al. Treatment of periodontitis and endothelial function. N E J Med. 2007;356:911–20. doi: 10.1056/NEJMoa063186. [DOI] [PubMed] [Google Scholar]
- 14.Caton JG, Armitage G, Berglundh T, Chapple IL, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri-implant diseases and conditions-introduction and key changes from the 1999 classification. J Periodontol. 2018;89:S1–8. doi: 10.1002/JPER.18-0157. [DOI] [PubMed] [Google Scholar]
- 15.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 16.O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972;43:38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- 17.Ramfjord SP, Emslie RD, Greene JC, Held AJ, Waerhaug J. Epidemiological studies of periodontal diseases. Am J Public Health Nat Health. 1968;58:1713–22. doi: 10.2105/ajph.58.9.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reitman S, Frankel S. A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol. 1957;28:56–63. doi: 10.1093/ajcp/28.1.56. [DOI] [PubMed] [Google Scholar]
- 19.Amador E, Dorfman LE, Wacker WE. Serum lactic dehydrogenase activity:An analytical assessment of current assays. Clin Chem. 1963;9:391–9. [PubMed] [Google Scholar]
- 20.Tanzer ML, Gilvarg C. Creatine and creatine kinase measurement. J Biol Chem. 1959;12:3201–4. [PubMed] [Google Scholar]
- 21.Carramolino-Cuéllar E, Tomás I, Jiménez-Soriano Y. Relationship between the oral cavity and cardiovascular diseases and metabolic syndrome. Med Oral Patol Oral Cir Bucal. 2014;19:e289. doi: 10.4317/medoral.19563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagpal R, Yamashiro Y, Izumi Y. The two-way association of periodontal infection with systemic disorders:An overview. Mediators Inflamm. 2015;2015:793898. doi: 10.1155/2015/793898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linden GJ, Linden K, Yarnell J, Evans A, Kee F, Patterson CC. All-cause mortality and periodontitis in 60-70-year-old men:A prospective cohort study. J Clin Periodontol. 2012;39:940–6. doi: 10.1111/j.1600-051X.2012.01923.x. [DOI] [PubMed] [Google Scholar]
- 24.Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, Smith AL, Bauer DC, Newman AB, et al. Cigarette smoking exposure and heart failure risk in older adults:The health, aging, and body composition study. Am Heart J. 2012;164:236–42. doi: 10.1016/j.ahj.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Minicucci M, Azevedo PS, Polegato BF, Paiva SA, Zornoff LA. Cardiac remodeling induced by smoking:Concepts, relevance, and potential mechanisms. Inflamm Allergy Drug Targets. 2012;11:442–7. doi: 10.2174/187152812803589958. [DOI] [PubMed] [Google Scholar]
- 26.Dalen H, Thorstensen A, Romundstad PR, Aase SA, Stoylen A, Vatten LJ. Cardiovascular risk factors and systolic and diastolic cardiac function:A tissue Doppler and speckle tracking echocardiographic study. J Am Soc Echocardiogr. 2011;24:322–32. doi: 10.1016/j.echo.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Lin YC, Wu CY, Chang LY, Chen CC, Chen HH, Lai YL, et al. Levels of high-mobility group box-1 in gingival crevicular fluid in nonsmokers and smokers with chronic periodontitis. J Form Med Assoc. 2017;116:933–9. doi: 10.1016/j.jfma.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Feres MM, Bernal MA, Matarazzo F, Faveri M, Duarte PM, Figueiredo LC. Subgingival bacterial recolonization after scaling and root planing in smokers with chronic periodontitis. Aust Dent J. 2015;60:225–32. doi: 10.1111/adj.12225. [DOI] [PubMed] [Google Scholar]
- 29.Preber H, Bergström J. Cigarette smoking in patients referred for periodontal treatment. Eur J Oral Sci. 1986;94:102–8. doi: 10.1111/j.1600-0722.1986.tb01372.x. [DOI] [PubMed] [Google Scholar]
- 30.Erley KJ, Swiec GD, Herold R, Bisch FC, Peacock ME. Gingival recession treatment with connective tissue grafts in smokers and non-smokers. J Periodontol. 2006;77:1148–55. doi: 10.1902/jop.2006.050252. [DOI] [PubMed] [Google Scholar]
- 31.Marfil-Álvarez R, Mesa F, Arrebola-Moreno A, Ramírez-Hernández JA, Magán-Fernández A, O'Valle F, et al. Acute myocardial infarct size is related to periodontitis extent and severity. J Dent Res. 2014;93:993–8. doi: 10.1177/0022034514548223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vedin O, Hagström E, Östlund O, Avezum A, Budaj A, Flather MD, et al. Associations between tooth loss and prognostic biomarkers and the risk for cardiovascular events in patients with stable coronary heart disease. Int J Cardiol. 2017;245:271–6. doi: 10.1016/j.ijcard.2017.07.036. [DOI] [PubMed] [Google Scholar]
- 33.Sheth TS, Verma SJ. Analysis of aspartate aminotransferase in gingival crevicular fluid:A study with initial therapy. J Indian Soc Periodontol. 2011;15:235. doi: 10.4103/0972-124X.85666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Banu S, Jabir NR, Mohan R, Manjunath NC, Kamal MA, Kumar KR, et al. Correlation of toll-like receptor 4, interleukin-18, transaminases, and uric acid in patients with chronic periodontitis and healthy adults. J Periodontol. 2015;86:431–9. doi: 10.1902/jop.2014.140414. [DOI] [PubMed] [Google Scholar]
- 35.Dabra S, China K, Kaushik A. Salivary enzymes as diagnostic markers for detection of gingival/periodontal disease and their correlation with the severity of the disease. J Indian Soc Periodontol. 2012;16:358. doi: 10.4103/0972-124X.100911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuroki A, Sugita N, Komatsu S, Yokoseki A, Yoshihara A, Kobayashi T, et al. Association of liver enzyme levels and alveolar bone loss:A cross-sectional clinical study in Sado Island. J Clin Exp Dent. 2018;10:e100. doi: 10.4317/jced.54555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Widita E, Yoshihara A, Hanindriyo L, Miyazaki H. Relationship between clinical periodontal parameters and changes in liver enzymes levels over an 8-year period in an elderly Japanese population. J Clin Periodontol. 2018;45:311–21. doi: 10.1111/jcpe.12861. [DOI] [PubMed] [Google Scholar]
- 38.De La Peña VA, Dios PD, Sierra RT. Relationship between lactate dehydrogenase activity in saliva and oral health status. Arch Oral Biol. 2007;52:911–5. doi: 10.1016/j.archoralbio.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 39.Miyoshi N, Tanigawa T, Nishioka S, Maruyama K, Eguchi E, Tanaka K, et al. Association of salivary lactate dehydrogenase level with systemic inflammation in a Japanese population. J Periodont Res. 2018;53:487–94. doi: 10.1111/jre.12537. [DOI] [PubMed] [Google Scholar]
- 40.Alshail F, Aljohar A, Alshehri M. Periodontal status and serum creatine kinase levels among young soccer players:A preliminary report. Niger J Clin Pract. 2016;19:655–8. doi: 10.4103/1119-3077.188708. [DOI] [PubMed] [Google Scholar]
- 41.Kanmaz B, Lamont G, Danacı G, Gogeneni H, Buduneli N, Scott DA. Microbiological and biochemical findings in relation to clinical periodontal status in active smokers, non-smokers and passive smokers. Tob Induc Dis. 2019;17:1–6. doi: 10.18332/tid/104492. [DOI] [PMC free article] [PubMed] [Google Scholar]


