Abstract
Background
Three clusters of coronavirus disease 2019 (COVID-19) linked to a tour group from China, a company conference, and a church were identified in Singapore in February, 2020.
Methods
We gathered epidemiological and clinical data from individuals with confirmed COVID-19, via interviews and inpatient medical records, and we did field investigations to assess interactions and possible modes of transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Open source reports were obtained for overseas cases. We reported the median (IQR) incubation period of SARS-CoV-2.
Findings
As of Feb 15, 2020, 36 cases of COVID-19 were linked epidemiologically to the first three clusters of circumscribed local transmission in Singapore. 425 close contacts were quarantined. Direct or prolonged close contact was reported among affected individuals, although indirect transmission (eg, via fomites and shared food) could not be excluded. The median incubation period of SARS-CoV-2 was 4 days (IQR 3–6). The serial interval between transmission pairs ranged between 3 days and 8 days.
Interpretation
SARS-CoV-2 is transmissible in community settings, and local clusters of COVID-19 are expected in countries with high travel volume from China before the lockdown of Wuhan and institution of travel restrictions. Enhanced surveillance and contact tracing is essential to minimise the risk of widespread transmission in the community.
Funding
None.
Introduction
On Dec 31, 2019, a cluster of viral pneumonia cases, subsequently identified as coronavirus disease 2019 (COVID-19), was reported in Wuhan, China.1 Subsequent reports suggested that community transmission had occurred in Wuhan and Hubei province, leading to the lockdown of Wuhan on Jan 23, 2020, and subsequently other cities in Hubei province, to control COVID-19 spread.2, 3 WHO declared a public health emergency of international concern on Jan 30, 2020.4 As of March 6, 2020, 98 192 confirmed cases and 3380 deaths were reported globally, including 17 481 cases and 335 deaths from 88 regions or countries outside of mainland China.5
Singapore, a city-state in southeast Asia, developed case-definitions, laboratory tests, and enhanced surveillance to detect affected individuals with COVID-19 early, to enable containment of the disease. Singapore confirmed its first imported case of COVID-19 from Wuhan on Jan 23, 2020.6 With the lockdown of Wuhan, inbound flights from Wuhan to Singapore had ceased since Jan 23, 2020. As of Feb 22, 2020, 89 people in Singapore were confirmed to have COVID-19, and the first 18 affected individuals all reported recent travel to Wuhan. Singapore identified several local clusters of COVID-19, with the first three linked to a tour group from China, a company conference, and a church.
To contain the spread of COVID-19, several pertinent questions need to be addressed. What is the infectiousness of cases? What are the settings and activities beyond family clusters where spread can occur? What measures should be taken to improve surveillance and case-detection? What measures can reduce disease spread? To answer these questions, we report data for the first three clusters of COVID-19 cases in Singapore, the epidemiological and clinical investigations done to ascertain disease characteristics and exposure types, and summary statistics to characterise the incubation period of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the serial interval between transmission pairs. Our findings will be important for countries and cities to calibrate detection and response efforts during the ongoing epidemic.
Methods
Study design
Since Jan 2, 2020, the Ministry of Health in Singapore has been refining local case-definitions for people suspected of having COVID-19 (appendix p 4). Doctors are required by law to notify the Ministry of Health of cases of COVID-19.7 Further, Singapore implemented enhanced surveillance on Jan 31, 2020, to test for COVID-19 among patients in intensive care units and people who died of unknown cause, all people with pneumonia in hospitals, and individuals with influenza-like illness in sentinel primary-care clinics. Hospital-based doctors also have permission to test patients who they view with suspicion for clinical or epidemiological reasons. A confirmed case of COVID-19 is defined as an individual with a respiratory sample positive for SARS-CoV-2, using a laboratory-based PCR test (appendix p 1). Phylogenetic analysis is done of available viral genomic sequences to ascertain genetic clustering.
Research in context.
Evidence before this study
We searched PubMed up to Feb 15, 2020 for reports published in English with no date limitations using the keywords “COVID-19” and “cluster”. A family cluster of coronavirus disease 2019 (COVID-19) was reported in Shenzhen, Guangdong. Transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has also been reported among co-workers in Germany.
Added value of this study
We analysed three clusters of COVID-19 in Singapore to assess interactions and possible modes of transmission. Our findings show that SARS-CoV-2 is transmissible in community settings beyond household clusters. Importation and limited local transmission of SARS-CoV-2 could have occurred before the lockdown of Wuhan and China's institution of travel restrictions.
Implications of all the available evidence
Countries should focus on enhancing detection and containment of local clusters of COVID-19, through surveillance of individuals with general pneumonia or influenza-like illnesses, and of people who have been in contact with unwell travellers from China. It is also important for countries to do active case-finding among close contacts of affected individuals, including contacts with mild symptoms, to contain clusters and stop them from spreading.
The Ministry of Health in Singapore identified the first three clusters of COVID-19 cases on Feb 3, 2020, Feb 5, 2020, and Feb 8, 2020. All epidemiological investigations and outbreak containment measures were implemented under the Infectious Diseases Act,7 which provides for use of data for analysis to control outbreaks.
Epidemiological investigation
We interviewed people with confirmed COVID-19 to obtain data for demographic characteristics, clinical symptoms, and activity patterns, from 14 days preceding symptom onset until isolation in hospital. We initiated contact tracing to identify close contacts (ie, people who spend a prolonged time within 2 m of a confirmed case) and other contacts who had some interactions with the case. We asked people with confirmed COVID-19 about possible contact with confirmed cases reported overseas in the 14 days before symptom onset. We used open source information from other countries (including government websites), news aggregators (eg, ProMed), and media reports to identify secondary transmissions in the respective clusters. For each cluster, we investigated the implicated setting to ascertain potential interactions. We reviewed activity maps of other confirmed cases in Singapore to identify potential epidemiological links to each cluster.
We placed close contacts under quarantine for 14 days from last exposure to the individual with confirmed COVID-19, either at home or at designated government quarantine facilities. We monitored their health status daily; people who developed symptoms were conveyed in dedicated ambulances to hospital for isolation and testing as part of active case-finding. We video-called individuals who were quarantined at home three times a day to verify their location; quarantine violators were tagged with a continuous tracking device. We placed other contacts (depending on risk stratification) on phone surveillance or advised them to self-monitor and visit a primary-care clinic if they became unwell.
Clinical management
We isolated people with confirmed COVID-19 in individual negative-pressure rooms with anterooms. We did blood investigations including a complete blood count, renal and liver function tests, and amounts of C-reactive protein and lactate dehydrogenase. Treatment was mainly supportive; we started some patients on oral lopinavir (400 mg) with ritonavir (100 mg) twice daily. We obtained clinical data for chronic medical illnesses, physical examinations, laboratory and radiological results, and clinical progression and outcome from inpatient medical records.
Analysis of disease transmission data
We reported the median (IQR) incubation period, defined as the duration between estimated dates of infection and reported symptom onset, using R. We reported the serial interval range between transmission pairs in the household cluster. We also calculated the probable number of transmissions arising from each confirmed case of COVID-19 by assuming that there was one unknown primary case for each of the three clusters.
Role of the funding source
This study received no funding. The corresponding authors had full access to all data in the study and had final responsibility for the decision to submit for publication.
Results
Confirmed cases of COVID-19
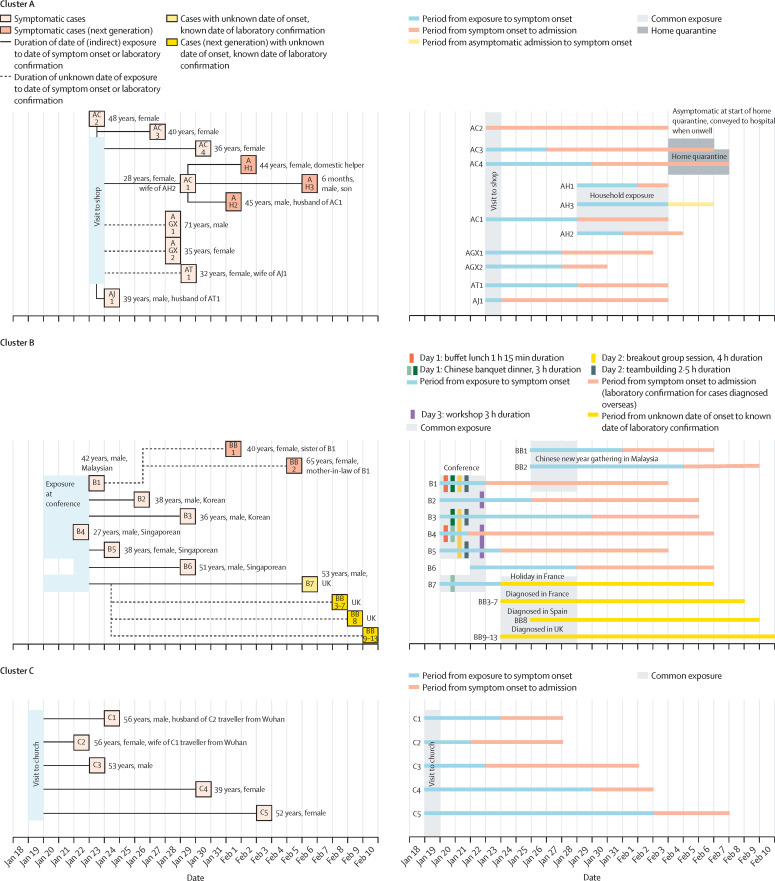
36 individuals were confirmed to have COVID-19, and these people were related to three local clusters, referred to as A (containing 11 people), B (consisting of 20 individuals), and C (comprising five people; figure 1 ). Of these affected individuals, 17 tested positive for SARS-CoV-2 in Singapore, of whom only two (both from cluster C) had recent travel history to China 14 days before onset of symptoms (table ). Two people from cluster A and 17 from cluster B were reported by the health authorities of countries where they resided or travelled to.
Figure 1.
Timing of events and cases in three clusters of COVID-19 in Singapore
Age and sex are shown for each case (left panels), with other pertinent information (eg, relationship or nationality). Timeline of events (right panels); onset dates of symptomatic cases are shown, when available. COVID-19=coronavirus disease 2019.
Table.
Demographic, clinical, and radiological characteristics of individuals who tested positive for SARS-CoV-2 in Singapore
| Individuals (n=17) | ||
|---|---|---|
| Age (years) | 40 (36–51) | |
| Gender | ||
| Male | 7 (41%) | |
| Female | 10 (59%) | |
| Ethnic origin | ||
| Chinese | 16 (94%) | |
| Other | 1 (6%) | |
| Nationality | ||
| Singaporean | 13 (76%) | |
| Chinese | 3 (18%) | |
| Indonesian | 1 (6%) | |
| Cluster | ||
| A (tourist group from China and shopworkers) | 9 (53%) | |
| B (company conference) | 3 (18%) | |
| C (church) | 5 (29%) | |
| Chronic illness | ||
| Yes* | 3 (18%) | |
| No | 14 (82%) | |
| Travel to China in past 14 days | ||
| Yes | 2 (12%) | |
| No | 15 (88%) | |
| Symptoms | ||
| Fever | 15 (88%) | |
| Cough | 14 (82%) | |
| Sore throat | 8 (47%) | |
| Shortness of breath | 6 (35%) | |
| Myalgia | 5 (29%) | |
| Diarrhoea | 4 (24%) | |
| Chest pain | 3 (18%) | |
| Runny nose | 1 (6%) | |
| Nausea or vomiting | 1 (6%) | |
| Chest radiography findings on admission† | ||
| Present | 8 (53%) | |
| Absent | 7 (47%) | |
| Interval between symptom onset and hospitalisation (days) | 4 (3–9) | |
Data are median (IQR) or n (%). SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
Allergic rhinitis (n=1), hypertension (n=1), and cervical spondylosis (n=1).
Data available for 15 individuals.
Cluster A
The Ministry of Health in Singapore was alerted to two individuals with locally acquired COVID-19 on Feb 3, 2020 (AC1 and AC2; figure 1 upper panels). They did not fit the case-definition for suspected COVID-19 but were tested because they reported frequent occupational contact with Chinese tourists. These two people were later identified to be linked epidemiologically to two other affected individuals (AGX1 and AGX2), a father and daughter reported by official and media websites in Guangxi, China,8, 9, 10 to be Chinese tourists who travelled to Singapore on Jan 22, 2020, and who visited several tourist sites on Jan 22–23, 2020, as part of a tour group. AGX1 and AGX2 subsequently departed for Malaysia before re-entry into Singapore for their flight to Guangxi on Jan 27, 2020, and they developed symptoms on Jan 28, 2020, after arrival in Guangxi. Details of the tour participants and the itinerary, obtained through the Singapore-based tour guide for the Singapore tour segment (AT1, who also tested positive for SARS-CoV-2) corroborated with details for AGX1 and AGX2 reported by Guangxi websites.
Of 20 tourists in the tour group from Guangxi, five or six were reported by AT1 to be coughing during the tour. To the best of our knowledge, only AGX1 and AGX2 had laboratory-confirmed COVID-19 (positive PCR for SARS-CoV-2).8 However, in view of the reported respiratory symptoms among tour group participants, it is possible that other tour group members were the primary cases.
Among the places visited by the tour group in Singapore were a complementary health products shop and a jewellery shop; both shops are patronised frequently by Chinese tour groups. The visits to the complementary health products shop lasted approximately 30 min, and the visit to the jewellery shop lasted roughly 1 h. Four assistants in the complementary health products shop (AC1, AC2, AC3, and AC4) and one assistant in the jewellery shop (AJ1) were identified to have COVID-19. All five shop assistants were at work on the day the tour group from Guangxi visited. AC1, AC2, AC3, and AC4 reported that they would assist customers to apply samples of medicinal oil on their bodies, and handwashing was not usually done between customers. Three secondary transmission cases were identified in the household of AC1 (AH1, AH2, and AH3), none of whom were contacts of other cases.
For the cases who were confirmed on or before Feb 5, 2020, 179 close contacts who were in Singapore and contactable were placed under quarantine, of whom two close contacts (AC3 and AC4) subsequently reported to be unwell and tested positive for SARS-CoV-2. An additional six close contacts were quarantined. For active surveillance, 16 shop assistants at the complementary health products shop and the sole remaining uninfected household member of AC1, who were all asymptomatic, were tested and none were positive for SARS-CoV-2.
Viral genomic sequences were available for four cases (AH1, AH2, AH3, and AT1) and phylogenetic analysis confirmed their linkage, as suggested by the epidemiological data (appendix pp 2–3).
Cluster B
On Feb 4, 2020, Malaysia confirmed a case of COVID-19 in an individual (B1) who had recent travel history to Singapore on Jan 16–23, 2020, for a company conference (a closed business meeting for employees from company branches globally), which was attended by at least 111 participants from 19 different countries on Jan 20–22, 2020. 17 attendees at the conference were from mainland China and at least one was from Wuhan. Subsequently, six participants at the conference who had no recent travel history to China (B2, B3, B4, B5, B6, and B7) tested positive for SARS-CoV-2 (figure 1 middle panels). Two affected individuals from Singapore were identified through contact tracing of participants after notification from the Malaysian International Health Regulation (IHR) focal point.
The conference programme included business presentations, workshops, breakout discussions, a welcome reception and meals, team-building games, and a Singapore city bus tour. Seating arrangements (where available) for the conference, and interviews with affected individuals, indicated close interactions between cases. Two groups (B1 and B3, and B4 and B7) were seated at the same tables for a 3-h Chinese banquet-style dinner on Jan 20, 2020, with three and two attendees from China, respectively. Four cases (B1, B3, B4, and B5) were in a 4-h breakout session on Jan 21, 2020, with 41 other participants, including ten from China, of whom three had dined with B1 and B3 or B4 and B7 at the Chinese banquet. Furthermore, the team-building games entailed close physical contact.
With initial news of B1, 15 conference participants remaining in Singapore were contacted to find out about their health status. Four people reported being unwell with fever, respiratory symptoms, or both and were tested for SARS-CoV-2; two individuals (B4 and B5) tested positive for the virus. The third local case (B6) was identified via activity mapping to have attended the conference and had subsequent interactions with company staff. 153 close contacts were placed under quarantine. Hotel staff were told to monitor their health status, and none reported being unwell during the conference or subsequently. 13 secondary cases of COVID-19 were reported among family members of B1 in Malaysia and contacts of B7 in France.
Cluster C
The Ministry of Health in Singapore identified two people from Singapore (C3 and C4), with no recent travel history to China, who tested positive for SARS-CoV-2 from enhanced pneumonia surveillance. Activity mapping showed that both individuals had visited the same church on Jan 19, 2020. C5 was identified through active case-finding. Two other people with COVID-19 were subsequently linked to this cluster (C1 and C2, who are husband and wife). These individuals were Chinese nationals from Wuhan who arrived in Singapore on Jan 19, 2020. Re-interviews with C1 and C2 found they had also visited the church on the same day. All five people were asymptomatic during the church visit (figure 1 lower panels).
The church is an independent church that occasionally receives a few visitors from China at the Mandarin service conducted every Sunday.11 Although C1 and C2 were not church members, they attended the 2-h morning service when they travelled to Singapore. They left immediately after the service and did not report having lunch at the church. Based on closed-circuit camera findings, C5 occupied the same seat as did cases C1 and C2 at the prayer meeting after the morning service, but they did not recall meeting each other.
Among the 227 regular church members, 191 members were contacted, of whom 142 attended the church on Jan 19, 2020. Of these people, only two had travel history to Guangdong, China, 14 days before Jan 19, 2020; both reported being well. Six were unwell and referred for further management and none tested positive for SARS-CoV-2. 93 close contacts were placed under quarantine.
No additional cases linked to any of the three clusters were identified as of Feb 14, 2020.
Analysis of disease transmission data
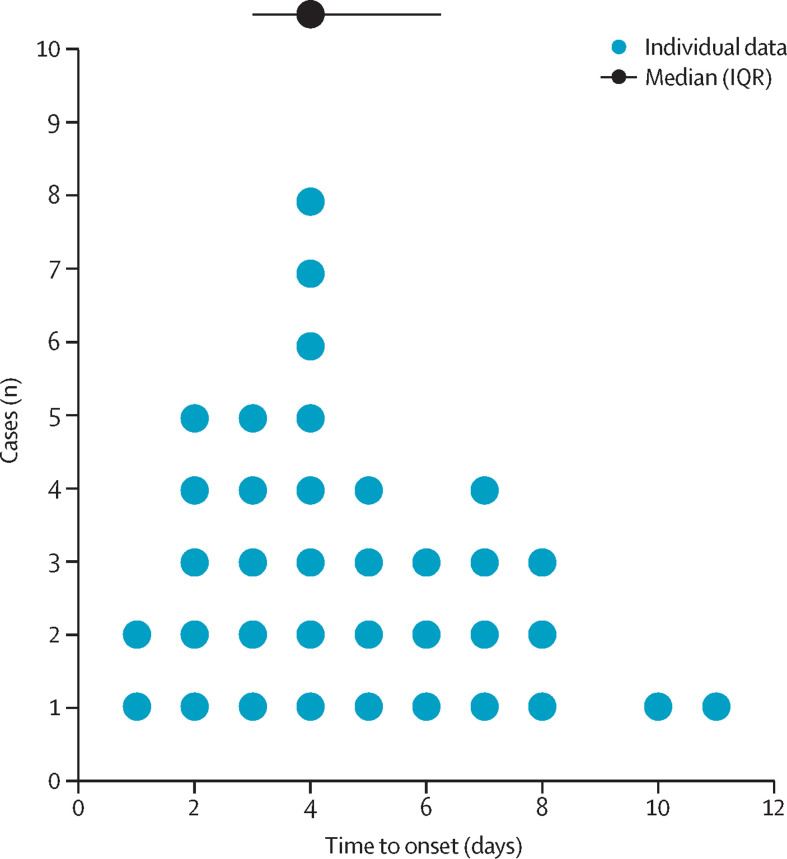
Although we were unable to identify the primary case or cases in each cluster with certainty, in cluster A, the cases in the two shops and the tour guide had inter-related interactions with the Guangxi tour group in which two cases were found. Exposures of the shop assistants were assumed to occur on Jan 23, 2020, and the tour guide on Jan 22, 2020, or Jan 23, 2020. In cluster C, the only overlap in activities was on Jan 19, 2020, when all five cases visited the church and exposures most likely occurred. For cluster B, we used information on reported activities to infer most likely infection times within the meeting. Excluding the household cluster, we had information on both estimated infection time and reported date of symptom onset for 19 people. The incubation periods are plotted in figure 2 . The median incubation period was 4 days (IQR 3–6). Without accounting for potential tertiary transmission within the household (infected by a case who was not the primary case), the serial interval for the three transmission pairs in the household cluster ranged between 3 days and 8 days.
Figure 2.
Incubation periods for cases with known probable exposure times
Median (IQR) time to onset was 4 days (IQR 3–6).
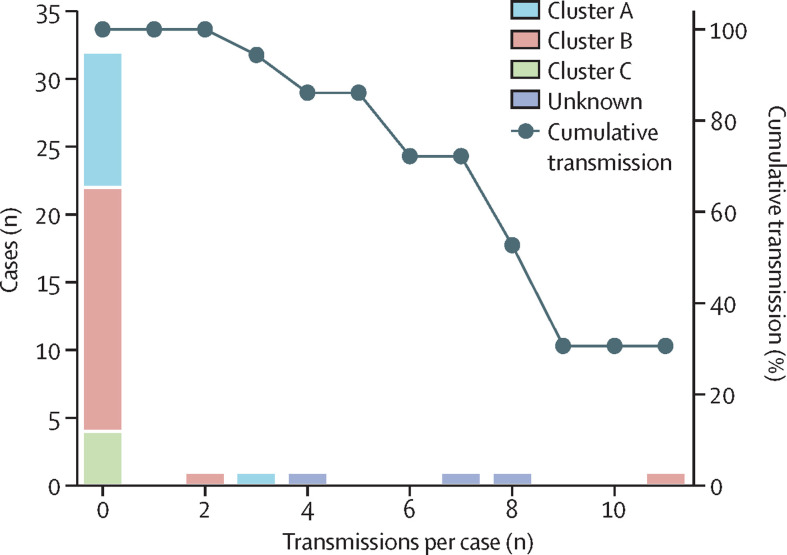
Assuming one unknown primary case seeded the outbreaks in each cluster, we noted that 31% of transmission pairs were associated with one individual (B7), and 32 observed cases had no onward transmission (figure 3 ).
Figure 3.
Probable secondary cases arising from each COVID-19 case
COVID-19=coronavirus disease 2019.
Clinical findings
Of 17 locally confirmed cases, fever and cough were the two most common symptoms, reported in 15 (88%) and 14 (82%) individuals, respectively (table). One case, a 6-month old male infant, was asymptomatic until one spike of fever 2 days into hospital admission. Pulmonary opacities were reported on chest radiography at admission in eight (53%) individuals, and developed over the course of admission in four additional people. Lymphopenia (<1·1 × 109 cells per L) was seen in six people and thrombocytopenia (<150 × 109 cells per L) in four individuals over the course of admission. Median time from symptom onset to hospital admission was 4 days (IQR 3–9).
The clinical course was uncomplicated for most individuals, with resolution of symptoms over the first few days. Hospital admission was prolonged because of persistently positive SARS-CoV-2 PCR from nasopharyngeal swab testing (median 6 days, range 3–9). One individual needed supplemental oxygen via nasal prongs and another two developed acute respiratory distress requiring intubation and intensive care. Four individuals received experimental treatment of lopinavir with ritonavir. No deaths were recorded in these three clusters as of March 7, 2020.
Discussion
We report three clusters showing local transmission of COVID-19 in Singapore. The three clusters involved a Chinese tour group, company conference, and a church and show the transmissibility of COVID-19 in community settings beyond household clusters. A household cluster was previously reported in Shenzhen, Guangdong, China.12 These findings have implications for public-health measures and outbreak investigations that other countries might consider to detect and contain transmission.
The first indication of human-to-human transmission in Singapore was detected 11 days after confirmation of the first imported case. China imposed a lockdown of Wuhan on Jan 23, 2020, and suspended all outgoing tour groups beginning Jan 27, 2020. Despite these measures, local clusters were subsequently identified in Singapore, with probable links to travellers from China before the measures to curb travel were implemented. Although the primary case or cases in all three clusters cannot be conclusively identified, they are postulated to be tourists or business visitors from China. The tour group implicated in cluster A originated from Guangxi at a time when relatively few cases had been reported in that region of China.13 Temperature screening for inbound travellers on flights from Wuhan was implemented in Singapore on Jan 3, 2020, and expanded to all flights from China on Jan 22, 2020. Nonetheless, it is unlikely that these primary cases could be identified by temperature screening, because there was no indication that they were febrile on arrival.
Therefore, it is important that countries, particularly those with a high travel volume from China, enhance their surveillance system to identify local cases, not merely among people with a travel history to China because cases could be present in the community. The local cases in cluster C were identified through enhanced pneumonia surveillance of people who had no history of travel to China, whereas the initial cases in cluster A were identified because of heightened suspicion by health-care workers, leading to testing. Among the first 84 confirmed cases in Singapore, ten were detected by enhanced pneumonia surveillance and testing of patients in intensive care units, and another eight affected individuals were detected based on doctors' discretion to test patients whom they viewed with suspicion for clinical or epidemiological reasons. Such surveillance systems are, therefore, important to identify cases in the community who would be missed if the focus were only on travellers, and they have enabled prompt investigation and containment measures. Furthermore, with swift response in contact tracing and quarantine of close contacts, two close contacts developed symptoms and were confirmed to be infected with SARS-CoV-2 during their period of quarantine, ensuring no further onward transmission of the virus. Only two of 425 close contacts identified by contact tracing developed COVID-19 (ie, most cases identified in the clusters did not transmit the SARS-CoV-2 virus to their close contacts), raising the hypothesis that a few spreading events can result in clusters of transmission, whereas for most cases, transmission ended.
The ease of international travel makes containment difficult. Cluster B was identified because of sharing of case data in Malaysia through the IHR focal point, and Singapore shared information on attendees at the company conference to respective IHR focal points where participants at the conference had originated. This work led to early identification of cases globally and highlights the importance of international cooperation and sharing of information under IHR to aid in active case-finding and containment.
The cases of COVID-19 in these three clusters are probably attributable to close or prolonged interactions. Direct physical contact was reported between shop assistants and tourists at the health products shop (cluster A). Handshaking and physical contact during team-building activities and sharing of meals were reported among participants of the business meeting (cluster B).14 Therefore, direct transmission could be possible by contact or indirect transmission (eg, via fomites and shared food). We have shown environmental contamination of common-touch surfaces in the isolation room of a confirmed case.15 This finding highlights the importance of emphasising personal and hand hygiene as a key public-health message that countries should adopt.
Recall bias could affect the accuracy of symptom-onset dates reported by cases. In cluster A, the date of onset of symptoms for AC2 was uncertain because the individual only sought primary-care treatment on Jan 30, 2020, 7 days after reported onset of symptoms. Other exposures are plausible. AC2 reported having symptoms on the day of the tour group's arrival, and we could postulate that AC2 acquired infection from other tourists before Jan 23, 2020, and seeded infections among colleagues, the tour guide, and the two people from Guangxi on Jan 23, 2020. However, case AJ1 had no interactions with AC2, unless AC2 acquired infection serendipitously at a similar time, independently. Similarly, in cluster C, C1 did not report symptoms until 5 days and C2 until 3 days, after attending church, and this difference could be attributable to recall bias of symptom-onset dates, particularly if symptoms were mild.
Other study limitations include the small sample size used to ascertain the incubation period, because primary cases could not be identified with certainty. Moreover, symptom-onset dates and the movement of and exposure history of cases detected overseas were either based on media reports or were unknown. Based on symptom-onset dates of 17 local cases, the median incubation period (4 days) corroborates other published findings.16, 17 Although there is interest on asymptomatic transmission, we are unable to address this point in our study, and further studies should be done to better understand disease transmissibility of asymptomatic cases.
In conclusion, as importation and local transmission could have occurred in other countries before the lockdown of Wuhan and institution of travel restrictions by China, local clusters outside China can be expected and efforts should be focused on surveillance for locally acquired cases and containment efforts to prevent widespread community transmission. It is important for countries to do active case-finding among close contacts of cases to prevent clusters from spreading.
Contributors
RP, CJC, BEY, and SC contributed to the literature search, data collection, data analysis, and writing of the report. HEC and ARC contributed to the data analysis on disease transmission and figures. SM-S, TMM, LC and RVTPL contributed to the laboratory testing and analysis. MPHST, CP, ML, JL, and VTJK contributed to the epidemiological data collection and analysis. MI-CC, DH, Y-SL and DCL contributed to the study design and writing of the report. VJML contributed to study design, the literature search, data collection, data analysis, and writing of the report. All authors read and approved the final report.
Singapore 2019 Novel Coronavirus Outbreak Research Team
Kai-qian Kam, Shirin Kalimuddin, Seow Yen Tan, Jiashen Loh, Koh Cheng Thoon, Shawn Vasoo, Wei Xin Khong, Nur-Afidah Suhaimi, Sherlynn J H Chan, Emma Zhang, Olivia Oh, Albert Ty, Charlene Tow, Yi Xian Chua, Wei Liang Chaw, Yixiang Ng, Farid Abdul-Rahman, Shafiq Sahib, Zheng Zhao, Cheryl Tang, Constance Low, Ee Hui Goh, Georgina Lim, Yan'an Hou, Imran Roshan, James Tan, Kelly Foo, Khine Nandar, Lalitha Kurupatham, Pei Pei Chan, Pream Raj, Yijun Lin, Zubaidah Said, Anne Lee, Cherie See, Jessey Markose, Joanna Tan, Guanhao Chan, Wanhan See, Xinyi Peh, Vincent Cai, Wen Kai Chen, Zongbin Li, Roy Soo, Angela L P Chow, Wycliffe Wei, Aysha Farwin, and Li Wei Ang.
Declaration of interests
We declare no competing interests.
Contributor Information
Singapore 2019 Novel Coronavirus Outbreak Research Team:
Kai-qian Kam, Shirin Kalimuddin, Seow Yen Tan, Jiashen Loh, Koh Cheng Thoon, Shawn Vasoo, Wei Xin Khong, Nur-Afidah Suhaimi, Sherlynn JH Chan, Emma Zhang, Olivia Oh, Albert Ty, Charlene Tow, Yi Xian Chua, Wei Liang Chaw, Yixiang Ng, Farid Abdul-Rahman, Shafiq Sahib, Zheng Zhao, Cheryl Tang, Constance Low, Ee Hui Goh, Georgina Lim, Yan'an Hou, Imran Roshan, James Tan, Kelly Foo, Khine Nandar, Lalitha Kurupatham, Pei Pei Chan, Pream Raj, Yijun Lin, Zubaidah Said, Anne Lee, Cherie See, Jessey Markose, Joanna Tan, Guanhao Chan, Wanhan See, Xinyi Peh, Vincent Cai, Wen Kai Chen, Zongbin Li, Roy Soo, Angela LP Chow, Wycliffe Wei, Aysha Farwin, and Li Wei Ang
Supplementary Material
References
- 1.Wuhan Municipal Health Commission Report on current pneumonia epidemic situation in the city. (In Chinese.) Dec 31, 2019. http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989
- 2.The State Council, People's Republic of China Wuhan novel coronavirus prevention and control command notice (no 1). (In Chinese.) Jan 23, 2020. http://www.gov.cn/xinwen/2020-01/23/content_5471751.htm
- 3.DW.com. Wuhan pneumonia virus continues to spread, Hubei orders 15 cities to be closed. (In Chinese.) Jan 24, 2020. https://www.dw.com/zh/a-52132769
- 4.World Health Organization Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) Jan 30, 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 5.World Health Organization Coronavirus disease 2019 (COVID-2019): situation report—33. Feb 22, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200222-sitrep-33-covid-19.pdf
- 6.Ministry of Health, Singapore Confirmed imported case of novel coronavirus infection in Singapore; multi-ministry taskforce ramps up precautionary measures. Jan 23, 2020. https://www.moh.gov.sg/news-highlights/details/confirmed-imported-case-of-novel-coronavirus-infection-in-singapore-multi-ministry-taskforce-ramps-up-precautionary-measures
- 7.Singapore Statutes Online Infectious Diseases Act, chapter 137. July 31, 2003. https://sso.agc.gov.sg/Act/IDA1976 (accessed Feb 29, 2020)
- 8.People's Government of Guangxi Zhuang Autonomous Region Emergency notice to find contacts of confirmed cases. (In Chinese.) Feb 3, 2020. http://m.gxzf.gov.cn/gxyw/20200203-793378.shtml
- 9.Yulin News 8 confirmed cases in Yulin City are in stable condition. (In Chinese.) Feb 3, 2020. http://m.gxylnews.com/html/news/2020/02/189458.html
- 10.Guangxi News Network 2 new cases of pneumonia confirmed by new coronavirus infection in Yulin, a total of 7 cases. (In Chinese) Feb 2, 2020. https://v.gxnews.com.cn/a/19225623
- 11.The Life Church and Missions About the church. (In Chinese) http://www.lifechurchmissions.com/ChurchHistory.aspx
- 12.Chan JF-W, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Novel coronavirus (2019-nCoV): situation report—3. Jan 23, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200123-sitrep-3-2019-ncov.pdf
- 14.Channel NewsAsia 3 new coronavirus cases in South Korea; 2 men had travelled to Singapore for conference. Feb 5, 2020. https://www.channelnewsasia.com/news/asia/wuhan-virus-coronavirus-south-korea-cases-12394934
- 15.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 doi: 10.1001/jama.2020.3227. published online March 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of 2019-nCoV from publicly reported confirmed cases: estimation and application. Feb 4, 2020. https://www.medrxiv.org/content/10.1101/2020.02.02.20020016v1 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.