Abstract
In the previous stage, there were too many patients with Corona virus disease 2019 (COVID-19) in Wuhan. Ordinary people, patients, even doctors, had a great sense of desperate. On the one hand, almost all doctors participated in the treatment of patients of COVID-19. On the other hand, the government restricted residents to go out, and the sick people were also afraid of being infected with COVID-19 when seeking medical treatment. Whether cancer patients seek medical treatment or not has become a contradiction for a long time. Our Viewpoint paper is to provide a positive signal to doctors and patients that patients with in the middle or advanced stage of cancer can receive radiotherapy and/or chemotherapy normally under protective measures.
Keywords: Radiotherapy, chemotherapy, COVID-19
Introduction
The COVID-19 (caused by SARS-CoV-2) has spread all over the world, men and women, young and old. Limited reports point out the infection rate of SARS-CoV-2 in patients with cancer from their institution at 0.79%, which was higher than the cumulative incidence of all diagnosed COVID-19 [1]. There is also a report about a patient died of COVID-19 after lung lobectomy for adenocarcinoma [2]. Hospitals are scary places to be, especially during the COVID-19 pandemic. Patients won’t come to the hospital as a last resort. It is generally known that cancer patients needed undergoing radiotherapy and chemotherapy in the middle or advanced stages. If they infected COVID-19 during this period, what’re means to them? Although the current guidelines suggested that should reducing the frequency of hospital visits during COVID-19 pandemic [1], we also need to take into account the patient’s desire to prolong their life through limited treatment. Given the limited number of clinical cases reported about “should patients stop their radiotherapy or chemotherapy during the COVID-19 pandemic?”, we would like to report a case and share some experiences.
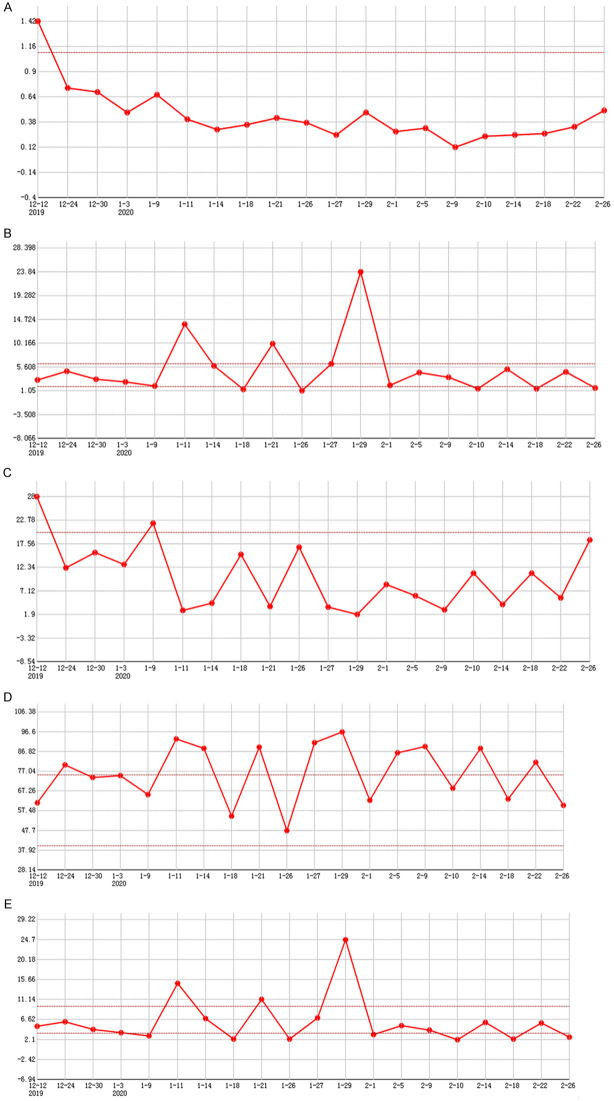
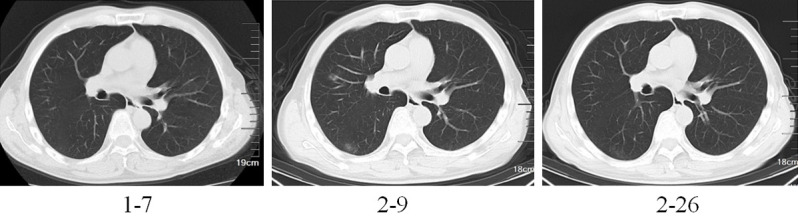
A 51-year-old man with pharynx discomfort was received nasopharyngoscopy examination and histopathological examination which indicated that the nasopharynx had non-keratotic squamous cell carcinoma. He has a ten-year history of chronic nephritis with no obvious edema, was treated intermittently with traditional Chinese medicine. There was no abnormal renal function on admission. After multidisciplinary consultation and discussions, he received image-guided radiotherapy at the lesion site (PTV70: 69.96GY/33FX) from December 13, 2019 and two rounds of chemotherapy with loplatin 35 mg/m2 (on December 18, 2019 and January 8, 2020). During the period of radiotherapy and chemotherapy, the vital signs of the patients were stable, and other biochemical indexes were basically normal except for hyponatremia and hypochloremia within 2 weeks (the lowest sodium value was 116.1 mmol/L and chlorine was 88.0 mmol/L on December 24, 2019). He ate outside the hospital from his own will since he was hospitalized. This may have set a stage about infecting COVID-19 because of a possible exposure history of densely populated places. His symptoms started on 9 February, 2020, From stuffy nose to fever (with a maximum axillary temperature of 38.0°C). He was performed a chest computed tomography examination immediately, which showed that new ground-glass shadows appeared in the right upper lobe, right lower lobe and posterior basal segment (Figure 1). Then, his nucleic acid detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from pharynx swab confirmed positive. His other details of blood routine examination showed no special abnormalities (Figure 2). He was transferred to the Department of Infectious Disease immediately, where he received the treatment such as antiviral treatment (ribavirin for 20 days, oseltamivir for 7 days, atomization of interferon a-1b for 19 days), immunity enhancement (thymic pentapeptide for 20 days, immunoglobulin for 12 days), anti-inflammatory treatment (moxifloxacin for 13 days, glucocorticoid for 20 days), oxygen inhalation and so on. During the treatment, the patient’s condition did not progress further. Chest CT showed that his double pneumonia was gradually absorbed. He was discharged after the twice negative RNA nucleic acid test of SARS-CoV-2 with the pharynx swab interval of 24 h.
Figure 1.
Male, 51 years old, chest CT before chemotherapy showed no abnormalities. Ground glass shadow revealed in the upper and lower lobe of the right lung after the onset of fever in February 9, 2020. A re-examination of CT found that the shadow was absorbed after active treatment on February 26, 2020.
Figure 2.
(A) is the absolute value of lymphocytes, (B) is the percentage of lymphocytes, (C) is the absolute value of neutrophils, (D) is the percentage of neutrophils, (E) is the absolute value of leukocytes.
The above cancer patient, who infected COVID-19 during radiotherapy or chemotherapy period. He received a good result through aggressive treatment such as ribavirin, oseltamivir, glucocorticoid, oxygen inhalation and so on. There is no definite clinical data to show that cancer patients were more susceptible to the SARS-CoV-2, and limited literature has not been able to prove that radiotherapy or chemotherapy increases the risk of infection. We believe that patients with the middle or advanced stage of cancer could be treated with radiotherapy or/and chemotherapy as scheduled under strict and tight protection.
The reasons are as follows: First, COVID-19 is preventable and controllable, which has been confirmed in some countries at present [3]. Second, cancer patients will have a cautious attitude to protect against COVID-19 when undergoing radiotherapy and/or chemotherapy in the middle or late stages [4]. They will have an in-depth understanding of hand washing, using higher-level medical protective masks, reducing aggregation, and so on. Third, both doctors and cancer patients are more alert to patients’ vital signs during in hospital. Cancer patients’ body temperature will be closely monitored, whom detailed medical history would be excavated deeply inquired. Even if these patients were infected with the SARS-CoV-2, they could be diagnosed at the early stage. Patients usually have a good outcome if they receive early treatment, such this 51-year-old man. Fourth, cancer patients want to live longer, otherwise why get radiotherapy and/or chemotherapy? As medical practitioners, we should try our best to help them realize this wish.
When going to give plans with radiotherapy and/or chemotherapy on these cancer patients in high-risk areas of the epidemic, medical practitioners should take the following measures as much as possible: First, give them enough scientific knowledge to learn how to prevent infection. Second, provide cancer patients a safe access from the treatment room and ward. Third, keep clean and free of SARS-CoV-2 residues in the radiotherapy room [5]. Fourth, refuse all suspicious personnel to contact them, including suspicious doctors.
Disclosure of conflict of interest
None.
References
- 1.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020 doi: 10.1001/jamaoncol.2020.0980. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azman AS, Luquero FJ. From China: hope and lessons for COVID-19 control. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30264-4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei W, Jiang H, Chen W, Zhou Y, Guo S, Zhong G, Zhou H, Wang S, Zhang H, Jiang W, Liu ZG. How should we implement radiotherapy for cancer patients in China during the endemic period of COVID-19? Radiother Oncol. 2020;147:100–102. doi: 10.1016/j.radonc.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao Y, Pan H, She Q, Wang F, Chen M. Prevention of SARS-CoV-2 infection in patients with decompensated cirrhosis. Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/S2468-1253(20)30080-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]