Abstract
Background
Adductor tenotomy is needed for clinically complex hips with soft-tissue contractures. It may be proposed that the patients who need adductor tenotomy during closed reduction would have poorer prognosis than the ones without need for adductor tenotomy. The main purposes were to compare the normalization of acetabular index angle (AI), to determine the incidence of femoral head avascular necrosis (AVN), and to predict the need for any secondary surgical intervention between the patients who need adductor tenotomy and those who do not during closed reduction for developmental dysplasia of the hip.
Materials and Methods
The study group consisted of 65 hips treated between 6 and 12 months of age. The mean age at the time of surgery was 8.1 ± 1.4 (6–12) months and the mean follow-up was 4.2 ± 1.5 years. Improvement of AI, rate and severity of AVN, and need for secondary surgery with its predictors were evaluated.
Results
Adductor tenotomy was performed in 22 hips (Group 1), but not in 43 hips (Group 2). Normalization of the AI was − 14.8° ± 3.5° versus − 14.3° ± 3.2°. The overall incidence of AVN was 18.4%. The rate of secondary surgical intervention was higher in Group 1 (63.1% versus 36.9%) (p = 0.014).
Conclusions
No significant difference was detected regarding the improvement of AI as well as the incidence of AVN between the groups. The need for adductor tenotomy during closed reduction was one of the main predictors of the possible secondary surgery.
Keywords: DDH, Adductor tenotomy, Avascular necrosis, Acetabular index, Closed reduction, Secondary surgery, Redislocation, Soft-tissue contracture, Open reduction, Developmental dysplasia of the hip
Introduction
Developmental dysplasia of the hip (DDH) is one of the most important pediatric orthopedic disorders characterized by abnormal relationship of the femoral head with the acetabulum, including isolated acetabular dysplasia, subluxation, and complete dislocation of the hip joint [1]. The incidence of this disorder has been reported as 3–4 per 1000 live births [1, 2]. When left untreated, pathological changes in the hip joint especially during the early years of life may have devastating effects on the child’s future joint function as well as daily living activities. In the clinical management of DDH, the ultimate goal is to obtain a stable concentrically reduced hip joint as early as possible.
Closed reduction with application of a spica cast remains the preferred treatment for children treated with splintage that has failed to provide a satisfactory concentric reduction [2, 3]. Treatment guidelines do not present a strict age-based cut-off for surgical procedures; however, they represent the increasing surgical complexity typically required with advanced age at presentation of the patients with DDH [4]. Contractures of the joint capsule and the ligaments around the joint preventing gentle reduction of the hip may explain the mechanism behind this situation [5]. Soft-tissue contractures that interfere with obtaining or maintaining ideal reduction must be eliminated to minimize the compressive or deforming forces on the vulnerable blood supply and cartilaginous structures [3, 6]. This may not only decrease the incidence and severity of growth disturbances of the proximal femoral epiphysis related to closed reduction, but also may decrease the need for open reduction. On the other hand, no consensus has been established on the need as well as the success of adductor tenotomy application during closed reduction as the primary treatment of DDH.
The main purposes were to compare the normalization of acetabular index angle (AI) (1), to determine the incidence of femoral head avascular necrosis (AVN) (2), and to predict the need for any secondary surgical intervention (3) between the patients who need adductor tenotomy and those do not during closed reduction for developmental dysplasia of the hip (DDH).
Materials and Methods
Clinical data of the patients treated for DDH between January 2005 and December 2012 were retrospectively evaluated after having approval from the Institutional Review Board (IRB). The patients who were diagnosed with either subluxated or dislocated hip joint according to the International Hip Dysplasia Institute (IHDI) classification system (grades 3–4), treated with closed reduction, and aged between 6 and 12 months during the treatment were identified. The ones with insufficient clinical data, who were lost to follow-up, with established diagnosis of neuromuscular disease, treated with methods other than closed reduction and tenotomy to achieve reduction were excluded from the study. Besides, the patients with a minimum follow-up of less than 3 years were excluded. Fifty-three patients (65 hips) who were treated with closed reduction for idiopathic primary DDH between the ages of 6–12 months were evaluated in the study.
Surgical Technique
All procedures were carried out by the same surgical team (TY, AIB). Traction was not applied in any of the patients before closed reduction. All reductions were achieved by gentle manipulation under general anesthesia, applying traction with the hip and knee flexed, while the greater trochanter was pushed anteriorly [2]. Reduction was performed without any extra force to avoid the increased risk of avascular necrosis due to forced reduction. In case the soft-tissue contracture limited the amount of abduction available to achieve a stable reduction, an adductor tenotomy was performed to help release the contracture as well as to increase the safe zone of abduction [7]. The hip range of motions of the patients was examined before and after tenotomy. If the arc of abduction/adduction between redislocation and comfortable, gravity assisted, abduction was < 30° and/or abduction in 90° flexion was < 45°, and an adductor longus release was performed [3]. We observed a remarkable increase after adductor tenotomy in terms of safe zone and maximum abduction. For pelvipedal spica casting, 90° of hip flexion and abduction not more than 45–50° at final hip position was routinely applied. Minimum 30° safe zone was aimed [6]. Clinically open reduction was indicated when a congruent, stable hip joint could not be obtained via closed reduction under general anesthesia or when extreme abduction was required to maintain reduction despite adductor tenotomy.
Additionally, we performed arthrography to all hips. Medial dye pool greater than 6 mm on arthrography was accepted as the main indication for open reduction. Intra-operatively, routine fluoroscopic control was performed after pelvipedal casting to check concentric reduction. Reduction was also routinely assessed by post-operative antero-posterior (AP) pelvic X-ray. If the post-operative control X-ray quality was not sufficient to interpret femoral head position, reduction was checked with pelvic MRI.
Routine post-reduction cast immobilization period was 3 months for all cases. Clinical follow-up visits were conducted at 6 weeks, 3 monthly intervals for the first year, 6 monthly intervals for the next 2 years, and annually thereafter. Following 3 months of cast immobilization, hip abduction orthosis was routinely ordered for an additional 3 months. Abduction orthosis was ordered to be used in a full-time manner, which was 22–23 h a day during the first month and 10–12 h a day for the last 2 months.
The patients were reviewed for clinical and radiologic outcomes first year control after closed reduction and fourth year control. Clinically patients’ hip range of motion (ROM) and Trendelenburg sign were evaluated. Radiological concentric reduction was evaluated on AP pelvic X-ray, AI was measured, and radiographic sings of AVN were investigated to determine the grade of AVN. Radiological results were assessed by authors (YC and MM) who were blinded to treatment group.
Radiographic Evaluation
Initial and post-reduction follow-up AI were measured on AP pelvis X-rays of all patients but not used as an inclusion or exclusion criteria. The AI normalization rate was calculated by dividing the preoperative AI angle by the degree of decrease in the AI angle determined at the last control compared to the preoperative value. Pre-operatively, dysplasia of the hip was categorized according to International Hip Dysplasia Institute (IHDI) classification system [8]. The incidence and grade of AVN were evaluated according to the X-rays obtained at the first year and latest follow-up visits. Avascular necrosis was diagnosed and graded according to Kalamachi and MacEwen [9].
Need for Secondary Surgical Intervention
In routine clinical practice, as the child grows, four radiographic markers are commonly used to ensure that a reduction was successful: improvement in the acetabular index, a sharp (not rounded) lateral border of the acetabulum, a narrow teardrop, and an intact Shenton line (Fig. 1). After closed reduction; when subluxation or dislocation of the hip was diagnosed with or without acetabular dysplasia in any of the follow-up visits, the patient was planned for secondary open surgical intervention. The indication for periacetabular osteotomy was AI measured higher than 30°in a patient older than 18 months of age. As in the case of closed reduction indication, all of the indications for secondary surgery were given by two senior surgeons (TY and AIB) who were specifically dealing with pediatric orthopedic cases.
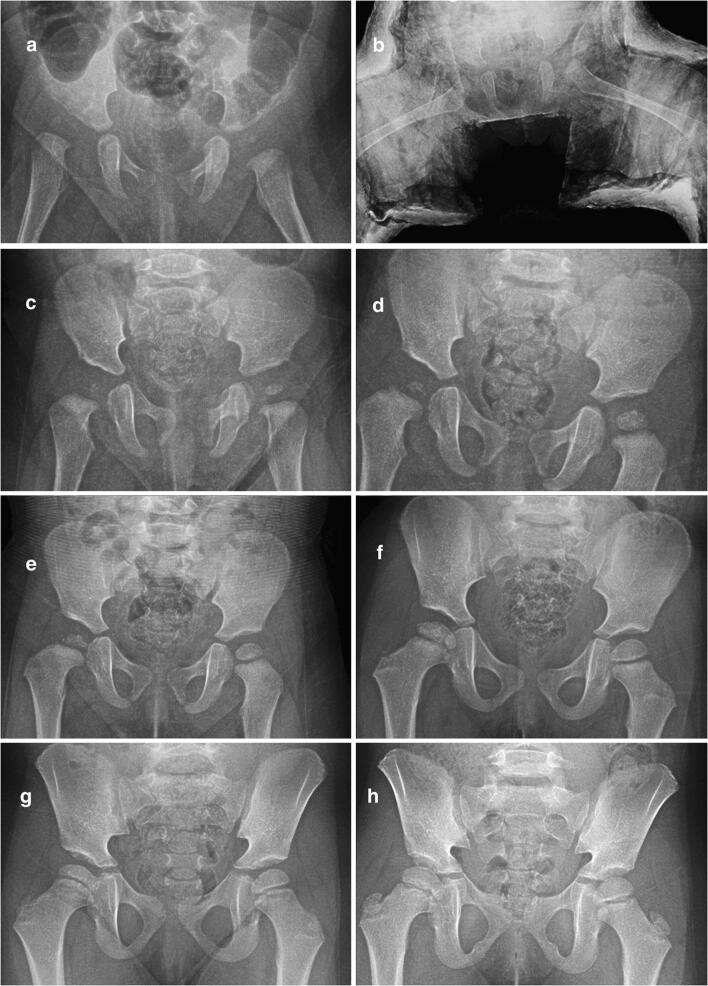
Fig. 1.
Follow-up radiographs of a patient with bilateral dysplastic hip treated with closed reduction and spica casting. a Preoperative AP radiography of a patient who was 6.5 months old. b Bilateral dysplastic hip was treated with closed reduction without tenotomy. c–h Follow-up radiographs of patient during 5 years
Statistical Analysis
All data were analyzed using the software SPSS 19.0 for Windows (SPSS Inc., Chicago, Illinois, USA) at a significance level of 0.05. Categorical variables were expressed as proportions (%). For categorical variables, differences between the groups were assessed using the Pearson Chi-squared test or two-tailed Fisher’s exact test. For comparison of continuous variables, Mann–Whitney U test was used. Multiple linear regression was used to analyze the association between the need for secondary surgical intervention and a set of factors including age, gender, initial AI, IHDI grade before closed reduction, harness usage, involved side (unilateral or bilateral), adductor tenotomy (performed during closed reduction or not), casting duration, and AVN of the femoral head detected during follow-up visits. For the patients who had bilateral involvement, each hip was considered separately, as an independent occurrence, for the purpose of statistical analysis. The power of our study was calculated by post hoc analysis.
Results
Table 1 summarizes demographic data and clinical features of the patients. An adductor tenotomy was performed during closed reduction in 22 hips (33.8%) (Group 1), whereas adductor tenotomy was not performed in 43 hips (66.2%) (Group 2). There was no statistically significant difference in the mean age at the time of closed reduction, mean follow-up time, initial AI, and final follow-up AI between the patient groups. The mean AI normalization was − 14.8 ± 3.5 in Group 1 and − 14.3 ± 3.2 in Group 2 (Table 2). Additionally, AI improvement ratio was 0.39 ± 0.11 in Group 1 and − 0.4 ± 0.12 in Group 2 (p = 0.8).
Table 1.
Demographic data of the study population
| Variable | Group 1 (22 hips) | Group 2 (43 hips) |
|---|---|---|
| Age at the time of closed reduction (months) (mean ± SD) | 8.4 ± 1.8 | 8.1 ± 1.2 |
| Age at the latest follow-up (years) (mean ± SD) | 5.2 ± 1.5 | 4.7 ± 1.4 |
| Follow-up time (years) (mean ± SD) | 4.6 ± 1.5 | 4 ± 1.6 |
| Gender (female/male) (n) | 19/3 | 42/1 |
| Previous harness or brace treatment (+/−) (n) | 17/5 | 34/9 |
| IHDI grade at time of reduction | ||
| Grade 3 (n) | 12 | 26 |
| Grade 4 (n) | 10 | 17 |
SD standard deviation, Group 1 adductor tenotomy was performed during closed reduction, Group 2 adductor tenotomy was not performed during closed reduction, n number, IHDI International Hip Dysplasia Institute
Table 2.
Progression of acetabular index angle, incidence and severity of avascular necrosis, and need for secondary surgical intervention
| Variable | Group 1 (22 hips) | Group 2 (43 hips) | p value |
|---|---|---|---|
| Acetabular index (°) | |||
| Pre-reduction (mean ± SD) | 36.6 ± 3.6 | 35.9 ± 2.9 | 0.42 |
| First year follow-up (mean ± SD)a | 26.8 ± 3.1 | 25.5 ± 2.7 | 0.33 |
| Final follow-up (mean ± SD)a | 20.6 ± 3.1 | 21.3 ± 2.5 | 0.22 |
| AI improvement (mean ± SD) | − 14.8 ± 3.5 | − 14.3 ± 3.2 | 0.35 |
| Findings of avascular necrosis after closed reductionb | |||
| No findings of AVN | 17(86.4%) | 36(83.8%) | |
| Total number of the hips with AVN | 5(13.6%) | 7(16.2%) | 0.53 |
| Grade 1 | |||
| Changes affecting the ossific nucleus | 5 | 5 | |
| Grade 2 | |||
| Lateral physeal damage | 0 | 0 | |
| Grade 3 | |||
| Central physeal damage | 0 | 2 | |
| Grade 4 | |||
| Total damage to the head and the physis | 0 | 0 | |
| Secondary surgical interventions during follow-up | |||
| Total secondary intervention (n/%) | 13 (59.1%) | 11 (25.5%) | 0.014 |
| Type of secondary surgery and number of operated patients | |||
| Need closed re-reduction during follow-up | 1 | 3 | |
| Pelvic osteotomy | 5 | 1 | |
| Open reduction | 2 | 2 | |
| Open reduction + pelvic osteotomy | 5 | 4 | |
| Open reduction + pelvic + femoral osteotomy | 0 | 1 | |
statistically significant p values are in bold
SD standard deviation, AI acetabular index, AVN avascular necrosis, SD standard deviation, n number
aThe patients who underwent secondary surgery were excluded
bKalamchi and MacEwen classification
The overall incidence of AVN in 65 hips was 18.4% (n = 12). Ten of them were classified as grade 1 (5 patients in Group 1; 5 patients in Group 2), whereas the other three were Grade 3. All of the hips with Grade-3 (n = 2) AVN were from Group 2 (Table 2).
The ratio of the hips that underwent secondary surgical intervention during follow-up after closed reduction, including the ones required secondary closed reduction, was noted as 36.9% (n = 24) in our study population. The need for secondary surgery was higher in Group 1 than in Group 2 (p = 0.014). Univariate analysis demonstrated that the need for adductor tenotomy during closed reduction, initial IHDI grade, AI before closed reduction, and AVN after closed reduction significantly associated with the need for a secondary surgical intervention (Tables 3, 4). These independent variables were included in multivariate regression analysis. According to multivariate regression analysis; need for adductor tenotomy during closed reduction and AI before closed reduction were identified as the major predictors of the need for secondary surgical intervention in patients treated with closed reduction between 6 and 12 months of age (Table 5).
Table 3.
Detailed chart of patients who needed secondary surgery after closed reduction
| Case no. | Tenotomy (+/−) | IHDI grade | Preoperative AI | AVN grade | Type of secondary surgery |
|---|---|---|---|---|---|
| 1 | + | 2 | 41 | 0 | Dega osteotomy |
| 2 | + | 3 | 34 | 0 | Open reduction |
| 3 | + | 3 | 34 | 0 | Open reduction + Dega osteotomy |
| 4 | + | 2 | 39 | 0 | Salter osteotomy |
| 5 | + | 4 | 38 | 0 | Closed re-reduction |
| 6 | + | 2 | 36 | 0 | Dega osteotomy |
| 7 | + | 2 | 36 | 0 | Dega osteotomy |
| 8 | + | 2 | 43 | 1 | Dega osteotomy |
| 9 | + | 3 | 43 | 1 | Open reduction + Dega osteotomy |
| 10 | + | 4 | 41 | 0 | Open reduction + Dega osteotomy |
| 11 | + | 2 | 41 | 0 | Salter osteotomy |
| 12 | + | 4 | 35 | 0 | Open reduction + Dega osteotomy |
| 13 | + | 3 | 33 | 1 | Open reduction |
| 14 | – | 4 | 34 | 0 | Closed re-reduction |
| 15 | – | 3 | 31 | 0 | Open reduction + Salter osteotomy |
| 16 | – | 3 | 38 | 3 | Open reduction + Dega osteotomy |
| 17 | – | 3 | 39 | 3 | Open reduction + Dega osteotomy |
| 18 | – | 3 | 32 | 1 | Closed re-reduction |
| 19 | – | 4 | 30 | 0 | Open reduction |
| 20 | – | 4 | 32 | 1 | Closed re-reduction |
| 21 | – | 4 | 30 | 0 | Open reduction |
| 22 | – | 2 | 34 | 0 | Dega osteotomy |
| 23 | – | 4 | 41 | 0 | Open reduction + Dega&femoral osteotomy |
| 24 | – | 3 | 38 | 0 | Open reduction + Dega osteotomy |
Tenotomy (+) represents patients needed adductor tenotomy during the closed reduction and casting
These values measured just before the second surgery
AVN grade represent the evaluation of hip at the last control. Patients who undergone closed re-reduction surgery did not need tenotomy. Additionally, they were not go any further surgery such as open reduction or any bony procedure
IHDI International Hip Dysplasia Institute, AI Acetabular Index
Table 4.
Independent variables related to the need for secondary surgical intervention according to univariate analysis
| Variables | Secondary surgery (+) | Secondary surgery (−) | p value |
|---|---|---|---|
| Age at the time of closed reduction (months) (mean ± SD) | 8.4 ± 1.6 | 7.9 ± 1.4 | 0.32 |
| Previous harness or brace treatment (+/−) (n)a | 16/16 | 33/8 | 0.61 |
| Adductor tenotomy (+/−) (n) | 13/11 | 9/32 | 0.01 |
| Casting duration (weeks) (mean ± SD) | 11.3 ± 3.4 | 10.6 ± 2.7 | 0.36 |
| IHDI Grade 3/4 (n)a | 11/13 | 27/14 | 0.03 |
| First admission AI (°) (mean ± SD)a | 37.3 ± 3.5 | 35.4 ± 2.7 | 0.03 |
| Avascular necrosis during follow-up (+/−) (n) | 8/16 | 4/37 | 0.01 |
statistically significant p values are in bold
SD standard deviation, IHDI International Hip Dysplasia Institute
aValues just before the closed reduction, not before the secondary surgery
Table 5.
Main predictors of secondary surgical intervention according to multivariate analysis
| p value* | OR (Exp(B)) | 95% CI for EXP(B) | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Adductor tenotomy | < 0.01 | 6.2 | 1.8 | 21.5 |
| Pre-reduction IHDI | 0.49 | 1.5 | 0.4 | 4.9 |
| Pre-reduction acetabular index angle | 0.02 | 1.3 | 1.1 | 1.5 |
| Avascular necrosis during follow-up | 0.36 | 2.1 | 0.4 | 9.6 |
statistically significant p values are in bold
OR odds ratio
*In a multivariate logistic regression with variables that may affect secondary surgical ratio. Secondary surgical need was found to be related to the adductor tenotomy need during the closed reduction and AI. The confidence interval is rather wide, because the numbers of confounding variables is small
Discussion
Although skin traction for a while before closed reduction of the affected hip joint performed or soft-tissue releases such as tenotomy of the psoas and adductor tendons during reduction under general anesthesia have been identified and discussed in the literature, no consensus has been established on the most appropriate and effective technique to overcome the soft-tissue barriers to obtain a safe concentric reduction when treating a patient with DDH [3]. Previous studies reported variable mid- and long-term outcomes following closed reduction with significant variations in technique [2, 10–13]. When soft-tissue contracture limits the amount of abduction available to achieve a stable reduction and sufficient safe zone, adductor tenotomy may provide a minimally invasive and effective option [6]. Generally, adductor tenotomy is needed in hips with soft-tissue contractures independently from the previous treatment approach performed before closed reduction. It may be proposed that patients who need adductor tenotomy during closed reduction would have poorer prognosis than the ones without need for adductor tenotomy. Therefore, the main questions of the present study were whether differences in clinical and radiographic prognosis may occur between the adductor tenotomy group and non-adductor tenotomy group in the means of AI improvement, AVN rates, and need for any secondary surgical intervention.
Residual acetabular dysplasia following the conservative or operative treatment of DDH has still been a major problem in the clinical practice of pediatric orthopedics. It has been reported in more than one-third of treated DDH patients [14–16]. Studies investigating the potential of the acetabulum to develop after closed reduction reported that various factors including age, preoperative brace usage, traction, initial AI, bilaterality, center-head distance discrepancy (CHDD), failure to concentric reduction, and avascular necrosis (AVN) of the femoral head may influence the remodeling of the hip [17]. The younger age and concentric reduction were generally mentioned as positive predictors of a good AI improvement in the literature [18, 19]. However, initial AI, gender, initial CHDD, bilaterality, and AVN were not [17, 19]. Tennant et al. [3] and Murray et al. [2] reported that tenotomy did not have a positive effect or negative effect on the development of acetabular index. According to the data, we acquired during the study, and no statistically significant differences were detected regarding the mean AI between the hips treated with or without adductor tenotomy neither before closed reduction nor at the latest follow-up. Besides, the improvement ratio of the AI from initial measurement until the latest follow-up was similar in both groups. Our findings were consistent with the previous studies mentioned above.
The incidence as well as the grade of AVN following the treatment of DDH remains the most important variable directly affecting the outcomes independently from the method of clinical management [20]. The potential role of various risk factors including radiographic appearance of ossific nucleus of the femoral head, abduction angle in the spica cast, gender, bilateral involvement, familial history, previous treatment modalities using Pavlik harness or abduction orthosis, and adductor tenotomy during closed reduction have been evaluated in literature [19–21]. According to the literature, incidence of AVN after closed reduction has been reported between 10 and 35% [2, 3, 6, 11, 19, 21]. In these studies, the effects of AVN-related variables were not parallel, and the ratios were different. Cooper et al. mentioned that this disparity was largely caused by differences in the definitions of AVN and the timing of follow-up [22]. In recent studies evaluating the AVN incidence with similar patient demographics and similar methodology of treatment to our study, authors did not observe any significant relationship between the need for adductor tenotomy during closed reduction and signs of AVN during follow-up. Furthermore, no additional protective effect of tenotomy against AVN was estimated [6, 11, 20]. Our results regarding the correlation of adductor tenotomy and the findings of AVN during follow-up were consistent with these studies. On the other hand, despite that no difference was detected regarding the incidence of AVN between the two groups in the current study, radiographic grade of the AVN was significantly higher in cases from Group 2.
One of the main focuses of the present study was the need for secondary surgical intervention after closed reduction with or without adductor tenotomy. The frequency of secondary surgical treatment was reported ranging between 12 and 66% in the literature [2, 3, 10, 11, 13, 14, 21, 23, 24]. The overall ratio of the hips that underwent secondary surgical procedures was 33.8% in our study population, which was consistent with the literature. On the other hand, it was significantly higher in the hips that needed adductor tenotomy during closed reduction (59.1% versus 25.5%). Age, gender, initial AI, initial reduction quality, grade of subluxation, application of harness before closed reduction, duration of casting, and AVN of the femoral head were the independent variables demonstrated to be related to the need for secondary surgery in the literature [6, 14, 15, 17–19, 24, 25]. According to our data, need for adductor tenotomy during closed reduction and pre-reduction AI was determined as the major predictors of secondary surgical intervention in patients treated for DDH between the ages 6 and 12 months. Adversely from our findings, Murray et al. [2] noted that adductor tenotomy performed during closed reduction had no correlation with the need for further interventions. However, heterogeneous age distribution (range 3–16 months) as well as routine traction protocol in their study may explain different outcomes. We did not determine and discuss the cut-off value of AI to predict secondary surgery need, as it was not in the scope of this work [26].
The major limitation of the present study was the retrospective evaluation of prospectively followed patient groups. Second, the study population was not a large series with relatively short-term follow-up. The statistical power of the study was 0.69 according to post hoc analysis. Although the statistical power was under 0.80, comparative analyses of the clinical and radiographic outcomes in a specific age group with a rare but serious orthopedic disorder were the strength of the study. Besides, we performed univariate and multivariate analyses of many different parameters to achieve a better understanding the value of adductor tenotomy to predict need of secondary surgical intervention.
Conclusion
No significant difference was detected regarding the improvement of AI as well as the incidence of AVN between the hips that needed adductor tenotomy during closed reduction and the ones that did not. On the other hand, significantly higher need for secondary surgical intervention was noted in adductor tenotomy group. This study may be a reference for further clinical investigations.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. This was a retrospective study of patient data, and IRB approval was obtained.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest regarding the submission and publication of this manuscript.
Ethical review committee statement
This study has been approved by the ethical review committee of Erzincan University.
Informed consent
For this type of study, informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hanifi Ucpunar, Email: hanifiucpunar@yahoo.com.
Muhammed Mert, Email: mmrt@hotmail.com.
Yalkin Camurcu, Email: yalkin.camurcu@gmail.com.
Hakan Sofu, Email: hakansofu@yahoo.com.
Timur Yildirim, Email: drtimur@hotmail.com.
Avni Ilhan Bayhan, Email: ilhanbayhan@hotmail.com.
References
- 1.Dezateux C, Rosendahl K. Developmental dysplasia of the hip. The Lancet. 2007;369(9572):1541–1552. doi: 10.1016/S0140-6736(07)60710-7. [DOI] [PubMed] [Google Scholar]
- 2.Murray T, Cooperman DR, Thompson GH, Ballock RT. Closed reduction for treatment of developmental dysplasia of the hip in children. American Journal of Orthopedics (Belle Mead, N.J.) 2007;36(2):82–84. [PubMed] [Google Scholar]
- 3.Tennant SJ, Eastwood DM, Calder P, Hashemi-Nejad A, Catterall A. A protocol for the use of closed reduction in children with developmental dysplasia of the hip incorporating open psoas and adductor releases and a short-leg cast: Mid-term outcomes in 113 hips. The Bone & Joint Journal. 2016;98B(11):1548–1553. doi: 10.1302/0301-620X.98B11.36606. [DOI] [PubMed] [Google Scholar]
- 4.Murphy RF, Kim YJ. Surgical management of pediatric developmental dysplasia of the hip. Journal of American Academy of Orthopaedic Surgeons. 2016;24(9):615–624. doi: 10.5435/JAAOS-D-15-00154. [DOI] [PubMed] [Google Scholar]
- 5.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. Journal of American Academy of Orthopaedic Surgeons. 2001;9(6):401–411. doi: 10.5435/00124635-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Barakat AS, Zein AB, Arafa AS, Azab MA, Reda W, Hegazy MM, Al Barbary HM, Kaddah MA. Closed reduction with or without adductor tenotomy for developmental dysplasia of the hip presenting at walking age. Current Orthopaedic Practice. 2017;28(2):195–199. doi: 10.1097/BCO.0000000000000478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy RF, Kim YJ. Surgical management of pediatric developmental dysplasia of the hip. Journal of the American Academy of Orthopaedic Surgeons. 2016;24(9):615–624. doi: 10.5435/JAAOS-D-15-00154. [DOI] [PubMed] [Google Scholar]
- 8.Narayanan U, Mulpuri K, Sankar WN, Clarke NM, Hosalkar H, Price CT. International Hip Dysplasia Institute. Reliability of a new radiographic classification for developmental dysplasia of the hip. Journal of Pediatric Orthopaedics. 2015;35(5):478–484. doi: 10.1097/BPO.0000000000000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. Journal of Bone and Joint Surgery. American Volume. 1980;62(6):876–888. doi: 10.2106/00004623-198062060-00002. [DOI] [PubMed] [Google Scholar]
- 10.Shin CH, Yoo WJ, Park MS, Kim JH, Choi IH, Cho TJ. Acetabular remodeling and role of osteotomy after closed reduction of developmental dysplasia of the hip. The Bone & Joint Journal. 2016;98(11):952–957. doi: 10.2106/JBJS.15.00992. [DOI] [PubMed] [Google Scholar]
- 11.Schur MD, Lee C, Arkader A, Catalano A, Choi PD. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. Journal of Children’s Orthopaedics. 2016;10(3):185–192. doi: 10.1007/s11832-016-0743-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiderius C, Jaramillo D, Connolly S, Griffey M, Rodriguez DP, Kasser JR, Millis MB, Zurakowski D, Kim YJ. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: A preliminary report. Journal of Pediatric Orthopedics. 2009;29(1):14–20. doi: 10.1097/BPO.0b013e3181926c40. [DOI] [PubMed] [Google Scholar]
- 13.Rampal V, Sabourin M, Erdeneshoo E, Koureas G, Seringe R, Wicart P. Closed reduction with traction for developmental dysplasia of the hip in children aged between one and five years. The Journal of Bone and Joint Surgery. 2008;90(7):858–863. doi: 10.1302/0301-620X.90B7.20041. [DOI] [PubMed] [Google Scholar]
- 14.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip Implications for secondary procedures. The Journal of Bone and Joint Surgery. 2004;86(6):876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 15.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. Journal of Bone and Joint Surgery. 1995;77(7):985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Terjesen T, Halvorsen V. Long-term results after closed reduction of late detected hip dislocation: 60 patients followed up to skeletal maturity. Acta Orthopaedica. 2007;78(2):236–246. doi: 10.1080/17453670710013744. [DOI] [PubMed] [Google Scholar]
- 17.Kitoh H, Kitakoji T, Katoh M, Ishiguro N. Prediction of acetabular development after closed reduction by overhead traction in developmental dysplasia of the hip. The Journal of Orthopaedic Science. 2006;11(5):473–477. doi: 10.1007/s00776-006-1049-2. [DOI] [PubMed] [Google Scholar]
- 18.Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. Journal of Pediatric Orthopedics. 1994;14(1):3–8. doi: 10.1097/01241398-199401000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Brougham DI, Broughton NS, Cole WG, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip. The Journal of Bone and Joint Surgery. 1988;70(5):733–736. doi: 10.1302/0301-620X.70B5.3192570. [DOI] [PubMed] [Google Scholar]
- 20.Gornitzky AL, Georgiadis AG, Seeley MA, Horn BD, Sankar WN. Does perfusion MRI after closed reduction of developmental dysplasia of the hip reduce the incidence of avascular necrosis? Clinical Orthopaedics and Related Research. 2016;474(5):1153–1165. doi: 10.1007/s11999-015-4387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roposch A, Stöhr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip. A meta-analysis. Journal of Bone and Joint Surgery. 2009;91(4):911–918. doi: 10.2106/JBJS.H.00096. [DOI] [PubMed] [Google Scholar]
- 22.Brougham DI, Broughton NS, Cole WG, Menelaus MB. Avascular necrosis following closed reduction of congenital dislocation of the hip. Review of influencing factors and long-term follow-up. The Journal of Bone and Joint Surgery. 1990;72(4):557–562. doi: 10.1302/0301-620X.72B4.2380203. [DOI] [PubMed] [Google Scholar]
- 23.Kim HT, Kim JI, Yoo CI. Acetabular development after closed reduction of developmental dislocation of the hip. Journal of Pediatric Orthopedics. 2000;20(6):701–708. doi: 10.1097/01241398-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Ge Y, Cai H, Wang Z. Quality of reduction and prognosis of developmental dysplasia of the hip: A retrospective study. HIP International. 2016;26(4):355–359. doi: 10.5301/hipint.5000348. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Xu H, Li J, Yu L, Liu Y, Southern E, Liu H. Early predictors of acetabular growth after closed reduction in late detected developmental dysplasia of the hip. Journal of Pediatric Orthopedics. Part B. 2015;24(1):35–39. doi: 10.1097/BPB.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 26.Li Y, Guo Y, Li M, Zhou Q, Liu Y, Chen W, Li J, Canavese F, Xu H. Multi-center Pediatric Orthopedic Study Group of China. Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. International Orthopaedics. 2018;42(3):631–640. doi: 10.1007/s00264-017-3726-5. [DOI] [PubMed] [Google Scholar]