Abstract
AIM
To review international guidelines and to share our infection control experience during the coronavirus disease 2019 (COVID-19) pandemic at a tertiary eye centre in Hong Kong.
METHODS
Infection control guidelines and recommendations from international ophthalmological bodies are reviewed and discussed. The measures at our hospital were drawn up as per international and local health authorities' guidelines and implemented with the collaboration of doctors, nurses and administrative staff.
RESULTS
The aims of our infection control measures are to 1) minimize cross-infection within the hospital; 2) protect and support hospital staff; 3) ensure environmental control. To minimize the risk of cross-infection, outpatient attendance and elective surgery have been reduced by 40%, and general anesthesia procedures were reduced by 90%. Patients entering the hospital are screened for fever, travel history, contact and cluster history, and COVID-19 related symptoms. To protect and support hospital staff, we ensure provision of adequate personal protective equipment (PPE) and provide clear guidelines on the level of PPE needed, depending on the clinical situation. Other protective measures include provision of work uniforms, easy access to alcohol-based hand rub, opening new lunch areas, implementation of self-monitoring and self-reporting systems, and communication via online education and updates. Finally, environmental control is achieved by ensuring regular disinfection of the hospital premise, enhancing ventilation, and usage of disposable ophthalmic instruments.
CONCLUSION
Our multi-pronged approach to infection control is, so far, successful in minimizing infection risks, while allowing the maintenance of essential ophthalmic services.
Keywords: COVID-19, coronavirus, SARS-CoV-2, ophthalmology, infection control, Hong Kong
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization (WHO) on 11 March 2020. The novel coronavirus (nCoV), now termed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has pushed the world into a state of emergency in weeks, resulting in more than two million cases worldwide[1]. Despite the comparisons that have been made to severe acute respiratory syndrome (SARS), COVID-19 has proven itself to be a uniquely formidable disease to contain and mitigate. With a variable incubation period (2-14d but can be up to 24d in rare cases)[2], multiple suspected routes of person-to-person transmission (droplet contact, oral-fecal route, or fomites)[3]–[5], an R0 of 2-2.5[6], and perhaps most challengingly, the presence of asymptomatic carriers, COVID-19 can only be combatted if both individual- and system-level vigilance are practiced. Healthcare workers are at high risk of contracting the virus, owing to increased exposure, reduced immunity due to long work hours and stress, a global shortage of personal protective equipment (PPE), and perhaps most importantly, an inadequate knowledge of infection prevention and control of this novel virus[7]. In particular, ophthalmologists are uniquely exposed to COVID-19.
Ophthalmology is a practice that relies heavily on physical examination. Pupil and extraocular examination, slit-lamp examination, applanation tonometry, and fundal examination all put us almost nose-to-nose with our patients. While the disease is still not fully understood, it is agreed on by international health bodies that SARS-CoV-2 is likely spread by droplet transmission[8]. One sneeze, cough, or simply conversing during an ophthalmological consultation could expose both the ophthalmologist and the patient to infection risk. In a large study involving 30 hospitals across China, researchers documented “conjunctival congestion” in 0.8% of 1099 laboratory-confirmed COVID-19 patients[2]. Reports of ophthalmologists acquiring COVID-19 at work prompted concerns that the disease could be spread by tears[9], prompting research into whether tear and conjunctival secretions could be a route of transmission. In one prospective study in China involving 30 patients with confirmed nCoV pneumonia, viral RNA was only isolated in the one patient who had conjunctivitis; the other 29 patients without ophthalmic symptoms did not have detectable RNA in their tear or conjunctival secretions[10]. In another study from Singapore, viral shedding in tears could not be detected in 17 patients, even in the one patient who developed conjunctivitis during hospital stay[11]. Nevertheless, while conjunctivitis is still an uncommon presentation of COVID-19, the death of Dr. Li Wenliang, the ophthalmologist who likely contracted the disease through droplet infection from an asymptomatic glaucoma patient[12], is sufficient to cause us to reflect on the infection control measures we should adopt in the ophthalmology setting during this pandemic.
Finally, as we are facing an aging population worldwide, and as ophthalmology is a specialty that caters to a large geriatric population, eye clinics are generally very crowded and busy. During a time when social distancing is pivotal in the control of viral spread, we must seek a balance between crowd control and delivering essential ophthalmic care to our patients.
As of April 19, 2020, there are 1024 confirmed cases in Hong Kong[13]. We believe that during a time of unprecedented uncertainty, setting up clear guidelines is necessary not only for the sake of minimizing infection risks, but also to alleviate anxiety and panic among staff. Here, we aim to review the current international guidelines and share our COVID-19 experience at Hong Kong Eye Hospital, the largest tertiary eye centre in the public health care system in Hong Kong. We are fortunate that as of the date of writing, we have not had a single case of patient or staff member infection acquired at Hong Kong Eye Hospital. This demonstrates that this model of care may be sustainable for a longer period of time, should the COVID-19 situation persist for months.
A REVIEW OF GUIDELINES IN THE INTERNATIONAL OPHTHALMOLOGY COMMUNITY
The International Council of Ophthalmology (ICO) launched their Global COVID-19 Resource Center on March 27, 2020, which has a compilation of COVID-19 related guidelines, resources and information provided by ICO Member societies[14].
We have also reviewed infection control guidelines from various health authorities and ophthalmological bodies around the world. Table 1 summarizes the key infection control measures in China, the United States, the United Kingdom, and Singapore[15]–[20].
Table 1. Key infection control measures of ophthalmological bodies in China, the United States, the United Kingdom, and Singapore.
| Country | Service adjustment | Patient triage | Crowd control | Personal protective equipment (PPE) | Equipment and environmental disinfection |
| China[15]–[16] | - Judicious adjustment of service volume - Postpone elective services and surgery - Avoid general anaesthesia |
- Set up triage units to identify patients with fever, symptoms of COVID-19 or positive travel history - Assess high risk patients in designated area |
- Reduce crowding in clinics to prevent cross-infection - Assign patients to different time slots for consultation |
- Wear surgical masks and practise hand hygiene - Ensure quality and supply of PPE |
- Ensure good ventilation - Disinfect consultation rooms and ophthalmic equipment - Use slit lamp breath shields and disposable tonometer tips |
| The United States[17] | - Postpone all elective visits and surgery - Assess infection risk of patients with urgent ophthalmic conditions and exercise corresponding level of precautions |
- Ask patients about fever and respiratory illness and whether they or a family member have travelled to a high-risk area in the past 14d prior to entering the clinic | - Decompress waiting areas and consider alternatives such as encouraging patients to wait in their cars or outdoor spaces | - Balance staff protection with PPE and conservation of scarce resources | - Disinfect consultation rooms and ophthalmic equipment with diluted household bleach or at least 70% alcohol after each patient encounter - Use slit lamp breath shields and disposable tonometer tips |
| The United Kingdom[18] | - Postpone all routine ophthalmic surgery and outpatient visits - Maintain emergency service for patients with sight-threatening conditions - Postpone routine diabetic retinopathy screening - Restrict general anaesthesia to cases where there is no other option |
- Contact patients via text messages prior to their appointment and advise them to seek medical advice if they are at risk or symptomatic - Identify and prevent high risk patients from entering the clinic by asking about symptoms of COVID-19, contact and travel history |
- Minimize onsite waiting time and patient journey time - Implement social distancing in waiting areas - Limit the number of accompanying adults |
- Follow PPE and staff protection requirements for ophthalmology - Choose PPE corresponding to risk level of clinical activity |
- Clean slit lamps before and after each patient, including the breath shields, switches and controls - Clean clinical areas and all equipment regularly |
| Singapore[19]–[20] | - Defer non-urgent appointments, elective surgeries and procedures - Maintain urgent eye care services |
- Perform temperature check and require patients to complete a declaration form on health status and travel history | - Allow only one accompanying person |
CURRENT INFECTION CONTROL STRATEGIES AT HONG KONG EYE HOSPITAL
In Hong Kong, the Hospital Authority (HA) announced the activation of Emergency Response Level in public hospitals in response to the COVID-19 situation on January 25, 2020[21]. Notably, all persons entering public hospitals and clinics are required to put on masks. Hospitals are also advised to review non-emergency services in order to focus resources on coping with COVID-19. Patients are urged to defer and reschedule routine follow-up appointments to reduce crowding at hospitals and out-patient clinics. In particular, ophthalmology clinics under HA have stepped up infection control measures, with special emphasis on crowd control, reduction of non-urgent services, and provision of adequate PPE to their staff[22].
While the infection control measures carried out at Hong Kong Eye Hospital share many similarities with those recommended by international ophthalmological bodies, ours differ in that universal masking is strictly adhered to inside hospital premises. In addition, whilst many international centres are only providing emergency eye services during this pandemic, we have maintained a core service in the past 3mo (first COVID-19 case recorded in HK on January 22, 2020) without incidence of cross-infection in our hospital. Of course, we may need to adjust our service delivery model in response to the global and local infection status.
The infection control measures at our centre evolved from our experience of the SARS in 2003. The main goals of these measures are to 1) minimize cross-infection between staff and patients, 2) protect and support hospital staff, and 3) ensure a safe and hygienic work environment.
Minimizing Cross-Infection Between Staff and Patients
To minimize cross-infection between staff and patients, we adhered to the principles of crowd reduction and patient triage. Of note, universal masking is practiced throughout the hospital—mask must be worn by every patient and visitor who enters the hospital, and proper wearing of the mask is ensured by staff at the entrance. Masks are kept on during consultations, laser procedures, and operations up until the point of skin preparation. Taping the upper edge of surgical masks during examination/laser procedures with condensing lenses/contact lenses can prevent lens surfaces from fogging up. Speaking is reduced as much as possible during consultations to reduce risk of droplet transmission.
Crowd Reduction
Before COVID-19, about 900 patients (many of them with accompanying persons) attended our hospital every day. To reduce caseload in response to the situation of COVID-19, all patients with routine follow-up are contacted via text messages and advised to defer and reschedule their appointment if their eye conditions are stable. Drug refill clinics have been set up for patients who require medication refill to allow minimum doctor-patient contact. Announcements have also been posted on the HA website to encourage people to stay at home and avoid non-urgent medical appointments. Patients are also advised to have no more than one accompanying person when attending our hospital. With these measures, our out-patient attendance rate has been reduced by about 40%. Meanwhile, all corporate and staff activities have been cancelled, including grand rounds, local and overseas training programs, clinical attachment by medical students, volunteering services, and staff recreational activities.
Reducing Outpatient Procedures, Elective Operations, and General Anesthesia Sessions
Although there is little evidence showing SARS-CoV-2 being present in tears[10]–[11], we avoid performing syringing and probing for all patients. The procedure can result in splashing of tears, increasing the risk of infection and generating anxiety among staff. In addition, reduction of aerosol-generating procedures (AGPs) is a top priority as they pose an increased risk of aerosol spread of infectious agents irrespective of the mode of transmission. As such, endoscopic dacryocystorhinostomy has been suspended, and operations requiring general anesthesia have been limited to emergency cases only, reducing caseload by 90%. Finally, elective operations have been reduced, with a total reduction of surgical load by 40%. The reduction of surgical volume also lowered the consumption of PPE during a time of scarce resources. In the case where surgery is deemed necessary, we follow strict infection control measures to reduce cross-infection risk between patients and our staff. Patients are required to wear surgical masks in the operation room up until skin preparation and draping, and masks are reapplied immediately after completion of surgery. For cases with COVID-related symptoms or positive travel history, nasopharyngeal swabs are performed to rule out COVID-19 before transferring the patient to the operation theatre. Finally, should a confirmed COVID-19 case require urgent eye surgery, the operating team is advised to inform the infection control team and be equipped with full PPE, which includes goggles, an N95 respirator, Association for the Advancement of Medical Instrumentation (AAMI) level 3 isolation gowns, disposable gloves, hair covers, +/- face shield, depending on the surgical procedure.
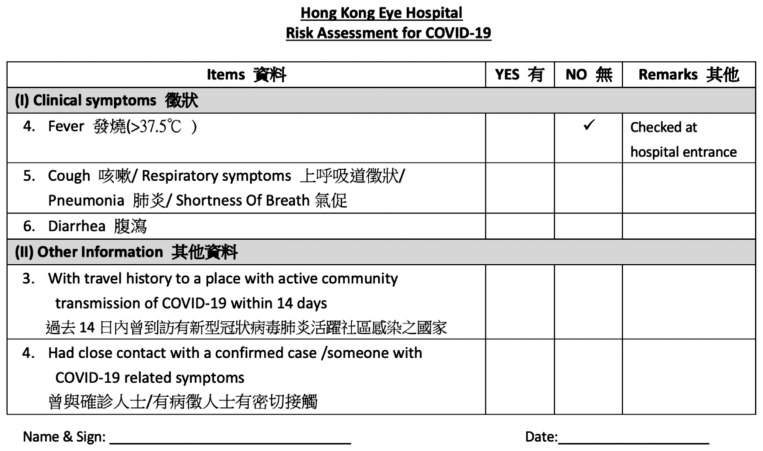
Fever Screening
Before entering our hospital, every patient and his/her accompanying person is required to undergo temperature checking (Figures 1 and 2). If his/her temperature is higher than 37.5°C, the patient is advised to postpone the appointment unless there is an urgent ophthalmic indication, and to seek medical advice at nearby General Outpatient Clinic or Accident and Emergency Department.
Figure 1. Signage at the hospital's main entrance alerting incoming patients to undergo temperature check and to wear a surgical mask.

Figure 2. Infrared body temperature screening system located at the main entrance of the hospital.

Patient triage
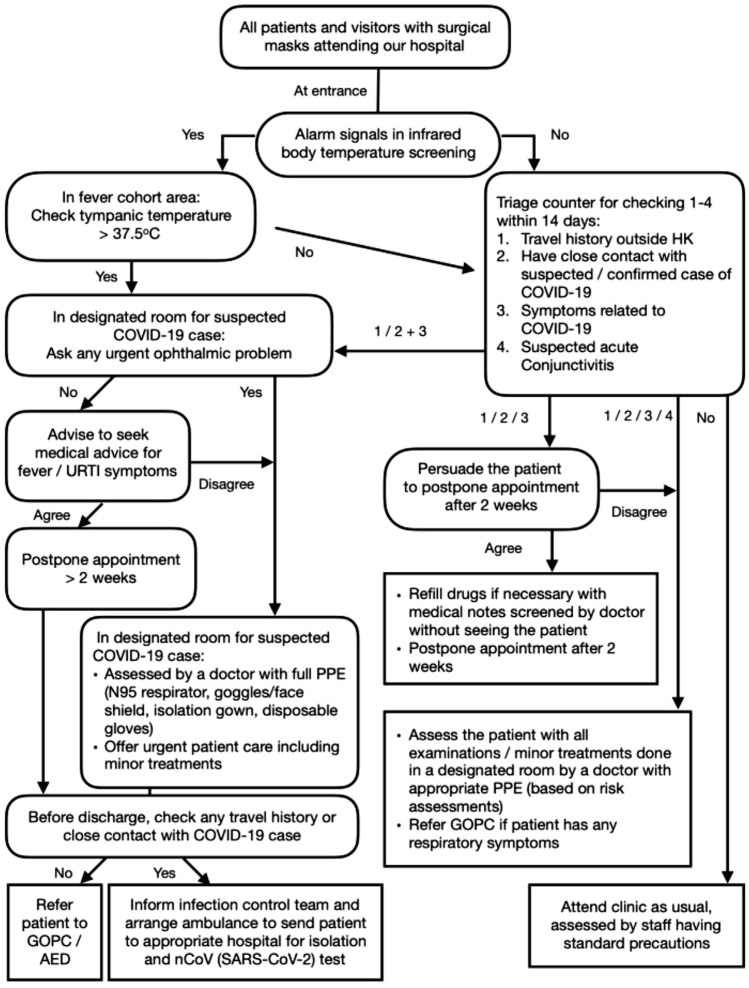
The workflow of COVID-19 screening at Hong Kong Eye Hospital is summarized in Figure 3. After fever screening, the patient and his/her accompanying person are interviewed by trained nurses using a screening questionnaire (Figure 4). If the patient has COVID-19 related symptoms, has travelled to areas with active COVID-19 transmission in the past 14d (a travel history indicator is available in our electronic health record system), or has had close contact with a confirmed or suspected case of COVID-19, he/she is advised to seek medical attention and to reschedule the appointment. If the patient has an urgent eye condition that requires immediate attention, he/she is assessed and managed by a doctor in a designated room to reduce infection risks to other patients and staff. In the 6wk that this screening protocol has been in effect, we have screened out a total of 143 patients fulfilling the above criteria; 87 patients were rescheduled to have later appointments, while the remaining 56 were seen in a designated room (see next section).
Figure 3. Workflow of COVID-19 screening at Hong Kong Eye Hospital.
URTI: Upper respiratory tract infection; GOPC: General outpatient clinic; AED: Accident and emergency department.
Figure 4. Screening questionnaire for COVID-19.
Designated examination rooms for suspected COVID-19 cases and high-risk patients
Anyone who fails fever and/or questionnaire screening is advised not to enter our hospital. However, if an urgent ophthalmic condition is suspected, the patient will be assessed in designated rooms (Figure 5) by a doctor equipped with appropriate PPE. Two designated rooms are available at our centre: one for seeing fever cases or cases fulfilling COVID-19 reporting criteria (Table 2)[23], and the other for seeing patients with suspected acute conjunctivitis or those with COVID-19 related symptoms, travel, contact, or cluster history. Disinfection of the slit lamp and ophthalmological instruments are performed after every case.
Figure 5. Designated consultation room for fever cases/cases fulfilling COVID-19 reporting criteria, equipped with neutral air pressure and an air purifier.

Table 2. Case reporting criteria for COVID-19 according to the Centre of Health Protection, Department of Health, Hong Kong[23].
| Clinical criteria | Epidemiological criteria |
| Presented with fevera or acute respiratory illness or pneumonia | Either one of the following conditions within 14d before onset of symptom: with travel history to a place with active community transmission of COVID-19 or had close contact with a confirmed case of COVID-19 |
aExcept fever due to a known etiology not related to respiratory infections.
Spacing out appointment time slots and special waiting areas
Appointment time slots are spaced out so as to minimize the number of patients in the waiting area at a given period of time. In addition, patients with fever or respiratory symptoms are arranged to wait in a designated area before consultation to avoid cross-infection among patients.
Eye Bank
The HA Eye Bank, which supplies donor ocular tissues to the whole of Hong Kong, is situated within Hong Kong Eye Hospital. Since non-urgent clinical services have been reduced as per Hong Kong HA directives, active solicitation for donation of ocular tissues has been temporarily suspended, resulting in a 70% reduction of ocular tissue donation. Donor corneas are currently only obtained from voluntary donation initiated by donor family, multiple organs donors, and referrals from other staff. These donated corneas, as well as our stock of frozen corneas, support the current demand in emergency operations. With recommendations from Eye Bank Association of America (EBAA)[24], the criteria for acceptance of potential donor corneas have been modified. The additional criteria include: 1) Potential donors did not have fever or lower respiratory symptoms; or if they did, it was not related to COVID-19; 2) The death of donor was not related to COVID-19; 3) The donor did not have travel history to an area with active community COVID-19 transmission.
Protecting and supporting hospital staff
Adequate protection is key to minimize infection risks and to alleviate panic and anxiety surrounding a novel infectious agent (Table 3)[25].
Table 3. Protective measures at Hong Kong Eye Hospital during COVID-19.
| Protective measures | Details |
| 1 Working uniforms Rationale: to reduce risk of cross-contamination via fomite transmission |
- Doctors are provided with scrubs to minimize cross-contamination inside and outside of the hospital Scrubs must be changed daily and cannot be worn outside of the hospital premise |
| 2 Provision of adequate PPE - Rationale: staff must be well protected to deliver care to our patients - All hospital staff are provided with PPE that is appropriate for the specific clinical setting - The hospital administration maintains good communication with the central supplies department to ensure stable supply of PPE - Staff are regularly reminded to be prudent with their use of PPE in the face of scarce resources |
- Universal masking within the hospital vicinity except for mealtimes - Goggles and disposable glovesa are provided - Arrangement of N95 respirator fit tests to ensure that appropriate models are being used by staff who need them When attending to a fever case/suspected case of COVID-19: Full PPE: fitted N95 respirator, at least AAMI level I isolation gown, disposable gloves, eye protection (goggles/face shield), with or without hair cover When attending to acute conjunctivitis, patients with COVID-19 related symptoms, or patients with positive travel contact, or cluster history: At least a surgical mask, disposable gloves, and eye protection (visors, goggles, or face shield) |
| 3 Easy access to alcohol-based hand rub Rationale: hand hygiene is the single most important measure in reducing disease transmission |
- In addition to bottles of alcohol-based hand rub in consultation rooms, wall-mounted bottles of alcohol-based hand rub have been installed throughout the hospital to ensure easy accessibility - Pocket-sized alcohol-based hand rubs were distributed to ensure frequent hand hygiene |
| 4 Optimizing non-clinical areas Rationale: meals are high-risk events as masks need to be removed and there is usually talking over food |
- Opening up of lecture hall and conference rooms during mealtimes to ensure adequate spacing between staff members - All staff are required to sit 6 feet apart from each other and to face the same direction when eating - Mask on immediately after meals before talking and chatting |
| 5 Regular review of infection control practices by the Infection Control team Rationale: as COVID-19 is a new and rapidly evolving situation, regular review by the Infection Control team is essential in ensuring rapid adaptation of policies to reduce risk of disease transmission |
- Weekly hospital rounds by Infection Control Nurses, providing training and updates on appropriate use of PPE, ensuring frequent and proper hand hygiene, and giving expert advice on infection control issues |
| 6 Staff health monitoring and reporting system Rationale: early detection protects staff and patients |
- All staff members must check their body temperatures every day before work - In line with the Hong Kong government's issuance of the Red Outbound Travel Alert[25], staff members are advised against travelling abroad, including to mainland China or Macau. If they do, there will be 14d of mandatory quarantine on their return with the quarantine period deducted from their annual leave - All staff who have travelled abroad must undergo COVID-19 testing before resuming clinical duty - If staff members experience any fever or COVID-19 related symptoms, they must report to their supervisors, refrain from work, and seek medical advice immediately - Staff who are quarantined due to close contact history with confirmed COVID-19 case are granted authorized absence |
| 7 Online education and updates Rationale: regular communication between hospital administration and staff reduces miscommunication, allows experience-sharing, and ensures timely management of identified problems. |
- Mandatory review of online infection control course - Daily-updated online information packs available on the Hospital Authority website - Regular staff forums via videoconferencing to provide updates and to allow staff to voice out concerns so that they can be addressed by the hospital management in a timely manner - Most face-to-face meetings have been replaced with videoconferencing - Resumption of grand round in webinar format to allow continued medical education without risk of cross-infection |
aGloves, if worn, should be removed after attending to each patient.
Environmental control
A regularly sanitized environment is crucial in combating any infectious disease, especially if the microbial agent can survive on inanimate objects for hours to days (Table 4, Figures 6 and 7).
Table 4. Environmental control measures at Hong Kong Eye Hospital.
| Environmental measures | Details |
| Cleaning of floors and surfaces | - Interior surfaces such as floors and walls are regularly cleaned with 1:49 bleach containing 5.25% sodium hypochlorite. 1:49 diluted bleach is sufficient in decontaminating surfaces or articles contaminated with secretions, vomitus, and excreta - Extra cleaning staff was hired for cleaning of frequently touched areas; public areas (e.g. door handles) are cleaned every two hours and elevator panels are cleaned every hour - Toilet covers are closed before flushing in order to prevent splashing and possible aerosol generation. |
| Enhanced ventilation | - The designated rooms are equipped with portable High- Efficiency Particulate Air (HEPA) units (Figure 6) |
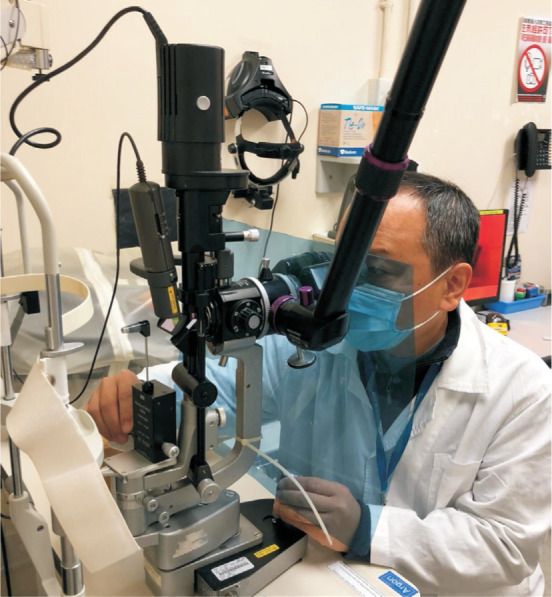
| Instruments | - Slit lamps have been fitted with plastic breath shields to block the exchange of droplets between the ophthalmologist and the patient (Figure 7), and are wiped down with 70% alcohol wipes after each patient - Non-contact tonometer is avoided as much as possible. If clinically indicated, Goldmann tonometers with disposable tips, Tonopen, or iCarePro are used instead |
Figure 6. Portable HEPA filter unit.

Figure 7. Slit lamp fitted with plastic breath shields.
DISCUSSION
The fight against COVID-19 has been challenging for the most part due to an initial lack of knowledge and information on this disease. This underscores the importance of emergency preparedness and the ability to adapt swiftly to any rapidly evolving situations. Notably, our infection control strategies align with international and local government guidelines, with particular emphasis on patient triage and isolation.
In fact, most of the current infection control measures were derived from experiences during the SARS outbreak in 2003. SARS and COVID-19 are caused by different species of coronavirus and share many similarities, one of which being the route of transmission. Direct contacts, droplets and fomites are established routes of transmission in both diseases; tears and eye discharge were also suspected SARS transmission routes[26]. However, while there were 1755 SARS cases in Hong Kong (including 386 health care workers, 8 of whom died)[27]–[28], there has not been any case of healthcare worker infection of COVID-19 in Hong Kong hospitals at the time of writing. This is undoubtedly at least partially due to the lessons learned from SARS: a case-control study of 72 hospital workers with SARS found that the likelihood of SARS infection was strongly associated with the perceived inadequacy of PPE supply, insufficient infection control training, and inconsistent use of PPE[29]. In the Ophthalmology Department of one of the most hard-hit acute hospitals in Hong Kong during SARS, infection control measures that were stratified according to clinical scenarios are very much in line with measures currently taken by ophthalmic centres worldwide, such as service volume adjustment, patient triage, universal precaution measures and environmental disinfection[30]. With these measures, none of the staff and patients was infected within that ophthalmology department, in both in-patient and outpatient areas throughout the massive SARS outbreak in 2003. These prior experiences have been invaluable to the battle against COVID-19 and have served as a blueprint for escalating infection control response to this rapidly evolving disease.
COVID-19 has also caused us to reflect on the future directions that we should take in maintaining quality ophthalmic care for our patients. While some ophthalmic conditions do not require immediate medical attention (e.g. mild cataract), many conditions can deteriorate quickly in a matter of hours or days without prompt treatment (e.g. acute primary angle closure, proliferative diabetic retinopathy, retinal detachment, etc.). Although many eye centres are still maintaining emergency face-to-face consultation services during this pandemic, it is becoming increasingly clear that telemedicine has an important role in ophthalmology. With the advent of portable smartphone diagnostic tools and the easy sharing of knowledge on social media, remote diagnosis has been made possible, such as in the cases of diabetic retinopathy and retinopathy of prematurity. While we acknowledge there are limitations and pitfalls in telemedicine, such as liability and regulatory concerns[31], telemedicine can help maintain accessibility to ophthalmic care should the COVID-19 situation persist for months or if similar diseases arise again in the future.
CONCLUSION
While COVID-19 is a novel microbial entity, the concept of infection control is not. To disrupt the chain of infection, a multi-pronged approach must be adopted to reduce possible sources of infections, protect susceptible hosts, and ensure environmental disinfection. COVID-19 is an on-going lesson in infection control preparedness; as we continue to evolve and adapt our responses to the rapidly changing situation, may we all learn from this pandemic in preparation for similar outbreaks in the future. We hope that our experience can provide a framework for fellow ophthalmology colleagues in other parts of the world.
Acknowledgments
Our current preventive measures are supported and executed by our medical, nursing, allied health, supporting, management, and administrative staff of our hospital. In particular, we would like to acknowledge the contributions from our Infection Control nurses, Ms. Iris Wong and Ms. Ada Cheung; Ms. Phyllis Yim, Ms. Ivy Leung, Ms. Wai Yee Chiu, Ms. Louise Lam and their nursing teams; Ms. Elaine Ng and her hospital administration team; Ms. Catherine Wong and her Eye Bank team. We would also like to thank microbiologist Dr. Naomi Cheng for her expert advice on infection control.
Some of the preventive measures were adopted or modified from other eye centres in Hong Kong, as well as from Hong Kong HA guidelines. We are thankful for their collective excellent efforts in combatting COVID-19 together.
Conflicts of Interest: Cheung SSL, None; Wong CYK, None; Chan JCK, None; Chan CK, None; Lam NM, None; Yuen HK, None; Wong VW, None; Tsang CW, None; Tham CCY, None.
REFERENCES
- 1.John Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at John Hopkins University. 2020. [Accessed on 19 April, 2020]. https://coronavirus.jhu.edu/map.html.
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020 [Google Scholar]
- 3.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, Wang YY, Xiao GF, Yan B, Shi ZL, Zhou P. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong SX, Lu XY, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Novel Coronavirus (2019-NCoV) Situation Reports-46. 2020. [Accessed on 24 March, 2020]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 7.Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020:S0195-S6701(20)30101-8. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-2019) Feb 16-24, 2020. [Accessed on 24 March, 2020]. http://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 9.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia JH, Tong JP, Liu MY, Shen Y, Guo DY. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seah IYJ, Anderson DE, Kang AEZ, Wang LF, Rao P, Young BE, Lye DC, Agrawal R. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020:S0161-S6420(20)30311-0. doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Academy of Ophthalmology. Coronavirus kills Chinese whistleblower ophthalmologist. 2020. [Accessed on 25 March, 2020]. https://www.aao.org/headline/coronavirus-kills-chinese-whistleblower-ophthalmol.
- 13.Centre of Health Protection, Department of Health, Hong Kong. Latest Situation of Coronavirus Disease (COVID-19) in Hong Kong. 2020. [Accessed on 19 April, 2020]. https://chp-dashboard.geodata.gov.hk/covid-19/en.html.
- 14.International Council of Ophthalmology. ICO Global COVID-19 Resource Center. 2020. [Accessed on 2 April, 2020]. http://www.icoph.org/news/news_detail/602/ICO-Global-COVID-19-Resource-Center.html.
- 15.China Center for Disease Control and Prevention. Interpretation of “Guidelines for the Prevention and Control of New Coronavirus Infections in Medical Institutions (First Edition)”. Jan 22, 2020. [Accessed on 27 March, 2020]. http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200123_211393.html.
- 16.Shao L, Wei WB. Suggestions on the protection for ophthalmologists against the infection of the novel coronavirus. Int Rev Ophthalmol. 2020;44:1–4. [Google Scholar]
- 17.American Academy of Ophthalmology. Alert: Important coronavirus context for ophthalmologists. 2020. [Accessed on 30 March, 2020]. https://www.aao.org/headline/alert-important-coronavirus-context.
- 18.Royal College of Ophthalmologists. Coronoavirus RCOphth update—need to know points. 2020. [Accessed on 26 March, 2020]. https://www.rcophth.ac.uk/wp-content/uploads/2020/03/Coronavirus-RCOphth-update-March-19th.pdf.
- 19.National University Hospital. Visitor Policy and Registration. 2020. [Accessed on 26 March, 2020]. https://www.nuh.com.sg/patients-visitors/Visiting-Policy-Registration/Pages/default.aspx.
- 20.Singapore National Eye Centre. Important notice: COVID-19. 2020. [Accessed on 26 March, 2020]. https://www.snec.com.sg.
- 21.Hospital Authority, Hong Kong. Hospital Authority activates Emergency Response Level. Jan 25, 2020. [Accessed on 26 March, 2020]. https://www.info.gov.hk/gia/general/202001/25/P2020012500689.htm.
- 22.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020;258(5):1049–1055. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centre of Health Protection, Department of Health, Hong Kong. Latest Overseas Situation of COVID-19 and Revised Reporting Criteria for Suspected Cases of COVID-19. Feb 28, 2020. [Accessed on 24 March, 2020]. https://www.chp.gov.hk/files/pdf/letters_to_doctors_20200228.pdf.
- 24.Eye Bank Association of America. Informational alert: Coronavirus disease 2019 (COVID-19) and eye tissue donation. Mar 2, 2020. [Assessed on 2 April, 2020]. https://restoresight.org/wp-content/uploads/2020/03/COVID-19-and-Eye-Tissue-Donation-March-2-2020.pdf.
- 25.Security Bureau, the Government of the Hong Kong Special Administrative Region. Outbound Travel Alert. Mar 17, 2020. [Accessed on 31 Mar, 2020].
- 26.World Health Organization. Update 27 F One month into the global SARS outbreak: Status of the outbreak and lessons for the immediate future. Apr 11, 2003. [Accessed on 17 April, 2020]. http://www.who.int/csr/sarsarchive/2003_04_11/en/.
- 27.Cheng VC, Lau SK, Woo PC, Yuen KY. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20(4):660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int J Occup Environ Health. 2004;10(4):421–427. doi: 10.1179/oeh.2004.10.4.421. [DOI] [PubMed] [Google Scholar]
- 29.Lau JT, Fung KS, Wong TW, Kim JH, Wong E, Chung S, Ho D, Chan LY, Lui SF, Cheng A. SARS transmission among hospital workers in Hong Kong. Emerging Infect Dis. 2004;10(2):280–286. doi: 10.3201/eid1002.030534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan WM, Liu DTL, Chan PKS, Chong KKL, Yuen KSC, Chiu TYH, Tam BSM, Ng JSK, Lam DSC. Precautions in ophthalmic practice in a hospital with a major acute SARS outbreak: an experience from Hong Kong. Eye. 2006;20(3):283–289. doi: 10.1038/sj.eye.6701885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morse AR. Telemedicine in ophthalmology: promise and pitfalls. Ophthalmology. 2014;121(4):809–811. doi: 10.1016/j.ophtha.2013.10.033. [DOI] [PubMed] [Google Scholar]