Abstract
Introduction
Monolateral rail fixators are more comfortable to the patients and have a lesser learning curve compared to ring fixators. Guidelines are still lacking for rational use of monolateral fixator for bone transport. This retrospective study aimed to analyze and compare the clinico-radiological outcomes of monolateral fixator in infected non union of tibia based on bone gap quantification.
Materials and Methods
This retrospective study included 35 patients of post traumatic infected osteocutaneous defects of tibia operated from May 2013 to May 2016. Group I having bone gap of 6 cm or less (n = 20) and group II with > 6 cm bone gap (n = 15). The mean age was 29.56 (range 18–62) years in group I and 29.67 (range 20–65) years in group II. The mean bone gap was 4.62 (2–6 cm) in group I and 7.6 cm (6.5–10 cm) in group II (P < 0.00001, Mann–Whitney test). The results were assessed by Association for the Study and Application of the Method of Ilizarov (ASAMI) criteria.
Results
Union was achieved primarily in 90% (n = 18) cases in group I and 73.34% (n = 11) cases in group II. The bone result was excellent, good, fair/poor in 14, 5, 1 in group I; and in 4, 6, 5 in group II, respectively (P = 0.020, Chi-square test). The functional results were excellent, good, fair/poor in 15, 4, 1 in group I; and 5, 8, 2 in group II, respectively (P = 0.0479, Chi-square test).
Conclusion
We recommend use of monolateral fixator in patients with infected diaphyseal non union of tibia with bone gap ≤ 6 cm. Use of monolateral fixator in patients with bone gap > 6 cm is associated with higher incidence of residual problems and complications.
Keywords: Monolateral fixator, Infected nonunion, Tibia, Distraction osteogenesis, ASAMI, Bone gap
Introduction
High energy trauma may lead to severe injuries to bone and soft tissues. Complications like infection, nonunion, bone loss, soft tissue defects and deformity are common with open fractures of tibia. Management of bone and soft tissue defect of tibia is always a surgical challenge requiring various modalities and orthoplastic approach. Various management options like Papineau type cancellous bone grafting, extensive debridement and local soft tissue rotational flaps, tibio-fibular synostosis, packing the defect with antibiotic impregnated beads, bone transport using ring or monolateral fixator etc. are well described in literature to deal with infected nonunion and its complications [1–7]. With use of Ilizarov’s principle of distraction osteogenesis many complications can be dealt simultaneously. Ilizarov ring fixator has proven its efficacy with excellent to good outcomes in 70–90% patients of infected nonunion of tibia [4, 7, 8]. But still there are some problems with ring fixator frames as they can be heavy, cumbersome, long learning curve and may have poor patient acceptance [1, 9–11]. Monolateral rail fixators have been reported to be relatively easier to apply, light weight, less cumbersome to the patient and more surgeon friendly. These are also proven to have better patient compliance when compared to ring fixators [7, 12, 13]. One study in literature suggested poor outcome of rail fixator compared to ring fixator in infected non union of tibia with bone gap > 6 cm [7]. Guidelines are still lacking for rational use of monolateral fixator for bone transport on the basis of bone gap quantification and only few studies in literature are available regarding the same [7, 14]. The present retrospective study aimed to analyze and compare the clinico-radiological outcomes and complications of monolateral fixator in infected non union of tibia based on bone gap quantification.
Materials and Methods
This retrospective study included 35 consecutive patients of post traumatic infected osteocutaneous defects of tibia treated with monolateral fixator, who presented to author’s tertiary level institute between May 2013 and May 2016. The study was approved by institutional review board and ethical committee. The study included all adult patients of post traumatic infected diaphyseal non union of tibia treated with monolateral rail fixator. The patients excluded from study were nonunion of tibia of reason other than trauma (like post tumor surgery, post deformity correction surgery of tibia), pathological fractures, periarticular nonunions at bone ends, non-sensate foot, age extremes (age > 65 years and < 18 years), any medical or skeletal illness affecting bone healing (rickets, osteomalacia, primary or metastatic tumors, osteopetrosis, Paget’s disease, chronic renal disease etc.), and with less than 6 month postoperative follow-up. Total 38 patients were treated with monolateral fixator (Limb Reconstruction System, S.H. Pitkar Orthotools Pvt Ltd, Pune, India). Three patients were excluded from the study, because they did not complete minimum follow-up of 6 months.
The commencement of study was done from January 2019. The data was collected from all clinical notes and radiographs of these patients available from hospital records. The patients were allocated into two groups based on their intraoperative bone gap quantification after radical debridement of necrotic bone. Intraoperative bone gap was measured with the help of measuring scale which was documented in the hospital case file of patient (Fig. 1). Bone gap was also confirmed on radiographs and the magnification in the radiographs was adjusted using diameter of pin shafts as guide. Patients having bone gap of 6 cm or less were counted in group I (n = 20 patients) and those with > 6 cm bone gap were counted in group II (n = 15 patients). The patients with more than 6 cm bone gap have to be treated with individualized protocol and need special attention as these are difficult to manage [7, 15, 16], so 6 cm bone defect (considered as larger defects [15]) was used as cut off value of bone gap for patients allotment in two groups. The Demographic profile of both the groups has been described in Table 1. Operative treatment included removal of any previous implant, exposure of fracture site, radical resection of necrotic or sclerotic bone, opening of medullary canal and soft tissue debridement. The bone ends were debrided till paprika sign became visible on both ends of non union. The final bone gap was measured post debridement. Monolateral fixator frame was applied after debridement of the non union site. Corticotomy was performed depending on the anatomical location of non union site after fixator application. Micobiological and histopathological samples were obtained of the tissue at the non union site. The rail fixation system included on an average of 9 half pins of 6 mm tapered diameter per patient. Single level corticotomy was done in all patients. In one patient of group I acute docking at fracture site was done. The fibular osteotomy or resection was performed wherever needed for deformity correction or acute shortening. Three patients in group I and two patients in group II already had split-skin grafting (SSG)/flap surgery prior to frame application.
Fig. 1.

Intraoperative photograph showing technique of measurement of intraoperative bone gap after radical debridement of bone and soft tissue
Table 1.
Demographic profile and clinical data of the study groups
| Criteria | Group I | Group II | P value |
|---|---|---|---|
| Number of patients (n) | 20 | 15 | |
| Sex | |||
| Male | 16 | 14 | 0.36 (Fisher’s exact test) |
| Female | 4 | 1 | |
| Mean age (years) | 29.56 (range 18–62) | 29.67 (range 20–65) | 0.43 (Mann–Whitney test) |
| Fracture site (tibia) | |||
| Proximal 1/3rd | 3 | 2 | 0.91 (Chi-square test) |
| Middle 1/3rd | 12 | 10 | |
| Distal 1/3rd | 5 | 3 | |
| Initial injury | |||
| Open | 18 | 15 | 0.49 (Fisher’s exact test) |
| Closed | 2 | 0 | |
| Initial treatment | |||
| External fixator | 18 | 15 | 0.49 (Fisher’s exact test) |
| Locking compression plate | 2 | 0 | |
| Active purulent discharge | 12 | 10 | |
| Mean bone gap (cm) | 4.62 (range 2–6) | 7.6 cm (range 6.5–10) | < 0.00001 (Mann–Whitney test) |
| Corticotomy site (tibia) | |||
| Proximal 1/3rd | 16 | 11 | 0.70 (Fisher’s exact test) |
| Distal 1/3rd | 4 | 4 | |
| Mean follow-up period (months) | 32.95 | 37.47 | 0.155 (Mann–Whitney test) |
| Mean time in external fixator (months) | 9.22 | 12.20 | 0.000381 (Mann–Whitney test) |
| External fixator index (months/cm) | 2.14 | 2.06 | 0.80 (Mann–Whitney test) |
| Paley classification [17] | 0.20 (Chi-square test) | ||
| A1 | 5 | 0 | |
| A2 | 0 | 0 | |
| B1 | 7 | 4 | |
| B2 | 6 | 7 | |
| B3 | 2 | 4 | |
Bold values signifies that the p value outcome of respective observation is < 0.05, which means there was statistically significant difference between the two groups with respect to respective observation
Patients were encouraged for active ankle and knee joint motion exercises postoperatively. Partial weight bearing was allowed with walker depending on patient’s compliance and pain tolerance. Postoperatively broad spectrum antibiotics were given for 2–3 days. Antibiotics were changed as per microbiological and culture sensitivity reports of tissue samples collected intraoperatively and continued for 2 weeks. Fixator, pin site and skin care was taught to the patients. Distraction at the corticotomy site was started after 7–9 days postoperatively at 1 mm/day. Monthly follow-up was done postoperatively for assessment of distraction at corticotomy site, formation of regenerate and any other complication.
On each monthly follow-up complications like deformity, shortening, muscle contractures, infection were assessed. Paley’s pin tract infection classification [18] was used for management and grading of pin tract infections. Grade 1 and grade 2 infections were grouped together for statistical analysis and labeled as superficial pin tract infections. Grade 3 infections were labeled as deep pin tract infections. Pin tract infections were managed initially by local care, incision and drainage, and oral antibiotics. Resistant deep pin tract infections were managed by intravenous antibiotics, and pin removal if necessary. Radiographs were assessed for alignment and docking. Fixator adjustment was done whenever necessary under local or regional anaesthesia. Freshening of edges and removal of interposed fibrous tissue was done whenever fixator adjustment was done in regional anaesthesia. After completion of distraction at the corticotomy site and achieving docking at the fracture site, the fixator was locked in static mode, Consolidation of regenerate and union at fracture site was assessed on regular monthly follow-up radiographs. Fixator frame was kept till union was achieved and regenerate had consolidated. Consolidation of regenerate was considered adequate when its radiodensity was comparable to the adjacent normal bone. Union at the fracture site was considered positive if there was presence of three out of four cortexes with bridging trebaculae in two different radiological views (AP and Lateral), no subjective pain on walking and no motion at fracture site on loosening of frame. Dynamisation was done before fixator removal in all patients. Patients were followed for minimum of 6 months after frame removal. Patients were advised to wear a protective below knee poly-vinyl cholride (PVC) brace for 6 months after fixator removal. Association for the Study and Application of the Method of Ilizarov (ASAMI) criteria [4] was used for assessment of bone and functional results (Table 2). External fixator index was calculated by dividing the frame-keeping period in months by the length of the regenerated bone. Statistical analysis of the data was performed using IBM SPSS software version 20. P value < 0.05 was considered statistically significant. Chi-square test and Fisher’s Exact test was used for Qualitative data. Mann–Whitney test used for Quantitative data.
Table 2.
Assessment of bone and functional results using Association for the Study and Application of the Methods of Ilizarov (ASAMI) criteria [4]
| Result | Bone results | Functional results |
|---|---|---|
| Excellent | Union, no infection, deformity < 7°, Limb length discrepancy (LLD) < 2.5 cm | Active, no limp, minimum stiffness (loss of < 15° knee extension/< 15° ankle dorsiflexion), no reflex sympathetic dystrophy (RSD), insignificant pain |
| Good | Union + any two of the following: absence of infection, < 7° deformity, LLD < 2.5 cm | Active with one or two of the following: limp, stiffness RSD, significant pain |
| Fair | Union + any one of the following: absence of infection, < 7° deformity, LLD < 2.5 cm | Active with three or all of the following: limp, stiffness, RSD, significant pain |
| Poor | Non-union/refracture/union + infection + deformity > 7° + LLD > 2.5 cm | Inactive (unemployment or inability to return to daily activities because of injury) |
| Failure | Not applicable | Amputation |
Results
Table 1 describes the clinical difference between the two groups. Fracture united primarily in 18 cases in group I (Fig. 2a–h) and 11 cases in group II (Figs. 3a–c, 4a–c) and after fixator adjustment with freshening of edges in 2 cases each in group I and group II. All corticotomy sites healed in both groups. No patient in both groups had persistent infection at fracture site. Mean gain in bone length was 4.42 cm (range 3–6 cm) in group I and 6.06 cm (range 4–8 cm) in group II (P < 0.00042, Mann–Whitney test). There was statistically significant difference between the two groups in terms of Bone and functional outcomes (Tables 3, 4). Complications in each group are depicted in Table 5. Three patients in group I and two patients in group II already had split-skin grafting (SSG)/flap surgery prior to frame application. These surgeries did not affect the final outcome of these patients compared to other patients. The bone result was excellent, good, fair/poor in 14, 5, 1 in group I; and in 4, 6, 5 in group II, respectively (P = 0.020, Chi-square test). The functional results were excellent, good, fair/poor in 15, 4, 1 in group I; and 5, 8, 2 in group II, respectively (P = 0.0479, Chi-square test, Table 3).
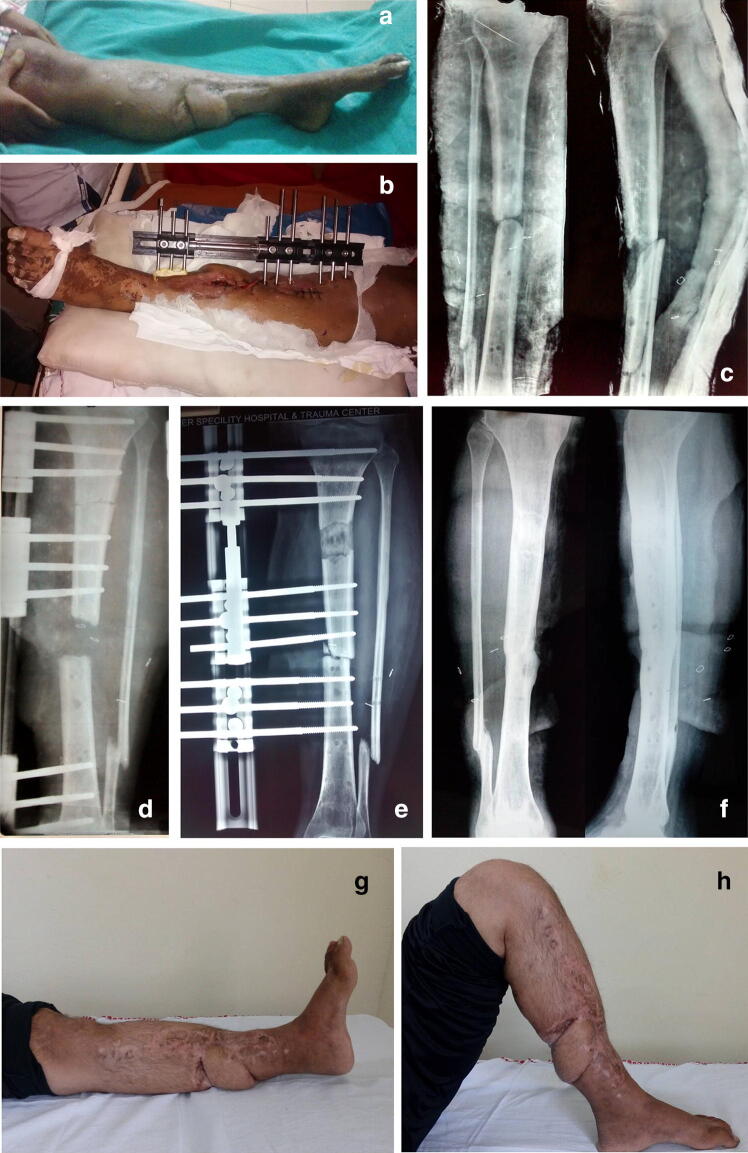
Fig. 2.
a Clinical photograph of 20-year-old male at the time of presentation showing already done flap and eqinus. b Immediate post operative clinical picture showing monolateral fixator in situ with proximal corticotomy suture line between proximal and middle clamp. c Anteroposterior and lateral radiograph of the same patient. d Immediate postoperative radiograph showing 3 cm bone gap and proximal corticotomy. e Five month follow-up radiograph showing good quality of regenerate. f Three year follow-up radiographs showing union at fracture site and consolidation of regenerate. g, h Clinical photographs of the same patient showing good range of motion at knee and ankle. Patient had excellent bony outcome and good functional outcome according to ASAMI criteria
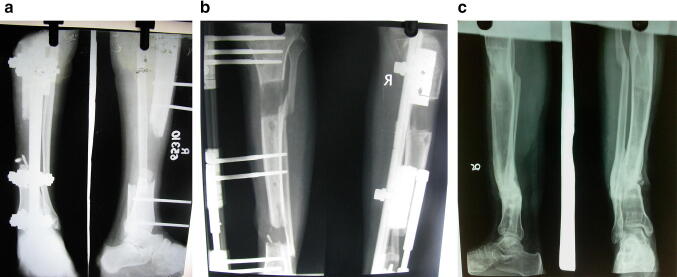
Fig. 3.
a Anteroposterior and lateral radiographs of 24-year-old male patient at the time of presentation showing 7 cm bone gap with external fixator in situ. b Three month follow-up anteroposterior and lateral radiographs showing bone transport. c Two year follow-up radiographs showing union at fracture site and consolidation of regenerate. Patient had excellent bony outcome and good functional outcome according to ASAMI criteria
Fig. 4.
a Anteroposterior and lateral radiographs of 25-year-old male patient at the time of presentation showing severe comminution of tibial diaphysis with external fixator in situ. b Immediate postoperative anteroposterior and lateral radiographs of same patient showing 9 cm bone gap with distal corticotomy. c Two year follow-up radiographs showing union at fracture site and consolidation of regenerate. Patient had 3 cm LLD with infection and had fair bony outcome and good functional outcome according to ASAMI criteria
Table 3.
Bone and functional results in ASAMI score
| Groups | Bone results | Functional results | Total | ||||
|---|---|---|---|---|---|---|---|
| Excellent | Good | Fair/poor | Excellent | Good | Fair/poor | ||
| Group I | 14 | 5 | 1 | 15 | 4 | 1 | 20 |
| Group II | 4 | 6 | 5 | 5 | 8 | 2 | 15 |
| P value (Chi-square test) | 0.020 | 0.0479 | – | ||||
Bold values signifies that the p value outcome of respective observation is < 0.05, which means there was statistically significant difference between the two groups with respect to respective observation
Table 4.
Comparison of residual problems between two study groups
| Groups | Group I (6 cm and less bone gap) | Group II (> 6 cm bone gap) | P value (Fisher’s exact test) |
|---|---|---|---|
| Number of patients (n) | |||
| Bone result criteria | 20 | 15 | |
| Infection | 5 | 7 | 0.282 |
| Deformity (> 7°) | 1 | 3 | 0.292 |
| Limb length discrepancy (LLD) > 2.5 cm | 0 | 6 | 0.0031 |
| Total number of patients with residual infection, deformity, LLD | 6 | 11 | 0.017 |
| Functional result criteria | |||
| Limp | 1 | 9 | 0.0006 |
| Knee stiffness (loss of > 15° knee extension) or ankle stiffness (loss of > 15° ankle dorsiflexion) | 4 (ankle stiffness) | 7 (ankle stiffness) | 0.144 |
| 2 (knee stiffness) | 2 (knee stiffness) | 1 | |
| Significant pain | 0 | 0 | NA |
| Reflex sympathetic dystrophy (RSD) | 1 | 0 | 1 |
| Total number of patients with residual problems as per ASAMI function criteria | 5 | 10 | 0.0192 |
Bold values signifies that the p value outcome of respective observation is < 0.05, which means there was statistically significant difference between the two groups with respect to respective observation
Table 5.
Complications
| Complication | Group I | Group II |
|---|---|---|
| Superficial pin tract infection | 8 | 10 |
| Deep pin tract infection | 5 | 7 |
| Fixator frame adjustment | 2 | 2 |
| Septic loosening of fixator | 0 | 1 |
| Aseptic loosening of fixator | 0 | 1 |
| Excessive sin tensioning | 0 | 1 |
| Refracture | 1 | 0 |
| Spontaneous Ankle Ankylosis | 1 | 0 |
| Corticotomy site infection | 0 | 1 |
Discussion
Long bone non union is associated with complications like diffuse osteopaenia, functional incompetence of the limb, muscular hypotrophy, damage to soft tissues, infection and joint stiffness [5, 9, 17]. Management of all these complications is not usually possible with a single surgical intervention and multiple procedures are needed to be performed for achieving a functional limb free from infection [18]. Distraction histiogenesis has been used to bridge both osseous and soft tissue defects without the need for ancillary bone grafting and soft tissue coverage [19]. Bone transport can be done with many devices like ring fixators, monolateral fixators or intramedullary nail system. The mono-lateral external fixator is a simple, unilateral assembly with excellent rigidity. It is better tolerated by the patient, easier to apply and light weight [20]. Both ring as well as monolateral fixators have shown satisfactory outcomes in treatment of infected nonunion of tibia [3, 4, 7, 8, 21–24]. Very few studies in literature [7, 14] have assessed monolateral fixator’s outcomes in management of infected nonunion of long bones on the basis of bone gap quantification. The present retrospective study aimed to analyze and compare the outcomes of monolateral fixator in infected non union of tibia based on bone gap quantification.
Union along with infection free bone capable of maximum functional use is the ultimate goal of treatment in infected non-union [1]. We were able to eradicate infection at fracture site in all patients because of radical resection of dead bone. A thorough debridement to vascularized, living tissue seems necessary, even when using Ilizarov technique [4, 9, 10, 17, 19, 25]. Rail fixators in the present study were able to treat infected nonunion of tibia successfully. Union was achieved primarily in 90% (n = 18) patients in group I and 73.34% (n = 11) patients in group II. One more procedure of fixator adjustment, removal of interposed soft tissue and freshening of bone ends resulted in union in two patients each in both the groups. However, no patient required bone grafting in the present study. Ajmera et al. [24] reported need of grafting in 8% of patients in his series and Harshwal et al. [23] reported need of additional Bone grafting at docking site in 5.4% patient in his series. Mudiganty et al. [26] did primary bone grafting in 12.5% patients and no secondary grafting. Rohilla et al. [7] reported no need of bone grafting in their study patients. Early freshening of edges and removal of interposed fibrous tissue with frame adjustment is helpful in achieving union early and decreasing the fixator index. This method is also used and advocated in literature [7, 27].
Pin tract infection was the most common complication in both the study groups with superficial infection more common than deep infection. Other studies in literature also had pin tract infection as the most common complication [7, 23, 24, 26]. Incidence of knee stiffness was comparable in both groups. The incidence of ankle stiffness was higher in group II but not statistically significant. Limb length discrepancy (LLD) at final follow-up of > 2.5 cm was found to be different in both groups with statistical significance (P = 0.0031, Fisher’s Exact test). This might be because of larger bone gap and higher fixator duration in group II compared to group I. Mudiganty et al. [26] reported LLD of > 2.5 cm in 25% patients at final follow-up of their case series.
Outcomes of present study are comparable to other studies reported in literature (Table 6) [7, 22–24, 26]. As per the ASAMI bone result criteria more patients in group II (11 patients, 73.34%) had residual problems as compared to 6 patients (30%) in group I (P = 0.017, Fisher’s Exact test) (Table 4). Similarly, as per ASAMI functional results criteria more patients in group II (10 patients, 66.67%) had some form of functional loss compared to 5 patients (25%) in group I (P = 0.0192, Fisher’s Exact test) (Table 4). According to ASAMI scoring criteria [4] the evaluated results showed a statistically significant difference in functional and bone results between the two groups based on bone gap quantification. We observed that patients in group II (bone gap > 6 cm) had more residual problems and complications as compared to patients in group I (6 cm or less) indicating better outcomes in group I (Table 4). We advocate use of monolateral fixator in patients with bone gap 6 cm and less, and rational use of this technique of fixation in patients having bone gap higher than 6 cm with caution. Bone gap > 6 cm are considered to be larger bone defects which require subjective management.
Table 6.
Bone and Functional result comparison with other studies in literature
| S. no. | Name of study | Number of patients | Excellent result (%) | Good result (%) | Fair/poor result (%) | |||
|---|---|---|---|---|---|---|---|---|
| Bone results | Functional results | Bone results | Functional results | Bone results | Functional results | |||
| 1. | Harshwal et al. [19] | 37 | 65 | 73 | 24 | 16 | 11 | 11 |
| 2. | Ajmera et al. [20] | 30 | 76 | 84 | 12 | 8 | 12 | 8 |
| 3. | Patil [18] | 54 | 67 | 80 | 25 | 13 | 8 | 7 |
| 4. | Mudiganty [22] | 40 | 57.5 | 32.5 | 40 | 65 | 2.5 | 2.5 |
| 5. | Rohilla et al. [7] (6 cm and less bone gap monolateral fixator group) | 24 | 50 | 75 | 45.8 | 20.8 | 4.2 | 4.2 |
| 6. | Rohilla et al. [7] (> 6 cm bone gap monolateral fixator group) | 11 | 18.18 | 36.36 | 36.36 | 45.45 | 45.46 | 18.19 |
| 7. | Present study group I (6 cm and less bone gap) | 20 | 70 | 75 | 25 | 20 | 5 | 5 |
| 8. | Present study group II (> 6 cm bone gap) | 15 | 26 | 33.34 | 40 | 53.34 | 33 | 13.32 |
A limitation of present study is retrospective nature and small number of patients in each group. A larger prospective randomised study with higher number of patient can better evaluate results statistically. However, such injuries are not very frequent in occurrence, limiting the inclusion of higher number of patients in the study. This is the first study in English literature focusing on importance of bone gap in use of monolateral fixators. Our results are comparable to other studies done in literature with similar objectives [7, 14]. Statistically proven results are the strength of the study.
Conclusion
Monolateral fixator proved to be successful method in the management of infected nonunion of tibia. We recommend use of monolateral fixator in patients with infected diaphyseal non unions of tibia with bone gap ≤ 6 cm. In bone gaps > 6 cm, use of monolateral fixators is associated with higher incidence of residual problems and complications. Hence the other modalities of treatment like ring fixator may have better outcomes.
Acknowledgements
No financial support was taken from any organization for this study.
Author Contributions
Manuscript has been read and approved by all the authors. We declare that manuscript represent honest work conducted at our tertiary care institute. We also declare that manuscript has not been sent to any other Journal for consideration for publication. Dr JW: collection of data, preparation of manuscript, operating surgeon. Dr RR: compilation of data, operating surgeon. Dr RS: writing of manuscript, operating surgeon. Dr RS: data analysis, writing of manuscript. Dr AD: compilation of data, writing of manuscript. Dr SV: collection of data, manuscript preparation, data analysis.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Ethical and human considerations
All procedures performed in this study were in accordance with the ethical standards of institution and with the 1964 Helsinki declaration and its later amendements. Ethical clearance was taken from the local ethical committee. Informed consent was obtained from all patients included in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jitendra Wadhwani, Email: drjitendra28.03@gmail.com.
Rajesh Rohilla, Email: drrajeshrohilla@rediffmail.com.
Ramchander Siwach, Email: rcsiwach.bps@gmail.com.
Roop Singh, Email: drroopsingh@rediffmail.com.
Ashish Devgan, Email: ashishdevgan@gmail.com.
Sumedha Vashishth, Email: summivashishth@gmail.com.
References
- 1.Keating JF, et al. The management of fractures with bone loss. Journal of Bone and Joint Surgery (British Volume) 2005;87-B:142–150. doi: 10.1302/0301-620X.87B2.15874. [DOI] [PubMed] [Google Scholar]
- 2.Baruah RK. Ilizarov methodology for infected non union of the tibia: Classic circular transfixion wire assembly vs. hybrid assembly. Indian Journal of Orthopaedics. 2007;41(3):198–203. doi: 10.4103/0019-5413.33682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farmanullah, et al. Evaluation of management of tibial non-union defect with Ilizarov fixator. Journal of Ayub Medical College Abbottabad. 2007;19(3):34–36. [PubMed] [Google Scholar]
- 4.Maini L, et al. The Ilizarov method in infected nonunion of fractures. Injury. 2000;31:509–517. doi: 10.1016/S0020-1383(00)00036-X. [DOI] [PubMed] [Google Scholar]
- 5.Jain AK, Sinha S. Infected nonunion of the long bones. Clinical Orthopaedics and Related Research. 2005;431:57–65. doi: 10.1097/01.blo.0000152868.29134.92. [DOI] [PubMed] [Google Scholar]
- 6.Wu CC. Single-stage surgical treatment of infected nonunion of the distal tibia. Journal of Orthopaedic Trauma. 2011;25(3):156–161. doi: 10.1097/BOT.0b013e3181eaaa35. [DOI] [PubMed] [Google Scholar]
- 7.Rohilla R, et al. Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Joint Journal. 2016;98-B:1399–1405. doi: 10.1302/0301-620X.98B10.37946. [DOI] [PubMed] [Google Scholar]
- 8.Yin P, et al. The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthopaedica Belgica. 2014;80:426–435. [PubMed] [Google Scholar]
- 9.Kanellopoulos AD, Soucacos PN. Management of nonunion with distraction osteogenesis. Injury. 2006;37S:S51–S55. doi: 10.1016/j.injury.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 10.Ring D, et al. Infected nonunion of the tibia. Clinical Orthopaedics and Related Research. 1999;369:302–311. doi: 10.1097/00003086-199912000-00032. [DOI] [PubMed] [Google Scholar]
- 11.Megas P, et al. The treatment of infected nonunion of the tibia following intramedullary nailing by the Ilizarov method. Injury. 2010;41:294–299. doi: 10.1016/j.injury.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 12.Seenappa HK, et al. Management of complex long bone nonunions using limb reconstruction system. Indian Journal of Orthopaedics. 2013;47:602–607. doi: 10.4103/0019-5413.121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Rosasy MA. Acute shortening and re-lengthening in the management of bone and soft tissue loss in complicated fractures of shaft tibia. Journal of Bone and Joint Surgery. 2007;89:80–88. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 14.Pal CP, et al. Comparative study of the results of compound tibial shaft fractures treated by Ilizarov ring fixators and limb reconstruction system fixators. Chinese Journal of Traumatology. 2015;18(6):347–351. doi: 10.1016/j.cjtee.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Keating J, et al. The management of fractures with bone loss. Journal of Bone and Joint Surgery (British Volume) 2005;87:142–150. doi: 10.1302/0301-620X.87B2.15874. [DOI] [PubMed] [Google Scholar]
- 16.Dagher F, Roukoz S. Compound tibial fractures with bone loss treated by the Ilizarov technique. Journal of Bone and Joint Surgery (British Volume) 1991;73(2):316–321. doi: 10.1302/0301-620X.73B2.2005164. [DOI] [PubMed] [Google Scholar]
- 17.Paley D, et al. Ilizarov treatment of tibial nonunions with bone loss. Clinical Orthopaedics and Related Research. 1989;241:146–165. [PubMed] [Google Scholar]
- 18.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clinical Orthopaedics and Related Research. 1990;250:81–104. [PubMed] [Google Scholar]
- 19.Toh CL, Jupiter JB. Infected nonunion of the tibia. Clinical Orthopaedics and Related Research. 1995;315:176–191. [PubMed] [Google Scholar]
- 20.Eralp L, et al. A review of problems, obstacles and sequelae encountered during femoral lengthening: Uniplanar versus circular external fixator. Acta Orthopaedica Belgica. 2010;76:628–635. [PubMed] [Google Scholar]
- 21.Chaddha M, et al. Management of massive posttraumatic bone defects in the lower limb with the Ilizarov technique. Acta Orthopaedica Belgica. 2010;76:811–820. [PubMed] [Google Scholar]
- 22.Patil S, Montgomery R. Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implications. Journal of Bone and Joint Surgery (British Volume) 2006;88-B:928–932. doi: 10.1302/0301-620X.88B7.17639. [DOI] [PubMed] [Google Scholar]
- 23.Harshwal RK, et al. Management of nonunion of lower extremity long bones using mono-lateral external fixator: Report of 37 cases. Injury. 2014;45(3):560–567. doi: 10.1016/j.injury.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Ajmera A, et al. Outcome of limb reconstruction system in open tibial diaphyseal fractures. Indian Journal of Orthopaedics. 2015;49:429–435. doi: 10.4103/0019-5413.159638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El-Rosasy MA. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. Journal of Bone and Joint Surgery (British Volume) 2007;89-B:80–88. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 26.Mudiganty S, et al. Treatment of infected nonunion with segmental defects with a rail fixation system. Strategies in Trauma and Limb Reconstruction. 2017;12(1):45–51. doi: 10.1007/s11751-017-0278-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iacobellis C, et al. Bone transport using the Ilizarov method: A review of complications in 100 consecutive cases. Strategies in Trauma and Limb Reconstruction. 2010;5:17–22. doi: 10.1007/s11751-010-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]