Abstract
Purpose
Type 2 diabetes requires patients to make lifestyle changes and perform daily self-care. To determine at what stages patients may need particular self-management support, we examined (1) whether patients’ performance of self-care related to their diabetes duration, and (2) whether illness characteristics (treatment and complications) and diabetes-related distress influenced this relationship.
Methods
Cross-sectional data from 590 type 2 diabetes patients were analysed through linear and logistic regression analysis. Self-care behaviours were assessed by the revised Summary of Diabetes Self-Care Activities (SDSCA) measure. Diabetes duration (model 1), treatment and complications (model 2), and distress, as assessed by the Problem Areas In Diabetes (PAID) scale (model 3), were stepwise included. Sociodemographic characteristics were added to all models to account for confounding.
Results
Patients with a longer history of diabetes were less physically active, but monitored their blood glucose levels more frequently than more recently diagnosed patients. These relationships were mediated by the presence of complications and the use of insulin, with lower levels of physical activity being found among patients with macrovascular complications and higher frequencies of glucose monitoring among patients on insulin. All predictors together explained maximally 5% of the variance in self-care, except for glucose monitoring (37%) and smoking (11%).
Conclusion
Type 2 diabetes patients’ self-care activity changes over the course of illness. To provide tailored self-management support, diabetes care providers should take into account patients’ phase of illness, including their treatment and complications, as well as their personal characteristics and distress level.
Keywords: Diabetes mellitus type 2, Self-care, Diabetes duration, Complications, Distress
Introduction
A healthy lifestyle and adequate self-care are considered key elements of good-quality care for type 2 diabetes mellitus. Currently, more than 380 million individuals worldwide are diagnosed with type 2 diabetes [1], which’s complications can have a major impact of the lives of patients as well as health care systems [1–5]. Physical exercise and a healthy diet have been proven effective in reducing the risk of these micro- and macrovascular complications. This also holds for regular foot and glucose checks to monitor and detect risk factors and symptoms of these complications [6]. For these reasons, medical doctors and nurses invest a lot of time in supporting patients with type 2 diabetes with self-care and making lifestyle changes. In recent years, the importance of tailoring this support to the specific needs of patients has been emphasised [7, 8], as research has shown that patients’ performance of self-care differs according to their sociodemographic and clinical characteristics, such as their age [9] and socioeconomic position [9, 10], as well as the presence of physical and mental health comorbidities [9, 11–13]. As patients’ personal characteristics and circumstances as well as their diabetes change over time, the health behaviours they (need to) perform are also likely to change and, consequently, their need for support. However, until now, diabetes self-management support programmes pay little attention to specific support needs and challenges that may arise in different phases in the illness process. Obtaining more insight into patients’ self-care behaviours over the course of illness could help determine at what stages of type 2 diabetes specific or additional support is needed. Therefore, we aimed to examine patients’ lifestyle and diabetes self-care behaviours in relation to their illness duration.
Regarding the relationship between illness duration and lifestyle and self-care behaviours, we did not formulate a priori hypotheses, as we found that previous studies show inconclusive results. Some research suggests that adherence to lifestyle and self-care recommendations may improve over time, as patients with a longer illness duration are expected to have grown more accustomed to living with diabetes and its management over the years [14]. Patients with a longer illness duration are also more likely to need insulin therapy and to experience complications, both of which may cause patients to perceive their condition as more serious and consequently to attach greater value to adherence to lifestyle and self-care recommendations [15–18]. Conversely, several studies have shown a longer duration of diabetes to be associated with poor glycaemic control [9, 19] and worse self-care [19]. Pharmacological treatment, and insulin therapy in particular, may negatively impact patients’ perceptions of the need to exercise and adhere to a healthy diet to control glucose levels. Sasi and colleagues have also suggested that the progressive nature of type 2 diabetes may be (partially) responsible for the worse self-care behaviours that they noticed in patients with a longer illness duration, as treatment regimens often become more intensive and complicated over time and thus more challenging for patients. In addition, experiencing complications could have a detrimental effect on adherence to lifestyle and self-care recommendations, as the physical discomfort caused by complications could interfere with physical activity and other health behaviours [19]. Besides, diabetes-related distress may play a role in the relationship between illness duration and self-care, as patients’ level of distress was found to increase with increased illness duration [20], and diabetes-related distress has been shown to both negatively [21] and positively [18] associate with engagement in self-care. Finally, adherence to diabetes self-care recommendations has been reported to differ dependent on the type of self-care activity at stake, suggesting that adequate performance of a specific self-care activity does not guarantee adequate performance of other self-care activities as well [22]. Hence, the objectives of our study were to gain more insight in whether the performance of various self-care behaviours by patients with type 2 diabetes relate to their illness duration (time since diagnosis), and whether certain diabetes-related characteristics, such as diabetes treatment and complications, and the level of diabetes-related distress impact on these relationships.
Methods
Design and setting
The design of the study was cross-sectional and used the baseline (pre-intervention) measurements from three randomized controlled trials (RCTs) of the Dutch Diacourse study. The Diacourse study was approved by the Medical Ethical Committee of the VU University Medical Center Amsterdam. In the Diacourse study, three self-management intervention programs were developed and tested for patients with type 2 diabetes at different stages of illness: 1. an interactive group-based course for patients with a diabetes duration between one and three years (‘short duration’; SD), 2. a peer support intervention for patients diagnosed more than three years ago (‘longer duration’, LD) and 3. a nurse-led individual intervention for patients who had recently had a first Acute Coronary Event (‘Diabetes and ACE’; DA) [23–25] (see the study protocols for more details). Between October 2011 and August 2013, SD and LD patients were recruited from 134 general practices (GP’s) in six regions in the Netherlands and DA patients were recruited from 13 hospitals distributed across the country.
Apart from being diagnosed with type 2 diabetes, the inclusion criteria for the SD sample were age of 18 to 85 years and an illness duration (since diagnosis) of minimally one and maximally three years. For the LD sample patients had to be aged 50 to 70 years and diagnosed with type 2 diabetes more than three years prior to inclusion. The inclusion criteria for the DA sample were age older than 35 years, a diabetes duration (since diagnosis) of at least one year and being recently (< three weeks) discharged from the hospital because of a first acute coronary event. The exclusion criteria for all three samples were not being able to sufficiently speak, read and/or understand the Dutch language and having insufficient mental or intellectual capabilities to participate in the study. For the SD and LD samples, patients were also excluded if they were receiving treatment for severe psychological or psychiatric conditions or if they were recently diagnosed with a life-threatening condition (e.g., cancer or stroke).
Measurements
Eligible patients were invited to participate in the study by their general practitioner (SD, LD) or cardiologist (DA), who provided them with written information. Patients who gave informed consent received a paper questionnaire which included questions about self-care and diabetes distress, as well as diabetes-related and sociodemographic characteristics, several weeks prior to participation in one of the three support programmes of the Diacourse study. Data from this first pre-intervention survey were analysed for the purpose of this study.
Self-care
Self-care was assessed using the Dutch version of the revised Summary of Diabetes Self-Care Activities (SDSCA) measure [26]. This instrument focuses on six aspects of diabetes self-care: exercise, glucose monitoring, foot care, general diet, specific diet and smoking. With the exception of smoking, all behaviours were assessed with two questions, which included asking the number of days on which these activities were performed during the past week (response options: 0 to 7 days). Smoking behaviour was assessed with one question, which asked whether the participant had smoked during the past week (response options: yes or no). The revised SDSCA has been validated against other measures of diet and exercise and has shown adequate internal consistency and test-retest reliability [26]. In our study, the Cronbach’s alphas of the scales were all above .70, except for the specific diet scale. Therefore, we analysed the two items from this scale (intake of the recommended servings of fruit/vegetables and of a low-fat diet) separately, as suggested by Toobert and colleagues [26].
Diabetes duration
Diabetes duration (at the time of the survey) was calculated from the date of diagnosis reported by the participants (LD, DA) or retrieved from the patients’ medical records (SD).
Diabetes-related characteristics
To assess the presence of microvascular complications, participants in the SD and LD studies reported whether they suffered from 1) eye problems, 2) kidney problems, 3) neurological problems, or 4) foot problems, as a result of their diabetes (response options: yes or no). The presence of macrovascular complications was assessed by asking the participants in these studies to indicate whether they suffered from cardiovascular disease. As it was impossible to determine whether the reported macrovascular conditions were related to the participants’ diabetes, we decided to treat all reported macrovascular conditions as complications of diabetes in this study. In the DA study, all participants had a macrovascular complication (ACE). The presence of microvascular complications in this study was derived from hospital records.
Type of diabetes treatment (lifestyle advice only, oral hypoglycaemic agents only or insulin) and the presence of comorbid conditions (e.g., cancer, respiratory problems, joint conditions or ‘other’) were self-reported by the participants in the SD and LD studies and derived from hospital records in the DA study.
Diabetes-related distress
To assess diabetes-related distress, we included the Dutch version of the Problems Areas in Diabetes (PAID) scale [27]. This scale consists of 20 items with five response options, ranging from 0 (no problem) to 4 (serious problem). The scores are summed and transformed to a total score ranging between 0 and 100, with higher scores indicating greater diabetes-related distress. The PAID scale was found to have strong concurrent and discriminant validity [28].
Sociodemographic characteristics
Age, gender, education level and living with or without a partner were self-reported by the participants. Education level was categorized into low (primary school, low general secondary education, preparatory or low vocational education), mid (intermediate or advanced general secondary education or intermediate vocational education), and high (high vocational education or college).
Statistical analyses
Descriptive statistics were calculated for the total population and separately for the three samples. For normally distributed continuous variables, we calculated the means with standard deviations (SDs), and for non-normally distributed variables, we calculated the medians with interquartile ranges (IQRs). One-way analyses of variance with post hoc Bonferroni tests were used to examine differences in exercising, glucose testing, foot care and diet between the three study samples. Differences in smoking behaviour were tested using chi-square tests.
To examine whether participants’ self-care behaviours were related to their illness duration, we conducted a separate regression analysis for each of the self-care behaviours. These were all linear regression analyses, except for smoking behaviour, which was analysed using logistic regression analysis. In all regression analyses, self-care behaviour was the dependent variable. We estimated a first model that included diabetes duration in years and diabetes duration in years squared (to account for potential non-linear effects) as independent variables (model 1). To examine whether the presence of micro- or macrovascular complications and the type of diabetes treatment mediated the relationship between illness duration and self-care, we added these variables to a second model (model 2). To examine the potential mediating role of distress, we analysed a third model with diabetes-related distress added as an independent variable (model 3). In all three models, we included participants’ gender, age, education level and the presence of comorbid conditions as independent variables to adjust for their potential confounding effects. All analyses were performed using SPSS (version 18.0).
Results
Characteristics of the study sample
The total sample of the three Diacourse studies consisted of 622 persons, 32 of whom had to be excluded because of missing data on the key variables of this study (diabetes duration and self-care), leaving data from 590 participants for analysis. The mean age of these participants was 64 years, and two thirds (64%) were male (Table 1). The median diabetes duration was almost six years. The majority used diabetes medication, either oral hypoglycaemic agents (60%) or insulin (24%). Almost half suffered from comorbid conditions (49%), with joint problems being most prevalent (28%). Microvascular complications were present in a third of the study sample, with foot problems (14%) and eye problems (12%) being most prevalent. Macrovascular complications were present in 45% of the participants.
Table 1.
Sociodemographic characteristics, illness-related characteristics and self-care behaviours of the total study sample and the separate SD, LD and DA samples
| Total sample N = 590 |
SD sample N = 180 |
LD sample N = 224 |
DA sample N = 186 |
|
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Gender: % male | 63.6 | 57.2 | 60.7 | 73.1 |
| Age, in years: mean (SD) | 64.2 (8.4) | 63.8 | 63.6 | 65.4 |
| Living with a partner: % | 78.4 | 75.1 | 83.9 | 74.7 |
| Education level: % | ||||
| Low | 31.2 | 29.5 | 22.9 | 42.9 |
| Mid | 47.4 | 48.0 | 49.8 | 44.0 |
| High | 21.4 | 22.5 | 27.4 | 13.0 |
| Illness-related characteristics | ||||
| Diabetes duration, in years: median (IQR) | 5.9 (2.6–12.3) | 2.3 (1.8–3.0) | 9.5 (6.5–14.5) | 7.8 (3.7–14.3) |
| Treatment: | ||||
| Oral hypoglycaemics: % | 60.2 | 65.2 | 58.5 | 57.5 |
| Insulin: % | 23.6 | 2.2 | 32.1 | 33.9 |
| Presence of microvascular complications: % | 33.3 | 21.7 | 49.1 | 25.3 |
| Presence of macrovascular complications: % | 44.7 | 21.1 | 16.7 | 100 |
| Presence of comorbid conditions: % | 48.5 | 54.3 | 53.8 | 36.6 |
| Diabetes distress (0–100): median (IQR) | 7.5 (2.5–17.8) | 6.3 (1.3–15.9) | 9.4 (2.5–21.3) | 5.0 (1.3–16.3) |
| Self-care | ||||
| No. of days physical exercise: mean (SD) | 3.83 (2.17) | 4.42 (1.90) | 4.08 (1.97) | 2.96 (2.38) |
| No. of days glucose monitoring: mean (SD) | 1.45 (2.35) | 0.43 (1.18) | 1.70 (2.50) | 2.15 (2.67) |
| No. of days foot care: mean (SD) | 1.51 (2.10) | 1.22 (1.92) | 1.57 (2.15) | 1.74 (2.18) |
| No. of days healthy diet-general: mean (SD) | 4.86 (1.92) | 5.14 (1.70) | 4.78 (1.82) | 4.68 (2.20) |
| No. of days sufficient fruit/vegetables intake: mean (SD) | 5.37 (1.97) | 5.38 (1.95) | 5.56 (1.78) | 5.13 (2.17) |
| No of days low-fat diet: mean (SD) | 4.60 (2.15) | 4.74 (2.16) | 4.69 (2.00) | 4.36 (2.32) |
| Non-smoking: % | 85.1 | 81.3 | 85.9 | 87.8 |
On average, the participants reported having been physically active for a little less than four days per week. Significant differences between the three samples existed in this respect (F(2,575) = 24.26, p < .001), with the participants of the DA sample being significantly less active (M = 2.96) than the participants of the SD sample (M = 4.42). Glucose monitoring and foot care were performed for an average of one to two days (M = 1.5) per week. The frequency of foot care did not statistically differ between the three samples, but glucose monitoring did (F(2, 575) = 27.92, p < .001): the SD participants reported fewer days of glucose self-monitoring (M = 0.43) than the LD participants (M = 1.70) and the DA participants (M = 2.15). Recommendations for a healthy diet were followed for approximately five days per week, and the majority of the participants indicated to not have smoked during the previous week. No differences existed between the three samples regarding these behaviours.
Effects of diabetes duration, diabetes-related characteristics and distress on self-care
Tables 2, 3 and 4 show that diabetes duration was significantly associated with the number of days participants reported to be exercising and self-monitoring their glucose levels, but not with the number of days they performed foot care, ate a healthy diet or smoked.
Table 2.
Effects of diabetes duration, diabetes-related characteristics and distress on exercising, glucose self-monitoring and foot care; results of linear regression analyses: standardized regression coefficients (β) and explained variance (adjusted R2)†
| Exercising (N = 558) | Glucose self-monitoring (N = 558) | Foot care (N = 559) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| β | β | β | β | β | β | β | β | β | |
| Diabetes duration | |||||||||
| In years | −.308** | −.229* | −.228* | .683*** | .260** | .257** | .190 | .019 | .016 |
| In years squared | .281** | .237* | .234* | −.319** | −.095 | −.090 | −.092 | .000 | .005 |
| Diabetes-related characteristics | |||||||||
| Oral hypoglycaemics | −.111 | −.110 | −.045 | −.046 | .011 | .009 | |||
| Insulin | −.115 | −.112 | .459*** | .451*** | .088 | .081 | |||
| Microvascular complications | −.006 | −.002 | .050 | .042 | .197*** | .189*** | |||
| Macrovascular complications | −.182*** | −.183*** | .055 | .056 | .069 | .070 | |||
| Diabetes-related distress | −.027 | .063 | .056 | ||||||
| Adjusted R2 | .017* | .051*** | .050*** | .168*** | .367*** | .370*** | .009 | .048*** | .049*** |
† All analyses adjusted for age, gender, education level and the presence of comorbid conditions
*Significant at .05 level, ** Significant at .01 level, *** Significant at .001 level
Table 3.
Effects of diabetes duration, diabetes-related characteristics and distress on adhering to recommendations of a healthy diet; results of linear regression analyses: standardized regression coefficients (β) and explained variance (adjusted R2)†
| Healthy diet-general (N = 553) | Fruit/vegetables intake (N = 551) | Low-fat intake (N = 554) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| β | β | β | β | β | β | β | β | β | |
| Diabetes duration | |||||||||
| In years | −.110 | −.012 | −.008 | .027 | .133 | .136 | −.054 | −.042 | −.041 |
| In years squared | .148 | .092 | .086 | .030 | −.028 | −.032 | −.019 | −.026 | −.026 |
| Diabetes-related characteristics | |||||||||
| Oral hypoglycaemics | −.095 | −.093 | −.039 | −.038 | .008 | .008 | |||
| Insulin | −.099 | −.090 | −.071 | −.065 | −.056 | −.055 | |||
| Microvascular complications | −.104* | −.095* | −.108* | −.102* | .064 | .065 | |||
| Macrovascular complications | −.039 | −.040 | −.077 | −.078 | .033 | .033 | |||
| Diabetes-related distress | −.069 | −.048 | −.006 | ||||||
| Adjusted R2 | .001 | .011 | .014 | .004 | .016* | .016* | .017* | .016* | .015 |
† All analyses adjusted for age, gender, education level and comorbid conditions
*Significant at .05 level, ** Significant at .01 level, *** Significant at .001 level
Table 4.
Effects of diabetes duration, diabetes-related characteristics and distress on smoking behaviour; results of logistic regression analyses: odds ratios (OR) with 95%-confidence intervals (95%-CI) and explained variance (Nagelkerke R2)†
| Non-smoking (versus smoking) (N = 556) | |||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Diabetes duration | |||
| In years | 1.009 (0.889–1.145) | 1.055 (0.921–1.208) | 1.065 (0.929–1.221) |
| In years squared | 1.002 (0.997–1.008) | 1.002 (0.996–1.008) | 1.001 (0.995–1.008) |
| Diabetes-related characteristics | |||
| Oral hypoglycaemics | 0.718 (0.347–1.485) | 0.729 (0.351–1.515) | |
| Insulin | 0.361* (0.150–0.872) | 0.390* (0.160–0.950) | |
| Microvascular complications | 0.819 (0.468–1.434) | 0.925 (0.521–1.643) | |
| Macrovascular complications | 1.601 (0.947–2.707) | 1.602 (0.943–2.722) | |
| Diabetes-related distress | 0.979** (0.964–0.993) | ||
| Nagelkerke R2 | .063** | .090** | .114*** |
† All analyses adjusted for age, gender, education level and comorbid conditions
*Significant at .05 level, ** Significant at .01 level, *** Significant at .001 level
Starting with exercise, Table 2 shows that the longer participants had diabetes, the less days they were physically active. Diabetes duration had both a linear and quadratic effect, and Fig. 1 (blue line, based on model 1) shows that the decline in physical activity was largest during the first years after diagnosis. Adding diabetes-related characteristics to the model (model 2) decreased the effects of diabetes duration (though they remained significant), suggesting that the presence of macrovascular complications in particular was partially responsible for the negative relationship between diabetes duration and exercise. Adding diabetes-related distress to the model (model 3) did not make a difference. The variance in time spent exercising explained by the last model remained small (5%).
Fig. 1.
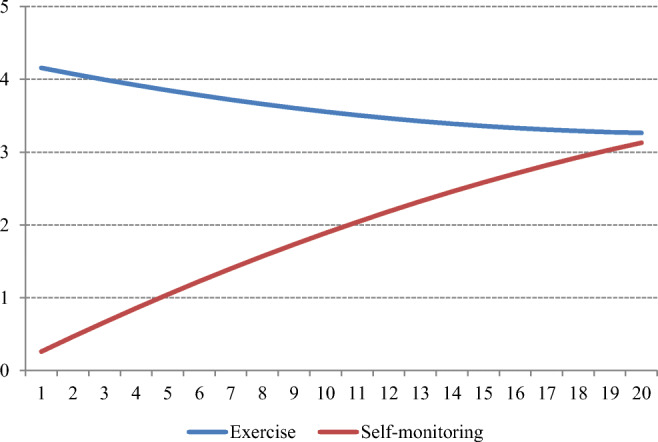
Illustration of the relationships between diabetes duration in years (X-axis) and the number of days per week (Y-axis) exercising (blue line) and self-monitoring (red line) (based on Table 2, model 1)
With regard to glucose self-monitoring, Table 2 shows that a longer diabetes duration increased the number of days that participants monitored their blood glucose levels. Figure 1 (red line, based on model 1) illustrates the not entirely linear relationship found between diabetes duration and the participants’ self-monitoring behaviour. The effects of diabetes duration substantially decreased after adding the diabetes-related characteristics (model 2). In particular, using insulin decreased the effects of diabetes duration on self-monitoring, suggesting that this was an important mediator. In addition, the total variance explained by the model increased from 17% to 37% by adding the diabetes-related characteristics, which indicates that using insulin has an important additive effect on glucose self-monitoring (in addition to diabetes duration).
Frequency of foot care was not related to diabetes duration (Table 2), but the presence of microvascular complications increased the number of days that the participants performed foot care, although the total variance remained low (5%).
With regard to healthy eating, Table 3 shows that diabetes duration was not a significant predictor. In fact, none of the diabetes-related variables in our analyses - except for the presence of microvascular complications, which had some small, negative effects - helped explain the participants’ eating behaviours. As such, the total variance in the participants’ eating behaviours explained by our models was less than 2%.
The duration of diabetes was not related to the participants’ smoking behaviour (Table 4); instead, the use of insulin and experiencing greater diabetes-related distress significantly decreased the likelihood of being a non-smoker. With all variables included, model 3 explained approximately 11% of the variance in smoking among the participants.
Discussion
In this study, we examined the relationship between lifestyle, self-care behaviours and disease duration in people with type 2 diabetes. We also explored the potential mediating roles of diabetes-related characteristics and diabetes-related distress in this relationship Our findings show that patients with a longer illness duration were less physically active; in particular during the first years after diagnosis the level of physical activity seems to decrease. Conversely, glucose self-monitoring was performed more often as illness duration increased. Regarding the opposing associations of diabetes duration with physical exercise and self-monitoring, it is possible that patients with a longer diabetes duration experience a greater number of health problems (e.g., fatigue and headache) that are not considered diabetes-related complications but do hinder physical activity and trigger the tendency to monitor blood glucose levels more often [29, 30]. Additionally, the negative association between diabetes duration and physical activity may indicate a shift in focus on the topics discussed during regular check-ups over time. These findings indicate that diabetes care providers may have to focus more on emphasizing the importance of an active lifestyle at later stages of illness progression, and on providing additional support to patients experiencing symptoms that may interfere with physical activity.
Relationships between diabetes duration and exercising or self-monitoring were partially mediated by the presence of macrovascular complications (exercising) and the use of insulin (self-monitoring). The presence of macrovascular complications had an additive, negative effect on exercise frequency. This finding that participants with macrovascular complications were less physically active could be the consequence of feelings of hesitation and uncertainty regarding physical exercise that are often experienced by individuals following an acute coronary event [31, 32]. However, as our study design did not allow causal interpretation, it should be noted that low levels of physical activity could have also contributed to the occurrence of macrovascular complications [33, 34]. The use of insulin was found to have additive effects on self-monitoring and smoking behaviour. The participants who used insulin monitored their blood glucose levels more frequently, but were also more often smokers. The fact that Dutch guidelines usually do not recommend regular or daily monitoring of blood glucose levels to patients not on insulin treatment [35] is most likely the main explanation for the positive association between insulin use and glucose monitoring, although diabetes duration continued to be positively related to glucose monitoring after treatment and complications had been added to the model. The relationship between insulin use and smoking may be explained by increased levels of diabetes distress, which have been found to be associated with insulin use in previous studies [36, 37], and to smoking in this study.
The presence of microvascular complications was found to have a positive effect on the frequency of foot care. The presumption that microvascular complications trigger self-care is supported by the positive association found between the presence of microvascular complications and the frequency of foot care, but not by the negative association found with dietary behaviours and the lack of association with physical activity and smoking behaviour. It may be that the presence of microvascular complications particularly impacts diabetes specific self-care behaviours, such as foot care [15], rather than more generic lifestyle behaviours such as physical activity, eating and smoking. In addition, the relatively large proportion of participants with a recent acute coronary event in the study sample could have masked the significance of microvascular complications as a cue to action for patients with type 2 diabetes to exercise, as we found that microvascular complications were positively related to exercising behaviour when analysing only the data from the SD sample [38]. The presence of microvascular complications in the DA sample may have been underreported, as it is likely that not all microvascular complications experienced by these patients were reported in the records maintained by their cardiologists [39].
Diabetes-related distress was only associated with smoking behaviour. Previous findings that diabetes-related distress is related to the presence of microvascular complications and insulin use in our sample [39] might elucidate why distress itself did not explain any additional variance in the regression models. Additionally, the participants’ scores on the PAID scale were generally low, which implies that they were not very concerned about their diabetes or its treatment.
Finally, it must be noted that although diabetes duration and its associated characteristics were found to be associated with the lifestyles and self-care behaviours of patients with type 2 diabetes, only a small proportion of the variance could be explained by these determinants. In other words, with the exception of glucose self-monitoring, self-care seems to be primarily influenced by other factors that were not included in this study, such as psychological characteristics, family support or other priorities.
A strength of our study is the large size of the total sample, which allowed us to examine a broad range of diabetes durations and diabetes-related characteristics. Baseline data from three RCT’s were combined to obtain the study sample. Although all three samples were part of the Dutch Diacourse study, it should be noted that the data collection procedures were not exactly the same. In the SD and LD samples, several illness-related characteristics, such as diabetes treatment, complications and comorbidities, were self-reported by patients, whereas in the DA study, data on these characteristics were derived from hospital records. Self-reported complications and conditions may not fully correspond with relevant symptoms and diseases from a medical point of view. Nonetheless, they have been proven to be important determinants of health behaviours and outcomes [40, 41]. Furthermore, the participants in this study may not be entirely representative of all patients with type 2 diabetes, as those included here were willing to participate in an intervention study on self-management, which may have led to an underrepresentation of patients who are less motivated to perform self-care. However, by recruiting general practices and hospitals in different regions across the Netherlands, and by covering the (travel) expenses of the participating patients, we aimed to keep the chances on selection bias in our study population as low as possible. Furthermore, as all inhabitants in the Netherlands are obligatory registered at a general practice, no selection could have occurred beforehand.
Notwithstanding its limitations, we believe that our study provided some valuable insights to support the self-care of patients with type 2 diabetes in clinical practice. We have added to existing literature by differentiating the impact of diabetes duration in itself from the impact of illness-related characteristics on self-care, and by reporting their relationship separately for the different, independent self-care behaviours that make up the diabetes care regimen. Our study results show that diabetes duration and several diabetes-related characteristics (i.e., presence of microvascular and macrovascular complications as well as treatment type) need to be taken into account when supporting patients in making lifestyle changes and adhering to self-care recommendations. Clinicians need to be aware that patients have different support needs dependent on the type of self-care behaviour at stake as well as on the phase of illness they find themselves in. For instance, with regard to physical activity, diabetes care providers should encourage physical exercise not only in consultations with patients in the first years after diagnosis but also in consultations with patients with a much longer diabetes duration, as their physical activity seems to decline. In these consultations, special attention needs to be paid to complications or conditions that might interfere with exercise either because of their disabling nature or because of patients’ fears or false beliefs that result in the avoidance of activity. In the early years of diabetes, other support may be necessary. Attention should be paid to the benefits and barriers that patients perceive with regard to adhering to lifestyle and self-care recommendations, especially in the absence of diabetes-related symptoms. Traditional patient education may not be sufficient, as it often neglects patients’ personal goals and their perceptions of their illness. Therefore, innovative strategies need to be developed to provide tailored person-centered support to help patients with type 2 diabetes adopt a healthy lifestyle and perform adequate self-care in all phases of their illness. Future research should examine whether (additional) support that takes into account the phase of illness – and then specifically the presence and the type of complications – is effective in improving self-care over the course of illness.
Conclusions
Patients with type 2 diabetes with a longer illness duration are less physically active than those with a shorter illness duration, which partially relates to the higher frequency of macrovascular complications in patients with a longer illness duration. In contrast, patients with type 2 diabetes with a longer illness duration monitor their blood glucose levels more frequently, which mainly relates to their use of insulin. To help patients adopt a healthy lifestyle and improve their self-care, diabetes care providers need to tailor their support to the phase of the illness that patients find themselves, to characteristics such as the presence of complications and the type of treatment, and to patients’ personal characteristics and perceptions.
Acknowledgements
The authors thank all patients, general practitioners and supportive staff in the primary care practices, cardiologists and supportive staff in the hospitals who participated in the Diacourse study. All other members of the Diacourse study group are acknowledged for their important contribution to the implementation of the Diacourse study: Guy Rutten, Kees Gorter, Rimke Vos (University Medical Center Utrecht, Utrecht, Netherlands); Amber van der Heijden (Amsterdam University Medical Centers, location VUmc, Amsterdam, the Netherlands); Caroline Baan (Tilburg University, Tilburg, the Netherlands; National Institute for Public Health and the Environment, Bilthoven, Netherlands). The Wiley Editing Service team provided basic editing services.
Compliance with ethical standards
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
This work was supported by the Dutch Diabetes Research Foundation (2009.70).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Marise Kasteleyn and Lianne de Vries contributed equally to this work.
References
- 1.International Diabetes Federation. IDF Diabetes Atlas. Eighth Edition. Available at: https://diabetesatlas.org/resources/2017-atlas.html. Accessed 21 Nov 2019.
- 2.Nouwen A, Adriaanse M, Van Dam K, Iversen M, Viechtbauer W, Peyrot M, et al. Longitudinal associations between depression and diabetes complications: a systematic review and meta-analysis. Diabet Med. 2019. 10.1111/dme.14054. [DOI] [PubMed]
- 3.Mehta Z, Cull C, Stratton I, Yudkin J, Jenkinson C, Fletcher A, et al. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). Diabetes Care. 1999. 10.2337/diacare.22.7.1125. [DOI] [PubMed]
- 4.Solli O, Stavem K, Kristiansen IS. Health-related quality of life in diabetes: the associations of complications with EQ-5D scores. Health Qual Life Outcomes. 2010;8:18. doi: 10.1186/1477-7525-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999. 10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O. [DOI] [PubMed]
- 6.American Diabetes Association Standards of medical Care in Diabetes - 2014. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 7.Young MD, Callister R, Collins CE, Plotnikoff RC, Aguiar EJ, Morgan PJ. Efficacy of a gender-tailored intervention to prevent weight regain in men over 3 years: a weight loss maintenance RCT. Obesity. 2017; [DOI] [PubMed]
- 8.Nelson LA, Mayberry LS, Wallston K, Kripalani S, Bergner EM, Osborn CY. Development and usability of REACH: a tailored theory-based text messaging intervention for disadvantaged adults with type 2 diabetes. JMIR Hum Factors 2016; [DOI] [PMC free article] [PubMed]
- 9.McBrien KA, Manns BJ, Hemmelgarn BR, Weaver R, Edwards AL, Ivers N, et al. The association between sociodemographic and clinical characteristics and poor glycaemic control: a longitudinal cohort study. Diabet Med. 2016;33:1499–507. [DOI] [PubMed]
- 10.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004. [DOI] [PubMed]
- 11.Beverly EA, Wray LA, Chiu CJ, Weinger K. Perceived challenges and priorities in co-morbidity management of older patients with Type2 diabetes. Diabet Med. 2011. [DOI] [PMC free article] [PubMed]
- 12.Kerr EA, Heisler M, Krein SL, Kabeto M, Langa KM, Weir D, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007; [DOI] [PMC free article] [PubMed]
- 13.Pouwer F, Nefs G, Nouwen A. Adverse effects of depression on glycemic control and health outcomes in people with diabetes. A Review. Endocrinol. Metab. Clin. North Am. 2013. [DOI] [PubMed]
- 14.Thorne S, Paterson B, Russell C. The structure of everyday self-care decision making in chronic illness. Qual Health Res. 2003; [DOI] [PubMed]
- 15.Matricciani L, Jones S. Who cares about foot care? Barriers and enablers of foot self-care practices among non-institutionalized older adults diagnosed with diabetes: an integrative review. Diabetes Educ [internet]. 2015;41:106–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25480398. [DOI] [PubMed]
- 16.Ruggiero L, Glasgow RE, Dryfoos JM, Rossi JS, Prochaska JO, Orleans CT, et al. Diabetes self-management: self-reported recommendations and patterns in a large population. Diabetes Care. 1997. [DOI] [PubMed]
- 17.Schoenberg NE, Drungle SC. Barriers to non-insulin dependent diabetes mellitus (NIDDM) self-care practices among older women. J Aging Health 2001; [DOI] [PubMed]
- 18.Thoolen B, De Ridder D, Bensing J, Gorter K, Rutten G. No worries, no impact? A systematic review of emotional, cognitive, and behavioural responses to the diagnosis of type 2 diabetes. Health Psych Rev. 2008;2:65–93 Available from: http://www.tandfonline.com/doi/abs/10.1080/17437190802311361.
- 19.Sasi ST, Kodali M, Burra KC, Muppala BS, Gutta P, Bethanbhatla MK. Self Care Activities, Diabetic Distress and other Factors which Affected the Glycaemic Control in a Tertiary Care Teaching Hospital in South India. J Clin Diagn Res. 2013; [DOI] [PMC free article] [PubMed]
- 20.Sparring V, Nyström L, Wahlström R, Jonsson PM, Östman J, Burström K. Diabetes duration and health-related quality of life in individuals with onset of diabetes in the age group 15—34 years – a Swedish population-based study using EQ-5D. BMC Public Health. 2013. [DOI] [PMC free article] [PubMed]
- 21.Fisher L, Mullan JT, Arean P, Glasgow RE, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010; [DOI] [PMC free article] [PubMed]
- 22.Delamater A. Improving patient adherence. Clin Diabetes. 2006;2:71–77. doi: 10.2337/diaclin.24.2.71. [DOI] [Google Scholar]
- 23.van Puffelen AL, Rijken M, Heijmans MJ, Nijpels G, Rutten GE, Schellevis FG. Living with diabetes: a group-based self-management support programme for T2DM patients in the early phases of illness and their partners, study protocol of a randomised controlled trial. BMC Health Serv Res. 2014;14:144 Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3977690&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed]
- 24.de Vries L, van der Heijden AA, van ‘t Riet E, Baan CA, Kostense PJ, Rijken M, et al. Peer support to decrease diabetes-related distress in patients with type 2 diabetes mellitus: design of a randomised controlled trial. BMC Endocr Disord. 2014;14:21. doi: 10.1186/1472-6823-14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasteleyn MJ, Gorter KJ, Stellato RK, Rijken M, Nijpels G, Rutten GE. Tailored support for type 2 diabetes patients with an acute coronary event after discharge from hospital – design and development of a randomised controlled trial. Diabetol Metab Syndr. 2014;6:5 Available from: http://dmsjournal.biomedcentral.com/articles/10.1186/1758-5996-6-5. [DOI] [PMC free article] [PubMed]
- 26.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care. Diabetes Care. 2000;23:943–50. [DOI] [PubMed]
- 27.Snoek F, Pouwer F, Welch G, Polonsky W. Diabetes-related emotional distress in. Diabetes Care. 2000;23:1305–1309. doi: 10.2337/diacare.23.9.1305. [DOI] [PubMed] [Google Scholar]
- 28.Welch GW, Jacobson AM, Polonsky WH. The problem areas in diabetes scale. An evaluation of its clinical utility. Diabetes Care. 1997;20:760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 29.Garg SK, Aurand LA, Rimler MS, Dailey GE. Diabetes duration and the efficacy and safety of insulin glargine versus comparator treatment in patients with type 2 diabetes mellitus. Endocr Pract. 2014;20:120–8. [DOI] [PubMed]
- 30.Spallone V, Morganti R, D’Amato C, Cacciotti L, Fedele T, Maiello MR, et al. Clinical correlates of painful diabetic neuropathy and relationship of neuropathic pain with sensorimotor and autonomic nerve function. Eur J Pain. 2011. [DOI] [PubMed]
- 31.Cooper AF, Jackson G, Weinman J, Horne R. A qualitative study investigating patients’ beliefs about cardiac rehabilitation. Clin Rehabil. 2005; [DOI] [PubMed]
- 32.Kasteleyn MJ, Gorter KJ, Van Puffelen AL, Heijmans M, Vos RC, Jansen H, et al. What follow-up care and self-management support do patients with type 2 diabetes want after their first acute coronary event? A qualitative study. Prim Care Diabetes 2014;8. [DOI] [PubMed]
- 33.Bassuk SS, Manson JE. Epidemiological evidence for the role of physical activity in reducing risk of type 2 diabetes and cardiovascular disease. J Appl Physiol. 2005. [DOI] [PubMed]
- 34.Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O’Keefe JH, et al. Physical Activity, Cardiorespiratory Fitness, and Exercise Training in Primary and Secondary Coronary Prevention. Circ J. 2013; [DOI] [PMC free article] [PubMed]
- 35.Eerste associatie van diabeteszorgverleners (EADV). Multidisciplinaire richtlijn over zelfcontrole van bloedglucosewaarden door mensen met diabetes. 2012. http://www.eadv.nl/page/Richtlijnen-1/Zelfcontrole-open?mod[1238][i]=57. Accessed 31 Jan 2019.
- 36.Stoop CH, Nefs G, Pop VJ, Wijnands-van Gent CJM, Tack CJ, Geelhoed-Duijvestijn PHLM, et al. Diabetes-specific emotional distress in people with type 2 diabetes: a comparison between primary and secondary care. Diabet Med. 2014. [DOI] [PubMed]
- 37.Delahanty LM, Grant RW, Wittenberg E, Bosch JL, Wexler DJ, Cagliero E, et al. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with type 2 diabetes. Diabet Med. 2007. [DOI] [PubMed]
- 38.van Puffelen AL, Heijmans MJWM, Rijken M, Rutten GEHM, Nijpels G, Schellevis FG. Illness perceptions and self-care behaviours in the first years of living with type 2 diabetes; does the presence of complications matter? Psychol Health. 2015;30. [DOI] [PubMed]
- 39.Kasteleyn MJ, de Vries L, van Puffelen AL, Schellevis FG, Rijken M, Vos RC, et al. Diabetes-related distress over the course of illness: results from the Diacourse study. Diabet Med. 2015;32. [DOI] [PubMed]
- 40.Idler R. Self-assessed health and mortality: a review of studies. In: Maes S, Leventhal H, Johnston M, editors. Int rev heal Psychol. New York: Wiley; 1992.
- 41.Perrig-Chiello P, Perrig W, Stähelin H. Health control beliefs in old age - relationship with subjective and objective health, and health behaviour. Psychol Health Med. 1999;4:83–94. doi: 10.1080/135485099106423. [DOI] [Google Scholar]


