Abstract
Objectives
The aim is to review current literature related to the diagnosis, management, and follow-up of suspected and confirmed Covid-19 cases.
Key findings
Medical Imaging plays an important auxiliary role in the diagnosis of Covid-19 patients, mainly those most seriously affected. Practice differs widely among different countries, mainly due to the variability of access to resources (viral testing and imaging equipment, specialised staff, protective equipment). It has been now well-documented that chest radiographs should be the first-line imaging tool and chest CT should only be reserved for critically ill patients, or when chest radiograph and clinical presentation may be inconclusive.
Conclusion
As radiographers work on the frontline, they should be aware of the potential risks associated with Covid-19 and engage in optimal strategies to reduce these. Their role in vetting, conducting and often reporting the imaging examinations is vital, as well as their contribution in patient safety and care. Medical Imaging should be limited to critically ill patients, and where it may have an impact on the patient management plan.
Implications for practice
At the time of publication, this review offers the most up-to-date recommendations for clinical practitioners in radiology departments, including radiographers. Radiography practice has to significantly adjust to these new requirements to support optimal and safe imaging practices for the diagnosis of Covid-19. The adoption of low dose CT, rigorous infection control protocols and optimal use of personal protective equipment may reduce the potential risks of radiation exposure and infection, respectively, within Radiology departments.
Keywords: COVID-19, Imaging, Radiography, CT, Chest, Guidelines
Introduction
Since the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic a few months ago, more than 6,573,568 laboratory-confirmed cases of the new virus have been reported, with over 388,041 confirmed deaths, as per June 4th, 2020.1 The coronavirus disease 2019 (Covid-19) resulting after infection from SARS-CoV-2 has already affected 210 countries and territories globally.2 This virus was first recorded in China's Hubei province, where the cause of the disease was initially unknown. Hence, it was first classified as unknown pneumonia.3
New information about Covid-19 emerges every day as more diagnostic tests are being carried out. Medical Imaging has a unique place in this new evidence-base and radiographers are working on the frontline to deliver care for some of the most seriously affected patients, often facing challenging situations with staff and resource shortages.
The aim is to review current literature related to the diagnosis, management, and follow-up of suspected and confirmed Covid-19 cases. Objectives include to: i) outline pathophysiology and basic epidemiology useful for radiographers, ii) discuss the role of medical imaging in the diagnosis of Covid-19, iii) summarise national and international guidelines of imaging Covid-19, iv) present main clinical and imaging findings and v) summarise current safety recommendations for medical imaging practice.
The search methods and keywords for this review are appended on Table 1 below for clarity. It has to be noted that in this review all available information at the time of publication was included, however we appreciate this is a fast developing area of study.
Table 1.
Literature inclusion criteria and search methods summarised.
| Keywords | COVID-19, AND Radiography OR Medical Imaging, AND Epidemiology, AND Chest-x-ray, OR CXR, OR Chest radiograph, AND Computed Tomography, OR CT, AND Magnetic Resonance Imaging, OR MRI, AND Ultrasound, AND Radiology, AND testing, AND symptoms, AND guidelines. |
| Academic Databases and key public health and professional body websites | Pubmed, Google scholar, European Centre for Disease Prevention and Control, World Health Organization, British Society of Thoracic Imaging, Society and College of Radiographers, Royal College of Radiologists, European Society of Radiology, European Society of Thoracic Imaging, American College of Radiology, Canadian Association of Radiologists, International Society of Radiographers & Radiologic Technologists, European Federation of Radiographer Societies. |
| Date range | January 1, 2020–May 19, 2020. |
| Inclusion criteria | Studies written in English language, published in peer-reviewed journals. Grey literature was also included if issued by professional bodies and key stakeholders of public health. Articles in press were also included. |
Pathophysiology
Coronaviruses belong to a large family of single-stranded RNA viruses. Although they are thought to cause mainly mild symptoms, the Middle East respiratory syndrome (MERS-CoV) and the severe acute respiratory syndrome (SARS-CoV) recently, caused many fatalities.4 In 2002, the SARS-CoV originating in China had a 11% mortality rate, while in 2012 the MERS-CoV in Saudi Arabia had a mortality rate of 34%. Both viruses originated from wild animals.4
SARS-CoV-2 targets the respiratory system. After the infection there is a variable incubation period ranging between 1 and 14 days. In some studies, average incubation periods of 3 days have been reported.5
Covid-19 incidence and epidemiological data
It has been found that the majority of Covid-19 patients are asymptomatic or with mild symptoms. However, for a significant minority of cases, Covid-19 can present as, or progress to, severe respiratory distress.6 The typical clinical symptoms associated with the Covid-19 disease include cough, fever, fatigue and dyspnea.7 However, many patients can initially develop nausea and diarrhea, as well as generalised muscular pain and lack of sense of smell or taste.8, 9, 10 Haemoptysis has also been reported on a less frequent basis.7 Less common non-respiratory symptoms have also been described such as headache, urticaria, or presentation of neurological clinical features prior to or following the onset of Covid-19-related symptoms.7 , 11 , 12
At the time of writing, the United States of America have reported the highest number of confirmed Covid-19 cases, as well as the highest number of deaths, followed by Spain, Italy, France and the UK. Mortality rate is measured using the case fatality rate (CFR), a measure describing the proportion of deaths within a defined population, and this rate varies considerably among different countries and is challenging to accurately calculate, as the number of asymptomatic or mild cases may be under-reported.13 According to the World Health Organization around 5% of confirmed cases are severe and require intensive care.14 Acute respiratory distress syndrome, organ failure, septic shock and severe pneumonia are the main causes of mortality.
Covid-19 patients with one or more comorbidities, including hypertension, diabetes, cardiovascular diseases, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), malignancies, chronic kidney disease and smoking, are associated with poorer clinical outcomes and higher mortality rates.15, 16, 17, 18 Severe asthma is also listed as a risk factor for hospitalisation.19 , 20
In addition, mortality rates have been found to dramatically increase with age. A recent UK study estimates an overall Covid-19 mortality rate of 0.66%, increasing to 7.8% for people over 80.21 A study from Italy reports that 83% of the deaths were people over 70 years old.22 Similarly, there is a sharp decline of death rate in children.21 Recent data shows that children with Covid-19 might be largely asymptomatic (90%) or demonstrate milder clinical manifestations and lower CFR compared to adults, while only younger than 1-year of age are more susceptible to severe disease.23, 24, 25 There are also disproportionately more deaths in men than women, with similar cases between the two genders. This was attributed to sex-based immunological differences, or sex-based behavioral differences such as prevalence of smoking.26 , 27
Diagnostic investigations for Covid-19
Swabs
Accurate detection of an active Covid-19 infection is vital for case identification, disease containment and optimal management of patients. Molecular techniques are the first-line method of diagnosing Covid-19. Most commonly they use respiratory samples, such as nasopharyngeal swabs28 with reverse-transcription polymerase chain reaction (RT-PCR), real-time RT-PCR (rRT-PCR) and reverse transcription loop-mediated isothermal amplification (RT-LAMP) being the most common methods employed.29 Viral tests are used to detect the presence of an antigen, e.g. the virus's RNA, in a patient, rather than antibodies, which affirm an immune response. However, antigen tests have limitations, including the time to obtain results, the relatively high false negative and false positive rates and the intermittent shortage of test kits during the outbreak.29, 30, 31 There is ongoing debate about the optimal testing for coronavirus, with antibody testing gaining momentum, but equally more time is required until these tests become widely available.32
Blood tests
Laboratory tests are widely available and cost effective, and are used in the diagnosis and management of Covid-19 patients, including differentiated white cell count, C reactive protein (CRP), D-dimer and erythrocyte sedimentation rate (ESR).33 Lymphopenia and mildly elevated CRP have been widely reported, with the degree of lymphopenia proposed as a risk factor for more severe disease.34
Imaging
Medical imaging plays an important role in supporting clinical decision making in the diagnosis, management and treatment of Covid-19 patients. Medical imaging may be useful for differential diagnosis between Covid-19 and other viral respiratory illnesses with similar symptoms.35, 36, 37 Chest radiographs, chest CT, lung ultrasound, as well as MRI are included in the arsenal of medical imaging, each one with advantages and limitations.
Chest radiographs (CXR)
Chest radiographs (CXR) are the most widely used imaging modality for suspected and confirmed Covid-19 cases.38 Mobile radiographs are being used with increasing frequency to avoid possible transmission during patient transfer to imaging departments, as well as the traditional role in imaging critically unwell patients.39
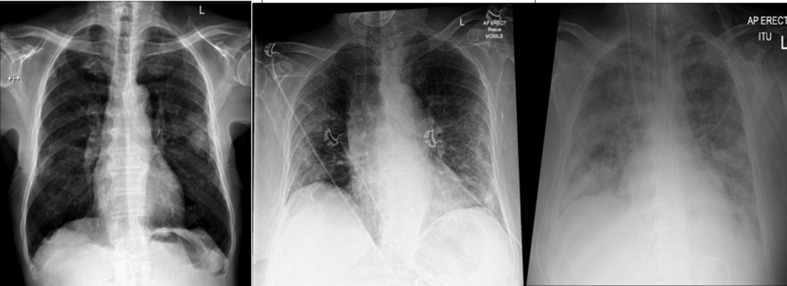
Classical CXR patterns of Covid-19 include ground-glass opacities, consolidation and bilateral interstitial opacification associated with atypical or organizing pneumonia.39, 40, 41, 42 Pneumothorax or lung cavitation are uncommon complications.38 , 43 Imaging appearances may vary with stage of the disease (days from first symptoms) and with disease severity (Fig. 1 ).44 CXRs may be normal in cases of confirmed Covid-19, both in early infection and in mild disease. In severe Covid-19 there is a proportionately greater lung involvement which tends to be denser peripherally and in the lower zones.38
Figure 1.
From left to right: Mild, moderate, and severe imaging manifestations of the disease on chest radiographs.
The role of CXRs as the initial radiological assessment of patients presenting with respiratory distress and possible Covid-19 is established. However, the available data on the accuracy of CXR in Covid-19 is limited, with smaller case numbers compared to chest CT research and often without the inclusion of normal or non-Covid-19 cases. For example, all patients within the analysis of Zhao et al.45 had a CXR performed but the findings have not been included.
Sensitivity of chest radiographs is dependent on the extent of Covid-19 infection. In a cohort study (n = 64 patients), CXR imaging of mild to moderate Covid-19 patients was found to have a sensitivity of 69%40 and Lomoro et al.42 found CXR sensitivity of 84% (27 of 32). Of the 170 non-hospitalised patients with mild symptoms, Bandirali et al.46 found 100 (58.8%) abnormal CXRs suggestive of Covid-19, however RT-PCR confirmation was not performed. A small case series with RT-PCR confirmed Covid-19 (n = 9 patients) reported 50% sensitivity (true positive n = 3) and specificity 33% (true negative n = 1) for CXR, with two false positive CXRs (breast tissue mimicking ground glass opacification and atelectasis) without CT correlation.47 Paucity of reported specificity, small sample sizes, lack of normal and non Covid-19 cases emphasises the requirement for imaging to be used as part of clinical decision making rather than in isolation. These findings can be summarised in Table 2 .
Table 2.
A summary of sensitivity and specificity studies for CXR in Covid-19 cases.
Chest Computed Tomography (chest CT)
Chest Computed Tomography (chest CT) has a limited but important role in clinical management of Covid-19 patients. CT should be reserved for seriously ill patients, with emerging awareness of high prevalence of pulmonary thrombosis.48 In addition, it can be used in the case of inconclusive chest radiographs49 or unavailability of PCR tests. In the case of follow-up imaging where CT is required for clinical decision making, low-dose chest CT may be considered, as it can offer up to an 8-fold dose reduction.50
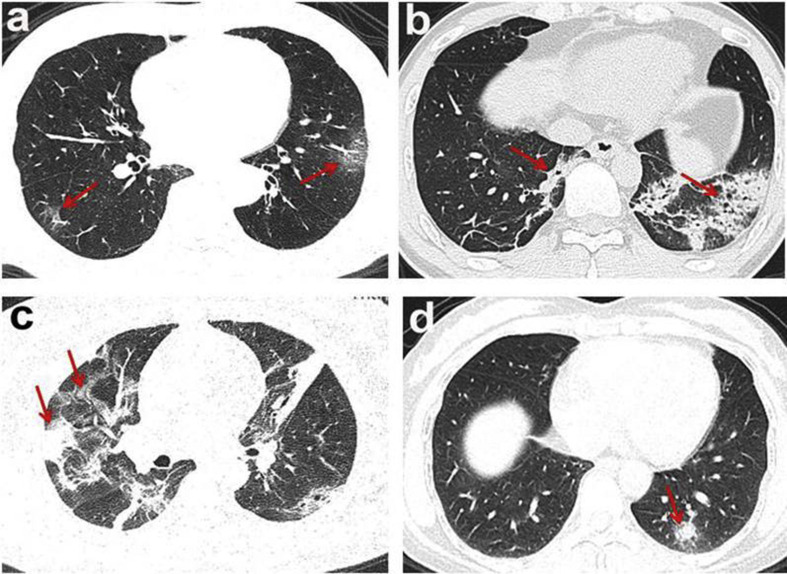
Systematic reviews and meta-analyses found that the most common imaging manifestations of the disease at CT were: bilateral, basal, ground glass opacities (GGOs), crazy-paving, peripheral consolidations, reverse halo (“atoll” sign) and peri-lobular patterns (Fig. 2 ).51 , 52 Bilateral pneumonia was predominant compared to unilateral, while most patients had more than two lobes involved, more often affecting the bases of the lungs than the apices. Pericardial effusion, pleural thickening or hydrothorax were uncommon CT findings.52, 53, 54 Though viral pneumonias generally show similar imaging features, there are some characteristic CT findings which may help differentiating COVID-19 from influenza-related pneumonia.55
Figure 2.
CT manifestations of Covid-19 disease. a. Ground-glass opacities, b. Consolidations, c. Consolidations with ground-glass opacities, d. Solid nodule.52
Asymptomatic patients demonstrate single or multiple ground-glass opacities, air bronchogram and nodules encircled by ground-glass opacities. These are the main patterns also for early symptomatic patients, with the extra possible finding of interlobular septal thickening.36 , 44 When imaging patients between 3 and 7 days after the onset of clinical symptoms, CT demonstrated fused consolidations with air bronchogram, which tended to slightly decrease in range and density when imaging was performed between 7 and 14 days after the full clinical manifestation of the disease has taken place.56 Finally, imaging in the dissipation period (2–3 weeks after the onset of symptoms) revealed further decrease in lesions and thickening of bronchial wall and interlobular septum. However, even though the majority of patients developed improvement after 14 days, some studies have shown increased consolidations and development of pleural effusion on follow-up CTs during the latter stages of the disease.44 Finally, a significant proportion of critically unwell patients with Covid-19 have pulmonary embolic disease ranging from 23 to 30% and the role of CT pulmonary angiography (CTPA) is being established.57 , 58
Despite paediatric patients having less severe symptoms than elderly cases, the CT findings in each age range are similar, most frequently bilateral sub-pleural ground-glass opacities and consolidation.59 Although, when compared to adults, the GGOs in children are more localised and of lower attenuation.60 Therefore, these findings were characterised as atypical. Furthermore, there is higher prevalence of peri-bronchial infiltrates and bronchial wall thickening in children compared to adults. This could be related to differences in distribution of the coronavirus infection along the respiratory epithelium between the two groups or to occurrence of co-infection.61
Similarly, chest CT performed in pregnant women diagnosed with Covid-19 disease, showed that the consolidation lesions were more prevalent than in the rest of the patients.62 Low-dose protocols were implemented for these patients, minimising the risks of radiation exposure.62 Imaging of pregnant women should always be performed with extreme caution, after a thorough risk-benefit analysis for mother and fetus.
Relative to CXR, chest CT has higher contrast resolution without superimposed anatomy, which facilitates identification of radiographically occult abnormalities, in particular early ground glass opacification. However, many diseases manifest with similar CT findings, which may explain the relatively low specificity and risk of false positive diagnoses.63 This is not coming as a surprise as in CT the three-dimensional nature of data acquisition and presentation ensures that superimposition of anatomy and pathology is minimised and any lesions can therefore be more easily identified and characterised.
These findings suggest that CT should not be used alone as a diagnostic tool, and that swab tests must always be performed for these patients. Although some studies conducted in China suggested chest CT as a first-line tool,37 , 64 , 65 it must be noted that chest CT should only be reserved for the critically ill patients with unexplained deterioration.
In the early stages of the Covid-19 pandemic, characteristic CT appearances were seen in asymptomatic patients undergoing imaging for other reasons.66 , 67 Hence, radiographers working in any healthcare setting must be aware and familiar with Covid-19 findings in order to eliminate the potential risks of further transmission and improve patient management. Reporting radiographers in particular are expected to be familiar with Covid-19 imaging findings and preliminary clinical evaluation by radiographers is an expected competency in different countries, including the United Kingdom.39
Point-of-care lung ultrasound (LUS)
The use of lung ultrasound (LUS) in Covid-19 is contentious and the evidence base is still evolving. Point-of-care LUS may have a role in the assessment of Covid-19 particularly in an intensive care setting to facilitate the evaluation of Covid-19 patients, allowing for cost reduction, better use of available resources and greater availability, while portability and the ability of follow-up are also advantageous.68 , 69
Some early studies show that LUS has a high sensitivity (93–98%) in imaging of acute respiratory distress syndrome (ARDS), as well as in cases of viral infections, such as the influenza pandemic in 2009.70 In addition, LUS reported a 93% sensitivity and 95% specificity when imaging critically ill patients with pneumonia.71 A summary of all reported diagnostic accuracy values can be found in Table 3 .
Table 3.
Summary of sensitivity and specificity of CXR, CT and LUS for the diagnosis of Covid-19.
Although its full diagnostic value in patient management is yet to be established for Covid-19 patients in larger studies, LUS can depict signs suggestive of alveolar damage, subpleural consolidations, white lung regions, as well as irregular B-lines.68 , 70 A recent study reported a strong correlation with chest CT findings, and LUS was recommended for imaging acute respiratory failure and lung inflammation.76 More research with larger sample sizes would be needed to establish its added value, particularly for children or pregnant patients. However high operator dependency will remain its weak point.
Magnetic Resonance Imaging (MRI)
Lastly, Magnetic Resonance Imaging (MRI), although not relevant for the evaluation of lung disease, it can contribute to the diagnostic pathway of patients with symptoms from the central nervous system. These may include various neurological manifestations, such as acute stroke, skeletal muscle injuries, consciousness impairment, or acute necrotizing hemorrhagic encephalopathy.77 , 78 The role of MRI currently in the diagnosis of further secondary to Covid19 complications, such as cardiac complications or persistent myositis, is still being explored and it is likely the application of MRI in this area will expand as we understand more about this disease.
Technical considerations for Covid-19 imaging
CXR imaging of suspected or confirmed Covid-19 cases should be performed with portable equipment within specifically designated isolated rooms for eliminating the risks of cross-infection within the Radiology department.79 An anterioposterior (AP) chest radiograph is performed on the patient's bed, despite known limitations of this technique, such as sub-optimal evaluation of the cardiothoracic ratio. In contrast, when CXR is performed within Radiology, a posterioanterior (PA) standard technique must be used, as indicated. Due to known risks of cross-infection, extreme care must be taken in relation to the optimal use of personal protective equipment (PPE) and decontamination of surfaces.79
The technical quality of chest radiographs impacts diagnosis; mobile radiographs are performed on critically unwell patients and as a mechanism to reduce possible transmission. Suboptimal image quality may occur due to rotation, incorrect exposure and reduced inspiration. It is therefore always important for the radiographer to check that all the technical and image quality criteria are fulfilled for every examination, where possible, and that neither patients' nor radiographers’ safety is compromised. A plethora of guidelines on radiographic imaging considerations during the Covid-19 pandemic, including a 10-point check list and other helpful evaluation tools, have been produced by the International Society of Radiographers and Radiological Technologists (ISRRT).80
Regarding chest CT imaging, a standard unenhanced CT protocol81 and multidetector (MDCT) CT scanners can be used; the examination is carried out during the end-inspiration phase, when patients can follow breathing instructions. Reconstruction to 1.25 mm slice thickness and multi-planar reconstruction is suggested.82 , 83 In case of clinical indications of pulmonary embolism and elevated D-dimers levels, a contrast-enhanced CT should be performed.84 Low dose CT should be used in paediatric and pregnant patients, to minimise radiation.
Advantages and limitations
The advantages of CXR include portability, which prevents cross-infection within Radiology, cost-effectiveness, and wider availability. However, the sensitivity of the method is relatively low. On the contrary, chest CT has higher sensitivity (97–98%)73 , 74 but lacks specificity, it is not widely available, has a higher radiation dose compared to CXR and its use requires thorough decontamination of the scanner room impacting workflows. LUS offers the advantage of portability in the intensive care units or in a pre-hospital setting.70 However, its diagnostic role has yet to be established. The role of MRI is only ancillary in the case of neurological complications and its use should be strongly weighted against the impact on workflows, subject to the delays caused by decontamination.
National and international guidelines
After the outbreak of the Covid-19 pandemic, many professional bodies and learned societies have been quick to issue official guidelines on how medical imaging should optimally be performed for early diagnosis and related management of these patients, but also how staff should be protected from cross-infection. Proportionate recommendations are offered for the protection of Radiographers, as frontline staff. This knowledge is necessary for any medical imaging professional.
Subtle differences have been noted on the suggested imaging pathways among different countries (Table 4 ). This could be mainly attributed to differences on the availability of antigen testing or of imaging equipment, the variability of diagnostic methods and techniques used. There may also be disproportionate lack of the required specialised staff (i.e. radiographers) to operate the equipment, and also dissimilar policies for the management of the pandemic. However a common denominator is that in most guidelines and recommendations medical imaging investigations are reserved for those patients who are critically ill, for those with inconclusive or insufficient prior diagnostic tests but with persistent symptoms, consistent with Covid-19, and for those patients where clinical management decisions need to be imminently considered.
Table 4.
Summary of official guidelines regarding imaging of Covid-19 patients.
| Chest x-ray | Chest CT | Lung ultrasound | |
|---|---|---|---|
| British Society of Thoracic Imaginghttps://www.bsti.org.uk/ | For critically ill patients. For stable patients, only if clinically required. |
Only for critically ill patients who have inconclusive CXR results. | Suggested to be used as a monitoring tool in critically ill patients. |
| European Society of Radiology/European Society of Thoracic Imaginghttps://www.myesr.org/https://www.myesti.org/ | For imaging within ICU units. | Restricted use of chest CT is recommended. | Suggested to be used at the bedside. |
| American College of Radiologyhttps://www.acr.org/ | Not recommended for diagnosis. No impact on clinical outcomes. Mobile CXR is suggested when clinically necessary. | Not recommended unless imaging will have an impact on management. | No information included. |
| Canadian Association of Radiologists/Canadian Society of Thoracic Radiologyhttps://car.ca/covid-19/ | Limited use has been suggested, to those in whom results will change the management plan. Mobile CXR is recommended. | Not recommended unless clinically required. | No information included. |
| Royal College of Radiologistshttps://www.rcr.ac.uk/ | For critically ill patients. | Suggested to be used only in critically ill patients, and when is likely to change the management plan. | No information included. |
| Fleischner Society (an international consortium of medical imaging of the lungs)https://fleischner.memberclicks.net/ | Not recommended in patients with mild symptoms. Indicated for critically ill patients. Its lower sensitivity compared to CT is underlined. Final decision is left to clinicians. | Not recommended in patients with mild symptoms. Indicated for critically ill patients. Final decision is left to clinicians. | No information included. |
| Royal College of Surgeons of Edinburghhttps://www.rcsed.ac.uk/ | No information included. | Only when it is likely to change the management plan, and for patients who will need critical care in their postoperative recovery. | No information included. |
| Royal Australian and New Zealand College of Radiologistshttps://www.ranzcr.com/our-work/coronavirus/position-statements-and-guidance | Recommended for hospitalised patients and monitoring of the disease. | Not recommended. | No information included. |
| International Society of Radiographers & Radiological Technologists (ISRRT)https://www.isrrt.org/(resources shared with the EFRS website) | Mobile CXR is recommended. | Not recommended for diagnosis or as a first-line tool. | Mobile equipment is suggested to be used. |
Most of the Societies and professional bodies suggest that chest x-rays should be reserved for critically ill patients; the BSTI identifies as such those who demonstrate oxygen saturation values below 94% (90% for patients with known COPD).49 However, they conclude that chest radiographs should not be used as a first-line tool due to low sensitivity, and that they must be restricted to imaging for intensive care unit patients.35
Similarly, the professional bodies suggest that CT imaging is indicated for those patients with clinical symptoms and inconclusive or normal imaging features on CXR and that the use of CT imaging for Covid-19 should be based on clinical need and the possibility to change the management plan.85 Furthermore, the intercollegiate general surgery guidance86 proposes for CT chest to be performed alongside abdominal imaging, especially to those patients requiring emergency surgery. This may have occurred as a consequence of the many incidental findings in asymptomatic cases. In addition, gastrointestinal may be the only presenting symptoms, hence rigorous infection control protocols must be employed regardless of the lack of respiratory-related symptoms, and radiographers must be prepared to manage these patients.87 It is also reported that CT findings are not specific enough, and they can mimic other infections.88 Hence, CT imaging is recommended only if the clinical teams decide that it will have an impact on the management of the patient. The European bodies (ESR and ESTI) concur with the limited use of chest CT, underlining the potential risks of infection during patient transportation.
In line with the above and perhaps more conservatively to their European counterparts, North American professional bodies underline that no imaging, either CXR or CT, are recommended for the diagnosis of Covid-19, and that viral testing should be the first-line method for diagnosis of the disease.89
The European societies suggest that lung ultrasound should be used at the bedside, when needed, to eliminate the risks of further infection.35
The Fleischner Society, an international consortium of world-renowned experts in lung imaging, including radiologists and pulmonologists, states that imaging is not suggested for suspected Covid-19 patients with mild symptoms, but it is recommended for patients with severe symptoms and worsening respiratory status.90 In addition, they underline that CXR is less sensitive in the early/mild infection in contrast with chest CT, which offers much more information at this stage. However, the final decision is left to the clinicians, as the availability of these methods, expertise and resources have to be considered. Consequently, there is a consensus that imaging these patients must be generally limited to those critically ill, and that the clinicians at the point-of-care must always make a thoughtful risk-benefit analysis for these procedures, taking into account the stage of the disease and patient's clinical condition.
Some variability exists among countries regarding the use of medical imaging, mainly due to availability of resources and equipment, but also due to new scientific data about disease progression, which become available with time. However, radiographers should always consider these guidelines to avoid unnecessary staff and patient infection and to minimise radiation dose to patients by vetting the requested examinations or minimising radiation dose accordingly.
Safety for patients and staff
Infection control
Optimal infection control procedures must take place within the Radiology department, to minimise the potential risks of transmission of the virus to radiographers and other healthcare staff. Decontamination of the imaging equipment is vital, and it has been widely discussed within the literature.79 , 80 , 91, 92, 93 A recent study within Radiology departments suggested that imaging equipment such as CT scanner components must be disinfected every time after contamination with 2,000 mg/L chlorine-containing disinfectant and the CT gantry must be fully wiped with 75% ethanol.94 Also, after decontamination the CT room must be closed for 1 h for ventilation and air circulation.92 These studies are in line with the recommendations issued by the CAR and CSTR, who also suggest standardized disinfection protocols after imaging of all suspected or confirmed Covid-19 patients, as well as unavailability of the equipment for a period of time.89 Keyboards, viewing stations, ultrasound probes, are also suggested to be disinfected after exposure, with alcohol-containing disinfectants (Fig. 3 ).92 , 95 Radiology departments are encouraged to contact their vendors in order to specify the optimal disinfectants for every piece of equipment. In addition, all healthcare staff associated with cleaning, must be trained in optimal decontamination strategies, and Radiology managers must develop specific infection control protocols to enhance safety within the departments.96, 97, 98
Figure 3.
Visual summary of the basic guidelines regarding infection control and prevention in the radiological department from the JACR.92
Radiology departments must also re-organise their facilities and staff in order to enhance safety and minimise the risks of infection. A recent study suggested some effective ways to achieve this, such as segregating radiographers into teams. Furthermore, additional isolation rooms need to be created near the emergency department, where mobile radiography units can be deployed to minimise transferring patients. A two-radiographer team was found to effectively reduce the potential risks of cross-infection.99 When non-urgent imaging is reintroduced, where possible, patients should be cohorted, outpatients screened at first presentation and possible Covid-19 patients imaged using dedicated equipment, appropriate radiographer PPE and decontamination procedures.100 However, it is crucial that asymptomatic transmission is recognised early; radiographers working on the frontline could conduct a preliminary clinical evaluation, as one method to facilitate rapid identification of unsuspected Covid-19.39
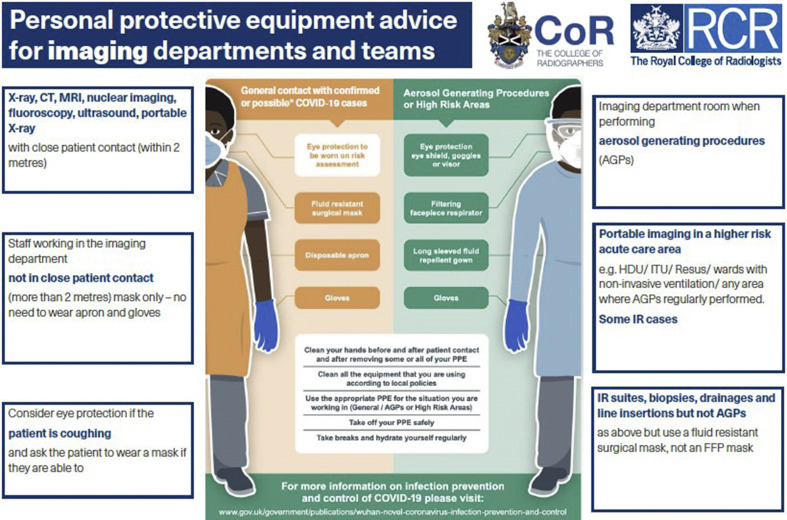
Personal protective equipment (PPE)
Personal Protective Equipment (PPE) is vital for radiographers and other frontline healthcare professionals, as they can help minimise the likelihood of infection. A shortage of PPE has been reported globally given the high demand. The use of PPE must be proportional to risk of exposure.101
A typical set of PPE for healthcare professionals consists of a long-sleeved gown, gloves, eye protection and a fluid repellent surgical mask or disposable respirator (N95, FFP2 or FFP3). This is the full PPE suggested by the European Centre for Disease Prevention and Control.102 However, the UK government suggests the use of aprons instead of a gown for non-aerosol generating procedures (Fig. 4 ).103 , 104 In addition, the sessional use of PPE, or reuse have been also recommended in case of extreme shortages, while the use of double gloves is not suggested. The Society of Radiographers (SoR) suggests that no radiographer should treat a patient without the PPE identified in the protocols.105 More guidance is also available on the ISRRT website80 in relation to this.
Figure 4.
PPE equipment advice for imaging departments and teams.104
Limitations
The Covid-19 pandemic is rapidly and continually evolving. What is certain is that medical imaging will continue to play a key role in supporting clinical decision-making. Further research is however needed to verify the added value of the different medical imaging modalities in diagnosis and patient management. Moreover, the epidemiology of the disease is constantly changing, often impacting on the imaging findings and imaging techniques required to delineate these. What is certain is that there is more to learn in the coming months, but the authors hope that this paper will be a first tool, useful to summarise current knowledge for the radiography workforce at the frontline.
Conclusion
Medical imaging has a pivotal role in the Covid-19 pandemic, offering the advantage of supplementary diagnosis and follow-up of the critically ill patients. Radiographers, as frontline staff, should be familiar with the main challenges and controversies related to imaging patients with Covid-19 so they can fulfill their role in safeguarding patient safety, patient care, optimise image quality as a tool for more accurate diagnosis, but also to engage in their reporting roles. Most importantly, they should be aware of ways to keep themselves safe and well during this unprecedented situation by correctly using the right PPE and ensuring all their workspaces are adequately decontaminated to minimise the risk of further infection.
Conflict of interest statement
None
Acknowledgements
City Radiography Research Fund can be listed as a funder of this project. Unrelated to the current submission, Dr Nick Woznitza is a clinical advisor to InHealth.
Contributor Information
N. Stogiannos, Email: nstogiannos@yahoo.com.
D. Fotopoulos, Email: d.fotopoulos@mbht.nhs.uk.
N. Woznitza, Email: Nicholas.woznitza@nhs.net.
C. Malamateniou, Email: christina.malamateniou@city.ac.uk.
References
- 1.World Health Organization Coronavirus disease 2019 (COVID-19) situation report-120. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200519-covid-19-sitrep-120.pdf?sfvrsn=515cabfb_2 Available from:
- 2.Worldometersinfo [Internet] Reported cases and deaths by country, territory, or conveyance. https://www.worldometers.info/coronavirus/ Available from:
- 3.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; StatPearls Treasure Island (FL): 2020. Features, evaluation and treatment coronavirus (COVID-19)https://www.ncbi.nlm.nih.gov/books/NBK554776/ [Internet] Available from: [PubMed] [Google Scholar]
- 4.Hassan S., Sheikh F.N., Jamal S., Ezeh J.K., Akhtar A. Coronavirus (COVID-19): a review of clinical features, diagnosis, and treatment. Cureus. 2020;12(3) doi: 10.7759/cureus.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yi Y., Lagniton P.N.P., Ye S., Li E., Xu R.H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020;16(10):1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C., Wang Y., Li X., Zhao J., Hu Y., Zhang L. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zu Z.Y., Jiang M.D., Xu P.P., Chen W., Ni Q.Q., Lu G.M. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 doi: 10.1148/radiol.2020200490. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lechien J.R., Chiesa-Estomba C.M., De Siati D.R., Horoi M., Le Bon S.D., Rodriguez A. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Oto-Rhino-Laryngol. 2020;277(1):1–7. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo S., Zhang X., Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-2019) Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.03.043. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu S., Lin J., Zhang Z., Xiao L., Jiang Z., Chen J. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. In Press. [DOI] [PubMed] [Google Scholar]
- 12.Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.031. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khafaie M.A., Rahim F. Cross-Country comparison of case fatality rates of COVID-19/SARS-COV-2. Osong Public Health Res Perspect. 2020;11(2):74–80. doi: 10.24171/j.phrp.2020.11.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grech V. Unknown unknows-COVID-19 and potential global morality. Early Hum Dev. 2020;144 doi: 10.1016/j.earlhumdev.2020.105026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Guan W.J., Liang W.H., Zhao Y., Liang H., Chen Z., Li Y. Comorbidity and its impact on 1590 patients with covid-19 in China: a nationwide analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00547-2020. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang B., Li R., Lu Z., Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging. 2020;12(7):6049–6057. doi: 10.18632/aging.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):e35. PMCID: PMC7096724. [PMC free article] [PubMed] [Google Scholar]
- 19.National Institute for Health and Care Excellence COVID-19 rapid guideline: managing symptoms (including at the end of life) in the community. https://www.nice.org.uk/guidance/ng163 Available from: [PubMed]
- 20.Centers for Disease Control and Prevention People with moderate to severe asthma. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html Available from:
- 21.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abbatecola A.M., Antonelli-Incalzi R. COVID-19 spiraling of frailty in older Italian patients. J Nutr Health Aging. 2020 doi: 10.1007/s12603-020-1357-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J. SARS-Cov-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. CDC COVID-19 response team Coronavirus Disease 2019 in children-United States. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6914e4-H.pdf february 12-april 2, 2020. Available from:
- 25.Tezer H., Bedir Demirdag T. Novel coronavirus disease (COVID-19) in children. Turk J Med Sci. 2020;50:592–603. doi: 10.3906/sag-2004-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics Provisional death counts for coronavirus disease (COVID-19) https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm#AgeAndSex Available from:
- 28.Udugama B., Kadhiresan P., Koslowski H.N., Malekjahani A., Osborne M., Li V.I.C. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020 doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 29.Zhai P., Ding Y., Wu X., Long J., Zhong Y., Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105955. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Yao L., Li J., Chen L., Song Y., Cai Z. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.25786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiao A.T., Tong Y.X., Gao C., Zhu L., Zhang Y.J., Zhang S. Dynamic profile of RT-PCR findings from 301 COVID-19 patients in Wuhan, China: a descriptive study. J Clin Virol. 2020:104346. doi: 10.1016/j.jcv.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kontou P.I., Braliou G.G., Dimou N.L., Nikolopoulos G., Bagos P.G. Antibody tests in detecting SARS-CoV-2 infection: a meta-analysis. 2020. [DOI] [PMC free article] [PubMed]
- 33.Lippi G., Plebani M. The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks. Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0240. In Press. [DOI] [PubMed] [Google Scholar]
- 34.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.-Q. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Revel M.P., Parkar A.P., Prosch H., Silva M., Sverzellati N., Gleeson F. COVID-19 patients and the radiology department-advice from the European society of radiology (ESR) and the European society of thoracic imaging (ESTI) Eur Radiol. 2020 doi: 10.1007/s00330-020-06865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang W., Sirajuddin A., Zhang X., Liu G., Teng Z., Zhao S. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19) Eur Radiol. 2020 doi: 10.1007/s00330-020-06827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dai W., Zhang H., Yu J., Xu H., Chen H., Luo S. CT imaging and differential diagnosis of COVID-19. Can Assoc Radiol J. 2020;79(2):195–200. doi: 10.1177/0846537120913033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobi A., Chung M., Bernheim A., Eber C. Portable chest x-ray in coronavirus disease-19 (COVID-19): a pictorial review. Clin Imag. 2020;64:35–42. doi: 10.1016/j.clinimag.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woznitza N., Nair A., Hare S.S. COVID-19: a case series to support radiographer preliminary clinical evaluation. Radiography. 2020;26(3):e186–e188. doi: 10.1016/j.radi.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong H.Y.F., Lam H.Y.S., Fong A.H., Leung S.T., Chin T., Lo C.S.Y. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020 doi: 10.1148/radiol.2020201160. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutierrez-Ocampo E., Villamizar-Pena R., Holguin-Rivera Y., Escalera-Antezana J.P. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Trav Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101623. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lomoro P., Verde F., Zerboni F., Simonetti I., Borghi C., Fachinetti C. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7:100231. doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fan L., Li D., Xue H., Zhang L., Liu Z., Zhang B. Progress and prospect on imaging diagnosis of COVID-19. Chin J Acad Radiol. 2020;3:4–13. doi: 10.1007/s42058-020-00031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020:215. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 45.Zhao D., Yao F., Wang L., Zheng L., Gao Y., Ye J. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bandirali M., Sconfienza L.M., Serra R., Brembillall R., Albano D., Pregliasco E. Chest radiograph findings in asymptomatic and minimally symptomatic quarantined patients in Codogno, Italy during COVID-19 pandemic. Radiology. 2020;295(3):E7. doi: 10.1148/radiol.2020201102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yoon S.H., Lee K.H., Kim J.Y., Lee Y.K., Ko H., Kim K.H. Chest radiographic and CT findings of the 2019 novel Coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21(4):494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.British Society of Thoracic Imaging Radiology decision tool for suspected COVID-19. https://www.bsti.org.uk/media/resources/files/NHSE_BSTI_APPROVED_Radiology_on_CoVid19_v6_modified1__-_Read-Only.pdf Available from:
- 50.Kang Z., Li X., Zhou S. Recommendation of low-dose CT in the detection and management of COVID-19. Eur Radiol. 2020:1–2. doi: 10.1007/s00330-020-06809-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.British Society of Thoracic Imaging Guidance for the reporting radiologist. https://www.bsti.org.uk/media/resources/files/BSTI_COVID-19_Radiology_Guidance_version_2_16.03.20.pdf Available from:
- 52.Li X., Zeng W., Li X., Chen H., Shi L., Li X. CT imaging changes of corona virus disease 2019 (COVID-19): a multi-center study in Southwest China. J Transl Med. 2020;18:154. doi: 10.1186/s12967-020-02324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bao C., Liu X., Zhang H., Li Y., Liu J. Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.03.006. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cao Y., Liu X., Xiong L., Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2: a systematic review and meta-analysis. J Med Virol. 2020:1–11. doi: 10.1002/jmv.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang H., Wei R., Rao G., Zhu J., Song B. Characteristic CT findings distinguishing 2019 novel coronavirus disease (COVID-19) from influenza pneumonia. Eur Radiol. 2020 doi: 10.1007/s00330-020-06880-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jin Y., Cai L., Cheng Z., Cheng H., Deng T., Fan Y.-P. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7(4) doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grillet F., Behr J., Calame P., Aubry S., Delabrousse E. Acute pulmonary embolism associated with COVID-19 pneumonia detected by pulmonary CT angiography. Radiol. 2020 doi: 10.1148/radiol.2020201544. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leonard-Lorant I., Delabranche X., Severac F., Helms J., Pauzet C., Collange O. Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship with D-Dimer levels. Radiol. 2020 doi: 10.1148/radiol.2020201561. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wei X., Jianbo S., Yu G., Xuehua P., Zhen L., Daoyu H. Clinical and CT features in pediatric patients with COVID-19 infection: different points of adults. Pediatr Pulmonol. 2020;55:1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Duan Y.N., Zhu Y.Q., Tang L.L., Qin J. CT features of novel coronavirus pneumonia (COVID-19) in children. Eur Radiol. 2020:1–7. doi: 10.1007/s00330-020-06860-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen A., Huang J., Liao Y., Liu Z., Chen D., Yang C. Differences in clinical and imaging presentation of pediatric patients with COVID-19 in comparison to adults. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu H., Liu F., Li J., Zhang T., Wang D., Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J Infect. 2020;80:e7–e13. doi: 10.1016/j.jinf.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang Y.X.J., Liu W.-H., Yang M., Chen W. The role of CT for Covid-19 patient's management remains poorly defined. Ann Transl Med. 2020;8(4):145. doi: 10.21037/atm.2020.02.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pan Y., Guan H., Zhou S., Wang Y., Li Q., Zhu T. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ding X., Xu J., Zhou J., Long Q. Chest CT findings of COVID-19 pneumonia by duration of symptoms. Eur J Radiol. 2020;127:109009. doi: 10.1016/j.ejrad.2020.109009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Samsami M., Zebarjadi Bagherpour J., Nematihonar B., Tahmasbi H. COVID-19 pneumonia in asymptomatic trauma patients; report of 8 cases. Arch Acad Emerg Med. 2020;8(1):e46. [PMC free article] [PubMed] [Google Scholar]
- 67.Albano D., Bertagna F., Bertolia M., Bosio G., Lucchini S., Motta F. Incidental findings suggestive of COVID-19 in asymptomatic patients undergoing Nuclear Medicine procedures in a high prevalence region. J Nucl Med. 2020 doi: 10.2967/jnumed.120.246256. [DOI] [PubMed] [Google Scholar]
- 68.Buonsenso D., Piano A., Raffaelli F., Bonadia N., de Gaetano Donati K., Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24(5):2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- 69.Moore S., Gardiner E. Point of care and intensive care lung ultrasound: a reference guide for practitioners during COVID-19. Radiography. 2020 doi: 10.1016/j.radi.2020.04.005. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. 2020;9999:1–4. doi: 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Elmahalawy, Doha N.M., Ebeid O.M., Abdel-Hady M.A., Saied O. Role of thoracic ultrasound in diagnosis of pulmonary and pleural diseases in critically ill patients. Egypt J Chest Dis Tuberc. 2017;66(2):261–266. doi: 10.1016/j.ejcdt.2016.10.005. [DOI] [Google Scholar]
- 72.Isikbay M., Hope M.D., Raptis C.A., Shah A., Bierhals A.J., Bhalla S. CT on the Diamond Princess: what might this tell us about sensitivity for COVID-19? Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 doi: 10.1148/radiol.2020200432. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Caruso D., Zerunian M., Polici M., Pucciarelli F., Polidori T., Rucci C. Chest CT features of COVID-19 in rome, Italy. Radiology. 2020 doi: 10.1148/radiol.2020201237. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Poggiali E., Dacrema A., Bastoni D., Tinelli V., Demichele E., Ramos P.M. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID-19) pneumonia? Radiology. 2020 doi: 10.1148/radiol.2020200847. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Filatov A., Sharma P., Hindi F., Espinosa P.S. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12(3) doi: 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute necrotizing hemorrhagic encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.British society of thoracic imaging. EXAMPLE covid-19 action card. Radiology portable CXR’s-‘at risk’ patients in ED or wards. https://www.bsti.org.uk/media/resources/files/Covid-19_CXR.pdf Available from:
- 80.International Society of Radiographers & Radiological Technologists International COVID-19 support for radiographers and radiologic Technologists. https://www.elearning.isrrt.org/mod/book/view.php?id=287&forceview=1 Available from:
- 81.Rodrigues J.C.L., Hare S.S., Edey A., Devaraj A., Jacob J., Johnstone A. An update on COVID-19 for the radiologist-A British society of Thoracic Imaging statement. Clin Radiol. 2020;75(5):323–325. doi: 10.1016/j.crad.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020;214 doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 83.Zhou S., Wang Y., Zhu T., Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in wuhan, China. AJR Am J Roentgenol. 2020;214:1–8. doi: 10.2214/AJR.20.22975. [DOI] [PubMed] [Google Scholar]
- 84.Rotzinger D.C., Beigelman-Aubry C., von Garnier C., Qanadli S.D. Pulmonary embolism in patients with COVID-19: time to change the paradigm of computed tomography. Thromb Res. 2020;190:58–59. doi: 10.1016/j.thromres.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Royal College of Radiologists RCR position on the role of CT in patients suspected with COVID-19 infection. https://www.rcr.ac.uk/college/coronavirus-covid-19-what-rcr-doing/clinical-information/rcr-position-role-ct-patients Available from:
- 86.Royal College of Surgeons of Edinburgh Intercollegiate general surgery guidance on COVID-19 UPDATE. https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update Available from:
- 87.Wilson M.P., Katlariwala P., Low G. Potential implications of novel coronavirus disease (COVID-19) related gastrointestinal symptoms for abdominal imaging. Radiography. 2020;26(3):274. doi: 10.1016/j.radi.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.American College of Radiology ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection Available from:
- 89.Canadian Association of Radiologists The Canadian association of radiologists (CAR) and the Canadian society on thoracic radiology recommendations on COVID-19 management in imaging departments. https://car.ca/wp-content/uploads/2020/03/CAR-CSTR-COVID-19-Recommendations-En.pdf Available from:
- 90.Rubin G.D., Ryerson C.J., Haramati L.B., Sverzellati N., Kanne J.P., Raoof S. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Chest. 2020. In Press. [DOI] [PMC free article] [PubMed]
- 91.Nakajima K., Kato H., Yamashiro T., Izumi T., Takeuchi I., Nakajima H. COVID-19 pneumonia: infection control protocol inside computed tomography suites. Jpn J Radiol. 2020 doi: 10.1007/s11604-020-00948-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kooraki S., Hosseiny M., Myers L., Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mirza S.K., Tragon T.R., Fukui M.B., Hartman M.S., Hartman A.L. Microbiology for Radiologists: how to minimize infection transmission in the radiology department. Radiographics. 2015;35:1231–1244. doi: 10.1148/rg.2015140034. [DOI] [PubMed] [Google Scholar]
- 94.Huang Z., Zhao S., Li Z., Chen W., Zhao L., Deng L. The battle against coronavirus disease 2019 (COVID-19): emergency management and infection control in a radiology department. J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.03.011. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zanardo M., Martini C., Monti C.B., Cattaneo F., Ciaralli C., Cornacchione P. Management of patients with suspected or confirmed COVID-19, in the radiology department. Radiography. 2020;26(3):264–268. doi: 10.1016/j.radi.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mohakud S., Ranjan A., Naik S., Deep N. COVID-19 preparedness for portable x-rays in an Indian hospital-Safety of the radiographers, the frontline warriors. Radiography. 2020;26(3):270–271. doi: 10.1016/j.radi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yu J., Ding N., Chen H., Liu X.-J., He W., Dai W. Infection control against COVID-19 in departments of Radiology. Acad Radiol. 2020;27(5):614–617. doi: 10.1016/j.acra.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang H.-W., Yu J., Xu H.-J., Lei Y., Pu Z.-H., Dai W.-C. Corona virus international public Health emergencies: implications for radiology management. Acad Radiol. 2020;27(4):463–467. doi: 10.1016/j.acra.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sim W.Y., Ooi C.C., Chen R.C., Bakar R.A., Tan C.C., Heng A.L. How to safely and sustainably reorganise a large general radiography service facing the COVID-19 pandemic. Radiography. 2020 doi: 10.1016/j.radi.2020.05.001. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mossa-Basha M., Azadi J., Klein J., Menias C., Filippi C., Tan B.S. RSNA COVID-19 task force: post-COVID surge radiology preparedness. https://www.rsna.org/-/media/Files/RSNA/covid-19/RSNA-COVID-19-PostSurgePreparedness.pdf Available from:
- 101.World Health Organization [Internet] Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19) Interim guidance. 19 March 2020 https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf?sequence=1&isAllowed=y Available from: [Google Scholar]
- 102.European Centre for Disease Prevention and Control Guidance for wearing and removing personal protective equipment in healthcare settings for the care of patients with suspected or confirmed COVID-19. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-guidance-wearing-and-removing-personal-protective-equipment-healthcare-settings-updated.pdf Available from:
- 103.Department of Health and Social Care Covid-19: personal protective equipment (PPE) plan. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879221/Coronavirus__COVID-19__-_personal_protective_equipment__PPE__plan.pdf Available from:
- 104.Royal College of Radiologists Personal protective equipment advice for imaging departments and teams. https://www.rcr.ac.uk/sites/default/files/radiology_ppe_poster_a3.pdf?utm_source=twitter&utm_medium=social&utm_tem=radiology_ppe_pdf&utm_campaign=covid19 Available from:
- 105.Society of Radiographers Covid-19: personal protective equipment (PPE) https://www.sor.org/news/covid-19-personal-protective-equipment-ppe Available from: