Abstract
Decubitus ulcer is a common complication in patients with spinal cord injury (SCI) that can be very difficult to treat. We report a case of a 51-year-old man with a right-heel decubitus ulcer after SCI. The ulcer initially covered an area of 4.8 cm × 4.5 cm and had a depth of 2 cm with denervation and hypoproteinemia. After surgical debridement of the wound, the patient received radial extracorporeal shock wave therapy (rESWT) as an alternative to skin flap transplantation to promote wound healing. The rESWT was administered at 10 Hz once or twice per week for 3 months, first from an R15 transmitter and later from a deep transmitter, with an increasing dosage of 2.0-3.5 bar given in 3000-6000 pulses. After 3 months of rESWT, the ulcer was completely healed. This case report demonstrates that rESWT can be an effective treatment option for patients with decubitus ulcers.
Keywords: Radial extracorporeal shock wave therapy, decubitus ulcer, spinal cord injury
Introduction
A decubitus ulcer is an area of localized damage to a tissue surface caused by prolonged pressure from compression or shear [1]. Decubitus ulcers are the most common complication associated with spinal cord injury (SCI), often occurring within a few days following SCI [2,3]. Many factors contribute to decubitus ulcers in patients with SCI, including loss of motor function and pain and pressure sensation, poor nutrition, anemia, and other factors [4]. The treatment of decubitus ulcer is a major clinical challenge. Patients with decubitus ulcer are often subjected to long hospital stays and devastation of quality of life, resulting in a financial burden to family and society [3,5].
Conventional therapies for decubitus ulcers include improvement of nutrition, removal of pressure, debridement, treatment of infection, application of dressings, and surgery [4]. Those therapies often fail to result in full healing of the wound, however, and sometimes they provide very little benefit.
Extracorporeal shock wave therapy (ESWT) is a safe, noninvasive, alternative treatment modality that has been used successfully in patients with various musculoskeletal problems, ischemic heart disease, and other conditions [6-8]. In contrast to conventional focused extracorporeal shock wave therapy (fESWT), radial extracorporeal shock wave therapy (rESWT) uses a type of pneumatically generated shock wave that disperses eccentrically from the transmitter without focusing the energy to a targeted spot [9]. Thus, rESWT can be applied to larger and more superficial treatment areas than fESWT. Different transmitters can be used to adjust the penetration depth and energy of rESWT [10,11], making it possible to use rESWT in a wide variety of clinical situations. Although rESWT is used to treat many diseases and conditions, including carpal tunnel syndrome, hemiplegic shoulder pain syndrome, and muscle spasms, there are few reports of its use in patients with refractory decubitus ulcer [12-14]. Here, we report on a patient with intractable decubitus ulcer who achieved complete recovery after receiving rESWT.
Case report
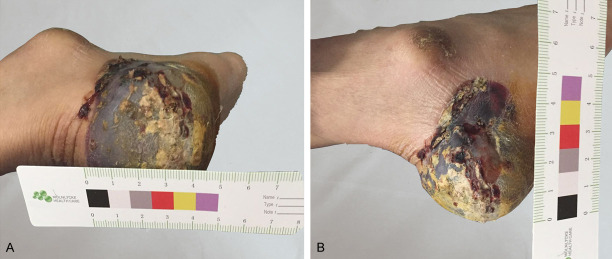
A 51-year-old man presented to the department in March 2016. The patient had a 21 day history of right-heel decubitus ulcer after SCI of the first lumbar vertebra complicated with pelvic fracture due to trauma (Figure 1). The decubitus ulcer started as a blood blister that first appeared one day after the patient underwent internal screw fixation of a first lumbar vertebra fracture. After the surgery, the patient suffered from motor and sensory disturbance of the lower limbs. Within 10 days, the blood blister progressed to a ulcer that penetrated to a depth of 2 cm and covered an area of 4.8 cm × 4.5 cm. The patient was treated with iodophor disinfection solution and external application of traditional Chinese medicine at a local hospital, but the decubitus ulcer worsened in terms of its surface area and depth.
Figure 1.
Right heel decubitus ulcer. A 51-year-old man presented with a 21-day history of a right-heel decubitus ulcer with an area of 4.8 cm × 4.5 cm and a depth of 2 cm. Blood blisters were visible on the wound surface. Traditional Chinese medicine had been applied to the wound.
The patient was 173 cm tall and weighed 70 kg before the spinal surgery. Twenty-one days after the spinal surgery, the patient had lost 4 kg of body weight and had the following clinical parameters: white blood cell count 8.34 × 109/L (normal range: 3.5-9.5 × 109/L), neutrophil percentage 80.7% (normal range: 40-75%), platelet count 231 × 109/L (normal range: 125-350 × 109/L), hemoglobin level 130 g/L (normal range: 130-175 g/L), serum albumin level 30.7 g/L (normal range: 40-50 g/L), C-reactive protein level 61 mg/L (normal range: 0-8 mg/l), procalcitonin level 0.12 ng/mL (normal range: 0-0.05 ng/mL), and fasting glucose level 4.78 mmol/L (normal range: 3.9-6.1 mmol/L). Renal and liver functions were normal.
The standard treatment for intractable decubitus ulcer involves surgical debridement and skin flap transplantation. Accordingly, the necrotic tissue was surgically debrided from the patient’s right heel by a general surgeon. The wound bled little during the surgery. Because the survival of transplanted skin flaps depends on the local microvessel density and hemoperfusion [15], and the patient suffered from poor circulation and nutritional status and displayed neurological impairment of the lower limbs, we determined that implanted skin flaps might not heal sufficiently and might even become infected or necrotic.
Therefore, as an alternative to skin flap transplantation, we treated the wound with intermittent ultra short-wave and rESWT (STORZ MEDICAL AG, Switzerland). In the first week after the decubitus ulcer was surgically debrided, we treated the patient once with 3000 pulses of rESWT at 10 Hz and 2.0 bar intensity using an R15 transmitter with a 15-mm diameter. For the rESWT application, the ulcer areas were covered by plastic sterile wound dressings (Zhejiang Kanglidi Medical Articles Co., Ltd), and the transmitter was wrapped in one finger of a sterile plastic glove. The procedure was performed without local anesthesia. Transmission gel was applied between the applicator and the wound. The applicator was moved slowly around the wound area, including at least 3 cm of healthy tissue around the wound edge. After the first rESWT treatment, the patient displayed good growth of local tissue. Therefore, in the following week, we treated the patient twice with 4000 pulses of rESWT at 3.0 bar. After the first 2 weeks of rESWT, the wound area had a rich blood supply and was partly scabbed (Figure 2). Starting in the third week, to accelerate the wound healing process, we replaced the R15 transmitter with a deep transmitter (diameter, 15 mm) and continued treating the patient with 4000 pulses at 3.0 bar twice per week [11]. One month later, the peripheral areas of the ulcer had healed (Figure 3), so we increased the rESWT dose to 6000 pulses at 3.5 bar and 10 Hz applied twice per week. Three months after the start of rESWT, the decubitus ulcer was completely healed (Figure 4).
Figure 2.

Image of the ulcer after 2 weeks of rESWT. rESWT was applied for 2 weeks after surgical debridement of the decubitus ulcer. The wound area had a rich blood supply and was partially scabbed. Fresh bloody exudation was seen around the wound, and the wound area was reduced to 3.5 cm × 2.5 cm.
Figure 3.

Image of the ulcer after 1 month of rESWT. The dose of rESWT was adjusted according to the observed healing of the ulcer. The wound area was reduced to 1.5 cm × 1.5 cm. The tissue surrounding the wound had healed, and the middle portion was scabbed after 1 month of weekly or bi-weekly rESWT.
Figure 4.
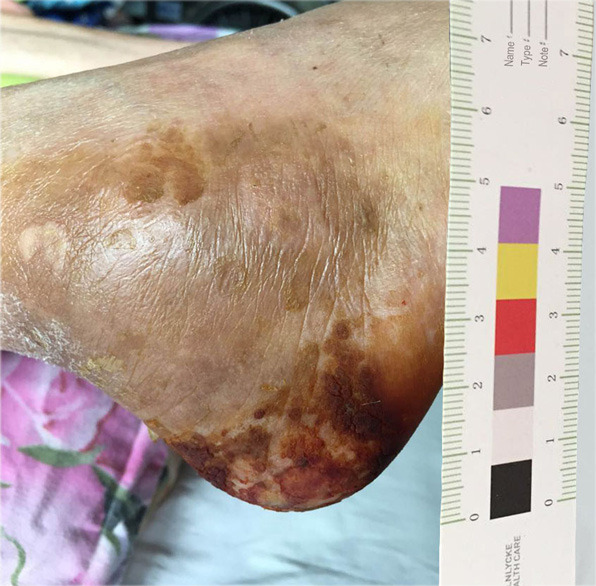
Image of the ulcer after 3 months of rESWT. After 3 months of rESWT, the scab fell off, and the ulcer was wholly healed.
Discussion
The application of rESWT to a surgically debrided decubitus ulcer on the heel of a patient with SCI resulted in complete healing of the wound after 3 months. Lower-limb decubitus ulcer is reported as a common problem worldwide [16]. Poor healing of decubitus ulcer is a troublesome clinical problem. The management of ulceration may include both non-surgical and surgical approaches, depending on the clinical details of the case [17]. The deep tissue penetration and large surface area of the ulcer described in this case report would usually be indications for skin flap transplantation after surgical debridement of the wound. Surgical debridement left a large cavity that drained poorly, however, which increased the risk of infection and treatment failure. In addition, the patient had poor nutritional status and loss of sensory function in the distal tissues as a result of SCI, which greatly increased the risk of skin flap necrosis. Therefore, to promote wound healing, we decided to treat the patient with ESWT, a noninvasive and safe therapy.
ESWT is widely used to treat chronic soft tissue injuries and had beneficial effects in various preclinical and clinical studies [18,19]. In one study, ESWT significantly reduced the size of digital ulcers and produced no adverse reactions in patients with systemic sclerosis [20]. In patients with deep-partial/full-thickness burns, ESWT played an important role as an adjuvant therapy and reduced burn-associated pruritus [21,22]. Those clinical results suggest that the enhancing effects of ESWT on wound healing might make ESWT suitable for the treatment of decubitus ulcers. Indeed, there are some reports of beneficial effects of ESWT in the treatment of ulcers; however, those reports described only incomplete healing or excluded deep ulcers [23,24].
ESWT is classified into fESWT and rESWT on the basis of the reflector design, which in part determines the pressure field and energy [12]. rESWT represents a breakthrough in clinical treatment because of its simplicity and safety. For instance, rESWT requires no anesthesia or image-guided location, and it lessens the risks of adverse reactions compared with fESWT by reflecting the pathology zone [24-26]. Decubitus ulcer is caused by local tissue hypoxia due to extrinsic pressure, friction, shear stress, and excessive moisture on the skin [27]. Because rESWT provides more superficial action over a larger surface area than fESWT, it might be more suitable for application in patients with external structure pathology such as decubitus ulcer [28]. Moreover, in rESWT, the transmitter can be moved during the application in order to achieve a wider range of management. By contrast, fESWT is fixed on one site. In general, the frequency of rESWT (1-22 Hz) is higher than that of fESWT (1-5 Hz). Therefore, if the same pulses are applied, rESWT can be performed in less time than fESWT, which tends to make patients more compliant. For all of those reasons, we decided to administer rESWT to our patient with lower-limb decubitus ulcer.
Although the surgical debridement left a large cavity, the decubitus ulcer was totally healed after 3 months of rESWT. We progressively increased the dose of rESWT according to the observed healing of the wound, eventually reaching a dosage of 6000 pulses at 3.5 bar given from a deep transmitter twice per week. Generally, the higher the dose, the greater the treatment effects, meaning that fewer sessions are required when higher doses are used [29,30].
The effects of rESWT were excellent, but the exact mechanisms by which rESWT promotes healing of decubitus ulcers remain poorly understood. Shock waves might increase the expression of angiogenesis-related growth factors such as nitric oxide synthase (eNOS), vascular endothelial growth factor (VEGF), and proliferative cell nuclear antigen (PCNA) [31,32]. Those factors would promote angiogenesis, leading to increased blood perfusion and reduced risk of ischemia, which is a major problem in ulcers [21]. One study found that shock wave therapy enhanced the migration of fibroblasts to wound areas [33], which suggests that shock waves modulate fibroblast recruitment and thus promote tissue remodeling [34]. Other reports showed that shock waves promoted the migration of circulating endothelial progenitor cells to chronically ischemic tissues [35], which suggests that shock wave therapy might accelerate decubitus ulcer healing by stimulating stem cells. Some studies showed that shock waves reduced inflammatory cell recruitment and cell apoptosis in wound areas [19,34], which might contribute to faster healing. Beyond that, a threshold number of more than 1000 impulses was shown to reduce bacterial growth [36], suggesting that the application of shock waves might help to prevent or even cure infections. In our case study, the large, hypoproteinemic wound on the patient’s lower limb did not become infected, possibly as a result of shock wave therapy.
In conclusion, among the various therapies that can be used to treat decubitus ulcer in the lower extremities, rESWT represents a safe, simple, and effective treatment option. A patient with decubitus ulcer of the lower limb after SCI was treated with surgical debridement and subsequent rESWT as an alternative to skin flap transplantation. The wound did not become infected after debridement and was completely healed after 3 months of rESWT. Thus, rESWT was a noninvasive and cost-effective alternative to skin flap transplantation for the treatment of a deep and large decubitus ulcer.
Acknowledgements
We thank Xiaotong Yu for assistance with the radial shock wave instrument. We gratefully acknowledge the clinical information provided by the patient.
Disclosure of conflict of interest
None.
References
- 1.Shi C, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention: a network meta-analysis. PLoS One. 2018;13:e0192707. doi: 10.1371/journal.pone.0192707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haisma JA, van der Woude LH, Stam HJ, Bergen MP, Sluis TA, Post MW, Bussmann JB. Complications following spinal cord injury: occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. J Rehabil Med. 2007;39:393–398. doi: 10.2340/16501977-0067. [DOI] [PubMed] [Google Scholar]
- 3.Liu LQ, Moody J, Traynor M, Dyson S, Gall A. A systematic review of electrical stimulation for pressure ulcer prevention and treatment in people with spinal cord injuries. J Spinal Cord Med. 2014;37:703–718. doi: 10.1179/2045772314Y.0000000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Recio AC, Felter CE, Schneider AC, McDonald JW. High-voltage electrical stimulation for the management of stage iii and iv pressure ulcers among adults with spinal cord injury: demonstration of its utility for recalcitrant wounds below the level of injury. J Spinal Cord Med. 2012;35:58–63. doi: 10.1179/2045772311Y.0000000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36:572–585. [Google Scholar]
- 6.Al-Abbad H, Simon JV. The effectiveness of extracorporeal shock wave therapy on chronic achilles tendinopathy: a systematic review. Foot Ankle Int. 2013;34:33–41. doi: 10.1177/1071100712464354. [DOI] [PubMed] [Google Scholar]
- 7.Ito K, Fukumoto Y, Shimokawa H. Extracorporeal shock wave therapy for ischemic cardiovascular disorders. Am J Cardiovasc Drugs. 2011;11:295–302. doi: 10.2165/11592760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Kieves NR, MacKay CS, Adducci K, Rao S, Goh C, Palmer RH, Duerr FM. High energy focused shock wave therapy accelerates bone healing. A blinded, prospective, randomized canine clinical trial. Vet Comp Orthop Traumatol. 2015;28:425–432. doi: 10.3415/VCOT-15-05-0084. [DOI] [PubMed] [Google Scholar]
- 9.Li TY, Chang CY, Chou YC, Chen LC, Chu HY, Chiang SL, Chang ST, Wu YT. Effect of radial shock wave therapy on spasticity of the upper limb in patients with chronic stroke: a prospective, randomized, single blind, controlled trial. Medicine (Baltimore) 2016;95:e3544. doi: 10.1097/MD.0000000000003544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seol PH, Ha KW, Kim YH, Kwak HJ, Park SW, Ryu BJ. Effect of radial extracorporeal shock wave therapy in patients with fabella syndrome. Ann Rehabil Med. 2016;4:1124–1128. doi: 10.5535/arm.2016.40.6.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Storz Medical Masterpuls MP200. Indications-concise instruction. https://www.storzmedical.com/images/brochures/MASTERPULS_MP50_MP100_MP200_en/
- 12.Ke MJ, Chen LC, Chou YC, Li TY, Chu HY, Tsai CK, Wu YT. The dose-dependent efficiency of radial shock wave therapy for patients with carpal tunnel syndrome: a prospective, randomized, single-blind, placebo-controlled trial. Sci Rep. 2016;6:38344. doi: 10.1038/srep38344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim SH, Ha KW, Kim YH, Seol PH, Kwak HJ, Park SW, Ryu BJ. Effect of radial extracorporeal shock wave therapy on hemiplegic shoulder pain syndrome. Ann Rehabil Med. 2016;40:509–519. doi: 10.5535/arm.2016.40.3.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T, Du L, Shan L, Dong H, Feng J, Kiessling MC, Angstman NB, Schmitz C, Jia F. A prospective case-control study of radial extracorporeal shock wave therapy for spastic plantar flexor muscles in very young children with cerebral palsy. Medicine (Baltimore) 2016;95:e3649. doi: 10.1097/MD.0000000000003649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lei J, Hou C, Duan P, Hao Z, Zhai Y, Meng Y. Clinical application of modified skin soft tissue expansion in early repair of devastating wound on the head due to electrical burn. Zhonghua Shao Shang Za Zhi. 2015;31:406–409. [PubMed] [Google Scholar]
- 16.Fioramonti P, Onesti MG, Fino P, Fallico N, Scuderi N. Extracorporeal shock wave therapy for the treatment of venous ulcers in the lower limbs. Ann Ital Chir. 2012;83:41–44. [PubMed] [Google Scholar]
- 17.Attinger CE, Janis JE, Steinberg J, Schwartz J, Al-Attar A, Couch K. Clinical approach to wounds: debridement and wound bed preparation including the use of dressings and wound-healing adjuvants. Plast Reconstr Surg. 2006;117:72S–109S. doi: 10.1097/01.prs.0000225470.42514.8f. [DOI] [PubMed] [Google Scholar]
- 18.Dolibog P, Franek A, Brzezinska-Wcislo L, Dolibog P, Wrobel B, Arasiewicz H, Chmielewska D. Shockwave therapy in selected soft tissue diseases: a literature review. J Wound Care. 2018;27:573–583. doi: 10.12968/jowc.2018.27.9.573. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi AA, Ross KM, Ogawa R, Orgill DP. Shock wave therapy in wound healing. Plast Reconstr Surg. 2011;128:721e–727e. doi: 10.1097/PRS.0b013e318230c7d1. [DOI] [PubMed] [Google Scholar]
- 20.Saito S, Ishii T, Kamogawa Y, Watanabe R, Shirai T, Fujita Y, Shirota Y, Fujii H, Ito K, Shimokawa H, Yamaguchi T, Kawaguchi Y, Harigae H. Extracorporeal shock wave therapy for digital ulcers of systemic sclerosis: a phase 2 pilot study. Tohoku J Exp Med. 2016;238:39–47. doi: 10.1620/tjem.238.39. [DOI] [PubMed] [Google Scholar]
- 21.Arno A, Garcia O, Hernan I, Sancho J, Acosta A, Barret JP. Extracorporeal shock waves, a new non-surgical method to treat severe burns. Burns. 2010;36:844–849. doi: 10.1016/j.burns.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 22.Joo SY, Cho YS, Seo CH. The clinical utility of extracorporeal shock wave therapy for burn pruritus: a prospective, randomized, single-blind study. Burns. 2018;44:612–619. doi: 10.1016/j.burns.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Larking AM, Duport S, Clinton M, Hardy M, Andrews K. Randomized control of extracorporeal shock wave therapy versus placebo for chronic decubitus ulceration. Clin Rehabil. 2010;24:222–229. doi: 10.1177/0269215509346083. [DOI] [PubMed] [Google Scholar]
- 24.Porso M, Loreti S, Nusca SM, Luziatelli S, Caccia D, Taborri G, Trischitta D, Taurino M, Padua L, Saraceni VM, Vulpiani MC, Vetrano M. Defocused shock wave therapy for chronic soft tissue wounds in the lower limbs: a pilot study. Ultrasound Med Biol. 2017;43:362–369. doi: 10.1016/j.ultrasmedbio.2016.08.038. [DOI] [PubMed] [Google Scholar]
- 25.Fu M, Cheng H, Li D, Yu X, Ji N, Luo F. Radial shock wave therapy in the treatment of chronic constriction injury model in rats: a preliminary study. Chin Med J (Engl) 2014;127:830–834. [PubMed] [Google Scholar]
- 26.Mangone G, Veliaj A, Postiglione M, Viliani T, Pasquetti P. Radial extracorporeal shock-wave therapy in rotator cuff calcific tendinosis. Clin Cases Miner Bone Metab. 2010;7:91–96. [PMC free article] [PubMed] [Google Scholar]
- 27.Chou CL, Lee WR, Yeh CC, Shih CC, Chen TL, Liao CC. Adverse outcomes after major surgery in patients with pressure ulcer: a nationwide population-based retrospective cohort study. PLoS One. 2015;10:e0127731. doi: 10.1371/journal.pone.0127731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang KV, Chen SY, Chen WS, Tu YK, Chien KL. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2012;93:1259–1268. doi: 10.1016/j.apmr.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 29.Lee SJ, Kang JH, Kim JY, Kim JH, Yoon SR, Jung KI. Dose-related effect of extracorporeal shock wave therapy for plantar fasciitis. Ann Rehabil Med. 2013;37:379–388. doi: 10.5535/arm.2013.37.3.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malliaropoulos N, Jury R, Pyne D, Padhiar N, Turner J, Korakakis V, Meke M, Lohrer H. Radial extracorporeal shockwave therapy for the treatment of finger tenosynovitis (trigger digit) Open Access J Sports Med. 2016;7:143–151. doi: 10.2147/OAJSM.S108126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang CJ, Huang HY, Pai CH. Shock wave-enhanced neovascularization at the tendon-bone junction: an experiment in dogs. J Foot Ankle Surg. 2002;41:16–22. doi: 10.1016/s1067-2516(02)80005-9. [DOI] [PubMed] [Google Scholar]
- 32.Wang FS, Wang CJ, Chen YJ, Chang PR, Huang YT, Sun YC, Huang HC, Yang YJ, Yang KD. Ras induction of superoxide activates erk-dependent angiogenic transcription factor hif-1alpha and vegf-a expression in shock wave-stimulated osteoblasts. J Biol Chem. 2004;279:10331–10337. doi: 10.1074/jbc.M308013200. [DOI] [PubMed] [Google Scholar]
- 33.Yang G, Luo C, Yan X, Cheng L, Chai Y. Extracorporeal shock wave treatment improves incisional wound healing in diabetic rats. Tohoku J Exp Med. 2011;225:285–292. doi: 10.1620/tjem.225.285. [DOI] [PubMed] [Google Scholar]
- 34.Omar MT, Alghadir A, Al-Wahhabi KK, Al-Askar AB. Efficacy of shock wave therapy on chronic diabetic foot ulcer: a single-blinded randomized controlled clinical trial. Diabetes Res Clin Pract. 2014;106:548–554. doi: 10.1016/j.diabres.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 35.Aicher A, Heeschen C, Sasaki K, Urbich C, Zeiher AM, Dimmeler S. Low-energy shock wave for enhancing recruitment of endothelial progenitor cells: a new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation. 2006;114:2823–2830. doi: 10.1161/CIRCULATIONAHA.106.628623. [DOI] [PubMed] [Google Scholar]
- 36.Gerdesmeyer L, von Eiff C, Horn C, Henne M, Roessner M, Diehl P, Gollwitzer H. Antibacterial effects of extracorporeal shock waves. Ultrasound Med Biol. 2005;31:115–119. doi: 10.1016/j.ultrasmedbio.2004.08.022. [DOI] [PubMed] [Google Scholar]