Abstract
Purpose
Diabetes is one of the leading causes of mortality and morbidity among women in India. The burden of diabetes among women was found to increase with age and exposure to the post-partum period. The present study examines the spatial variation in the prevalence of diabetes among women in the late reproductive age-group of 35–49 years across 640 districts in India.
Methods
The study utilized data from the recent round of the National Family Health Survey, 2015–16. Age-standardized prevalence rates were calculated, followed by an examination of economic inequality using the poor-rich-ratio (PRR) and Wagstaff’s concentration index. Spatial variation in the prevalence of diabetes was explored with a series of quantile maps, univariate, and bivariate LISA cluster maps. Further, to explore the district-level diabetes prevalence among women in the country, Ordinary Least Square and Spatial Autoregressive (SAR) models were used.
Results
The study findings affirm the presence of spatial clustering in the burden of diabetes among women. The burden is relatively higher among women from the Southern and Eastern parts of the country. Findings establish obesity, hypertension, and living in urban areas as major correlates of diabetes.
Conclusion
Program with an aim to lower the intensity of community-based prevalence of diabetes, especially among women in their late reproductive ages, should adopt differential approaches across different states/districts in the context of their lifestyle, dietary pattern, working pattern, and other socio-cultural practices.
Electronic supplementary material
The online version of this article (10.1007/s40200-020-00545-w) contains supplementary material, which is available to authorized users.
Keywords: India, Chronic diseases, Diabetes, Districts, Geospatial, Women
Introduction
In the twenty-first century, diabetes is one of the leading threats to human health and is increasing rapidly all over the world at an alarming rate. It is one of the most common diseases that involve a range of metabolic disorders due to an increase in blood sugar levels. It is chronic and may be caused by an absence or insufficient production of insulin or an inability of the body to utilize insulin properly. It may trigger due to genetic disposition, lifestyle, or dietary habits. It leads to an increased concentration of glucose in the blood (hyperglycaemia), which is a symptom and not the cause of this disease. It is associated with numerous health conditions like obesity, hypertension, and a range of heart-related ailments [1].
Today diabetes has become more prevalent than ever before. Though it may affect people of any age, those over 35 years are most affected. According to the recent estimates by International Diabetes Federation (IDF), in 2016, 422 million people live with diabetes around the world, and this number is projected to grow to 762 million by 2030 [2]. Diabetes is divided into type 1 and type 2. Bodies of Individuals who have type 1 diabetes do not produce insulin, whereas those with type-2 diabetes do not respond to insulin or do not make enough insulin. It has also been estimated that 85 to 90% of these diabetes cases constitute type-2 diabetes globally [3].
Recent studies by the World Health Organization (WHO) show that a considerable number of people with diabetes originate from low-and-middle-income countries. Existing literature suggests this elevation in the incidence of diabetes in developing countries, to be contributed by the increasing urbanization, changing lifestyles pattern, which is primarily sedentary. Additionally, the global nutrition transition marked by increased intake of high-energy foods with poor nutritional composition has acted as a catalyst in further accelerating the levels [4].
In recent years, diabetes has been identified as one of the leading causes of morbidity and mortality, influencing not just older adults but also young and middle-aged persons. Around 2.2 million deaths worldwide were attributable to high blood glucose, and the increased risks of associated complications (e.g., heart disease, stroke, kidney failure), which often result in premature death and these complications are often listed as the underlying cause of death instead of diabetes [2].
In the current health transition in India, resulting as a unification of demographic and epidemiological shift, the burden of Non-Communicable Diseases (NCDs) has been projected to be doubled by 2030. This is primarily due to development-oriented changes in the lifestyle and dietary patterns of the population [4–6]. There has been tremendous heterogeneity across the districts in the country, which has widened significantly after the advent of the economic liberalization of the 1990s. Consequently, the pattern of development and lifestyle changes have not been uniform and are greatly influenced by social stratification and class, resulting in differential prevalence in obesity, hypertension, and other risk factors for diabetes [7].
Moreover, existing literature points out the existence of a gap between the level of obesity for the women who have been experiencing the post-partum period at least once and those who have never undergone a conception [8, 9]. Studies also recommend that the effect of being in a post-partum period further accelerates by the action of changes in the level of urbanization and dietary practices [8, 9]. Therefore, it is crucial to explore the spatial variations in the burden of diabetes for strengthening policy-related interventions.
Thus, with the increasing prevalence of diabetes in India, this paper attempts to answer research questions about the nature and types of meso-scale variables affecting the prevalence of diabetes among women in their late reproductive ages? And, what is the nature of spatial clustering and dispersion of diabetes among women in India? Given these research questions, the primary objective of this paper is to explore the spatial heterogeneity and identify the correlates of diabetes among women age 35–49 years across 640 districts in India.
Material and methods
Data
The study utilized data from the fourth round of the National Family Health Survey (NFHS)-4 in India, which is a cross-sectional survey conducted during 2015–16. NFHS is conducted under the stewardship of the Ministry of Health and Family Welfare (MoHFW), Government of India. The survey provides information on demographic and health indicators at the national, regional, state, and district levels from a nationally representative sample.
NFHS-4 (2015–16) collected information from a total of 601,509 households and 699,686 women aged between 15 and 49 years [10]. It is for the first time that NFHS has measured population-based blood glucose levels among all the interviewed women aged 15–49 years and men aged 15–54 years. The information on the emerging health issues, including the prevalence of diabetes for each of 640 districts in the country for women is available in the public domain [10]. However, all the estimates generated for men and selected estimates on women were provided only at state level. The district-level shapefile was retrieved from GitHub through https://github.com/datameet/maps/tree/master/Districts. Other relevant information regarding the study design and response rates in the NFHS-4 can be obtained from the Demographic and Health Surveys website [10].
Ethical statement
This study utilizes secondary data from a national survey conducted under the stewardship of the Ministry of Health & Family Welfare, Government of India, with the help of the International Institute for Population Sciences as the nodal agency. The data does not contain any identifiable information on the study subjects. This de-identified data has been archived in the Demographic and Health Surveys (DHS) public repository, where the data is easily accessible using https://www.dhsprogram.com/data/available-datasets.cfm. All the study tools utilized in the survey have received ethical approval from the Institutional Review Board (IRB) at the International Institute for Population Sciences (IIPS), Mumbai, India.
Study population
As already discussed, experiencing the post-partum period at least once increases the risk of being obese, which is a primary risk factor of diabetes. Thus, in the present study number of children ever born (CEB) is considered as a proxy of experiencing a post-partum period. Also, the study assumes that women in their late reproductive ages, i.e., 35–49 years have completed their desired family size. Thus, after stratifying the data for age and removing the outliers, the data on 235,056 women aged 35–49 years have been analyzed to draw inferences.
Outcomes
The presence of diabetes is considered to be the outcome of interest. It is a general practice of utilizing fasting blood sugar levels to measure whether or not an individual suffers from diabetes. However, as NFHS does not provide data on fasting blood sugar during the survey, a respondent was considered as diabetic if the random blood sugar (RBS) level was ≥140 mg/dl [10].
Predictor variables
The predictors included in the study were based on the existing literature that aims to identify the burden and risk factors associated with various chronic diseases [8, 11, 12]. Health-related inequalities are grounded on socio-economic and demographic factors; thus, the study included age (in years), place of residence, social group, religion, years of schooling, and wealth index. Out of all the variables included in the study, social group (caste) and religion are essential indicators of Socio-economic status (SES), as they affect the dietary patterns and accessibility to health care resources in India [13, 14]. The social group was divided into two categories on the basis of social exclusion, namely socially deprived and not-deprived. The deprived group consisted of Scheduled Castes and Scheduled Tribes, which are traditionally most underprivileged sections of the Indian society, whereas, all the other castes combined to form not deprived category [14]. Also, as NFHS does not provide data on the income of the individual, the DHS wealth index has been used as a proxy. The construction utilizes information on all the possible assets, and utility services present in any household. The wealth index was constructed using a Principle Component Analysis (PCA), as suggested by Rutstein [15].
It is worth mentioning that as the study is based on women in their late reproductive ages, it is important to include the total number of Children Ever Born (CEB). Additionally, the study included two major comorbidities of diabetes, i.e., obesity [16] and hypertension [17]. Obesity and hypertension were computed using Body Mass Index (BMI) and measured Diastolic (DBP) and Systolic Blood Pressure (SBP), respectively. An individual falls into the category of obese if his/her BMI is higher than or equal to 30 kg/m2 [10]. Also, the respondent was considered as hypertensive if the systolic blood pressure (SBP) was ≥140 mmHg or diastolic blood pressure (DPB) was ≥90 mmHg, or the respondent is presently taking medications to lower the blood pressure [10]. It was the first time in the history of NFHS that biomarker data were collected at the district level for all states and Union Territories (UTs) of the country. Additionally, all the aforementioned cut-offs have been derived from the accepted ranges utilized by the National Family Health Survey [10].
Statistical analysis
The study aims to explore the levels, inequalities, and spatial differentials of diabetes among women in the age-group of 35–49 years in India. The entire analysis was, therefore, divided into two sets of statistical methods. In the first set of statistical tools, the age-adjusted prevalence of diabetes among selected women has been calculated. Age-adjusted prevalence rates were calculated using the direct standardization method, considering Census 2011, as the standard population. The proportion of age-specific census population by the total census population was used as weights [18]. Additionally, in order to explore economic inequality in the prevalence of diabetes, the poor-rich-ratio (PRR) and Wagstaff’s concentration index have been utilized.
In the second approach, to carry out the sub-national level analysis, districts have been chosen as the unit of analysis. Initially, a shapefile for 640 districts was generated for conducting the exploratory spatial analysis. This exploratory spatial analysis included generating a district-level quintile map. Further to examine the spatial dependence and clustering of diabetes burden appropriate measures like, Moran’s I indices, and univariate Local Indicator of Spatial Autocorrelation (LISA) cluster and significance maps were generated. Spatial weights of order one, using a Queen’s contiguity weight matrix were generated, which are essential for the computation of spatial autocorrelation indices. Queen’s contiguity matrix is a method of calculating weights based on contiguity from the polygon boundary file. It was selected to explore the existence of interdependence between diabetes prevalence and the selected set of predictors in the neighbouring districts. Further measures like Bivariate Moran’s I indices, Local Indicator of Spatial Autocorrelation (LISA), and spatial regression techniques have been used to examine the spatial dependence and correlates of diabetes [11, 17, 19, 20].
At the preliminary level, Ordinary Least Square (OLS) regression with diabetes prevalence as an outcome was taken into consideration. Additionally, to control the spatial effects, spatial autoregressive (SAR) models were fitted to the data. Diagnostics tests for spatial dependence were carried out for both the models to identify the best spatial fit. A larger value of Legrange Multiplier (LM) and a relatively larger value of adjusted R2 explains the better model adequacy. Additionally, lower values of the Akaike Info Criterion (AIC), demonstrates better suitability of the model [17].
The basic analysis was completed using STATA Version 15.0 (StataCorp, Texas). Geo-Da version 1.12.1.129 (Teknowledgist, New York) was used to do the spatial analysis. Data visualization was done using R Studio version 1.1.463 (R Studio, Inc.). All the estimates provided in this study are derived by applying appropriate sampling weights contributed by Demographic and Health Survey (DHS) India, 2015–16.
Results
The present study on the spatial variation in the prevalence of diabetes among women in their late reproductive ages (35–49 years) is based on a nationally represented sample of 235,056 women from all 36 States/Union Territories (UTs) covering 640 districts of India.
Description of the study subjects
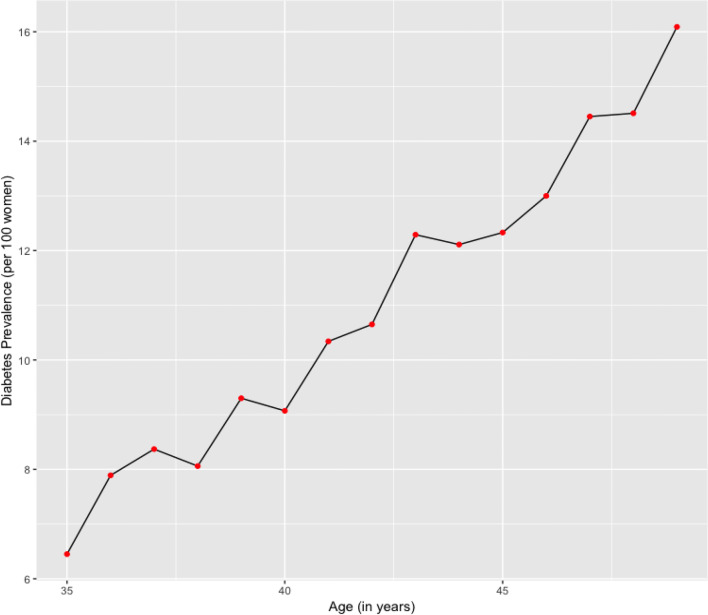
Figure 1 depicts the diabetes prevalence among women in their late reproductive ages (35–49 years) by age in single years. The findings from the figure suggest that with an increase in age (in years), the burden of diabetes increases. Thus, diabetes prevalence for women aged 35, 40, 45, 49 years is 6.5, 9.1, 12.3, and 16.1 per 100 women, respectively.
Fig. 1.
Prevalence of diabetes among women in their late reproductive ages (35–49 years) in India, National Family Health Survey, 2015–16
Table 1 provides the findings from the descriptive statistics for the sample under consideration. The majority of the respondent belonged to 35–39 years of age-group (37.34%). Around 65.0% of the respondent belonged to rural areas, and 82.0% followed Hinduism. Around 72% of the respondent belonged to socially non-deprived sections of the society. Around 80% had education below nine years. Twenty-three percent of the respondent belonged to the richest wealth quintile. Fifty-seven percent of the respondent had more than two children ever born. The majority of the respondents were not obese (89.9%) and not hypertensive (91.2%).
Table 1.
Descriptive Statistics and age-standardized prevalence of diabetes along with 95% CI among women in their late reproductive ages (35–49 years) in India, 2015–16
| Predictors | Weighted Percentage [Frequency] | Age-standardized prevalence |
|---|---|---|
| Age (in years) | ||
| 35–39 | 37.34 [88726] | |
| 40–44 | 32.08[75153] | |
| 45–49 | 30.58[71177] | |
| Place of Residence | ||
| Rural | 64.41 [164512] | 9.28 [9.24–9.33] |
| Urban | 35.59 [70544] | 13.15 [13.08–13.22] |
| Caste | ||
| Socially Deprived | 28.35 [82569] | 9.62 [9.55–9.69] |
| Socially Non-Deprived | 71.65 [152487] | 10.99 [10.94–11.04] |
| Religion | ||
| Hindu | 81.98 [176733] | 10.42 [10.38–10.46] |
| Non-Hindu | 18.02 [58323] | 11.75 [11.65–11.85] |
| Years of Schooling | ||
| 0–9 | 79.23 [188660] | 10.08 [10.04–10.12] |
| 10 or more | 20.77 [46396] | 13.20 [13.11–13.30] |
| Wealth Index | ||
| Poorest | 17.14 [43967] | 7.01 [6.93–7.09] |
| Poorer | 18.96 [48922] | 8.59 [8.51–8.68] |
| Middle | 20.05[48057] | 9.97 [9.88–10.05] |
| Richer | 21.26 [46760] | 12.95 [12.86–13.05] |
| Richest | 22.60 [47350] | 13.46 [13.37–13.55] |
| Number of children ever born | ||
| At most 2 | 42.94 [90753] | 11.89 [11.82–11.95] |
| More than 2 | 57.06 [144303] | 9.79 [9.74–9.84] |
| Obesity | ||
| Yes | 89.85 [20629] | 20.84 [20.68–21.00] |
| No | 10.15 [214404] | 9.47 [9.43–9.51] |
| Hypertension | ||
| Yes | 8.82 [18743] | 18.89 [18.71–19.08] |
| No | 91.18 [182022] | 9.34 [9.30–9.39] |
| Total | 100.00 [235056] | 10.65 [10.62–10.69] |
The burden of diabetes by selected background characteristics
The burden of diabetes by selected background characteristics is presented in Table 1. To calculate the burden of diabetes among women in their late reproductive ages (35–49 years), the age-standardized prevalence of diabetes was calculated, where the standardization of age was done using the weights generated from the Census of India, 2011 [18].
The results suggest that the age-adjusted prevalence of diabetes among women aged 35–49 years in India was about 10.7%. The prevalence of diabetes was higher amongst respondent from urban areas [PR = 13.15 (13.08–13.22)], belonging to the socially-non-deprived group [PR = 10.99 (10.94–11.04)], non-Hindu religion [PR = 11.75 (11.65–11.85)], and those with ten or more years of schooling [PR = 13.20 (13.11–13.30)] than their respective counterparts. Furthermore, the prevalence was found to be increasing by wealth, i.e., it was least for the poorest category [PR = 7.01 (6.93–7.09)] and highest for richest wealth [PR = 13.46 (13.37–13.55) group. The prevalence was highest among women with at most two Children Ever Born (CEB) [PR = 11.89 (11.82–11.95)]. Women in their late reproductive ages who were obese were more likely to be diabetic than those who were non-obese [PR = 20.84 (20.68–21.00)]. Also, the prevalence of diabetes was higher among women with hypertension [PR = 18.89 (18.71–19.08)].
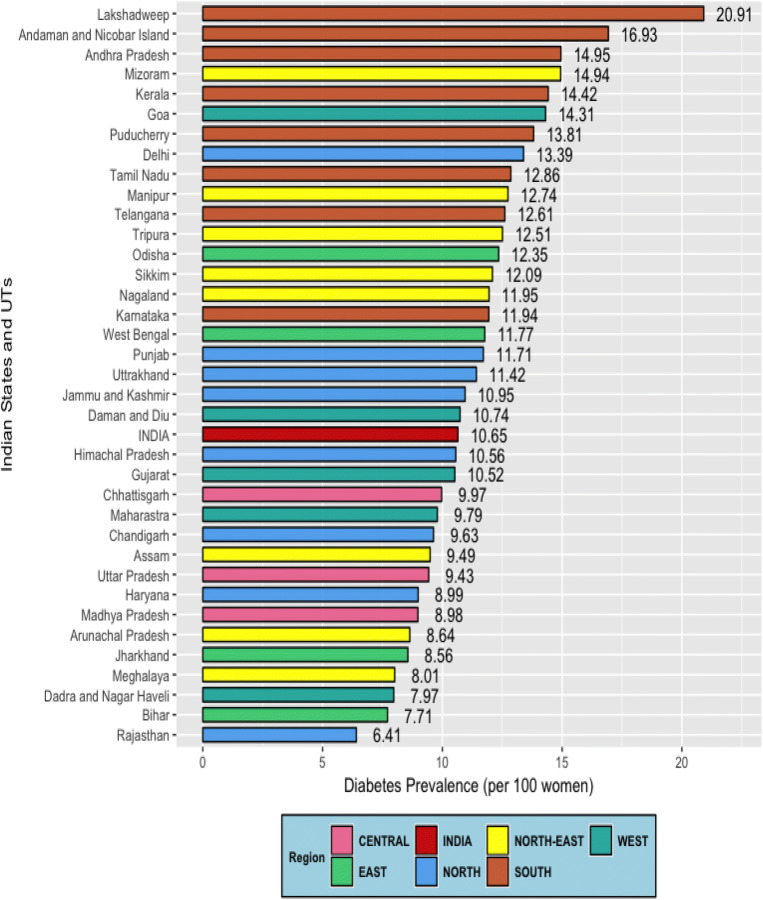
Age-standardized prevalence of diabetes across different States/Union Territories (UTs) is presented in Fig. 2. Results portray that all the Southern states, along with Mizoram, and Goa have a substantially higher prevalence of diabetes. On the other hand, states Rajasthan, Bihar, Meghalaya, Jharkhand, and Arunachal Pradesh had a lower age-adjusted prevalence of diabetes than the national average.
Fig. 2.
Age-standardized prevalence of diabetes among women in their late reproductive ages (35–49 years) across different States/Union Territories in India, 2015–16
Inequalities in the diabetes burden
To identify the inequalities in the burden of diabetes, two indicators, namely, poor-rich-ratio (PRR) and Wagstaff’s concentration index, have been utilized. It is apparent from the results in Table 2 that there is a massive gap in the prevalence of diabetes across poor and non-poor with a relatively larger concentration among non-poor, which holds even across different categories of the place of residence, educational attainment of women and various regions in the country. However, the disparity in the prevalence of diabetes is highest in the Eastern and Southern regions of the country and also among the women who have completed 0–9 years of schooling. These findings are also affirmed with the concentration index concerning the place of residence, years of education, and region of residence. The results depict that in all sub-groups of the selected predictors, a positive value of concentration index exists, which means that the prevalence of diabetes is higher for the women belonging to well-off households in all the selected sub-groups. However, the value to concentration Index was found to be higher among women from Eastern, North-eastern, and Southern regions.
Table 2.
Poor-rich-ratio and concentration index in the prevalence of diabetes among women in late reproductive ages (35–49 years) in India, 2015–16
| Predictors | Diabetes Prevalence | Concentration Index (CI) | SE (CI) | ||
|---|---|---|---|---|---|
| Poor | Rich | Poor/Rich Ratio | |||
| Residence | 0.1343*** | 0.004 | |||
| Urban | 10.05 | 13.08 | 0.77 | 0.0509*** | 0.005 |
| Rural | 8.05 | 11.61 | 0.69 | 0.1179*** | 0.005 |
| Years of Schooling | 0.1343*** | 0.004 | |||
| 0–9 Years | 8.24 | 12.79 | 0.64 | 0.144*** | 0.004 |
| 10 or more years | 9.22 | 11.90 | 0.77 | 0.043*** | 0.007 |
| Region | 0.1343*** | 0.004 | |||
| Northern | 6.69 | 10.15 | 0.66 | 0.1118*** | 0.009 |
| North-eastern | 9.30 | 12.90 | 0.72 | 0.1400*** | 0.009 |
| Central | 7.84 | 12.11 | 0.65 | 0.1296*** | 0.007 |
| Eastern | 8.42 | 13.55 | 0.62 | 0.1594*** | 0.008 |
| Western | 7.77 | 11.36 | 0.68 | 0.1157*** | 0.012 |
| Southern | 9.76 | 15.65 | 0.62 | 0.1304*** | 0.008 |
*p < 0.05, **p < 0.01, ***p < 0.001
Spatial variation in the prevalence of diabetes
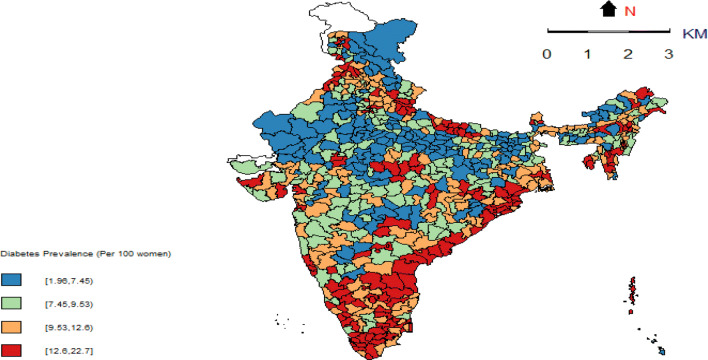
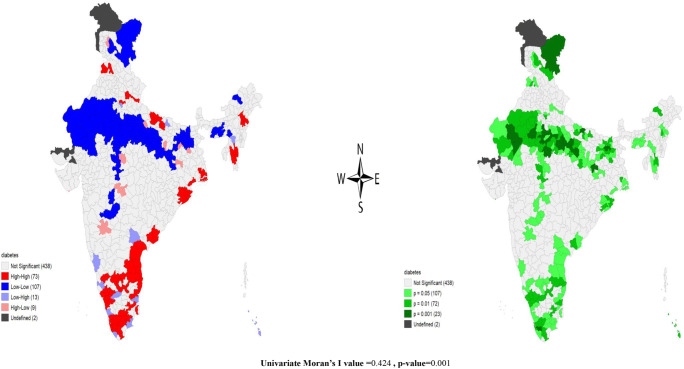
The spatial heterogeneity in the prevalence of diabetes among women in their late reproductive ages has dual evidence from quintile map as well as univariate LISA maps, presented in Figs. 3 and 4, respectively. It is evident from the quintile map that 254 districts in the country have a very high level of diabetes prevalence (greater than 10.7%) among women in their late reproductive ages. Another 130 districts have a moderately high prevalence of diabetes ranging from 8.7 to 10.6%. Most of these districts are located in the Southern and Eastern parts of the country. Findings suggest striking geographic clustering (Moran’s I = 0.42, p value = 0.001) of higher diabetes prevalence in the Southern and Eastern parts of the country; on the other hand, there were regions with substantially lower diabetes prevalence rates in parts of Central India. A detailed description of districts classified as hot spots (73 districts: Southern = 38 districts; Eastern: 11 districts; North-eastern:10 districts; Central region:8 districts; Northern:6 districts) and cold spots (107 districts: Central region: 44 districts; Northern:31 districts; Eastern: 22 districts; North-eastern:7 districts; Western = 4 districts) is provided in the supplementary material provided (Additional file 1 and Additional file 2).
Fig. 3.
Quintile map depicting the spatial distribution of diabetes across 640 districts of India, 2015–16 (NFHS-4)
Fig. 4.
Univariate LISA (cluster and significance) maps depicting spatial clustering and spatial outliers of diabetes across 640 districts of India, 2015–16 (NFHS-4)
Bivariate LISA results
Bivariate LISA examines the spatial relationship between the exposure and the outcome variable for the 640 districts of the country. Further, the values of Moran’s-I results presented in Table 3 provide quantitative evidence that the districts that had a higher proportion of urban areas were more likely to record higher prevalence rates of diabetes. However, the value of bivariate Moran’s I is highest with respect to the proportion of women aged 35–49 years having two or less CEB (Moran’s I = 0.38, p < 0.001), having obesity (Moran’s I = 0.27, p < 0.000), coming from economically better-off households (Moran’s I = 0.22, p < 0.000), living in urban areas (Moran’s I = 0.19, p < 0.000) and having hypertension (Moran’s I = 0.14, p < 0.000).
Table 3.
Bivariate Moran’s I statistics for diabetes prevalence by selected background characteristic in India, 2015–16
| Predictors | Moran’s I value (p-value) |
|---|---|
| Urban | 0.19 (0.000) |
| Non-SC/ST | 0.02 (0.412) |
| Non-Hindu | 0.14 (0.238) |
| Ten years of schooling or more | 0.07 (0.000) |
| Women having two or less CEB | 0.38 (0.000) |
| Rich | 0.22 (0.000) |
| Obesity | 0.27 (0.000) |
| Hypertension | 0.14 (0.000) |
Spatial correlates of diabetes burden
Results of the Ordinary Least Squares (OLS), Spatial Lag Model (SLM) and, Spatial Error Model (SEM) are presented in Table 4. All the variables which were significantly associated in the bivariate analysis were included in the regression model. The results from the OLS regression analysis show that having obesity and hypertension, two or more CEB, belonging to economically well-off households and urbanisation, are significantly associated with the burden of diabetes across India. Further, spatial models (SLM and SEM) are utilized to take spatial dependence into consideration. Findings from the model diagnostics suggest that SEM performs better than the other two models. The auto-regressive coefficient (error lag value λ) is 0.51, indicating a significantly higher spatial clustering in the diabetes prevalence, which is accounted for the geographical pattern of measured and unmeasured independent variables. The findings portray that the prevalence of diabetes among women aged 35–49 years in India is significantly affected by space. Being obese, hypertensive, and having two or less number of children ever born (CEB) and living in urban areas were the key predictors significantly explaining the spatial dependence in the prevalence of diabetes. It is worth emphasizing that the inclusion of spatial weights in the model has increased the predicting power of the model from 34% in case of OLS to 47% in the selected spatial regression model (SEM), indicating spatial clustering in the prevalence of diabetes among women aged 35–49 years in the country.
Table 4.
Ordinary Least Squares, Spatial Error and Spatial Lag model to assess the association between diabetes and selected background variables among women aged 35–49 years, India, 2015–16
| Predictors | Ordinary Least Square (OLS) | Spatial Lag Model (SLM) | Spatial Error Model (SEM) |
|---|---|---|---|
| Urban | 0.030 (0.000) | 0.027 (0.000) | 0.018 (0.044) |
| Ten or more years of schooling | 0.024 (0.139) | 0.017 (0.264) | 0.010 (0.019) |
| Women with CEB less than two | 0.058 (0.000) | 0.027 (0.001) | 0.036 (0.005) |
| Rich | 0.044 (0.000) | 0.031 (0.001) | 0.013 (0.314) |
| Obesity | 0.236 (0.000) | 0.180 (0.000) | 0.221 (0.000) |
| Hypertension | 0.121 (0.000) | 0.109 (0.000) | 0.111 (0.000) |
| Constant | 4.121 (0.000) | 1.203 (0.035) | 4.411 (0.000) |
| Number of Observations | 640 | 640 | 640 |
| Log likelihood | −1612.12 | −1562.68 | −1560.95 |
| AIC | 3242.24 | 3145.36 | 3139.9 |
| Adjusted R square | 0.34 | 0.46 | 0.47 |
| Lag Coefficient (ρ) | 0.452 (0.000) | ||
| Error Lag Value (λ) | 0.512 (0.000) |
Discussion
In the existing epidemiological transition in India, especially after the economic liberalization in the early 1990s, the burden of NCDs with the dominance of diabetes has been projected to be doubled by 2030 [21]. Development-oriented changes in the lifestyle of people, increasing urbanization, economic prosperity, and dietary practices have been considered as the major correlates of the increasing prevalence of diabetes. However, the pattern of development and lifestyle changes have not been uniform across the country and vary to a large extent by class and social stratification. This has resulted in a differential prevalence of obesity, hypertension, and other risk factors for diabetes [21].
The burden of various chronic NCDs were reported to increase disproportionally among the women who are about to achieve their menopause in different country settings [22–26]. Thus, women in the later stages of their reproductive cycle are more prone to get affected by one or more chronic diseases [22–26]. Additionally, the estimates from the Causes of Disease statistics suggest that diabetes-related mortality is higher amongst the women as compared to men in India [27]. Therefore, an attempt has been made in this study to explore the burden and inequalities in the diabetes burden among women in the late reproductive years in India. This issue is vital, as diabetes control in any population has a dual challenge of reducing the levels as well as inequalities across different sub-population. Monitoring and tackling disparities in diabetes and increased risks of associated complications like cardiovascular disease, stroke, kidney failure, etc., between socio-economic groups within countries has become an increasingly important objective for health interventions.
The analysis in this paper has been organized to focus on the correlates and spatial heterogeneity in the prevalence of diabetes among women aged 35–49 years across 640 districts in India using a nationally representative sample of 235,056 women from all 36 States/Union Territories (UT). Socio-economic and cultural heterogeneity in different regions of the country is expected to result in a differential lifestyle, which works as a catalyst in intensifying the pace of epidemiological transition with the ongoing age-structural transition.
Results portray that the prevalence of diabetes among women in their late reproductive ages was highest among those with two or fewer children ever born, who are more likely to be educated, belonging to economically prosperous households, living in urban areas and hence enjoying changing lifestyle with modernization, increased access to high energy (refined and processed) food and development. Findings clearly portray a higher prevalence of diabetes among urban women in India, who are one and a half times more likely to suffer from diabetes than their rural counterparts. These results are similar to the findings of Deshpande et al. (2008) and Ramachandran et al. (2012) based on data from South Asian countries that have pointed the increased diabetes risk was related with age, ethnicity, physical inactivity, obesity, and family history of diabetes [1, 28]. The urban-rural divide in the prevalence of diabetes is narrowing as urbanization is spreading widely, and is adversely affecting the lifestyle of populations [29].
Women in their late reproductive ages who were obese were more likely to be diabetic than those who were non-obese. This may be primarily because increasing obesity creates metabolic disturbances associated with insulin resistance, which occurs when beta cells of the pancreas do not produce and utilize sufficient insulin, a similar finding of Park et al., 1995, on their study in South Korea. Keen et al., 1979 identified obesity as a primary risk factor for diabetes about four decades back and highlighted that among obese women, even moderate changes in pre-pregnancy weight could affect the risk of gestational diabetes. Therefore, all the programs and services to address NCDs among women in their reproductive ages should prioritize addressing overweight and obesity among women to reduce the risk of diabetes [29].
Consistent with the theoretical premises and findings from other studies in the region [29], hypertension has been another comorbidity of diabetes among women in India as the prevalence of diabetes was higher among women with hypertension. Imam and Hossain (2012) also observed that diabetes is more common among those persons who have a sedentary lifestyle, i.e., are mostly physically inactive, having high blood pressure and excess body weight. This complete picture is prominent in the urban areas compared to the rural areas [30].
The findings of this study portray a relatively larger concentration of diabetes among women in the Southern and Eastern parts of the country, which are traditionally and culturally known as rice-meat-and-fish-eating areas, with higher consumption of sweets and snacks which are rich in trans-fats [31–33]. The clustering in diabetes prevalence is also affirmed with significantly higher values of Moran’s I and auto-regressive coefficient accounting for the geographical pattern of measured and unmeasured independent variables. The findings portray that in the prevalence of diabetes among women aged 35–49 years in India, is significantly affected by space. Being obese, hypertensive, and having two or less number of children ever born (CEB) were the key predictors significantly explaining the spatial dependence in the prevalence of diabetes among women aged 35–49 years in India. Among all the predictors included in the spatial model, the chance of suffering from diabetes is increasing with the highest pace with increasing obesity and hence creates a startling situation. However, as the study utilized data from a cross-sectional survey, no causal associations can be drawn.
Conclusion
The study findings indicate that accelerating rates of chronic morbidities, like diabetes needs to be given a importance in context of women who are about to complete their reproductive cycle, i.e., about to reach menopause. Also, increasing obesity among women aged 35–49 years needs to be prioritized as part of promoting a healthy lifestyle through physical exercise and salubrious dietary practices. A larger share of diabetes in India consists of type-2 diabetes, which can be prevented or delayed through lifestyle interventions. Many international randomized controlled trials have confirmed that we can stop the progression from pre-diabetes to type-2 diabetes by using planned lifestyle behaviour change programs [34]. Therefore, programs and interventions to lower the intensity of community-based prevalence of diabetes, especially among women in their late reproductive ages, should adopt differential approach across different states/districts in the context their lifestyle, dietary pattern, working pattern and other socio-cultural practices keeping levels of obesity in the central place.
Electronic supplementary material
(PDF 59 kb)
(PDF 73 kb)
Acknowledgements
The authors would like to acknowledge the research co-ordinators in Demographic and Health Surveys (DHS) India that developed the study’s research protocol. We would also like to acknowledge the helpful comments of the anonymous referees.
Abbreviations
- BMI
Body Mass Index
- DBP
Diastolic Blood Pressure
- NCD
Non-Communicable Diseases
- NFHS
National Family Health Survey
- SBP
Systolic Blood Pressure
Author’s contribution
SKS apprehended the idea. PP designed the experiment, analyzed it, interpreted the results, and drafted the manuscript. SKS and SVS supervised the work. Authors take responsibility for the integrity of the work as a whole from inception to the published article. All the authors read and approved the final manuscript.
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability
This study utilizes secondary data from a national survey conducted under the stewardship of the Ministry of Health & Family Welfare, Government of India, with the help of the International Institute for Population Sciences as the nodal agency. The data has been archived in a public repository. Therefore, the data is easily accessible for research purposes.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict/competing interests.
Code availability
Not Applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of Diabetes and Diabetes-Related Complications [Internet]. Vol. 88, Physical Therapy. 2008. p. 1254–64. Available from: https://academic.oup.com/ptj/ptj/article/2858146/Epidemiology. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization. Global report on diabetes: executive summary. Geneva: World Health Organization; 2016.
- 3.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Shridhar G, Rajendra N, Murigendra H, Shridevi P, Prasad M. Modern diet and its impact on human health. J Nutr Food Sci [Internet] 2015;05(06):9–11. [Google Scholar]
- 5.Raha O, Chowdhury S, Dasgupta S, Raychaudhuri P, Sarkar BN, Raju PV, Rao VR. Approaches in type 1 diabetes research: A status report. International journal of diabetes in developing countries. Int J Diabetes Dev C. 2009;29(2):85. [DOI] [PMC free article] [PubMed]
- 6.Min MU, Li-Fa XU, Dong HU, Jing WU, Ming-Jie BA. Dietary patterns and overweight/obesity: a review article. Iran J Public Health. 2017;46(7):869. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5563867/pdf/IJPH-46-869.pdf. [PMC free article] [PubMed]
- 7.Singh SK, Pedgaonkar S, Puri P, Gupta J. Diabetes-free life in India: application of survival function analysis. J Soc Heal Diabetes [Internet] 2018;6:48–55. doi: 10.1055/s-0038-1676192. [DOI] [Google Scholar]
- 8.Arabin B, Stupin JH. Overweight and obesity before, during and after pregnancy. Vol. 74, Geburtshilfe und Frauenheilkunde. 2014. p. 646–55. [DOI] [PMC free article] [PubMed]
- 9.Khadilkar A, Chiplonkar S, Khadilkar V, Kajale N. Changes in body composition in apparently healthy urban Indian women up to 3 years post-partum [Internet]. Indian J Endocr Metab. 2015;19:477. Available from: http://www.ijem.in/text.asp?2015/19/4/477/159032. [DOI] [PMC free article] [PubMed]
- 10.International Institute for Population Sciences. National Family Health Survey (NFHS-4). 2016. Available from: http://rchiips.org/NFHS/NFHS-4Reports/India.pdf. [PubMed]
- 11.Shil A, Puri P, Prakash R. A geospatial analysis of non-communicable disease (NCD) burden in Indian agro-climatic and political regions. J Public Health (Bangkok). 2017.
- 12.Singh SK, Kashyap GC, Puri P. Potential effect of household environment on prevalence of tuberculosis in India: evidence from the recent round of a cross-sectional survey. BMC Pulm Med. 2018;18:66. doi: 10.1186/s12890-018-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anders S, Schroeter C. Diabetes, diet-health behavior, and obesity.pdf. Front Endocrinol. 2015;6(33):1–8. doi: 10.3389/fendo.2015.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Puri P, Khan J, Shil A, Ali M. A cross-sectional study on selected child health outcomes in India : quantifying the spatial variations and identification of the parental risk factors. Sci Rep. 2020:1–15. [DOI] [PMC free article] [PubMed]
- 15.Rutstein S. Steps to construct new DHS Wealth Index. Usaid [Internet]. 2015; Demographi. Available from: https://www.dhsprogram.com/programming/wealthindex/Steps_to_constructing_the_new_DHS_Wealth_Index.pdf%0Ahttp://www.dhsprogram.com/topics/wealth-index/Wealth-Index-Construction.cfm.
- 16.Meshram II, Vardhana V, Rao M, Sudershan Rao V, Laxmaiah A, Polasa K. Regional variation in the prevalence of overweight/obesity, hypertension and diabetes and their correlates among the adult rural population in India. Br J Nutr. 2016;115(7):1265–1272. doi: 10.1017/S0007114516000039. [DOI] [PubMed] [Google Scholar]
- 17.Khan J, Shil A, Prakash R. Exploring the spatial heterogeneity in different doses of vaccination coverage in India. PLoS One [Internet] 2018;13(11):e0207209. doi: 10.1371/journal.pone.0207209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puri P, Singh SK, Srivastava S. Reporting heterogeneity in the measurement of hypertension and diabetes in India. J Public Health. 2020;28(1):23–30. doi: 10.1007/s10389-019-01017-z. [DOI] [Google Scholar]
- 19.Khan J, Mohanty SK. Spatial heterogeneity and correlates of child malnutrition in districts of India. BMC Public Health. 2018;18(1):1–13. doi: 10.1186/s12889-017-4524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh A, Pathak PK, Chauhan RK, Pan W. Infant and child mortality in India in the last two decades: A geospatial analysis. PLoS One. 2011;6(11). [DOI] [PMC free article] [PubMed]
- 21.Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. Australas Med J. 2014;7(1):45–48. doi: 10.4066/AMJ.2014.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gold EB. The timing of the age at which natural menopause occurs. Obstet Gynecol Clin N Am. 2011;38(3):425–440. doi: 10.1016/j.ogc.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt CW. Age at menopause: do chemical exposures play a role? Environ Health Perspect. 2017;125(6):1–5. doi: 10.1289/EHP2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu X, Jones M, Mishra GD. Age at natural menopause and development of chronic conditions and multimorbidity: results from an Australian prospective cohort. Hum Reprod. 2020;35(1):203–211. doi: 10.1093/humrep/dez259. [DOI] [PubMed] [Google Scholar]
- 25.Levine ME, Lu AT, Chen BH, Hernandez DG, Singleton AB, Ferrucci L, Bandinelli S, Salfati E, Manson JAE, Quach A, Kusters CDJ, Kuh D, Wong A, Teschendorff AE, Widschwendter M, Ritz BR, Absher D, Assimes TL, Horvath S. Menopause accelerates biological aging. Proc Natl Acad Sci U S A. 2016;113(33):9327–9332. doi: 10.1073/pnas.1604558113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Slopien R, Wender-Ozegowska E, Rogowicz-Frontczak A, Meczekalski B, Zozulinska-Ziolkiewicz D, Jaremek JD, et al. Menopause and diabetes: EMAS clinical guide. Maturitas [Internet] 2018;117:6–10. doi: 10.1016/j.maturitas.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Government of India. Cause of Death Statistics [Internet]. 2015. Available from: http://censusindia.gov.in/vital_statistics/causesofdeath.html.
- 28.Ramachandran A. Trends in prevalence of diabetes in Asian countries. World J Diabetes [Internet]. 2012;3(6):110. Available from: http://www.wjgnet.com/1948-9358/full/v3/i6/110.htm. [DOI] [PMC free article] [PubMed]
- 29.Kerr EA, Heisler M, Krein SL, Kabeto M, Langa KM, Weir D, Piette JD. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–1640. doi: 10.1007/s11606-007-0313-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tasneem Imam BH. Diabetes prevalence: a comparison between urban and rural areas of Bangladesh. Irjals. 2012;1(4):114–126. [Google Scholar]
- 31.Sifferlin A. Study: Does Eating White Rice Raise Your Risk of Diabetes? | TIME.com [Internet]. TIME. 2012 [cited 2018 Oct 24]. Available from: http://healthland.time.com/2012/03/16/study-does-eating-white-rice-raise-your-risk-of-diabetes/.
- 32.Khalik S. Diabetes: The rice you eat is worse than sugary drinks, Health News & Top Stories - The Straits Times [Internet]. The Straitstimes. 2016 [cited 2018 Oct 24]. Available from: https://www.straitstimes.com/singapore/health/diabetes-the-rice-you-eat-is-worse-than-sugary-drinks.
- 33.Green R, Milner J, Joy EJM, Agrawal S, Dangour AD. Dietary patterns in India: a systematic review. Br J Nutr. 2016;116(1):142–148. doi: 10.1017/S0007114516001598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, Khunti K. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. Br Med J. 2007;334(7588):299–302. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 59 kb)
(PDF 73 kb)
Data Availability Statement
This study utilizes secondary data from a national survey conducted under the stewardship of the Ministry of Health & Family Welfare, Government of India, with the help of the International Institute for Population Sciences as the nodal agency. The data has been archived in a public repository. Therefore, the data is easily accessible for research purposes.