Abstract
In response to the coronavirus disease 2019 (COVID-19) pandemic, 107 countries had implemented national school closures by March 18, 2020. It is unknown whether school measures are effective in coronavirus outbreaks (eg, due to severe acute respiratory syndrome [SARS], Middle East respiratory syndrome, or COVID-19). We undertook a systematic review by searching three electronic databases to identify what is known about the effectiveness of school closures and other school social distancing practices during coronavirus outbreaks. We included 16 of 616 identified articles. School closures were deployed rapidly across mainland China and Hong Kong for COVID-19. However, there are no data on the relative contribution of school closures to transmission control. Data from the SARS outbreak in mainland China, Hong Kong, and Singapore suggest that school closures did not contribute to the control of the epidemic. Modelling studies of SARS produced conflicting results. Recent modelling studies of COVID-19 predict that school closures alone would prevent only 2–4% of deaths, much less than other social distancing interventions. Policy makers need to be aware of the equivocal evidence when considering school closures for COVID-19, and that combinations of social distancing measures should be considered. Other less disruptive social distancing interventions in schools require further consideration if restrictive social distancing policies are implemented for long periods.
Introduction
WHO declared the coronavirus disease 2019 (COVID-19) outbreak, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), to be a pandemic on March 12, 2020.1 On March 18, 2020, the UN Educational, Scientific and Cultural Organization estimated that 107 countries had implemented national school closures related to COVID-19, affecting 862 million children and young people, roughly half the global student population. This situation had rapidly escalated from 29 countries with national school closures a week before.2 School closures are based on evidence and assumptions from influenza outbreaks that they reduce social contacts between students and therefore interrupt the transmission.3
School closures can affect deaths during an outbreak either positively, through reducing transmission and the number of cases, or negatively, through reductions in the health-care workforce available to care for those who are sick. Studies of UK children and young people report that the mean number of daily social contacts during school holidays are approximately half that of school term days;4, 5 however, contacts continue and mixing between children and adults and between children at different schools actually increases during holidays and school closures.4, 5, 6, 7 The evidence for the effectiveness of school closures and other school social distancing measures comes almost entirely from influenza outbreaks, for which transmission of the virus tends to be driven by children. It is unclear whether school measures are effective in coronavirus outbreaks—for example, due to severe acute respiratory syndrome (SARS), or Middle East respiratory syndrome (MERS) and, most specifically, COVID-19, for which transmission dynamics appear to be different.
Four systematic reviews8, 9, 10, 11 of the effects of school closure on influenza outbreaks or pandemics suggest that school closure can be a useful control measure, although the effectiveness of mass school closures is often low. School closure strategies might be national, regional, local, or reactive closure of individual schools in response to student infection rates. A systematic review,8 commissioned by the UK Department of Health in 2014, to inform influenza pandemic preparations, included 100 epidemiological and 45 modelling studies and concluded that school closures can reduce transmission of pandemic influenza if instituted early in outbreaks. School closures result in greater reductions in peak than in cumulative attack rates and, according to modelling studies, are likely to have the greatest effect if the virus has low transmissibility (reproductive number [R] <2) and if attack rates are higher in children than in adults. A second review9 of modelling studies by the same authors drew similar conclusions.
A 2018 review10 of 31 studies that addressed whether school closure had a quantifiable effect on influenza transmission reported that school closure reduced the peak of the related outbreak by a mean of 29·7% and delayed the peak by a median of 11 days. They also reported that earlier school closure predicted a greater reduction in the outbreak peak, although these estimates did not come from formal meta-analyses.10 A 2015 systematic review11 of social distancing practices, including school closures, for influenza pandemics reported a wide variation in the reduction of transmission (range 1–50%) but noted that up to 70% of students might shift social contacts to other non-school sites during closures, reducing the effect of closures. A 2020 systematic review12 of school closures and other social distancing measures during influenza outbreaks also found compelling evidence that closures reduced transmission, particularly among school-aged children (5–17 years). However, there was substantial evidence that transmission surged again once schools reopened, and there was little consensus on the appropriate timing of closures, let alone reopening of schools.
One way that school closures are effective during outbreaks might be through forcing parents to work at home and thus reducing work-related contacts. However, reviews have also noted the adverse effects of school closure, including economic harms to working parents, health-care workers, and other key workers being forced from work to childcare, and to society due to loss of parental productivity, transmission from children to vulnerable grandparents, loss of education, harms to child welfare particularly among the most vulnerable pupils, and nutritional problems especially to children for whom free school meals are an important source of nutrition.8, 10, 11 Social isolation itself brings a range of psychological harms.13 A rapid review13 found evidence that, during unplanned school closures, children's activities and contacts decreased but did not cease, with some evidence that this was particularly so among older children and those whose parents disagreed with closures.7
The economic harms of school closures are high. A UK study14 from 2008 suggested that approximately 16% of the workforce are the main caregivers for dependent children and are at very high risk of absenteeism if schools are closed, a proportion that rises to 30% in the health and social care sectors. In the USA, unpublished estimates suggest that 29% of health-care workers have childcare obligations.15 A 2010 economic modelling analysis16 of school closures as mitigating interventions during influenza outbreaks suggested that 4-week or 13-week closures reduced the clinical attack rate minimally but markedly increased the economic cost to the nation, in particular through forced absenteeism by working parents, in the UK, France, Belgium, and the Netherlands. Costs have been estimated to be as high as 0·2–1% of UK national gross domestic product (GDP) per annum for school closure for 12–13 weeks,14 or up to 3% of GDP for an 8-week closure in US studies.17 Reviews have not summarised economic harms from school closure in detail, but economic modelling from an influenza outbreak in Hong Kong, China, suggested that the most cost-effective models were selective local closures rather than city-wide closures.18
Notably, regardless of official school closure or other distancing policies, unofficial student and staff absenteeism (whether due to illness or precautionary) can be very high during epidemics. Staff absenteeism can lead to forced local school closures.19 School dismissal—whereby all students, except the most vulnerable and children of health-care and other essential workers, are sent home but the school stays open—has been suggested to be a less strict intervention than school closure, although there is no evidence supporting its use separately to full closure.20
There are many other potential social distancing actions available for schools that are less drastic than full closure, although these have received little attention.21 A 2018 systematic review21 of such strategies noted that potential practices include suspending affected classes or year groups, or changing the school organisation structure to reduce student mixing (eg, by closing playgrounds, cancelling non-essential activities and meetings, keeping students in constant class groups or classrooms, increasing spacing between students in classes, shortening the school week, and staggering school start and lunch or break times across year groups or classes). The review concluded that few studies have been done but that a small number of modelling studies supported the use of alternative strategies during influenza outbreaks.22, 23 There were no UK studies included in this review.21 In the 2009 H1N1 influenza pandemic, Taiwan instituted class suspensions rather than school closures, facilitated by keeping students in a homeroom class with a core teacher and having other teachers routinely moving between classes. Studies suggest that this approach was an effective social distancing measure in this outbreak while reducing social disruption.24
To reduce the transmission of COVID-19, many countries had instituted large-scale or national closure of schools by March, 2020. These actions appear largely based on assumptions that the benefits apparent in influenza outbreaks are also likely to be true for COVID-19. There are several theoretical reasons why school closures might be less effective in COVID-19 than in influenza outbreaks. Children contribute more to influenza transmission than do adults,25 with low levels of immunity and high levels of transmission due to symptomatic disease. However, in the COVID-19 pandemic thus far, children appear to form a much lower proportion of cases than expected from their population, although evidence for this is mixed and some data suggest that children might be as likely to be infected as adults but largely remain asymptomatic or have a mild form of the disease.26 It remains unclear whether the low proportion of confirmed COVID-19 cases among children in mainland China relate to a reduced risk of infection, having subclinical or milder infections, or specific population factors (eg, one-child policy). Evidence of COVID-19 transmission through child–child contact or through schools is not yet available, although family transmission has an important role in the outbreak.
In some previous coronavirus outbreaks, evidence suggested that transmission in schools was very low or absent.27 As modelling studies of school closures for influenza outbreaks rely on assumptions about the proportion of cases transmitted in schools being relatively high,28 these models cannot be assumed to be informative regarding effectiveness for COVID-19. Emerging epidemiological data suggest little evidence of transmission of COVID-19 through schools in China, although this might reflect closure of schools during most of the outbreak. Notably, school closures began with not reopening schools after the Chinese New Year holidays.29 As of April 3, 2020, Taiwan has been recognised to have effectively minimised spread of COVID-19,30 but with national policies that avoided widespread planned school closures and instead mandated initially local class closures, and subsequently local temporary school closures, based on low thresholds for infected cases within individual schools.30 In view of the scarce information and pressure on countries to consider school closures to deal with the COVID-19 pandemic, we did a systematic review of the literature to answer the question: what is known about the use of and effectiveness and cost-effectiveness of school closure and other school social distancing practices on infection rates and transmission during coronavirus outbreaks?
Methods
We sought to include quantitative studies using diverse designs to model or empirically evaluate the effects of school closure and other school social distancing practices on infection rates and transmission during coronavirus outbreaks. Our search was designed to be inclusive of any studies providing data on schools or nurseries. We searched various electronic databases on March 9, 2020, and again on March 19, 2020, with no language restrictions. We searched PubMed using search terms and database-appropriate syntax: SARS [tw] OR “severe acute respiratory syndrome”[mh] OR “severe acute respiratory syndrome” OR “Middle East Respiratory Syndrome Coronavirus”[mh] OR “middle east respiratory syndrome*”[tw] OR “MERS-CoV”[tw] OR Mers[tw] OR “Middle Eastern Respiratory Syndrome*”[tw] OR “MERSCoV*”[tw] OR coronavirus[mh] OR Coronavirus Infections[mh] OR coronavirus*[tw] OR “COVID-19”[tw] or “2019-nCoV”[tw] or “SARS-CoV-2”[tw]) AND (Schools[mh:noexp] OR schools, nursery[mh] OR “Child Day Care Centers”[mh] OR “Nurseries, Infant”[mh] OR school[tiab] OR schools[tiab] OR preschools[tiab] OR preschool[tiab] OR “pre school”[tiab] OR “pre schools”[tiab] OR nursery[tiab] OR nurseries[tiab] OR kindergarten[tiab] OR kindergarten[tiab] OR “day care” OR daycare AND child* OR infant*. We searched the WHO Global Research Database on COVID-19 using the term “school”, which only retrieved one article that we excluded as it did not contain research. Therefore, we searched again using the search terms “child”, “children”, “childhood”, “infant”, “baby”, “babies”, “pediatric”, and “paediatric”. We also searched the preprint server medRxiv for all papers using the search terms “SARS or MERS or coronavirus or COVID-19”. We did not find it useful to include search terms relating to schools as the search facilities were not sophisticated.
All articles were triple screened (by SJR, HC, and JP) on title and abstract. We excluded opinion pieces, systematic reviews, studies addressing other viruses, university-specific settings, epidemiological studies not examining intervention effects (eg, of prevalence of infection in schools), and studies in other languages with no English translation. All full-text articles identified were reviewed by RMV. For each retrieved full-text article, we hand searched included references and examined the citation chain for additional studies. We did not attempt to rate the quality of included studies in this Review. We considered findings from preprint articles separately to published peer-reviewed articles.
Results
Study selection and characteristics
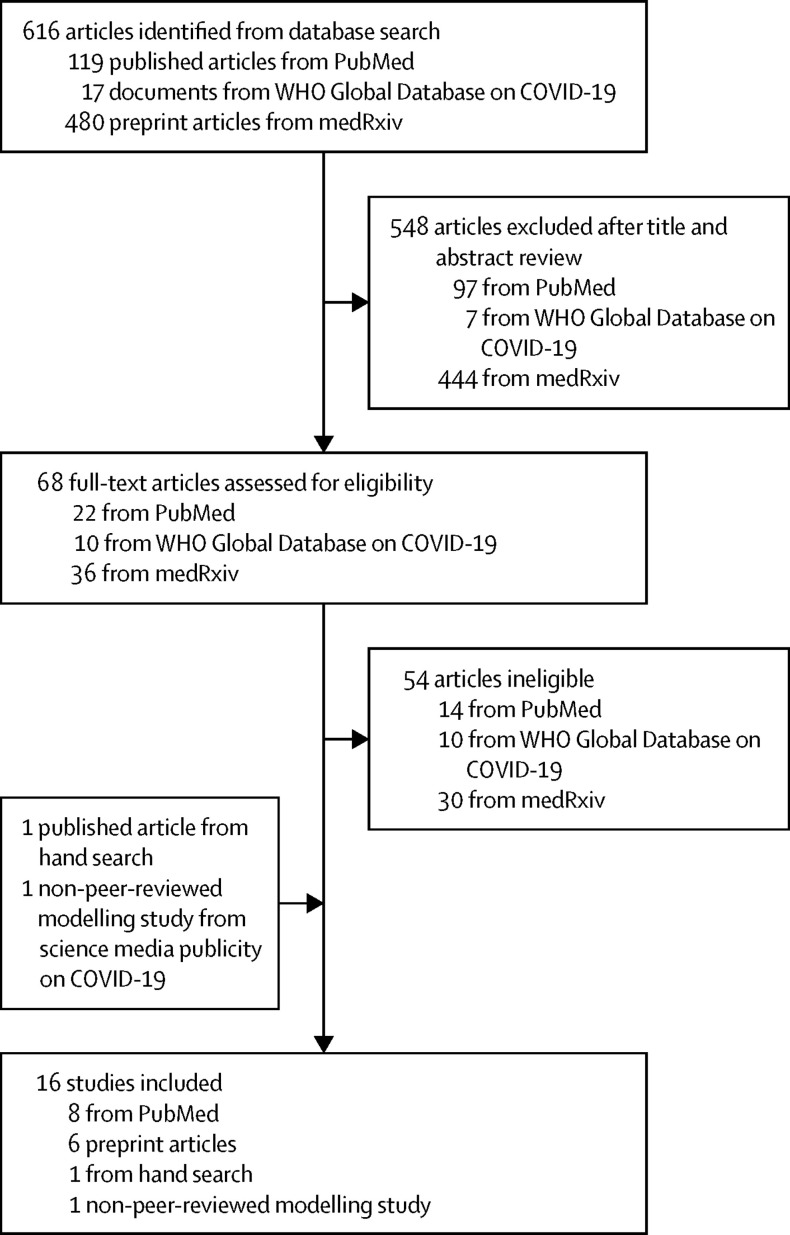
The PubMed search identified 119 articles, of which 22 full-text articles were assessed and eight included in the Review. Searching the WHO Global Research Database on COVID-19 did not return relevant articles. The search on medRxiv yielded 480 articles, of which 36 full-text preprint articles were assessed and six included in the Review. Hand searching of full-text articles identified one additional reference, and one additional modelling study31 published as a non-peer-reviewed report was identified and included. In total, 16 studies were included in this Review (figure ).
Figure.
Study selection process
COVID-19=coronavirus disease 2019
All published articles concerned the 2003 SARS outbreak. One preprint article32 concerned the effect of school closures on transmission of other (endemic) coronaviruses (229E, NL63, OC43, and HKU1) and five preprints and one report31 concerned the COVID-19 pandemic.
Six papers described or evaluated school actions as part of control measures undertaken in response to the SARS outbreak in Taiwan,24 Singapore,33, 34, 35 and Beijing, China.36, 37 Two papers were modelling studies that estimated SARS transmission in schools38 or the effect of school closure39 on transmission in SARS outbreaks. One paper reported qualitative research with health-care workers after the SARS outbreak relating to the effect of school closures.40 Five preprint articles reported on school closures during the COVID-19 outbreak in mainland China41, 42, 43 and Hong Kong.12, 44 One preprint article described the impact of school closure on winter transmission of other human coronaviruses.32 One report modelled the impact of school closures in the UK on transmission of COVID-19.31
Effectiveness of school social distancing measures
Preprint studies41, 42 report that school closures were initiated nationally across mainland China in late January, 2020—which manifested as delaying the restarting of schools after the Chinese New Year holidays—as part of a broader series of control measures during the COVID-19 epidemic. No data are available on the effectiveness of school closure as there was little variation in timing of closures (closures were reportedly applied in all Chinese cities uniformly and without delay) and school closures were part of a broad range of quarantine and social distancing measures. Both of these studies concluded that the overall package of quarantine and social distancing was effective in reducing the epidemic in mainland China,41, 42 although the relative contribution of school closures was not assessed.
Preprint studies of actions in Hong Kong related to COVID-19 noted that a 4-week school closure was initiated across the city on Feb 1, 2020, approximately 1 week after the first cases were identified in Hong Kong. School closures were implemented at the same time as a number of other stringent social distancing measures, with school closures extended initially to March, 2020, then to April, 2020.12, 44 Collectively, these measures were considered to have reduced the R below 1, controlling the spread of the outbreak.12 As in mainland China, no data were available from either paper on the effect of school closures separate from other measures. Cowling and colleagues12 noted that the social distancing measures implemented during the COVID-19 outbreak reduced community transmission by 44%, which was much greater than the estimated 10–15% reduction in influenza transmission conferred by school closures implemented alone during the 2009 pandemic in Hong Kong.44
During the SARS epidemic, schools in Beijing were closed on April 24, 2003, approximately 6 weeks after the beginning of the outbreak, and remained closed for over 2 months. One study36 concluded that school closures made very little difference to the prevention of SARS in Beijing, given the very low attack rate in schools before the closure and the low prevalence of disease in children. A second study37 estimated the effective R for each day of the Beijing SARS outbreak, noting that school closures occurred after the R had dropped below 1 and that school closures in this case added little to control of the outbreak. Class cancellation strategies, in which upper high-school and college students remained on college campuses but did not attend classes, were also widely used during the SARS outbreak in mainland China.45 There was no recorded transmission of SARS in schools during the outbreak in mainland China.46
A review33 of the 2003 SARS outbreak in Singapore noted that twice daily, mandatory temperature screening of all children aged 6–16 years in schools was part of the containment measures instituted. Pupils were excluded from school if their temperature was more than 37·8°C for students aged 12 years or younger, or more than 37·5°C for students older than 12 years. Although there were school children diagnosed with SARS in Singapore, none of them were identified through temperature screening.35 All educational facilities in Singapore were closed for 3 weeks from March 27, 2003 (the SARS outbreak ran from late February to May 2003), together with suspension of other activities to prevent the congregation of large groups of children.34
A review24 of responses in Taiwan to the SARS outbreak and 2009 H1N1 influenza pandemic noted that schools were designated as alternative health-care sites in case the health system was overwhelmed during the SARS outbreak, but that there were no school social distancing measures (including closures) introduced during the SARS outbreak. This finding is in contrast to the use of class suspensions during the H1N1 pandemic in Taiwan.24
Schools were also closed in Hong Kong during the SARS epidemic; however, the extent to which this was at a city-wide or local level is unclear. There was no evidence of spread of the infection in schools, with spread among children almost entirely through family settings and living in the same apartment blocks as infected cases.27
A preprint study by Jackson and colleagues32 used routine viral surveillance to examine the effects on transmission of endemic human coronaviruses (229E, NL63, OC43, and HKU1) and other viruses of a 5-day closure of nearly all schools in the greater Seattle metropolitan area in February, 2019, due to extreme weather on transmission of these viruses. Their study estimated that the school closure resulted in a 5·6% (95% CI 4·1–6·9) reduction in coronavirus infections, similar to influenza H1N1 (7·6%; 5·2–9·7) but higher than influenza H3N2 (3·1%; 2·5–3·2), all of which were prevalent at the time.32
Modelling studies
A preprint modelling study43 examined the effect of school closure together with other social distancing measures in Wuhan, China. The study used transmission data representative of COVID-19, but it was unclear whether epidemiological data from the outbreak were used further in the modelling. This study concluded that the package of social distancing measures was effective in reducing the final size and peak incidence of the outbreak while also delaying the peak.43 However, it did not examine the effect of school closures relative to other measures. It modelled different timings of relaxation of social distancing measures and concluded that earlier relaxation (after 2 months of restrictions) risked a second peak, whereas 3 months of restrictions did not result in a second peak.43
Only one study examined the effect of school closures separately to other social distancing measures. In a non-peer-reviewed but widely cited report from an established group, Ferguson and colleagues31 modelled the estimated effects of a range of different social distancing measures and combinations of measures. They used UK population and schools data together with data on transmission dynamics reported from the COVID-19 outbreak in Wuhan. Using data from previous influenza outbreaks, they assumed that per-capita contacts within schools were double those in households, workplaces, or the community, and that, overall, approximately a third of transmission occurred in schools. They modelled a scenario in which all schools and 25% of universities were closed and where the effect on non-school social contacts was an increase of 50% in household contact rates for families with children and a 25% increase in community contacts during the closure. They concluded that school closure as an isolated measure was predicted to reduce total deaths by around 2–4% during a COVID-19 outbreak in the UK, whereas single measures such as case isolation would be more effective, and a combination of measures would be the most effective. The authors concluded that school closure is predicted to be insufficient to mitigate (never mind suppress) the COVID-19 pandemic in isolation, which is in contrast to seasonal influenza epidemics where children are the key drivers of transmission.31
An early modelling study of a SARS-like illness in school children concluded that a school closure policy would reduce the effective R by 12–41% depending on the proportion of between-household mixing that occurred during school hours. The study noted that modelling was based on plausible assumptions regarding characteristics of the SARS virus, noting that obtaining good quality estimates of epidemiological parameters for SARS was difficult as the outbreak was contained rapidly.39
A modelling study of the transmission of SARS in hospitals and in elementary school classrooms in Taiwan using data from the 2003 SARS outbreak concluded that a single case of SARS would infect an average of 2·6 secondary cases in a population from transmission in hospital, whereas less than 1 secondary infection would be generated per case in a school classroom.38
Broader societal issues
Conflict between the work and family requirements of health-care professionals during the SARS epidemic was explored in qualitative research with 100 Canadian emergency and critical care nurses, many of whom had been involved with the SARS outbreak.40 The study found that health-care workers experience substantial personal dilemmas in balancing work and family commitments, particularly relating to childcare needs if schools are closed and childcare services are unavailable. The study concluded that there was a need for provision of adequate resources to protect the families of health-care workers during outbreaks to maintain maximal staffing.40
Discussion
This Review provides the first summary of data on school closures and other school social distancing practices during coronavirus outbreaks. We were able to include only nine published studies and seven non-peer-reviewed studies. We decided to include unreviewed studies as data would not otherwise be available on COVID-19, although findings were interpreted with caution. Except for one modelling study, none of the included studies were designed to specifically examine the effectiveness of school distancing measures. Thus, data provided on the effect of school measures were of relatively low quality.
We identified a remarkable dearth of policy-relevant data on the implementation of school social distancing during coronavirus outbreaks. This finding is perhaps not surprising for the rapidly emerging COVID-19 pandemic, but previous coronavirus outbreaks such as SARS and MERS provide limited information about the effectiveness of school closures and no data on cost-effectiveness. No data on other less disruptive school social distancing practices during coronavirus outbreaks were identified.
Data from the SARS outbreak in mainland China, Hong Kong, and Singapore suggest that school transmission played no substantial role in the outbreak, and that school closures and other activities such as school temperature monitoring did not contribute to control of infection transmission. It is possible that these findings reflect an effect of school closures in rapidly stopping transmission; however, this is unlikely as schools remained open for prolonged periods during the early part of the outbreak. Modelling studies from the SARS outbreak produced different results. Although Becker and colleagues39 estimated that school closure resulted in potentially important reductions in transmission, Liao and colleagues38 estimated that transmission in school classrooms was low.
School closures were rapidly deployed across mainland China and Hong Kong in early 2020 as part of a wider set of control measures for COVID-19, with the result that no data were available on the comparative effectiveness of school closure interventions in isolation. Authors of preprint studies41, 44 concluded that school closures likely contributed to the control of COVID-19 in China as part of a package of very broad quarantine measures. However, they provide no data to support this assertion and indeed it might be very difficult to disentangle the relative contribution of school closures.
Modelling studies from the COVID-19 pandemic support the use of national school closure as part of a package of social distancing measures. Yet, the only study to examine school closures as a separate intervention warned that the impact was relatively marginal, given the reasonable assumptions that household and community contacts would rise as a consequence.
There are few data available from the literature on coronavirus outbreaks to guide countries on the use of school closures or other school social distancing practices during the COVID-19 pandemic. Available evidence is consistent with a broad range of impacts of school closures, from little effect on reducing transmission through to more substantial effects. Yet, the economic costs and potential harms of school closure are undoubtedly very high.
As evidence from coronavirus outbreak control is scarce, we must turn to evidence for the benefits of school closures from influenza epidemics and pandemics. School closures have been widespread in some countries during influenza pandemics, and many studies report important effects on reducing transmission and the size of the pandemic. Yet, there is considerable heterogeneity in the impact of school closures on transmission depending on characteristics of influenza serotype transmission. Systematic reviews of influenza outbreaks suggest that school closures are likely to have the greatest effect if the virus has low transmissibility (R<2), particularly if attack rates and transmission are higher in children than in adults.8 Although our information on SARS-CoV-2 remains incomplete, this appears not to be the case with COVID-19 outbreaks. Reported R values for COVID-19 are high (≥2·5).47 Although children appear to contract infection at the same rate as adults, they largely have mild or asymptomatic forms of the disease and appear to be less likely to spread the virus through coughing or sneezing; however, a precise understanding is as yet lacking. Notably, analyses using UK clinical data from the 1957 Asian influenza pandemic suggest that school closures would reduce the epidemic size by less than 10% when the R was similar to that of COVID-19 (ie, 2·5–3·5).48 Reviews also note that the benefits of school closure might be less than what have been assumed or modelled, as social contacts between children and between children and adults continue as part of informal childcare and non-school gatherings of children and young people.11 This conclusion is a particular concern for COVID-19, with its higher mortality among older people, as around 40% of the UK's grandparents provide regular childcare for their grandchildren.49
The WHO Director-General noted on March 12, 2020, that “all countries must strike a fine balance between protecting health, preventing economic and social disruption, and respecting human rights”.1 Currently, the evidence to support national closure of schools to combat COVID-19 is very weak and data from influenza outbreaks suggest that school closures could have relatively small effects on a virus with COVID-19's high transmissibility and apparent low clinical effect on school children. At the same time, these data also show that school closures can have profound economic and social consequences.
More research is urgently needed on the effectiveness of school closures and other school social distancing practices to inform policies related to COVID-19. We also need more detailed knowledge about how COVID-19 affects children and young people, as the role of school measures in reducing COVID-19 transmission depends on the susceptibility of children to infection and their infectiousness once infected.12 However, observational studies might be uninformative if closures are national and implemented at the same time as other mitigation measures. Better learning might come from countries that have instituted later or subnational closures. Modelling studies—particularly those parameterised for COVID-19 in children, and those that can consider interaction with other contextual factors (eg, timing, parents working from home, and additional social mixing as a consequence of school closures) or different strategies (national vs staged roll out)—are likely to be more informative and are urgently needed.
These findings pose a dilemma for policy makers seeking measures to protect populations. School closure presents an apparently common-sense method of dramatically reducing spread of disease and the evidence from previous influenza outbreaks appears compelling. However, policy makers need to be aware of the equivocal evidence when proposing or implementing national or regional school closures for COVID-19, given the very high costs of lengthy school closures during pandemics. Decisions about closures and their timing and length involve a series of trade-offs between conflicting factors, and a substantial loss of health-care staff to childcare duties during closures might substantially reduce any benefit to health systems and populations brought by closures of schools.50 Nonetheless, in a context of high rates of staff absence through disease, school systems will be under strain and schools remaining open only for the children of health-care and other essential workers might be a better strategy than a haphazard process of schools closing and therefore providing no childcare for any essential workers.
The scale and speed of school closures are unprecedented globally. It is unclear how long countries can maintain tight suppression measures before behavioural fatigue in the population occurs.31 Given predictions that social distancing measures might need to be in place for many months or even years,31 there is an urgent need to identify how countries can safely return students to education and parents to work. Education is one of the strongest predictors of the health and the wealth of a country's future workers, and the impact of long-term school closure on educational outcomes, future earnings, the health of young people, and future national productivity has not been quantified.
Once the number of COVID-19 cases begin to fall, the measures used to achieve suppression might evolve over time. Schools have begun to reopen in parts of China,2 and it will be essential for studies to monitor the effect of the reopening of schools on the numbers of COVID-19 cases. Examining countries that have not implemented school closures will also be important. Taiwan reopened schools in late February, 2020, relatively early in the outbreak; it has not yet initiated further large-scale closures but has been recognised to have effectively minimised spread of COVID-19. Policy makers and researchers should also look to other school social distancing interventions that are much less disruptive than full school closure and might substantially contribute to maintaining the control of this pandemic. Although strong evidence is not available for the effectiveness of these practices, they might be implementable with much less disruption, financial costs, or harms. Modelling and observational studies are urgently needed to guide policy on the opening of schools once the pandemic is under control.
Contributors
RMV conceptualised the paper, reviewed full-text articles, extracted the data, and wrote the first draft of the manuscript. Searches and screening of papers were done by SJR, HC, and JP, who were advised by CS. JW and OM also contributed to screening of papers. OM, CB, and RB helped to revise the paper and consider policy implications. All authors contributed to revision of the final version of the manuscript.
Declaration of interests
We declare no competing interests.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published text.
References
- 1.WHO WHO Director-General's opening remarks at the Mission briefing on COVID-19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mission-briefing-on-covid-19
- 2.United Nations Educational. Scientific and Cultural Organization COVID-19 educational disruption and response. 2020. https://en.unesco.org/themes/education-emergencies/coronavirus-school-closures
- 3.Jackson C, Vynnycky E, Mangtani P. The relationship between school holidays and transmission of influenza in England and Wales. Am J Epidemiol. 2016;184:644–651. doi: 10.1093/aje/kww083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eames KT, Tilston NL, White PJ, Adams E, Edmunds WJ. The impact of illness and the impact of school closure on social contact patterns. Health Technol Assess. 2010;14:267–312. doi: 10.3310/hta14340-04. [DOI] [PubMed] [Google Scholar]
- 5.Eames KT, Tilston NL, Edmunds WJ. The impact of school holidays on the social mixing patterns of school children. Epidemics. 2011;3:103–108. doi: 10.1016/j.epidem.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Hens N, Ayele GM, Goeyvaerts N, et al. Estimating the impact of school closure on social mixing behaviour and the transmission of close contact infections in eight European countries. BMC Infect Dis. 2009;9:187. doi: 10.1186/1471-2334-9-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brooks SK, Smith L, Webster R, et al. The impact of unplanned school closure on children's social contact: rapid evidence review. OSF Preprints. 2020 doi: 10.31219/osf.io/2txsr. published online March 17. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson C, Mangtani P, Vynnycky E. Public Health England; London: 2014. Impact of school closures on an influenza pandemic: scientific evidence base review. [Google Scholar]
- 9.Jackson C, Mangtani P, Hawker J, Olowokure B, Vynnycky E. The effects of school closures on influenza outbreaks and pandemics: systematic review of simulation studies. PLoS One. 2014;9 doi: 10.1371/journal.pone.0097297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bin Nafisah S, Alamery AH, Al Nafesa A, Aleid B, Brazanji NA. School closure during novel influenza: a systematic review. J Infect Public Health. 2018;11:657–661. doi: 10.1016/j.jiph.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Rashid H, Ridda I, King C, et al. Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatr Respir Rev. 2015;16:119–126. doi: 10.1016/j.prrv.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against COVID-19 and influenza in Hong Kong: an observational study. medRxiv. 2020 doi: 10.1101/2020.03.12.20034660. published online March 16. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadique MZ, Adams EJ, Edmunds WJ. Estimating the costs of school closure for mitigating an influenza pandemic. BMC Public Health. 2008;8:135. doi: 10.1186/1471-2458-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bayham J, Fenichel EP. The impact of school closure for COVID-19 on the US healthcare workforce and the net mortality effects. medRxiv. 2020 doi: 10.1101/2020.03.09.20033415. published online March 17. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keogh-Brown MR, Smith RD, Edmunds JW, Beutels P. The macroeconomic impact of pandemic influenza: estimates from models of the United Kingdom, France, Belgium and the Netherlands. Eur J Health Econ. 2010;11:543–554. doi: 10.1007/s10198-009-0210-1. [DOI] [PubMed] [Google Scholar]
- 17.Brown ST, Tai JH, Bailey RR, et al. Would school closure for the 2009 H1N1 influenza epidemic have been worth the cost?: a computational simulation of Pennsylvania. BMC Public Health. 2011;11:353. doi: 10.1186/1471-2458-11-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong ZS, Goldsman D, Tsui KL. Economic evaluation of individual school closure strategies: the Hong Kong 2009 H1N1 pandemic. PLoS One. 2016;11 doi: 10.1371/journal.pone.0147052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sobers-Grannum N, Springer K, Ferdinand E, St John J. Response to the challenges of pandemic H1N1 in a small island state: the Barbadian experience. BMC Public Health. 2010;10(suppl 1):S10. doi: 10.1186/1471-2458-10-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fong MW, Gao H, Wong JY, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerg Infect Dis. 2020;26:26. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uscher-Pines L, Schwartz HL, Ahmed F, et al. School practices to promote social distancing in K-12 schools: review of influenza pandemic policies and practices. BMC Public Health. 2018;18:406. doi: 10.1186/s12889-018-5302-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lofgren ET, Rogers J, Senese M, Fefferman NH. Pandemic preparedness strategies for school systems: is closure the only way? Ann Zool Fenn. 2008;45:449–458. [Google Scholar]
- 23.Ridenhour BJ, Braun A, Teyrasse T, Goldsman D. Controlling the spread of disease in schools. PLoS One. 2011;6 doi: 10.1371/journal.pone.0029640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yen MY, Chiu AW, Schwartz J, et al. From SARS in 2003 to H1N1 in 2009: lessons learned from Taiwan in preparation for the next pandemic. J Hosp Infect. 2014;87:185–193. doi: 10.1016/j.jhin.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wallinga J, Teunis P, Kretzschmar M. Using data on social contacts to estimate age-specific transmission parameters for respiratory-spread infectious agents. Am J Epidemiol. 2006;164:936–944. doi: 10.1093/aje/kwj317. [DOI] [PubMed] [Google Scholar]
- 26.Shen K, Yang Y, Wang T, et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts' consensus statement. World J Pediatr. 2020 doi: 10.1007/s12519-020-00343-7. published online February 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong GW, Li AM, Ng PC, Fok TF. Severe acute respiratory syndrome in children. Pediatr Pulmonol. 2003;36:261–266. doi: 10.1002/ppul.10367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cauchemez S, Ferguson NM, Wachtel C, et al. Closure of schools during an influenza pandemic. Lancet Infect Dis. 2009;9:473–481. doi: 10.1016/S1473-3099(09)70176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Z. Outbreak of COVID-19 in China and the country's responses. Retroviruses and Opportunistic Infections (CROI) 2020: special session SS-1: International Antiviral Society–USA; March 8–11, 2020.
- 30.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. published online March 3. [DOI] [PubMed] [Google Scholar]
- 31.Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Imperial College; London: 2020. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson ML, Hart GR, McCulloch DJ, et al. Effects of weather-related social distancing on city-scale transmission of respiratory viruses. medRxiv. 2020 doi: 10.1101/2020.03.02.20027599. published online March 3. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tan CC. SARS in Singapore—key lessons from an epidemic. Ann Acad Med Singapore. 2006;35:345–349. [PubMed] [Google Scholar]
- 34.Chan KP. Control of severe acute respiratory syndrome in Singapore. Environ Health Prev Med. 2005;10:255–259. doi: 10.1007/BF02897699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chng SY, Chia F, Leong KK, et al. Mandatory temperature monitoring in schools during SARS. Arch Dis Child. 2004;89:738–739. doi: 10.1136/adc.2003.047084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pang X, Zhu Z, Xu F, et al. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA. 2003;290:3215–3221. doi: 10.1001/jama.290.24.3215. [DOI] [PubMed] [Google Scholar]
- 37.Cowling BJ, Ho LM, Leung GM. Effectiveness of control measures during the SARS epidemic in Beijing: a comparison of the Rt curve and the epidemic curve. Epidemiol Infect. 2008;136:562–566. doi: 10.1017/S0950268807008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao CM, Chang CF, Liang HM. A probabilistic transmission dynamic model to assess indoor airborne infection risks. Risk Anal. 2005;25:1097–1107. doi: 10.1111/j.1539-6924.2005.00663.x. [DOI] [PubMed] [Google Scholar]
- 39.Becker NG, Glass K, Li Z, Aldis GK. Controlling emerging infectious diseases like SARS. Math Biosci. 2005;193:205–221. doi: 10.1016/j.mbs.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 40.O'Sullivan TL, Amaratunga C, Phillips KP, et al. If schools are closed, who will watch our kids? Family caregiving and other sources of role conflict among nurses during large-scale outbreaks. Prehosp Disaster Med. 2009;24:321–325. doi: 10.1017/s1049023x00007044. [DOI] [PubMed] [Google Scholar]
- 41.Tian H, Liu Y, Li Y, et al. The impact of transmission control measures during the first 50 days of the COVID-19 epidemic in China. medRxiv. 2020 doi: 10.1101/2020.01.30.20019844. published online March 10. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions for containing the COVID-19 outbreak. medRxiv. 2020 doi: 10.1101/2020.03.03.20029843. published online March 13. (preprint). [DOI] [Google Scholar]
- 43.Prem K, Liu Y, Russel LTW, et al. The effect of control strategies that reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China. medRxiv. 2020 doi: 10.1101/2020.03.09.20033050. published online March 12. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kwok KO, Li KK, Chan HHH, et al. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. medRxiv. 2020 doi: 10.1101/2020.02.26.20028217. published online February 27. (preprint). [DOI] [Google Scholar]
- 45.Huang C, Liu X, Sun S, et al. Insights into the transmission of respiratory infectious diseases through empirical human contact networks. Sci Rep. 2016;6 doi: 10.1038/srep31484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chow CB. Post-SARS infection control in the hospital and clinic. Paediatr Respir Rev. 2004;5:289–295. doi: 10.1016/j.prrv.2004.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vynnycky E, Edmunds WJ. Analyses of the 1957 (Asian) influenza pandemic in the United Kingdom and the impact of school closures. Epidemiol Infect. 2008;136:166–179. doi: 10.1017/S0950268807008369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Age UK. 5 million grandparents take on childcare responsibilities. 2017. https://www.ageuk.org.uk/latest-news/articles/2017/september/five-million-grandparents-take-on-childcare-responsibilities/
- 50.House T, Baguelin M, Van Hoek AJ, et al. Modelling the impact of local reactive school closures on critical care provision during an influenza pandemic. Proc Biol Sci. 2011;278:2753–2760. doi: 10.1098/rspb.2010.2688. [DOI] [PMC free article] [PubMed] [Google Scholar]