Abstract
A 69-year-old man was admitted to Hanawa Kousei Hospital with acute hepatitis attributed to alcohol consumption. His condition improved with conservative treatment. Computed tomography (CT) showed localized thickening of the colonic wall at the splenic flexure;carcinoembryonic antigen level was slightly elevated to 9.7 ng/mL. Colonoscopy (CS) showed an ulcerative lesion in the colonic splenic flexure. Ischemic colitis (IC) and type 4 colon cancer were suspected, but biopsy was not confirmatory. Malignancy could not be ruled out by contrast-enhanced CT;repeat CS showed circumferential stenosis of the colonic splenic flexure. Ischemic colitis was suspected based on changes between the first and second CS. Biopsy histopathology led us to diagnose stricture-type IC. Constipation, but not intestinal obstruction, occurred. Conservative treatment improved the stenosis. Excessive alcohol consumption may lead to IC;imaging studies may be useful to distinguish IC from colon cancer. Since most cases of ischemic colitis can be improved with conservative treatment, patients with stricture-type ischemic colitis may also be treated without surgery early on, with follow-up that includes careful, periodic imaging.
Keywords: ischemic colitis, stricture, acute alcoholic hepatitis, carcinoembryonic antigen
Introduction
Ischemic colitis (IC) is a disease with major symptoms of abdominal pain, lower gastrointestinal bleeding, and diarrhea;it is associated with various causes 1, 2), and is classified into transient, stricture, and gangrenous types 3). In cases in which the possibility of cancer cannot be ruled out, stricture-type IC with intestinal obstruction and gangrenous-type IC generally require surgery, but 80-85% of all IC cases are expected to be improved by conservative treatment 4). On the other hand, endoscopic and computed tomography (CT) findings of IC can be similar to those of malignant tumors 5, 6). These must be distinguished from each other, so careful follow-up is necessary.
Here, we report a case of stricture-type IC. Endoscopic and contrast-enhanced CT findings were used to differentiate IC from malignancy. The current case is interesting in that the stenosis improved with conservative treatment although symptomatic constipation continued through treatment and IC progressed to the stricture type during conservative management.
Case Report
A 69-year-old man presented with general malaise, anorexia, and a history of daily alcohol consumption;he was admitted to Hanawa Kousei Hospital. There was no pertinent history pertaining to medical treatment, family, medication, blood transfusion, or allergy. He had been drinking approximately 900 mL of sake daily for the past 49 years, and had a 29 pack-year smoking history. He had bowel movements once or twice daily with no history of habitual laxative use or enemas. On physical examination, he was lucid, had a heart rate of 84/min, blood pressure of 138/66 mm Hg, and a temperature of 36.9°C;there was jaundice and hepatomegaly. Laboratory findings included white blood cells 9,100/μL, red blood cells 366×10 4/μL, hemoglobin 12.9 g/dL, platelets 15.1×10 4/μL, total protein 5.4 g/dL, albumin 2.3 g/dL, total bilirubin 5.85 mg/dL, direct bilirubin 4.02 mg/dL, aspartate aminotransferase 185 U/L, alanine aminotransferase 182 U/L, lactate dehydrogenase 526 U/L, alkaline phosphatase 1,312 U/L, gamma glutamyl transpeptidase 1.782 U/L, amylase 42 U/L, blood urea nitrogen 29.4 mg/dL, serum creatinine 1.54 mg/dL, C-reactive protein 6.31 mg/dL, carcinoembryonic antigen (CEA) 9.7 ng/mL, carbohydrate antigen 19-9 (CA19-9) 54 U/mL, and soluble interleukin-2 receptor 510 U/mL. Hepatitis virus markers and autoantibodies were negative. Urine was positive for ketone bodies. A non-contrast CT confirmed hepatomegaly, with no evidence of bile duct obstruction or malignant tumor (Fig. 1a and b). In addition, CT showed localized colonic wall-thickening at the splenic flexure (Fig. 1b). We diagnosed the patient as having acute alcoholic hepatitis in light of his drinking history. He had avoided medical checkups previously; on the other hand, he had no other conditions, such as hypertension, diabetes mellitus, hyperlipidemia, or hyperuricemia, after admission. His clinical symptoms, jaundice, and liver dysfunction rapidly improved with fluid replacement and rest. Non-contrast CT on admission showed colonic wall-thickening at the splenic flexure, and a blood test showed a slight increase in CEA. Since the patient had not previously undergone CS, it was performed to rule out colon cancer on the seventh hospital day. The colonic splenic flexure showed redness over two-thirds of its circumference and an ulcerative, slightly constricted lesion approximately 5 cm in length (Fig. 2). Differential diagnosis included IC, colon cancer, malignant lymphoma, infectious enteritis, and inflammatory bowel disease, but the histopathological findings on biopsy showed only nonspecific inflammatory changes. On the 12th hospital day, contrast-enhanced CT of the abdomen revealed a thickened colonic splenic flexure wall. There was no enhancement of the intestinal wall (Fig. 3 a and b). Although calcification of the aorta was observed, there was no evidence of calcification or occlusion in the superior mesenteric artery, inferior mesenteric artery, superior mesenteric vein, inferior mesenteric vein, branches, or portal vein. The patient had constipation after initiation of conservative treatment, and malignancy could not be ruled out from the findings of contrast-enhanced CT. On day 30 after starting treatment, a second CS revealed complete circumferential stenosis of the colonic splenic flexure with difficulty in passing the scope through the proximal side (Fig. 4). With gastrografin contrast radiography through CS, full-circumference stenosis to approximately 3 cm was recognized (Fig. 5). Stricture-type IC was suspected based on the first endoscopy and rapid course of circumferential stenosis. Histopathological findings on biopsy showed erosion of the mucosa, edema of the stroma, and infiltration of inflammatory cells, confirming the diagnosis of IC (Fig. 6 a and b). Surgery was also considered, but the patient had only mild symptoms of constipation, which were judged not to be indicative of complete intestinal obstruction. Therefore, conservative treatment with oral laxatives and intestinal motion regulators was performed. CEA decreased to 6.0 ng/mL on the 56th hospital day. CS showed scarring and healing of the lesion on the 105th hospital day (Fig. 7), and histopathological findings on biopsy showed no evidence of malignancy.
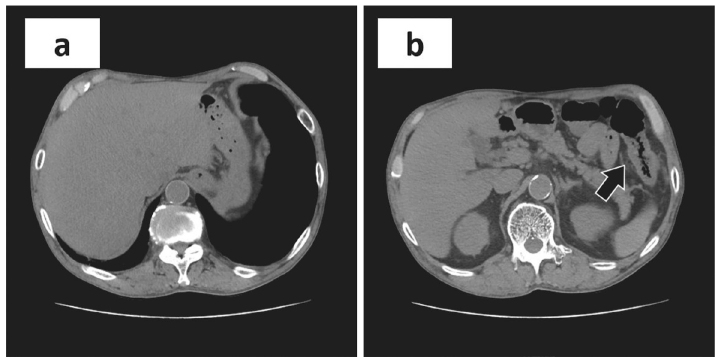
Fig. 1.
Abdominal (non-contrast) computed tomography on admission.
(a) Hepatomegaly. (a, b) No evidence of bile duct obstruction or malignancy. (b) Localized thickening of the colonic splenic flexure wall (arrow).
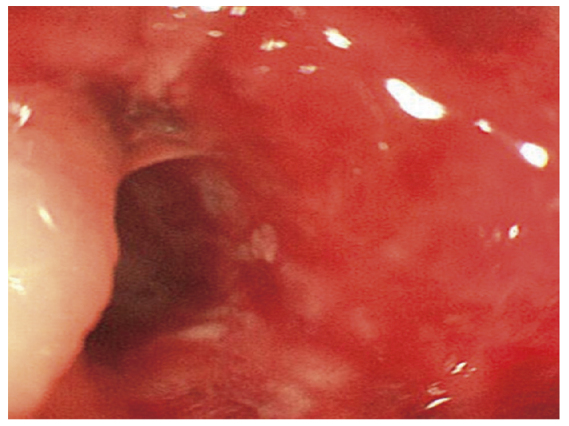
Fig. 2.
Initial endoscopy.
On the 8th hospital day, colonoscopy showed a two-thirds circumference of redness and an ulcerative, slightly constricted, longitudinal lesion of approximately 5 cm at the colonic splenic flexure.
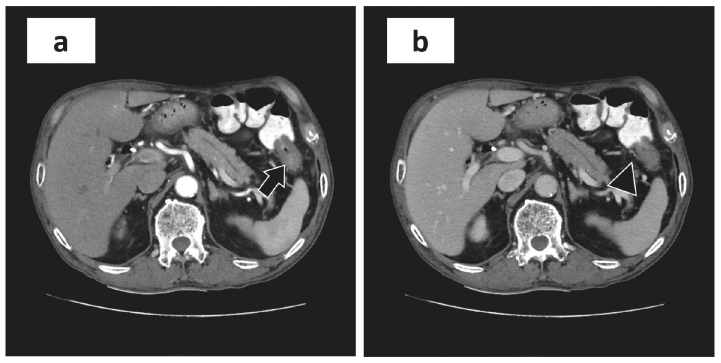
Fig. 3.
Abdominal contrast-enhanced computed tomography.
(a: arterial phase, b: equilibrium phase) On the 12th hospital day, CT showed a thickened colonic splenic flexure wall (arrow, arrowhead). There was no enhancement of the intestinal wall. Although calcification of the aorta was observed, there was no evidence of calcification or occlusion in the superior mesenteric artery, inferior mesenteric artery, superior mesenteric vein, inferior mesenteric vein, branches, or portal vein.
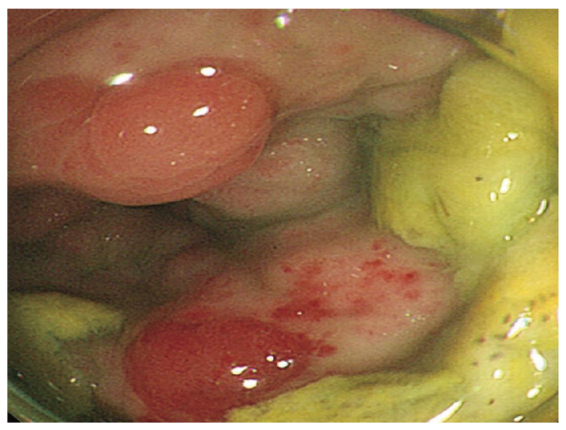
Fig. 4.
Second endoscopy.
On the 30th hospital day, the second CS showed circumferential stenosis of the colonic splenic flexure with difficulty passing the scope through the proximal side.
Fig. 5.
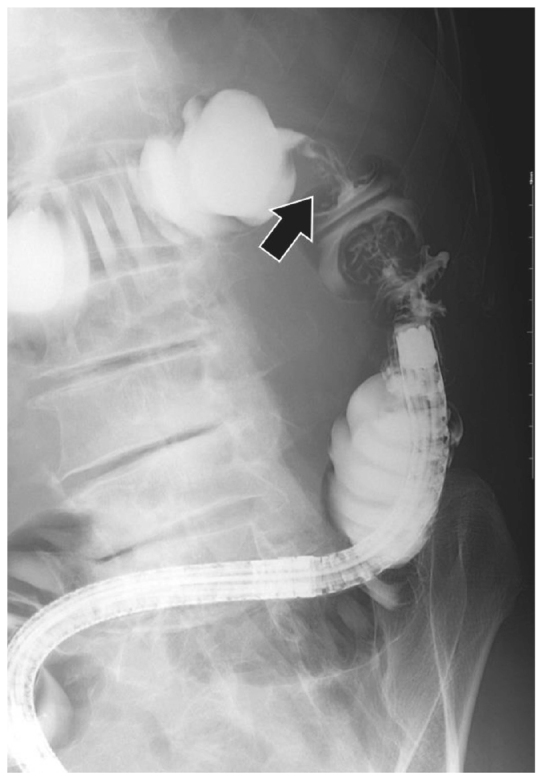
Gastrografin contrast radiography through CS.
Full-circumference stenosis of approximately 3 cm is evident.
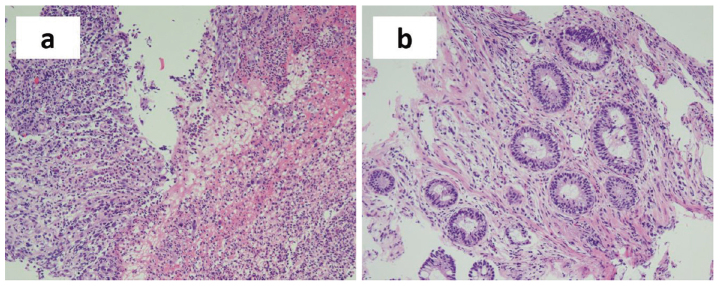
Fig. 6.
Histopathological findings of the specimen obtained by endoscopic biopsy.
Hematoxylin and eosin staining of pathological specimens showed (a) erosion of the mucosa, (b) edema of the stroma, and infiltration of inflammatory cells. (magnification, 10×)
Fig. 7.
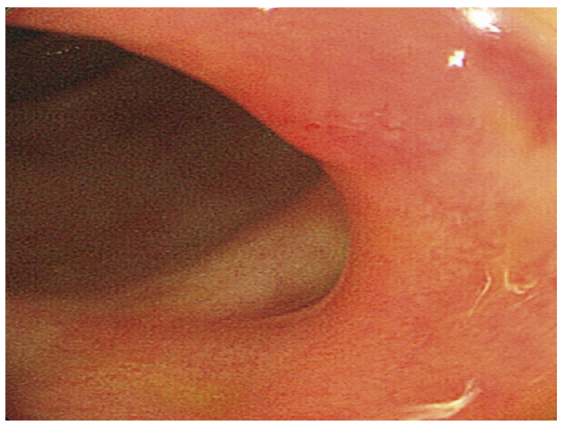
Third endoscopy.
On the 105th hospital day, CS showed scarring and healing of the lesion.
Discussion
In the current case, we identified two important clinical issues. First, excessive alcohol consumption may have led to IC. Second, imaging may not distinguish IC from malignancy, but even stricture-type IC can be improved with conservative treatment.
First, excessive alcohol consumption may have led to IC. Drugs, constipation, irritable bowel syndrome, abdominal surgery, atherosclerosis induced by hypertension, coronary artery disease, peripheral vascular disease, cerebrovascular disease, congestive heart failure, smoking, and diabetes have been implicated in the development of IC 7-11). In the present case, the patient was a smoker, and CT showed arterial calcification, thought to be arteriosclerosis, which contributes to the development of IC. We know of no prior reports of IC during the course of acute alcoholic hepatitis, but there have been reports of IC after temporary alcohol abuse 12) and an increased risk of mesenteric ischemia in alcoholics 13). Causes include blood coagulation disorders such as suppression of fibrinolysis due to increased production of plasminogen activator inhibitor-1 by alcohol consumption 14) and mesenteric vasoconstriction by suppressing endothelium-dependent vasorelaxation 15). Taken together with the findings of the current case, this suggests that our patient had a similar condition. It has also been reported that severe dehydration, caused by strenuous exercise in triathlon runners as well as extreme dietary habits and decreased blood flow to the colon, is associated with the development of IC 16, 17). In the current case, dehydration was exacerbated by repeated heavy alcohol consumption;moreover, positive urine ketone bodies and renal dysfunction were observed, suggesting severe dehydration as a cause of IC in this case.
Second, imaging studies of IC may require differentiation from malignant tumors, but even stricture-type IC can be improved with conservative treatment. It has been reported that endoscopic and CT findings of IC may resemble those of malignant tumors 5, 6). In the present case, it was difficult to differentiate type 4 (invasive) colon cancer from the ulcerative, slightly constricted lesions of CI observed at the first endoscopy, along with thickening of the colonic intestinal wall on contrast-enhanced CT, and mild elevation of CEA. However, stricture-type IC was suspected based on the findings of a longitudinal ulcer and the rapid course of stenosis on repeated CS examination, and a definitive diagnosis of IC could be made by histopathology. Serum CEA is known to be elevated by smoking, liver cirrhosis, and inflammatory bowel disease, as well as by malignant tumors 18). It has also been reported that active inflammation of the colonic mucosa stimulates the elevation of CEA 19), and there has been a report on an association between IC and elevated CEA levels 20). In our case, a slight increase in CEA was suspected to be due to smoking, but decrease in CEA was observed after conservative treatment that improved the IC, suggesting that inflammation of the colon due to IC may have been related to elevated CEA. The classic clinical manifestation of IC is sudden lower gastrointestinal bleeding with abdominal pain and a desire to defecate. However, these clinical symptoms have only been recognized in 44% of all reported cases 21). In stricture-type IC, symptoms of intestinal obstruction, such as constipation and abdominal distension, are observed 22). In the current case, the patient was asymptomatic before the first endoscopy and showed constipation symptoms associated with stenosis. With regard to treatment, it has been reported that surgery is frequently required for IC in the right colon 23). However, IC in the left colon may be improved by conservative treatment in patients with transient or stricture type IC without intestinal obstruction. The present case developed stricture-type ischemic colitis in the left colon without complete intestinal obstruction. Conservative treatment with oral laxatives and intestinal motion regulators alone improved stenosis.
In conclusion, excessive alcohol consumption may have led to IC;differential diagnosis was required because the imaging of IC resembled that of malignancy. In particular, if colon cancer cannot be ruled out in stricture-type IC, it may easily lead to surgery. However, if the stricture does not result in bowel obstruction, conservative treatment may be sufficient. Thus, we should be familiar with the causes and pathophysiology of IC and follow-up conservatively treated patients with careful imaging evaluations when a diagnosis of IC is suspected.
Conflict of Interest
The authors declare no conflicts of interest related to this article.
References
- 1.Mosli M, Parfitt J, Gregor J. Retrospective analysis of disease association and outcome in histologically confirmed ischemic colitis. J Dig Dis, 14: 238-243, 2013. [DOI] [PubMed] [Google Scholar]
- 2.Longstreth GF, Yao JF. Epidemiology, clinical features, high-risk factors, and outcome of acute large bowel ischemia. Clin Gastroenterol Hepatol, 7: 1075-1080, 2009. [DOI] [PubMed] [Google Scholar]
- 3.Marston A. Ischaemic colitis-clinical aspects. Bibl Gastroenterol, 9: 137-142, 1970. [PubMed] [Google Scholar]
- 4.Elder K, Lashner BA, Al Solaiman F. Clinical approach to colonic ischemia. Cleve Clin J Med, 76: 401-409, 2009. [DOI] [PubMed] [Google Scholar]
- 5.Khor TS, Lauwers GY, Odze RD, Srivastava A. “Massforming” variant of ischemic colitis is a distinct entity with predilection for the proximal colon. Am J Surg Pathol, 39: 1275-1281, 2015. [DOI] [PubMed] [Google Scholar]
- 6.Deepak P, Devi R. Ischemic colitis masquerading as colonic tumor: case report with review of literature. World J Gastroenterol, 17: 5324-5326, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yadav S, Dave M, Edakkanambeth Varayil J, et al. A population-based study of incidence, risk factors, clinical spectrum, and outcomes of ischemic colitis. Clin Gastroenterol Hepatol, 13: 731-738, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walker AM, Bohn RL, Cali C, Cook SF, Ajene AN, Sands BE. Risk factors for colon ischemia. Am J Gastroenterol, 99: 1333-1337, 2004. [DOI] [PubMed] [Google Scholar]
- 9.Huerta C, Rivero E, Montoro MA, García-Rodriguez LA. Risk factors for intestinal ischaemia among patients registered in a UK primary care database: a nested case-control study. Aliment Pharmacol Ther, 33: 969-978, 2011. [DOI] [PubMed] [Google Scholar]
- 10.Chang L, Kahler KH, Sarawate C, Quimbo R, Kralstein J. Assessment of potential risk factors associated with ischaemic colitis. Neurogastroenterol Motil, 20: 36-42, 2008. [DOI] [PubMed] [Google Scholar]
- 11.Habu Y, Tahashi Y, Kiyota K, et al. Reevaluation of clinical features of ischemic colitis. Analysis of 68 consecutive cases diagnosed by early colonoscopy. Scand J Gastroenterol, 31: 881-886, 1996. [DOI] [PubMed] [Google Scholar]
- 12.Lee JH, Noh GT, Lee RA. Extensive bowel ischemia with heavy alcohol consumption: report of a case. J Korean Soc Coloproctol, 28: 61-65, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen CF, Kao WT, Liu KT, Chen SL, Huang YT, Huang CC. Alcohol use disorders associated with an increased risk of mesenteric ischemia: A nationwide cohort study. Drug Alcohol Depend, 194: 264-270, 2019. [DOI] [PubMed] [Google Scholar]
- 14.Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World, 21: 42-52, 1997. [PMC free article] [PubMed] [Google Scholar]
- 15.Horie Y, Ishii H. Effect of alcohol on organ microcirculation: its relation to hepatic, pancreatic and gastrointestinal diseases due to alcohol. Nihon Arukoru Yakubutsu Igakkai Zasshi, 36: 471-485, 2001. (in Japanese, Abstract in English) [PubMed] [Google Scholar]
- 16.Murray B, Stofan J, Sallis B. Return to competition following ischemic colitis caused by severe dehydration. J Sport Rehabil, 16: 271-276, 2007. [DOI] [PubMed] [Google Scholar]
- 17.Shibata M, Nakamuta H, Abe S, et al. Ischemic colitis caused by strict dieting in an 18-year-old female: report of a case. Dis Colon Rectum, 45: 425-428, 2002. [DOI] [PubMed] [Google Scholar]
- 18.Shapiro M, Scapa E. Elevated carcinoembryonic antigen (CEA) levels in a patient with no malignancy. Hepatogastroenterology, 47: 163-164, 2000. [PubMed] [Google Scholar]
- 19.Smithson JE, Warren BF, Young S, Pigott R, Jewell DP. Heterogeneous expression of carcinoembryonic antigen in the normal colon and upregulation in active ulcerative colitis. J Pathol, 180: 146-151, 1996. [DOI] [PubMed] [Google Scholar]
- 20.Furukita Y, Ohnishi K, Tanida N, Fujishima N, Hamaguchi N, Kaihotsu N. A case of ischemic colitis associated with abnormally elevated serum level of CEA. J Jpn Surg Assoc, 71: 449-453, 2010. (in Japanese, abstract in English) [Google Scholar]
- 21.Montoro MA, Brandt LJ, Santolaria S, et al. Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol, 46: 236-246, 2011. [DOI] [PubMed] [Google Scholar]
- 22.Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg, 25: 228-235, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sotiriadis J, Brandt LJ, Behin DS, Southern WN. Ischemic colitis has a worse prognosis when isolated to the right side of the colon. Am J Gastroenterol, 102: 2247-2252, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]