Abstract
It is now widely accepted that most human cancers, including colorectal cancers (CRCs), develop from premalignant lesions through a long-term multistep process. Host immunity is a key determinant that maintains most premalignant lesions in a stable state via immunosurveillance. However, premalignant cells use diverse strategies to escape host immunosurveillance. A switch in the immune function from immunosurveillance to immunosuppression facilitates the progression of premalignant lesions to established CRCs. This review summarizes the recent progress in understanding alterations in the immune landscape, including immune cell compositions, functions and cytokine products, in the premalignant stage of CRC and provides an updated discussion on its translational significance along the colorectal adenoma-carcinoma sequence.
Keywords: Colorectum, premalignant lesion, immunity, immune cell, cytokine
Introduction
In humans, cancer appears to develop through a long-term premalignant stage accompanied by substantial alterations in histological, immunological, genetic and molecular aspects [1,2]. In support of this observation, numerous clinical studies have revealed that most colorectal cancers (CRCs) appear to develop through a long-term premalignant stage. Clinically, adenoma, familial adenomatous polyposis, Peutz-Jeghers syndrome, juvenile polyposis, and dysplasia in inflammatory bowel diseases (IBDs) have been frequently recognized as premalignant lesions of CRC. Clinical data suggest that adenoma is the most common premalignant lesion and that CRCs develop predominantly from adenomas, with other types accounting for less than 5% of the overall incidence of CRC [1,3]. This causal relationship between adenoma and CRC has been referred to as the colorectal adenoma-carcinoma sequence.
According to the immunoediting hypothesis, the emergence of a premalignant adenoma in the colorectum induces a three-phase immune response (elimination, equilibrium and escape) [4]. In the elimination (immunosurveillance) phase, the host immune system can theoretically eradicate premalignant cells and induce early regression of premalignant lesions. However, spontaneous regression of premalignant lesions rejected by the host immune system is difficult to document, as early-stage premalignant lesions are usually very small and rarely observed in the clinic. In the equilibrium phase, some premalignant cells use various strategies to acquire the ability to evade host immunosurveillance, and premalignant lesions persist in the body for a long time. In the escape phase, the premalignant cells that acquired the ability to evade immunosurveillance escape immune control, undergo uncontrolled invasive growth, and finally develop into malignancies. Therefore, the change in the immune landscape from immunosurveillance to immunosuppression is a prerequisite for the progression of a premalignant lesion to a cancerous lesion [5].
In this review, we focus on the current research progress and understanding of immune alterations in immune cell compositions, functions and cytokine products at the premalignant stage and discuss the clinical translational significance of such changes on the progression of colorectal premalignant lesions to CRC.
Major types of immune cells present in premalignant tissues
Host immunity comprises many types of immune cells, and its relative function is modulated by various factors. To investigate the existence of immune cells in colorectal premalignant (adenoma) lesions, the density, location and phenotypes of these cells have been studied. To date, studies have shown that the adenoma microenvironment contains a high density of immune cells that might exert both antitumor and protumor functions [5-9]. These immune cells are densely located in both the adenomatous epithelium and stroma [7-9] and have complex interactions with premalignant cells that determine whether premalignant lesions remain stable or progress [10,11].
From a phenotypic perspective, T lymphocytes and macrophages are the most frequently observed immune cells in premalignant lesions and are named tumor-infiltrating lymphocytes (TILs) and tumor-associated macrophages (TAMs). A markedly increased population of TILs has been reported in adenoma tissues, and most TILs are distributed in the stromal region and infiltrate into the adenomatous epithelium. TILs in adenoma tissues are CD4-positive TH cells and CD8-positive cytotoxic T lymphocytes (CTLs) [12,13]. CD4-positive TH cells play a critical role in regulating the host immune response. Their function in the tumor microenvironment is very complex and variable and depends on the characterization of subsets and conditions. CD8-positive CTLs play a critical role in eliminating transformed cells by releasing toxic granules upon recognizing specific tumor antigenic peptides presented on the surface of tumor cells. More recently, Chang et al. demonstrated a striking immune activation profile characterized by CD4-positive T cells, the proinflammatory cytokines tumor necrosis factor (TNF)-α and interleukin (IL)-12, and checkpoint molecules in patients with Lynch syndrome polyps; this profile was independent of the DNA mutation rate [14]. The impact of CD8-positive CTLs on the progression of oral premalignant lesions has been reported [15]. Phenotypic analysis of T lymphocytes along the human adenoma-carcinoma sequence revealed a higher population of CD8-positive CTLs in premalignant adenoma tissues than in CRC tissues [16]. Karlsson et al. examined the CD4-positive/CD8-positive T lymphocyte ratio in colitis-associated premalignant (dysplastic) lesions and found an increase in the CD4-positive/CD8-positive T lymphocyte ratio in sentinel lymph nodes draining dysplastic epithelium compared to those draining normal mucosa [5]. This increase correlated with the degree of dysplasia, as reflected by a significant increase in the ratio in low-grade dysplasia compared to that in indefinite dysplastic lesions. Their observation suggests that host immunosurveillance plays an important role in suppressing premalignant lesions in patients with long-standing ulcerative colitis [5]. Regulatory T cells (Tregs) can create an immunosuppressive milieu that restricts the release of cytotoxic granules from CTLs, which prevents killing of premalignant cells. Jang et al. observed that a decrease in the CD8-positive T cell/Treg ratio may contribute to the generation of an immune environment suitable for the progression of adenomas to CRCs [17]. Thus, the general consensus seems to indicate that CTLs are critical for host antitumor immunity [18].
Several new subsets of TH lymphocytes, i.e., TH17 cells have been identified, and their roles have been studied primarily in premalignant lesions [19]. One study revealed that defects in mothers against decapentaplegic homolog 4 (Smad4) and transforming growth factor (TGF)-β could result in spontaneous development of polyps in the upper part of the gastrointestinal tract of mice, which exhibited increased levels of transcripts encoding IL-1β, IL-6, IL-11, TGF-β and TNF-α; additionally, lamina propria cells isolated from premalignant polyp lesions contained an abundance of IL-17A-expressing TH17 cells [20]. These results support the hypothesis that the premalignant lesions may have arisen because of unchecked TH17 cell activity. Increased levels of TH17 cells and the TH17 cytokine IL-17A have been found in human premalignant tissues and premalignant tongue tissue of carcinogen-treated mice, but these levels declined and were replaced with an immune inhibitory cell phenotype after the final establishment of oral cancers [2]. Similarly, we also reported that the density of IL-17A-labeled TH17 cells was significantly increased in colorectal adenoma tissues [21,22]. In addition, the involvement of other new TH subsets, such as TH9 and TH22, in the pathogenesis of CRC has been recently discussed [19]; however, the exact role of these subsets in the premalignant stage remains to be investigated.
Natural killer (NK) cells are large granular lymphocytes, and previous studies have revealed that they play an important tumor surveillance role in innate immunity [23]. However, recent studies reported that NK cells can also be classified into type I and type II according to their function. CD1d-restricted invariant, type I, natural killer T (iNKT) cells are early responding, potent regulatory cells of immune responses. iNKT cells can also perform tumor surveillance and provide natural protection against the emergence of cancer. Numerous studies have revealed that iNKT cells not only have an important regulatory function in inflammation development but also are involved in tumor immunosurveillance [24]. By establishing a transgenic mouse model that expresses high levels of CD1d and a T cell receptor (TCR) from an autoreactive type II NKT cell, Liao et al. showed that type II NKT cells significantly contribute to intestinal inflammation and colitis in mice [25]. Wang et al. studied iNKT cell-mediated regulation of tumor immunity in the Apcmin/+ mouse adenoma-carcinoma sequence model [26] and found that the deficiency of iNKT cells in APCMin/+ mice (generated by crossing APCMin/+ mice with iNKT deficient mice) resulted in a markedly decreased number of intestinal polyps, which was associated with enriched populations of immunosuppressive cells such as IL-10- and IL-17-producing cells and a reduced frequency of Tregs in the polyps. In addition, a switch of the macrophage phenotype from M2 to M1 occurred, and the expression level of TH1 cytokines, such as interferon (IFN)-γ), was increased in adenomatous tissues. These results suggest that iNKT cells play an important role in promoting intestinal polyp formation; this role is thought to enhance Treg cell accumulation and suppress host antitumor TH1 immunity. These findings may open new avenues for understanding the effect of immune cells on the establishment of premalignant adenomatous lesions.
Macrophages are another common type of immune cell in premalignant lesions. A novel classification of macrophages based on their function has been hypothesized: M1-type macrophages exert antitumor effects, whereas M2-type macrophages exert protumor effects [27]. During cancer development, the functional changes in macrophages in the premalignant/malignant stages that determine the site to which they migrate probably depends on the phenotypes present in the tumor microenvironment and on the milieu factors [28-30]. In general, scientists have postulated that a functional switch of macrophages from the M1 to the M2 phenotype might contribute to tumor progression [27,28,30]. Identifying such functional changes in the development of CRC could be important because a new immunotherapeutic strategy aimed at blocking the functional shift from M1 to M2 may be a promising approach to prevent human cancer development [27]. Recently, Soncin et al. [31] examined the role of the microenvironment in the self-renewal of tumor-promoting macrophages in adenomatous polyps obtained from ApcMin/+ mice, a widely used animal model for the study of intestinal tumorigenesis. They found that macrophages expanded in situ in adenomas by self-renewal, without recruitment of new cells. Further RNA sequencing (RNA-seq) and Ki-67 analyses showed that macrophages in polyps were actively cycling. Similarly, the tumor microenvironment was also conducive to the self-renewal of tumor-associated macrophages.
Maglietta and colleagues compared the density of immune cells between adenomatous polypoid lesions and nonpolypoid lesions [32] and reported that the density of immune cells (mainly T lymphocytes and macrophages) in premalignant polypoid lesions was significantly higher than that in nonpolypoid lesions. Certain markers exhibited significant size-related differences regardless of lesion morphology. In addition, large neoplasms have more stromal immune cells than small neoplasms [32]. Infiltration of T cells and macrophages is more obvious in CRC tissues than in normal tissues, and the populations of both of these cells in the CRC stroma and epithelium are greatly increased [6,7]. Whether the density of macrophages in the tumor microenvironment can be used as a prognostic predictor is still under debate [27,29,33]; however, CRC patients with a higher population of TILs tend to have better prognoses than those with a lower population of TILs [10,34,35]. In addition, phenotypic analysis demonstrated that a high population of CD8-positive T cells in the CRC epithelium is associated with a favorable prognosis of patients with CRCs [36]. Since many new subsets of TH cells have been identified, prompt evaluation of their importance is necessary.
Dendritic cells (DCs) are the most efficient antigen-presenting cells and play a relevant role in tumors by exerting differential protumorigenic and antitumorigenic effects. DC defects in CRC have been studied [37]. Michielsen et al. showed that conditioned media collected from metastatic colorectal cancer patients significantly inhibited the maturation of DCs [38]. They further found that tumor-conditioned media contained high levels of the chemokines CCL2, CXCL1, and CXCL5 in addition to vascular endothelial growth factor (VEGF), which might significantly inhibit upregulation of CD86, CD83, CD54 and HLA-DR on monocyte-derived dendritic cells in response to lipopolysaccharide (LPS) [39]. Orsini and colleagues examined the maturation and generation of DCs from monocytes in patients with CRC and found that DCs from CRC patients had lower expression levels of costimulatory molecules and a lower ability to present antigens to allogeneic T cells than DCs from healthy controls [40]. At the premalignant stage, transformed cells can develop diverse mechanisms that suppress the generation, maturation and function of DCs to escape immune recognition and elimination [41]. Changes in the maturation status of DCs in patients with cancers might result in changes in the density and location of mature DCs (mDCs) and immature DCs (iDCs) in the tumor microenvironment. Indeed, Bell et al. showed that in breast cancer tissue, iDCs reside predominantly within the tumor center, while mDCs reside in peritumoral regions [42]. Moreover, we previously demonstrated that mDC density was slightly decreased in premalignant adenoma tissues but significantly decreased in CRC tissues, whereas the iDC density was decreased in both adenoma and CRC tissues compared with control tissues [8]. The differentiation of DCs from monocytes is modulated by many factors. Cyclooxygenase-2 (COX-2) is an important factor regulating DC maturation and function. Our results showed that the mRNA level of COX-2 gradually increased from the adenoma stage to the CRC stage, and double immunofluorescence images showed that the PGE2 receptors EP2 and EP4 downstream of COX-2 were clearly expressed in DCs. These findings imply a possible regulatory pathway through which COX-2 mediates DC differentiation, maturation and function across the premalignant-malignant transition [43]. The effect of DCs on initiating host antitumor immunity is mediated via IL-12 production. By using real-time PCR and immunohistochemistry, we showed that both the mRNA and protein expression levels of IL-12 are highly increased in premalignant adenoma tissues and decreased in CRC tissues compared with healthy control tissues [44]. Such results suggest that DCs undergo phenotypic and cytokine product changes between the premalignant adenoma stage and the CRC stage.
One proposed strategy by which premalignant cells escape immunosurveillance is to suppress host antitumor function by recruiting immunosuppressive cells into the tumor microenvironment [45]. Tregs are a subpopulation of T cells that play a critical role in the maintenance of immunological tolerance and homeostasis [46]. Considerable evidence suggests that Tregs are the key determinant of immunosuppressive functions and significantly inhibit host antitumor immunity in various types of human malignances. Regarding the role of Tregs in CRC, the majority of current studies are conducted in established CRCs, and only a few studies are performed in premalignant adenomas. The study by Lan et al. [21] reported an increased mRNA expression level of FoxP3 (a specific biomarker for Tregs) in human colorectal adenomas. We examined the dynamics of FoxP3-labeled Tregs along the human colorectal adenoma-carcinoma sequence. Our data showed that the population of Tregs was significantly increased in adenoma tissues compared with control tissues and was even higher in CRC tissues than in adenoma tissues [9]. Furthermore, we showed that the levels of the Treg-immunosuppressive cytokines IL-10 and TGF-β were also increased in premalignant adenoma lesions [9,47], indicating a potential mechanism by which Tregs contribute to establishing an immunosuppressive milieu at the adenoma stage [9].
Myeloid-derived suppressor cells (MDSCs) can significantly dampen host antitumor immune function and promote tumor development. Possible mechanisms include enhanced induction of immunosuppressive cells, blockade of lymphocyte homing and functions and expression of negative immune checkpoint molecules [48-50]. Expansion of MDSCs in the tumor microenvironment is modulated by a vast network of tumor-derived factors, including PGE2, IL-1β, IL-6, IL-10, and TGF-β [51], the levels of which have been reported to increase in premalignant adenoma tissues [8,44,52]. Several studies have examined the importance and mechanisms of MDSCs in premalignant colorectal lesions. For example, Ma et al. found that an increase in MDSCs started from premalignant lesions and persisted to malignant lesions in both the colon and pancreas [53]. Further studies revealed that the chemokines CCL2 and CXCR2 could modulate the protumor effect of MDSCs in colorectal premalignant lesions [54,55]. Jayakumar A and Bothwell ALM demonstrated that the pro-polyp formation effect of the transcription factor Stat6 is mediated through stimulation of MDSC expansion but inhibition of CD8-positive T cells in the ApcMin/+ mouse model [56].
In summary, during the progression of a premalignant lesion to CRC, immune cells undergo phenotypic and functional changes (Table 1). Some immune cells, such as CD8-positive CTLs, play a critical role in initiating host anticancer immunity. However, immunosuppressive immune cells, such as Tregs, MDSCs and M2 macrophages, also start to accumulate in the premalignant adenoma microenvironment, which might contribute to the establishment of an immunosuppressive milieu and then to the progression of premalignant adenomas to CRCs (Figure 1).
Table 1.
Summary of major type of immune cell changes at the premalignant and malignant stages
| Cell type | Premalignant | Malignant |
|---|---|---|
| T lymphocytes | ||
| CD4 | ↑ | ↑ |
| CD8 | ↑ | ↓ |
| Macrophages | ||
| M1 | ↑ | ↓ |
| M2 | ↑ | ↑ |
| DCs | ||
| iDC | ↑ | ↑↑ |
| mDC | ↑ | ↓↓ |
| Tregs | ↑ | ↑ |
| MDSC | ↑ | ↑ |
| NK cells | ||
| iNKT | ↑ | ↑↑ |
| NKT | ↑ | ↓↓ |
Figure 1.
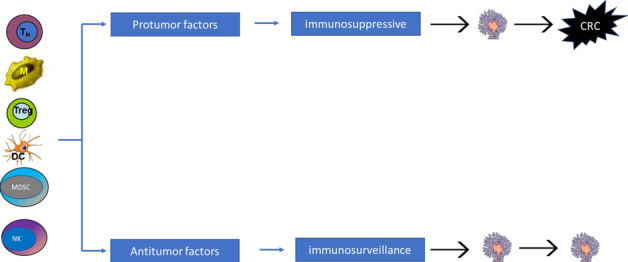
Schematic representation of immune cells contributing to functional immune changes at the premalignant stage. Altered immune cells contribute to the immune function status, which may determine the progression of a premalignant lesion to CRC.
Changes in the cytokine milieu at the premalignant stage
Cytokines released from immune cells are the most important factors in the modulation of host antitumor immunity, and many cytokines may also have a protumor effect and directly stimulate the proliferation and progression of premalignant adenomatous cells [57]. Therefore, a better evaluation of the cytokine profile from the premalignant to malignant stages may help explain the mechanisms of the host immunity switch from immunosurveillance to immunosuppression during the establishment of CRC [22,58-60]. We conducted a series of studies to examine the expression of relevant cytokines and observed alterations in the cytokine milieu along the adenoma-carcinoma sequence [21,22,44,52,61,62]. Our results showed that cytokine levels change significantly along this sequence [8,21,52,63-68]-the level of the TH1 cytokine IFN-γ, which is a key mediator of the host immune defense and plays an essential role in the initiation of antitumor immunity and immunoediting [69,70], is increased in adenomas but decreased in CRC; however, the levels of TH2 cytokines, such as IL-4, IL-6 and IL-10, are gradually increased from the adenoma stage to the CRC stage [44,71-73]. The important role of those cytokines in the pathogenesis of CRC has been well studied and summarized [57,64].
Perhaps the most compelling clinical evidence for an interactive link between TH cytokines and CRC development comes from recent observations that reported the protumor effect of cytokines produced by novel subsets of TH cells [19,74]. For instance, the TH 17 cytokine IL-17 has been suggested to participate in the establishment of premalignant adenomas. Several animal studies have shown that IL-17 promotes the establishment of adenomas in mice by directly stimulating cell transformation and enhancing angiogenesis [75-77]. We and others have examined the IL-17 expression level in both human adenomas and CRCs and found that it starts to increase from the adenoma stage and increases continuously to the CRC stage [22,78]. Notably, the increase in IL-17A mRNA levels in adenoma tissues is associated with the severity of dysplasia, and adenoma patients with higher degrees of dysplasia have higher levels of IL-17A mRNA than those with low degrees of dysplasia [22]. This finding suggests that TH17 cytokines promote the progression from premalignant lesions to cancer because research indicates that the degree of dysplasia in an adenoma is a histological hallmark for the risk of CRC, and adenoma patients with high grades of dysplasia may have a high risk of developing CRC [79]. IL-33 is another novel cytokine that has been reported to be involved in the pathogenesis of the adenoma-carcinoma sequence [61,74]. Previously, we examined the dynamics of IL-33 and its functional receptor ST2 along the human colorectal adenoma-carcinoma sequence and found that the expression levels of IL-33 and ST2 mRNA followed the order of adenoma > CRC > normal control [61]. Combining these results with important evidence obtained from previous studies of the role of IL-33 in CRC pathogenesis [80,81], we concluded that the IL-33/ST2 axis is involved in colorectal neoplastic transformation.
IL-21 is an IL-2 family cytokine produced by activated T cells to regulate immune responses [82]. Extensive evidence suggests that IL-21 has an antitumor capacity mediated through its multiple effects, including enhancing adaptive T cell immunity, promoting NK cell activation and antibody production, and regulating CD8-positive CTL expansion [82]. Regarding the role of IL-21 in colorectal tumorigenesis, recent animal studies have reported both protumor and antitumor effects of IL-21 in CRC mouse models [83,84]. More recently, we evaluated the role of IL-21 in human premalignant adenomas and CRCs. Our data show a large change in IL-21 mRNA expression, which began to increase at the adenoma stage and was maintained at an increased level at the CRC stage. In patients with CRC, this increase is significantly correlated with overall survival; patients with high IL-21 levels tend to have longer overall survival times than those with low IL-21 levels. Considering that studies have reported the antitumor capacity of IL-21 [85], the increased level of IL-21 in adenoma tissues may reflect enhanced host antitumor immunity elicited by transformed adenoma cells. In addition, our study showed that the IL-21 receptor is predominantly located in CD3-positive TILs in the adenoma stroma but not in transformed adenoma cells. This finding might imply that IL-21 is involved in adenoma transformation mainly via the regulation of immune cell function. Recently, the role of IL-9 and IL-22 in the pathogenesis of CRC has been discussed [19]. Current evidence indicates that these two cytokines may participate in the development of colonic inflammation; however, whether they contribute to the regulation of host immunity in the premalignant stage remains to be investigated.
Taken together, the current evidence indicates that proinflammatory cytokines produced by premalignant cells and surrounding stromal cells have undergone a significant change (Table 2) and may participate in modulating the progression of premalignant lesions to CRC lesions.
Table 2.
Summary of major cytokine changes in the premalignant and malignant milieu
| Cytokines | Premalignant | Malignant |
|---|---|---|
| IL-1 family | ||
| IL-1α | ↑ | ↑ |
| IL-1β | ↑ | ↑↑ |
| IL4 | ↑ | ↑ |
| IL-6 | ↑ | ↑ |
| IL-8 | ↑ | ↑ |
| IL-10 | ↑ | ↑ |
| TH17 cytokine | ||
| IL-17A | ↑ | ↑↑ |
| IL-17F | ↑ | ↑ |
| IL-21 | ↑ | ↓ |
| IL-22 | ↑ | ↑ |
| IL-33 | ↑ | ↑↑ |
| IFN-γ | ↑ | ↓↓ |
Translational significance of immune changes at the premalignant stage
Multiple lines of evidence demonstrate that an immune switch from immunosurveillance to immunosuppression favors the progression of premalignant lesions to malignant tumors. The translational significance of immunological parameters in patients with CRC has been intensively studied. Here, we limit our discussion to the translational significance of immunological parameters in premalignant adenomas.
Some researchers have reported that the transition from normal colorectal mucosa to adenoma and then to cancer is associated with a progressive decline in stromal CD8-positive T cell counts [17]. An Italian group recently examined the association of immune cells with the clinicopathological features of patients with adenomas [32] and found that the density of CD4-positive T lymphocyte infiltration increased significantly with polyp size and that larger and more dysplastic adenomas had higher CD4-positive T cell densities than smaller and less dysplastic adenomas. In addition, the densities of CD8-positive T cells and CD68-positive macrophages were significantly higher in polypoid adenomas than in nonpolypoid lesions. Moreover, the density of FoxP3-positive Tregs has been reported to be increased during progression through the premalignant adenomatous stage and early cancerous stages [17]. Substantial evidence suggests that the presence of immune cells in the tumor microenvironment may play a critical role in the development of cancers, including CRC. Human neutrophils are the most abundant subpopulation of leukocytes and are frequently seen in tumor tissues; numerous studies have reported that neutrophil infiltration is increased in CRC [86]. An elevated neutrophil/lymphocyte ratio (NLR) in peripheral blood may reflect the host immune response and is correlated with poor clinical outcomes in patients with advanced CRC [87]. Recently, a study reported that the NLR is significantly higher in neoplastic polyps than in nonneoplastic polyps [88]. Researchers have evaluated the increased NLR along the colorectal adenoma-carcinoma sequence and found that the NLR in patients with CRC is significantly higher than that in patients with adenoma [89]. In adenomas, the NLR is associated with polyp size, and patients with polyps larger than 10 mm tend to have significantly higher NLRs than those with polyps smaller than 10 mm [89]. Another study revealed that the leukocyte count, neutrophil ratio and NLR followed the order of CRC > adenoma > control [90]. Thus, the NLR may reflect the host systemic immune reaction elicited by colorectal tumorigenesis. The NLR is postulated to have predictive significance in distinguishing the neoplastic potential of colonic polyps and could be used as a noninvasive test for monitoring polyps [90].
Furthermore, the clinical translational significance of cytokine levels has been studied. The data demonstrate that an early, swift decrease in the TH1/TH2 cytokine ratio in peripheral blood was observed during progression from normal mucosa to adenoma and CRC [71,73]. We recently found that the tissue expression levels of IL-17A mRNA along the adenoma-carcinoma sequence followed the order of CRC > adenoma > control. Interestingly, the level of IL-17A mRNA in adenomatous tissues was associated with the severity of dysplasia, which is the main histological hallmark of disease progression towards CRC. A few studies have reported that the levels of cytokines may be associated with increased risk of adenoma. For example, Sasaki and colleagues found that increased serum levels of IL-6 are positively associated with the presence of colorectal adenoma [91-93]. Kim et al. reported that the prevalence of colorectal adenomas was associated with increased concentrations of IL-6 and TNF-α [60]. These findings are supported by data from a meta-analysis by Godos et al. [94], suggesting that elevated levels of cytokines are correlated with the risk of premalignant adenomas and contribute to the establishment of CRC. Although those data might support the idea that immunological changes reflect the progression of premalignant lesions, the immunological network in premalignant lesions is much more complex than previously thought. For example, the positive correlation between cytokine levels and adenoma risk was not confirmed by other studies [95,96]. Much additional work is needed.
Current clinical trials have documented that use of aspirin and nonaspirin nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the risk of colorectal adenomas. Therefore, approaches to recover the inhibited host antitumor immunity or block the protumor factors in premalignant adenomatous lesions could be novel immunotherapeutic strategies to prevent CRC. Current immunotherapeutic strategies for developed human cancers include anti-inflammatory mediator antibodies, immune adjuvants and vaccines, chimeric antigen receptor (CAR) T cell therapy, and CTL therapy based on antigen-specific humoral or immune cell-mediated suppression of human tumors. However, immunotherapy for premalignant lesions has been considered and tested only in animal models [2]. The current common clinical strategy for the treatment of premalignant adenomas is removal by colonoscopic resection techniques upon discovery. Thus, as adenomas are the main premalignant lesion in CRC, immunotherapeutic efficacy against adenomas has been documented only in animals. Wang and colleagues recently tested the efficacy of iNKT cell-directed immunotherapy and found that iNKT cell-directed therapy could subvert the natural polyp-enhancing effect of iNKT cells, overcome immunosuppression, and significantly decrease the polyp burden (number) in ApcMin/+ mice [97]. Because cytokine signals can be easily targeted pharmacologically, the effect of cytokine signal blockade on adenoma formation in mice has been examined. IL-6 has been considered a critical mediator of CRC development. Blockade of IL-6 or IL-6 receptor signaling in CRC animal models has been shown to significantly suppress the development of CRC [98]. In addition, studies have shown that IL-6 overexpression in ApcMin/+ mice increases the numbers and sizes of both intestinal and colon polyps [99], whereas administration of an anti-mouse IL-6 receptor antibody by intraperitoneal injection from 6 to 15 weeks of age results in a significantly decreased polyp burden and decreased mean polyp diameter in ApcMin/+ mice compared with mice in the control groups [100]. The therapeutic significance of blocking signals from other cytokines, i.e., IL-17 and IL-33, in CRC prevention has been tested in animal models. In mice, blockade of IL-17A significantly inhibited premalignant hyperplasia and CRC development [76], while blockade of IL-17 signaling significantly reduced the incidence of chemical-induced colon cancer [77]. We recently demonstrated that administration of an anti-IL-17A antibody by intraperitoneal injection for 4 weeks greatly decreased the number of inflammation-induced premalignant adenomatous polyps and CRCs in mice [67]. In addition, blocking signaling by the IL-33 receptor ST2 via administration of an antibody specific for ST2 was demonstrated to significantly inhibit the development of adenoma and CRC in ApcMin/+ mice [17]. In general, most immunotherapeutic studies performed in ApcMin/+ mice aim to validate the efficacy in preventing CRC development. Valid immunotherapeutic studies evaluating the prevention of premalignant adenoma remain to be performed.
Conclusion
The emergence of premalignant lesions in the colorectum elicits a strong immune response, during which immune cells undergo marked populational, phenotypic and functional changes that can significantly impair immunosurveillance and then help premalignant cells escape immune control (see Figure 2). Premalignant lesions will remain stable or grow slowly when antitumor immunity prevails but progressively increase in size, progress from a low degree to a high degree of dysplasia and finally develop into CRC once protumor forces overcome antitumor forces and immune escape occurs. A few translational studies have examined the preliminary efficacy of targeting immunosuppressive cells and enhancing antitumor immunity in preventing the progression of premalignant adenomas to CRCs. More precise studies are needed to further clarify the exact mechanisms of the immunosurveillance-immunosuppression switch, with special emphasis on the molecular pathways followed by immunosuppressive cells and immunomodulators to inhibit T cell functions and initiate the progression of colorectal premalignant lesions.
Figure 2.
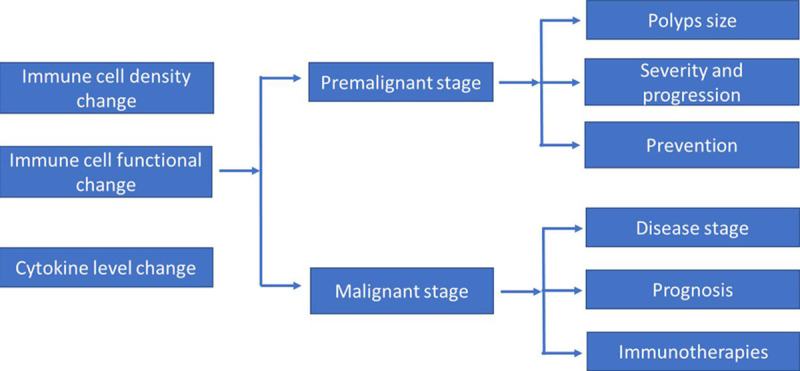
Schematic summary of the translational significance of immune factors at the premalignant and CRC stages. Current data suggest that altered immunological parameters might have translational significance at the premalignant and CRC stages.
Acknowledgements
This study were supported by the National Nature Science Foundation of China (Program No. 81071969) and the Medical Research Program, Northern Norway Regional Health Authority, Norway (Program No. SFP-44-04).
Disclosure of conflict of interest
None.
Abbreviations
- APC
antigen presenting cell
- CAR
chimeric antigen receptor
- COX2
cyclooxygenase 2
- CRC
colorectal cancer
- CTL
cytotoxic T lymphocyte
- iDC
immature dendritic cell
- IFN-γ
interferon γ
- IL
interleukin
- iNKT
invariant natural killer T
- LPS
lipopolysaccharide
- mDC
mature dendritic cell
- MDSCs
myeloid-derived suppressor cells
- MIC-1
macrophage inhibitory cytokine-1
- NSAIDs
non-aspirin nonsteroidal anti-inflammatory drugs
- NK
natural killer
- NLR
neutrophil-to-lymphocyte ratio
- PGE2
prostaglandin E2
- RNA-seq
RNA sequencing
- Smad4
mothers against decapentaplegic homolog 4
- TAM
tumor-associated macrophages
- TCR
T cell receptor
- TGF-β
transforming growth factor β
- TIL
tumor infiltrating lymphocyte
- TNF-α
tumor necrosis factor α
- Tregs
regulatory T cells
- VEGF
vascular endothelial growth factor
References
- 1.Conteduca V, Sansonno D, Russi S, Dammacco F. Precancerous colorectal lesions (Review) Int J Oncol. 2013;43:973–84. doi: 10.3892/ijo.2013.2041. [DOI] [PubMed] [Google Scholar]
- 2.Young MRI. Redirecting the focus of cancer immunotherapy to premalignant conditions. Cancer Lett. 2017;391:83–88. doi: 10.1016/j.canlet.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandouk F, Al Jerf F, Al-Halabi MH. Precancerous lesions in colorectal cancer. Gastroenterol Res Pract. 2013;2013:457901. doi: 10.1155/2013/457901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol. 2004;22:329–60. doi: 10.1146/annurev.immunol.22.012703.104803. [DOI] [PubMed] [Google Scholar]
- 5.Karlsson M, Lindberg K, Karlen P, Ost A, Thorn M, Winqvist O, Eberhardson M. Evidence for immunosurveillance in intestinal premalignant lesions. Scand J Immunol. 2010;71:362–8. doi: 10.1111/j.1365-3083.2010.02377.x. [DOI] [PubMed] [Google Scholar]
- 6.Banner BF, Sonmez-Alpan E, Yousem SA. An immunophenotypic study of the inflammatory cell populations in colon adenomas and carcinomas. Mod Pathol. 1993;6:295–301. [PubMed] [Google Scholar]
- 7.Cui G, Yuan A, Vonen B, Florholmen J. Progressive cellular response in the lamina propria of the colorectal adenoma-carcinoma sequence. Histopathology. 2009;54:550–60. doi: 10.1111/j.1365-2559.2009.03273.x. [DOI] [PubMed] [Google Scholar]
- 8.Yuan A, Steigen SE, Goll R, Vonen B, Husbekk A, Cui G, Florholmen J. Dendritic cell infiltration pattern along the colorectal adenoma-carcinoma sequence. Apmis. 2008;116:445–56. [PubMed] [Google Scholar]
- 9.Hua W, Yuan A, Zheng W, Li C, Cui J, Pang Z, Zhang L, Li Z, Goll R, Cui G. Accumulation of FoxP3+ T regulatory cells in the tumor microenvironment of human colorectal adenomas. Pathol Res Pract. 2016;212:106–12. doi: 10.1016/j.prp.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Whiteside TL. The role of immune cells in the tumor microenvironment. Cancer Treat Res. 2006;130:103–24. doi: 10.1007/0-387-26283-0_5. [DOI] [PubMed] [Google Scholar]
- 11.Schottelius AJ, Dinter H. Cytokines, NF-kappaB, microenvironment, intestinal inflammation and cancer. Cancer Treat Res. 2006;130:67–87. doi: 10.1007/0-387-26283-0_3. [DOI] [PubMed] [Google Scholar]
- 12.Dock J, Ramirez CM, Hultin L, Hausner MA, Hultin P, Elliott J, Yang OO, Anton PA, Jamieson BD, Effros RB. Distinct aging profiles of CD8+ T cells in blood versus gastrointestinal mucosal compartments. PLoS One. 2017;12:e0182498. doi: 10.1371/journal.pone.0182498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Preza GC, Yang OO, Elliott J, Anton PA, Ochoa MT. T lymphocyte density and distribution in human colorectal mucosa, and inefficiency of current cell isolation protocols. PLoS One. 2015;10:e0122723. doi: 10.1371/journal.pone.0122723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang K, Taggart MW, Reyes-Uribe L, Borras E, Riquelme E, Barnett RM, Leoni G, San Lucas FA, Catanese MT, Mori F, Diodoro MG, You YN, Hawk ET, Roszik J, Scheet P, Kopetz S, Nicosia A, Scarselli E, Lynch PM, McAllister F, Vilar E. Immune profiling of premalignant lesions in patients with lynch syndrome. JAMA Oncol. 2018;4:1085–1092. doi: 10.1001/jamaoncol.2018.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaves ALF, Silva AG, Maia FM, Lopes GFM, de Paulo LFB, Muniz LV, Dos Santos HB, Soares JMA, Souza AA, de Oliveira Barbosa LA, Loyola AM, Murta EFC, Michelin MA, de Azambuja Ribeiro RIM. Reduced CD8(+) T cells infiltration can be associated to a malignant transformation in potentially malignant oral epithelial lesions. Clin Oral Investig. 2019;23:1913–1919. doi: 10.1007/s00784-018-2622-8. [DOI] [PubMed] [Google Scholar]
- 16.Liu F, Hu X, Zimmerman M, Waller JL, Wu P, Hayes-Jordan A, Lev D, Liu K. TNFalpha cooperates with IFN-gamma to repress Bcl-xL expression to sensitize metastatic colon carcinoma cells to TRAIL-mediated apoptosis. PLoS One. 2011;6:e16241. doi: 10.1371/journal.pone.0016241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jang TJ. Progressive increase of regulatory t cells and decrease of CD8+ T cells and CD8+ T cells/regulatory T cells ratio during colorectal cancer development. Korean J Pathol. 2013;47:443–51. doi: 10.4132/KoreanJPathol.2013.47.5.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galon J, Bruni D. Approaches to treat immune hot, altered and cold tumours with combination immunotherapies. Nat Rev Drug Discov. 2019;18:197–218. doi: 10.1038/s41573-018-0007-y. [DOI] [PubMed] [Google Scholar]
- 19.Cui G. TH9, TH17, and TH22 cell subsets and their main cytokine products in the pathogenesis of colorectal cancer. Front Oncol. 2019;9:1002. doi: 10.3389/fonc.2019.01002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hahn JN, Falck VG, Jirik FR. Smad4 deficiency in T cells leads to the Th17-associated development of premalignant gastroduodenal lesions in mice. J Clin Invest. 2011;121:4030–42. doi: 10.1172/JCI45114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cui G, Yang H, Zhao J, Yuan A, Florholmen J. Elevated proinflammatory cytokine IL-17A in the adjacent tissues along the adenoma-carcinoma sequence. Pathol Oncol Res. 2015;21:139–46. doi: 10.1007/s12253-014-9799-1. [DOI] [PubMed] [Google Scholar]
- 22.Cui G, Yuan A, Goll R, Florholmen J. IL-17A in the tumor microenvironment of the human colorectal adenoma-carcinoma sequence. Scand J Gastroenterol. 2012;47:1304–12. doi: 10.3109/00365521.2012.725089. [DOI] [PubMed] [Google Scholar]
- 23.Levy EM, Roberti MP, Mordoh J. Natural killer cells in human cancer: from biological functions to clinical applications. J Biomed Biotechnol. 2011;2011:676198. doi: 10.1155/2011/676198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Cardell SL. The Yin and Yang of invariant natural killer t cells in tumor immunity-suppression of tumor immunity in the intestine. Front Immunol. 2017;8:1945. doi: 10.3389/fimmu.2017.01945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao CM, Zimmer MI, Shanmuganad S, Yu HT, Cardell SL, Wang CR. Dysregulation of CD1d-restricted type ii natural killer T cells leads to spontaneous development of colitis in mice. Gastroenterology. 2012;142:326–34. e1–2. doi: 10.1053/j.gastro.2011.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Y, Sedimbi S, Lofbom L, Singh AK, Porcelli SA, Cardell SL. Unique invariant natural killer T cells promote intestinal polyps by suppressing TH1 immunity and promoting regulatory T cells. Mucosal Immunol. 2018;11:131–143. doi: 10.1038/mi.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mantovani A, Schioppa T, Porta C, Allavena P, Sica A. Role of tumor-associated macrophages in tumor progression and invasion. Cancer Metastasis Rev. 2006;25:315–22. doi: 10.1007/s10555-006-9001-7. [DOI] [PubMed] [Google Scholar]
- 28.Lewis CE, Pollard JW. Distinct role of macrophages in different tumor microenvironments. Cancer Res. 2006;66:605–12. doi: 10.1158/0008-5472.CAN-05-4005. [DOI] [PubMed] [Google Scholar]
- 29.Chen JJ, Lin YC, Yao PL, Yuan A, Chen HY, Shun CT, Tsai MF, Chen CH, Yang PC. Tumor-associated macrophages: the double-edged sword in cancer progression. J. Clin. Oncol. 2005;23:953–64. doi: 10.1200/JCO.2005.12.172. [DOI] [PubMed] [Google Scholar]
- 30.Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer. 2004;4:71–8. doi: 10.1038/nrc1256. [DOI] [PubMed] [Google Scholar]
- 31.Soncin I, Sheng J, Chen Q, Foo S, Duan K, Lum J, Poidinger M, Zolezzi F, Karjalainen K, Ruedl C. The tumour microenvironment creates a niche for the self-renewal of tumour-promoting macrophages in colon adenoma. Nat Commun. 2018;9:582. doi: 10.1038/s41467-018-02834-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maglietta A, Maglietta R, Staiano T, Bertoni R, Ancona N, Marra G, Resta L. The immune landscapes of polypoid and nonpolypoid precancerous colorectal lesions. PLoS One. 2016;11:e0159373. doi: 10.1371/journal.pone.0159373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Funada Y, Noguchi T, Kikuchi R, Takeno S, Uchida Y, Gabbert HE. Prognostic significance of CD8+ T cell and macrophage peritumoral infiltration in colorectal cancer. Oncol Rep. 2003;10:309–13. [PubMed] [Google Scholar]
- 34.Pages F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C, Fridman WH. Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene. 2010;29:1093–102. doi: 10.1038/onc.2009.416. [DOI] [PubMed] [Google Scholar]
- 35.Nagtegaal ID, Marijnen CA, Kranenbarg EK, Mulder-Stapel A, Hermans J, van de Velde CJ, van Krieken JH. Local and distant recurrences in rectal cancer patients are predicted by the nonspecific immune response; specific immune response has only a systemic effect--a histopathological and immunohistochemical study. BMC Cancer. 2001;1:7. doi: 10.1186/1471-2407-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res. 1998;58:3491–4. [PubMed] [Google Scholar]
- 37.Legitimo A, Consolini R, Failli A, Orsini G, Spisni R. Dendritic cell defects in the colorectal cancer. Hum Vaccin Immunother. 2014;10:3224–35. doi: 10.4161/hv.29857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Michielsen AJ, O’Sullivan JN, Ryan EJ. Tumor conditioned media from colorectal cancer patients inhibits dendritic cell maturation. Oncoimmunology. 2012;1:751–753. doi: 10.4161/onci.19570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Michielsen AJ, Hogan AE, Marry J, Tosetto M, Cox F, Hyland JM, Sheahan KD, O’Donoghue DP, Mulcahy HE, Ryan EJ, O’Sullivan JN. Tumour tissue microenvironment can inhibit dendritic cell maturation in colorectal cancer. PLoS One. 2011;6:e27944. doi: 10.1371/journal.pone.0027944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Orsini G, Legitimo A, Failli A, Ferrari P, Nicolini A, Spisni R, Miccoli P, Consolini R. Defective generation and maturation of dendritic cells from monocytes in colorectal cancer patients during the course of disease. Int J Mol Sci. 2013;14:22022–41. doi: 10.3390/ijms141122022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reis e Sousa C. Dendritic cells in a mature age. Nat Rev Immunol. 2006;6:476–83. doi: 10.1038/nri1845. [DOI] [PubMed] [Google Scholar]
- 42.Bell D, Chomarat P, Broyles D, Netto G, Harb GM, Lebecque S, Valladeau J, Davoust J, Palucka KA, Banchereau J. In breast carcinoma tissue, immature dendritic cells reside within the tumor, whereas mature dendritic cells are located in peritumoral areas. J Exp Med. 1999;190:1417–26. doi: 10.1084/jem.190.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharma S, Stolina M, Yang SC, Baratelli F, Lin JF, Atianzar K, Luo J, Zhu L, Lin Y, Huang M, Dohadwala M, Batra RK, Dubinett SM. Tumor cyclooxygenase 2-dependent suppression of dendritic cell function. Clin Cancer Res. 2003;9:961–8. [PubMed] [Google Scholar]
- 44.Cui G, Goll R, Olsen T, Steigen SE, Husebekk A, Vonen B, Florholmen J. Reduced expression of microenvironmental Th1 cytokines accompanies adenomas-carcinomas sequence of colorectum. Cancer Immunol Immunother. 2007;56:985–95. doi: 10.1007/s00262-006-0259-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu Y, Cao X. Immunosuppressive cells in tumor immune escape and metastasis. J Mol Med (Berl) 2016;94:509–22. doi: 10.1007/s00109-015-1376-x. [DOI] [PubMed] [Google Scholar]
- 46.Sakaguchi S, Miyara M, Costantino CM, Hafler DA. FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol. 2010;10:490–500. doi: 10.1038/nri2785. [DOI] [PubMed] [Google Scholar]
- 47.Cui G, Yuan A, Goll R, Florholmen J. IL-17A in the tumor microenvironment of the human colorectal adenoma-carcinoma sequence. Scand J Gastroenterol. 2012;47:1304–12. doi: 10.3109/00365521.2012.725089. [DOI] [PubMed] [Google Scholar]
- 48.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–74. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marvel D, Gabrilovich DI. Myeloid-derived suppressor cells in the tumor microenvironment: expect the unexpected. J Clin Invest. 2015;125:3356–64. doi: 10.1172/JCI80005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Groth C, Hu X, Weber R, Fleming V, Altevogt P, Utikal J, Umansky V. Immunosuppression mediated by myeloid-derived suppressor cells (MDSCs) during tumour progression. Br J Cancer. 2019;120:16–25. doi: 10.1038/s41416-018-0333-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lechner MG, Liebertz DJ, Epstein AL. Characterization of cytokine-induced myeloid-derived suppressor cells from normal human peripheral blood mononuclear cells. J Immunol. 2010;185:2273–84. doi: 10.4049/jimmunol.1000901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cui G, Yuan A, Sun Z, Zheng W, Pang Z. IL-1beta/IL-6 network in the tumor microenvironment of human colorectal cancer. Pathol Res Pract. 2018;214:986–992. doi: 10.1016/j.prp.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 53.Ma PW, Beatty P, McKolanis J, Schoen R, Brand R, Finn OJ. Myeloid derived suppressor cells (MDSC) and anti-MUC1 immunosurveillance in pre-malignancy and cancer. Journal of Immunology. 2018;200:122. [Google Scholar]
- 54.Chun E, Lavoie S, Michaud M, Gallini CA, Kim J, Soucy G, Odze R, Glickman JN, Garrett WS. CCL2 promotes colorectal carcinogenesis by enhancing polymorphonuclear myeloid-derived suppressor cell population and function. Cell Rep. 2015;12:244–57. doi: 10.1016/j.celrep.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katoh H, Wang D, Daikoku T, Sun H, Dey SK, Dubois RN. CXCR2-expressing myeloid-derived suppressor cells are essential to promote colitis-associated tumorigenesis. Cancer Cell. 2013;24:631–44. doi: 10.1016/j.ccr.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jayakumar A, Bothwell ALM. Stat6 promotes intestinal tumorigenesis in a mouse model of adenomatous polyposis by expansion of MDSCs and inhibition of cytotoxic CD8 response. Neoplasia. 2017;19:595–605. doi: 10.1016/j.neo.2017.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fantini MC, Pallone F. Cytokines: from gut inflammation to colorectal cancer. Curr Drug Targets. 2008;9:375–80. doi: 10.2174/138945008784221206. [DOI] [PubMed] [Google Scholar]
- 58.Choi JW, Liu H, Shin DH, Yu GI, Hwang JS, Kim ES, Yun JW. Proteomic and cytokine plasma biomarkers for predicting progression from colorectal adenoma to carcinoma in human patients. Proteomics. 2013;13:2361–74. doi: 10.1002/pmic.201200550. [DOI] [PubMed] [Google Scholar]
- 59.Jacobson-Brown P, Neuman MG. Colorectal polyposis and immune-based therapies. Can J Gastroenterol. 2004;18:239–49. doi: 10.1155/2004/742713. [DOI] [PubMed] [Google Scholar]
- 60.Kim S, Keku TO, Martin C, Galanko J, Woosley JT, Schroeder JC, Satia JA, Halabi S, Sandler RS. Circulating levels of inflammatory cytokines and risk of colorectal adenomas. Cancer Res. 2008;68:323–8. doi: 10.1158/0008-5472.CAN-07-2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cui G, Qi H, Gundersen MD, Yang H, Christiansen I, Sorbye SW, Goll R, Florholmen J. Dynamics of the IL-33/ST2 network in the progression of human colorectal adenoma to sporadic colorectal cancer. Cancer Immunol Immunother. 2015;64:181–90. doi: 10.1007/s00262-014-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu Z, Yang L, Cui Y, Wang X, Guo C, Huang Z, Kan Q, Liu Z, Liu Y. Il-21 enhances NK cell activation and cytolytic activity and induces Th17 cell differentiation in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1133–44. doi: 10.1002/ibd.20923. [DOI] [PubMed] [Google Scholar]
- 63.Csiszar A, Szentes T, Haraszti B, Balazs A, Petranyi GG, Pocsik E. The pattern of cytokine gene expression in human colorectal carcinoma. Pathol Oncol Res. 2004;10:109–16. doi: 10.1007/BF02893465. [DOI] [PubMed] [Google Scholar]
- 64.Mager LF, Wasmer MH, Rau TT, Krebs P. Cytokine-induced modulation of colorectal cancer. Front Oncol. 2016;6:96. doi: 10.3389/fonc.2016.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cui G, Yuan A, Goll R, Vonen B, Florholmen J. Dynamic changes of interleukin-8 network along the colorectal adenoma-carcinoma sequence. Cancer Immunol Immunother. 2009;58:1897–905. doi: 10.1007/s00262-009-0702-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yuan A, Chen JJ, Yao PL, Yang PC. The role of interleukin-8 in cancer cells and microenvironment interaction. Front Biosci. 2005;10:853–65. doi: 10.2741/1579. [DOI] [PubMed] [Google Scholar]
- 67.Qi H, Yang H, Xu G, Ren J, Hua W, Shi Y, Torsvik M, Florholmen J, Cui G. Therapeutic efficacy of IL-17A antibody injection in preventing the development of colitis associated carcinogenesis in mice. Immunobiology. 2015;220:54–9. doi: 10.1016/j.imbio.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 68.Shi Y, Lin H, Cui J, Qi H, Florholmen J, Liu Z, Cui G. The role of interleukin-17A in colorectal tumorigenesis. Cancer Biother Radiopharm. 2013;28:429–32. doi: 10.1089/cbr.2012.1396. [DOI] [PubMed] [Google Scholar]
- 69.Dunn GP, Bruce AT, Sheehan KC, Shankaran V, Uppaluri R, Bui JD, Diamond MS, Koebel CM, Arthur C, White JM, Schreiber RD. A critical function for type I interferons in cancer immunoediting. Nat Immunol. 2005;6:722–9. doi: 10.1038/ni1213. [DOI] [PubMed] [Google Scholar]
- 70.Takeda K, Nakayama M, Hayakawa Y, Kojima Y, Ikeda H, Imai N, Ogasawara K, Okumura K, Thomas DM, Smyth MJ. IFN-gamma is required for cytotoxic T cell-dependent cancer genome immunoediting. Nat Commun. 2017;8:14607. doi: 10.1038/ncomms14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Contasta I, Berghella AM, Pellegrini P, Adorno D. Passage from normal mucosa to adenoma and colon cancer: alteration of normal sCD30 mechanisms regulating TH1/TH2 cell functions. Cancer Biother Radiopharm. 2003;18:549–57. doi: 10.1089/108497803322287628. [DOI] [PubMed] [Google Scholar]
- 72.Cui G, Florholmen J. Polarization of cytokine profile from Th1 into Th2 along colorectal adenoma-carcinoma sequence: implications for the biotherapeutic target? Inflamm Allergy Drug Targets. 2008;7:94–7. doi: 10.2174/187152808785107589. [DOI] [PubMed] [Google Scholar]
- 73.Pellegrini P, Berghella AM, Del Beato T, Cicia S, Adorno D, Casciani CU. Disregulation in TH1 and TH2 subsets of CD4+ T cells in peripheral blood of colorectal cancer patients and involvement in cancer establishment and progression. Cancer Immunol Immunother. 1996;42:1–8. doi: 10.1007/s002620050244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cui G, Yuan A, Pang Z, Zheng W, Li Z, Goll R. Contribution of IL-33 to the pathogenesis of colorectal cancer. Front Oncol. 2018;8:561. doi: 10.3389/fonc.2018.00561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nam JS, Terabe M, Kang MJ, Chae H, Voong N, Yang YA, Laurence A, Michalowska A, Mamura M, Lonning S, Berzofsky JA, Wakefield LM. Transforming growth factor beta subverts the immune system into directly promoting tumor growth through interleukin-17. Cancer Res. 2008;68:3915–23. doi: 10.1158/0008-5472.CAN-08-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chae WJ, Gibson TF, Zelterman D, Hao L, Henegariu O, Bothwell AL. Ablation of IL-17A abrogates progression of spontaneous intestinal tumorigenesis. Proc Natl Acad Sci U S A. 2010;107:5540–4. doi: 10.1073/pnas.0912675107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hyun YS, Han DS, Lee AR, Eun CS, Youn J, Kim HY. Role of IL-17A in the development of colitis-associated cancer. Carcinogenesis. 2012;33:931–6. doi: 10.1093/carcin/bgs106. [DOI] [PubMed] [Google Scholar]
- 78.Xie Z, Qu Y, Leng Y, Sun W, Ma S, Wei J, Hu J, Zhang X. Human colon carcinogenesis is associated with increased interleukin-17-driven inflammatory responses. Drug Des Devel Ther. 2015;9:1679–89. doi: 10.2147/DDDT.S79431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Toll AD, Fabius D, Hyslop T, Pequignot E, DiMarino AJ, Infantolino A, Palazzo JP. Prognostic significance of high-grade dysplasia in colorectal adenomas. Colorectal Dis. 2011;13:370–3. doi: 10.1111/j.1463-1318.2010.02385.x. [DOI] [PubMed] [Google Scholar]
- 80.Maywald RL, Doerner SK, Pastorelli L, De Salvo C, Benton SM, Dawson EP, Lanza DG, Berger NA, Markowitz SD, Lenz HJ, Nadeau JH, Pizarro TT, Heaney JD. IL-33 activates tumor stroma to promote intestinal polyposis. Proc Natl Acad Sci U S A. 2015;112:E2487–96. doi: 10.1073/pnas.1422445112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mertz KD, Mager LF, Wasmer MH, Thiesler T, Koelzer VH, Ruzzante G, Joller S, Murdoch JR, Brummendorf T, Genitsch V, Lugli A, Cathomas G, Moch H, Weber A, Zlobec I, Junt T, Krebs P. The IL-33/ST2 pathway contributes to intestinal tumorigenesis in humans and mice. Oncoimmunology. 2016;5:e1062966. doi: 10.1080/2162402X.2015.1062966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Spolski R, Leonard WJ. Interleukin-21: basic biology and implications for cancer and autoimmunity. Annu Rev Immunol. 2008;26:57–79. doi: 10.1146/annurev.immunol.26.021607.090316. [DOI] [PubMed] [Google Scholar]
- 83.Shapiro M, Nandi B, Gonzalez G, Prabhala RH, Mashimo H, Huang Q, Frank NY, Munshi NC, Gold JS. Deficiency of the immunostimulatory cytokine IL-21 promotes intestinal neoplasia via dysregulation of the Th1/Th17 axis. Oncoimmunology. 2017;6:e1261776. doi: 10.1080/2162402X.2016.1261776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.De Simone V, Ronchetti G, Franze E, Colantoni A, Ortenzi A, Fantini MC, Rizzo A, Sica GS, Sileri P, Rossi P, MacDonald TT, Pallone F, Monteleone G, Stolfi C. Interleukin-21 sustains inflammatory signals that contribute to sporadic colon tumorigenesis. Oncotarget. 2015;6:9908–23. doi: 10.18632/oncotarget.3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sondergaard H, Skak K. IL-21: roles in immunopathology and cancer therapy. Tissue Antigens. 2009;74:467–79. doi: 10.1111/j.1399-0039.2009.01382.x. [DOI] [PubMed] [Google Scholar]
- 86.Rao HL, Chen JW, Li M, Xiao YB, Fu J, Zeng YX, Cai MY, Xie D. Increased intratumoral neutrophil in colorectal carcinomas correlates closely with malignant phenotype and predicts patients’ adverse prognosis. PLoS One. 2012;7:e30806. doi: 10.1371/journal.pone.0030806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011;104:1288–95. doi: 10.1038/bjc.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Karaman H, Karaman A, Erden A, Poyrazoglu OK, Karakukcu C, Tasdemir A. Relationship between colonic polyp type and the neutrophil/ lymphocyte ratio as a biomarker. Asian Pac J Cancer Prev. 2013;14:3159–61. doi: 10.7314/apjcp.2013.14.5.3159. [DOI] [PubMed] [Google Scholar]
- 89.UçmakA F, Tuncel ET. Relationship between lesions in adenomatous polyp-dysplasia-colorectal cancer sequence and neutrophil-to-lymphocyte ratio. Med Sci Monit. 2016;22:4536–4541. doi: 10.12659/MSM.898879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tanoglu A, Karagoz E. Has the neutrophil/lymphocyte ratio a predictive role in distinguishing neoplastic potential of colonic polyps? Asian Pac J Cancer Prev. 2014;15:2393. doi: 10.7314/apjcp.2014.15.5.2393. [DOI] [PubMed] [Google Scholar]
- 91.Sasaki Y, Takeda H, Sato T, Orii T, Nishise S, Nagino K, Iwano D, Yaoita T, Yoshizawa K, Saito H, Tanaka Y, Kawata S. Serum Interleukin-6, insulin, and HOMA-IR in male individuals with colorectal adenoma. Clin Cancer Res. 2012;18:392–9. doi: 10.1158/1078-0432.CCR-11-0896. [DOI] [PubMed] [Google Scholar]
- 92.Bobe G, Albert PS, Sansbury LB, Lanza E, Schatzkin A, Colburn NH, Cross AJ. Interleukin-6 as a potential indicator for prevention of high-risk adenoma recurrence by dietary flavonols in the polyp prevention trial. Cancer Prev Res (Phila) 2010;3:764–75. doi: 10.1158/1940-6207.CAPR-09-0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bobe G, Murphy G, Albert PS, Sansbury LB, Lanza E, Schatzkin A, Colburn NH, Cross AJ. Serum cytokine concentrations, flavonol intake and colorectal adenoma recurrence in the Polyp Prevention Trial. Br J Cancer. 2010;103:1453–61. doi: 10.1038/sj.bjc.6605915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Godos J, Biondi A, Galvano F, Basile F, Sciacca S, Giovannucci EL, Grosso G. Markers of systemic inflammation and colorectal adenoma risk: meta-analysis of observational studies. World J Gastroenterol. 2017;23:1909–1919. doi: 10.3748/wjg.v23.i10.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Henry CJ, Sedjo RL, Rozhok A, Salstrom J, Ahnen D, Levin TR, D’Agostino R Jr, Haffner S, DeGregori J, Byers T. Lack of significant association between serum inflammatory cytokine profiles and the presence of colorectal adenoma. BMC Cancer. 2015;15:123. doi: 10.1186/s12885-015-1115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang X, Liu S, Zhou Y. Circulating levels of C-reactive protein, interleukin-6 and tumor necrosis factor-alpha and risk of colorectal adenomas: a meta-analysis. Oncotarget. 2016;7:64371–64379. doi: 10.18632/oncotarget.11853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang Y, Sedimbi SK, Lofbom L, Besra GS, Porcelli SA, Cardell SL. Promotion or suppression of murine intestinal polyp development by iNKT cell directed immunotherapy. Front Immunol. 2019;10:352. doi: 10.3389/fimmu.2019.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Waldner MJ, Foersch S, Neurath MF. Interleukin-6--a key regulator of colorectal cancer development. Int J Biol Sci. 2012;8:1248–53. doi: 10.7150/ijbs.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baltgalvis KA, Berger FG, Pena MM, Davis JM, Muga SJ, Carson JA. Interleukin-6 and cachexia in ApcMin/+ mice. Am J Physiol Regul Integr Comp Physiol. 2008;294:R393–401. doi: 10.1152/ajpregu.00716.2007. [DOI] [PubMed] [Google Scholar]
- 100.Yaoita T, Sasaki Y, Yokozawa J, Sato T, Kanno N, Sakuta K, Yagi M, Yoshizawa K, Iwano D, Nagino K, Nomura E, Abe Y, Nishise S, Takeda H, Kawata S, Ueno Y. Treatment with anti-interleukin-6 receptor antibody ameliorates intestinal polyposis in Apc(Min/+) mice under high-fat diet conditions. Tohoku J Exp Med. 2015;235:127–34. doi: 10.1620/tjem.235.127. [DOI] [PubMed] [Google Scholar]


