Abstract
Objective
Although acute coronary syndrome (ACS) is an uncommon entity in young patients, it constitutes an important problem due to the devastating effects of the disease on the more active lifestyle of young patients. At present, there are no guidelines regarding the prevention of ACS in young patients.
Methods
We performed a retrospective study of ACS patients between 2014 and 2017. Epidemiological data, clinical findings, and short-term outcomes were evaluated between young ACS patients (≤50 years old) and elderly ACS patients (>50 years old).
Results
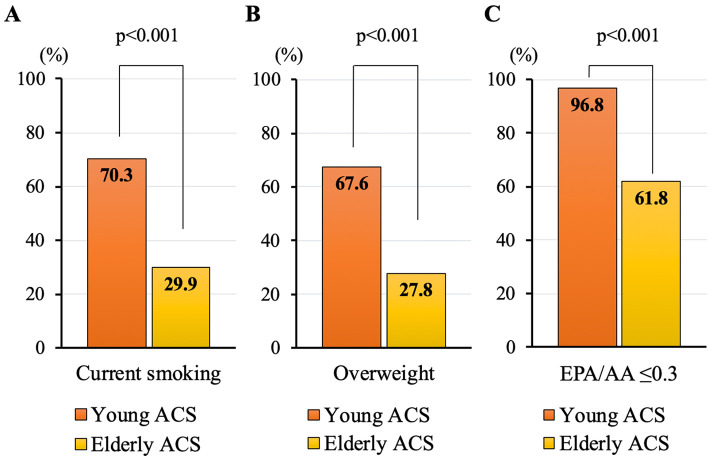
Of a total of 361 consecutive ACS patients, 37 were young ACS patients (10.2%). Compared with elderly ACS patients, young ACS patients showed a higher prevalence of males (94.6% vs. 73.8%, p<0.001), current smoking (70.3% vs. 29.9%; p<0.001), and overweight persons (67.6% vs. 27.8%, p<0.001). The eicosapentaenoic acid (EPA)/arachidonic acid (AA) ratio was significantly lower in young ACS patients than in elderly ACS patients [0.17 (0.12-0.25) vs. 0.25 (0.18-0.37), p=0.002]. The prevalence of cardio-pulmonary arrest and percutaneous cardiopulmonary support use was higher in young ACS patients than in elderly ACS patients (24.3% vs. 8.6%, p=0.003, 16.2% vs. 3.1%, p<0.001).
Conclusion
The features were markedly different between young ACS patients and elderly ACS patients. In young ACS patients, smoking, being overweight, and a low EPA/AA ratio were distinctive risk factors, and more serious clinical presentations were observed at the onset of ACS than in older patients.
Keywords: acute coronary syndrome, young patients, smoking, EPA/AA, cardiac arrest
Introduction
Coronary heart disease remains a major cause of death and disability in all regions of the world (1). Although acute coronary syndrome (ACS) primarily occurs in the older age group, younger people can also be affected, and the number of ACS in younger people has been gradually increasing (2). Furthermore, it constitutes an important problem for patients and treating physicians due to the devastating effects of the disease on the more active lifestyle of younger patients. However, there are currently no guidelines or consensus regarding the prevention and treatment of ACS in young patients.
In the present study, we compared the clinical pictures of ACS in young patients with those of elderly patients to help determine the optimal prevention and treatment strategies.
Materials and Methods
Study population
This study was designed as a single-center retrospective study to evaluate the predictive factors and clinical characteristics of ACS in young patients. We analyzed the data of consecutive patients with ACS who underwent percutaneous coronary intervention (PCI) for de novo native coronary artery lesions between January 2014 and December 2017 at Aichi Medical University. ACS included ST segment elevation myocardial infarction, non-ST segment elevation myocardial infarction, or unstable angina. Patients <50 years old were classified as young ACS patients, while those ≥50 years old were classified as elderly ACS patients.
Procedures and coronary risk factors
PCI was performed according to the standard techniques. Stenting strategy (stent type, stent size, direct stenting, or non-stent strategy), thrombus aspiration or distal protection, and post-dilatation were left to the operator's discretion. Before or during PCI, all patients were administered 200 mg of aspirin and a loading dose of a P2Y12 inhibitor (300 mg of clopidogrel or 20 mg of prasugrel). On the day after the loading dose, a maintenance dose of dual antiplatelet therapy [aspirin 100 mg and a P2Y12 inhibitor (75 mg of clopidogrel or 3.75 mg of prasugrel)] was administered. Hypertension was defined as a medical history of systemic hypertension or the use of antihypertensive treatment. Dyslipidemia was defined as a previous diagnosis of dyslipidemia or the use of a lipid-lowering treatment. Overweight was defined as having a body mass index (BMI) ≥25 kg/m2 based on the proposed classification by the WHO (3). For the short-term outcome, the all-cause mortality within 30 days after the index PCI was evaluated.
Statistical analyses
All statistical analyses were performed with the SPSS software program (version 22.0; IBM, Armonk, USA). Data are expressed as the mean ± standard deviations or as medians and interquartile ranges with differences (95% confidence intervals). Categorical variables are expressed as frequencies (%). The normality of distribution was tested by the Kolmogorov-Smirnov test. Continuous variables were compared using the unpaired Student's t-test, and categorical variables were compared using the chi-squared or Fisher's exact tests where appropriate. Mann-Whitney U tests were performed for non-parametric data. Statistical significance was assumed at a probability (p) value of <0.05.
Results
Patient characteristics
A total of 361 consecutive ACS patients were evaluated in the present study. Of these, 37 were young ACS patients, accounting for 10.2% of total ACS patients, and the remaining 324 (89.8%) were elderly ACS patients (Supplementary material 1). The proportion of men was predominantly higher among the young ACS patients than among the elderly ACS patients (94.6% vs. 73.8%, p<0.001). In terms of conventional risk factors, there were no significant differences in the prevalence of hypertension, diabetes, and dyslipidemia between the two groups (Table 1). The prevalence of current smoking was significantly higher among young ACS patients than among elderly ACS patients (Fig. 1). Regarding anthropometric measurements, in young ACS patients, the BMI was significantly higher (27.8±4.7 kg/m2 vs. 23.0±3.8 kg/m2, p<0.001) as was the prevalence of overweight than in elderly ACS patients (Fig. 1). Regarding the medications administered before admission, angiotensin receptor blockers, Ca-channel antagonists, and antiplatelet agents were more commonly used in elderly ACS patients than in young ACS patients (Supplementary material 2).
Table 1.
Baseline Characteristics.
| Young ACS (n=37) |
Elderly ACS (n=324) |
p | ||||
|---|---|---|---|---|---|---|
| Age, years | 44.9±4.1 | 71.1±9.8 | <0.001 | |||
| Male gender | 35 (94.6) | 239 (73.8) | 0.005 | |||
| Hypertension | 17 (45.9) | 194 (59.9) | 0.10 | |||
| Diabetes | 11 (29.7) | 96 (29.6) | 0.99 | |||
| Dyslipidemia | 16 (43.2) | 173 (53.4) | 0.24 | |||
| Current smoker | 26 (70.3) | 97 (29.9) | <0.001 | |||
| Hemodialysis | 1 (2.7) | 10 (3.1) | 0.90 | |||
| Previous myocardial infarction | 3 (8.1) | 22 (6.8) | 0.76 | |||
| Height, cm | 170.2±5.5 | 161.5±9.4 | <0.001 | |||
| Body weight, kg | 80.2±13.9 | 60.5±13.3 | <0.001 | |||
| Body mass index, kg/m2 | 27.8±4.7 | 23.0±3.8 | <0.001 | |||
| HDL-cholesterol, mg/dL | 38.4±7.1 | 42.7±12.4 | 0.02 | |||
| LDL-cholesterol, mg/dL | 104.7±30.9 | 101.4±31.6 | 0.82 | |||
| Triglyceride, mg/dL | 156 (114-198) | 102 (73-138) | <0.001 | |||
| HbA1c, % | 6.5±1.8 | 6.3±0.9 | 0.17 | |||
| CRP, mg/dL | 0.17 (0.08-0.35) | 0.18 (0.08-0.59) | 0.64 | |||
| EPA, μg/mL | 33.8 (27.0-46.6) | 47.2 (30.4-66.0) | 0.02 | |||
| DHA, μg/mL | 112.7 (84.9-126.5) | 123.8 (101.4-156.0) | 0.02 | |||
| AA, μg/mL | 211.9 (168.4-250.3) | 182.2 (149.5-217.7) | 0.01 | |||
| EPA/AA ratio | 0.17 (0.12-0.25) | 0.25 (0.18-0.37) | 0.002 |
Values are mean±SD, n (%), or median (interquartile range).
ACS: acute coronary syndrome, EPA: eicosapentaenoic acid, DHA: docosahexaenoic acid, AA: arachidonic acid
Figure 1.
Distinctive risk factors associated with ACS in young patients. (A) Prevalence of current smoking between young ACS patients and elderly ACS patients. (B) Prevalence of overweight between young ACS patients and elderly ACS patients. (C) Prevalence of EPA/AA ≤0.3 between young ACS patients and elderly ACS patients. ACS: acute coronary syndrome, EPA: eicosapentaenoic acid, AA: arachidonic acid
Laboratory findings
Low-density lipoprotein cholesterol levels were similar between the two groups. High-density lipoprotein cholesterol levels were significantly lower and triglycerides significantly higher in young ACS patients than in elderly ACS patients [Table 1; 38.4±7.1 mg/dL vs. 42.7±12.4 mg/dL, p=0.02; 156 (114-198) mg/dL vs. 102 (73-138) mg/dL, p<0.001, respectively]. The HbA1c values were similar between the two groups. Serum eicosapentaenoic acid (EPA) and serum docosahexaenoic acid were significantly lower and serum arachidonic acid (AA) significantly higher in young ACS patients than in elderly ACS patients. Consequently, the EPA/AA ratio was significantly lower in young ACS patients than in elderly ACS patients [0.17 (0.12-0.25) vs. 0.25 (0.18-0.37), p=0.002]. The prevalence of patients with an EPA/AA ratio ≤0.3 was significantly higher in young ACS patients than in elderly ACS patients (Fig. 1).
Clinical presentations
Angiographic findings and clinical presentations are shown in Table 2. There was no significant difference in the classification of ACS (ST segment elevation myocardial infarction, non-ST segment elevation myocardial infarction, or unstable angina) between the two groups. Single-vessel disease predominated in young ACS patients (83.8%), whereas it was found in approximately half of the elderly ACS patients (51.5%). Regarding the clinical presentations, more serious conditions were observed in young ACS patients than in elderly ACS patients. Patients with a higher Killip class were more frequently observed among young ACS patients than among elderly ACS patients. The prevalence of patients with cardio-pulmonary arrest (CPA) on arrival as well as those requiring percutaneous cardiopulmonary support (PCPS) was significantly higher among young ACS patients than among elderly ACS patients (Fig. 2). Even after PCI, patients with a lower thrombolysis in myocardial infarction (TIMI) flow grade were more frequently observed among young ACS patients than among elderly ACS patients. While the difference was not statistically significant, the 30-day mortality was numerically higher in young ACS patients than in elderly ACS patients.
Table 2.
Clinical Presentations.
| Young ACS (n=37) |
Elderly ACS (n=324) |
p | ||||
|---|---|---|---|---|---|---|
| Clinical presentation | 0.47 | |||||
| STEMI | 30 (81.1) | 211 (65.1) | ||||
| NSTEMI | 2 (5.4) | 25 (7.7) | ||||
| UAP | 5 (13.5) | 88 (27.2) | ||||
| Systolic blood pressure, mmHg | 139.6±27.8 | 147.0±29.6 | 0.24 | |||
| Killip classification | <0.001 | |||||
| Class I | 23 (62.2) | 269 (83.0) | ||||
| Class II | 1 (2.7) | 10 (3.1) | ||||
| Class III | 1 (2.7) | 16 (4.9) | ||||
| Class IV | 12 (32.4) | 29 (9.0) | ||||
| Vessel related to the ACS | 0.22 | |||||
| Left anterior descending artery | 22 (59.5) | 137 (42.3) | ||||
| Left circumflex artery | 2 (5.4) | 45 (13.9) | ||||
| Right coronary artery | 13 (35.1) | 129 (39.8) | ||||
| Left main artery | 0 (0) | 12 (3.7) | ||||
| Bypass graft | 0 (0) | 1 (0.3) | ||||
| No. of affected vessels | 0.01 | |||||
| 1 | 31 (83.8) | 167 (51.5) | ||||
| 2 | 6 (16.2) | 103 (31.8) | ||||
| 3 | 0 (0) | 54 (16.7) | ||||
| TIMI flow grade before PCI | 0.07 | |||||
| 0 | 23 (62.2) | 146 (45.1) | ||||
| I | 0 (0) | 39 (12.0) | ||||
| II | 6 (16.2) | 48 (14.8) | ||||
| III | 8 (21.6) | 91 (28.1) | ||||
| TIMI flow grade after PCI | <0.001 | |||||
| 0 | 1 (2.7) | 0 (0) | ||||
| I | 3 (8.1) | 0 (0) | ||||
| II | 3 (8.1) | 16 (4.9) | ||||
| III | 30 (81.1) | 308 (95.1) | ||||
| Maximum CK, IU/L | 2,135 (792-5,383) | 1,154 (307-2,762) | <0.001 | |||
| 30-day mortality | 5 (13.5) | 22 (6.8) | 0.14 |
Values are mean±SD or n (%).
STEMI: ST segment elevation myocardial infarction, NSTEMI: non-ST segment elevation myocardial infarction, UAP: unstable angina, ACS: acute coronary syndrome, TIMI: thrombolysis in myocardial infarction, PCI: percutaneous coronary intervention, IABP: intra-aortic balloon pump counterpulsation, PCPS: percutaneous cardiopulmonary support
Figure 2.
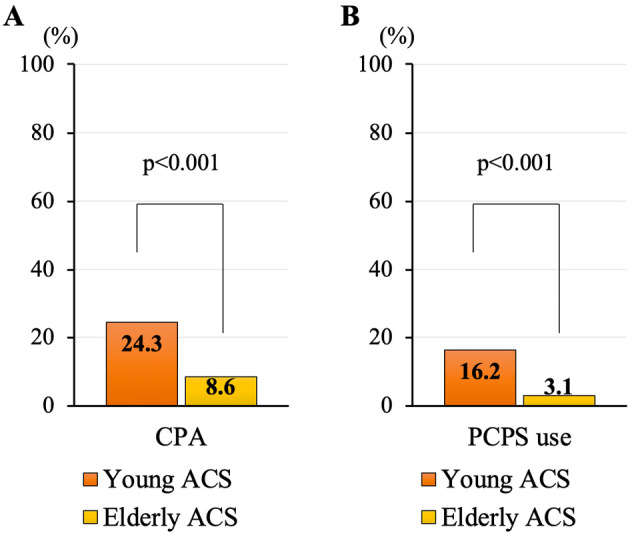
Prevalence of CPA on arrival and PCPS use. (A) Prevalence of CPA on arrival between young ACS patients and elderly ACS patients. (B) Prevalence of PCPS use between young ACS patients and elderly ACS patients. CPA: cardio-pulmonary arrest, PCPS: percutaneous cardiopulmonary support, ACS: acute coronary syndrome
Discussion
The present study highlighted the differing features between young and elderly ACS patients. The main findings were as follows: 1) a higher prevalence of men, current smokers, and overweight individuals was observed among young ACS patients; 2) the EPA/AA ratio was lower in young ACS patients than in older ones; and 3) despite multivessel diseases being uncommon, serious conditions were more frequently observed in young ACS patients than in older ones.
Although ACS has a tragic impact on the daily life of younger patients, there are currently no guidelines or consensus regarding the prevention and treatment of ACS in this population. Furthermore, there have been almost no large-scale trials recently focusing on young ACS patients. Under these circumstances, the present study might therefore provide a roadmap for the more effective prevention and management of young ACS patients.
ACS is generally known to occur more often in men than in women (4). In the present study as well, an overwhelming majority of young ACS patients were men (94.6%), which is consistent with the high prevalence of men reported in the Framingham Heart Study (5). It has also been well established that cigarette smoking is a powerful risk factor for coronary artery disease (6,7). Cigarette smoking promotes vascular endothelial dysfunction and inflammation, resulting in atherosclerosis progression and changes in plaque composition (8,9). In public settings, the smoking rate is higher among younger people than older people, and Japan Tobacco reported that the smoking rate of Japanese men in their 30s and 40s was around 35% (10). The smoking rate in young ACS patients (70.3%) in the present study is still higher than in the general population. Being overweight was also found to be characteristic of young ACS patients (67.6%) in this study and is widely recognized as a risk factor for coronary heart disease in the elderly. An autopsy study demonstrated that a high BMI was associated with both fatty streaks and raised coronary atherosclerotic lesions in young men (11).
Of note, however: hypertension, diabetes, and dyslipidemia were not distinctive features in this population when compared with elderly ACS patients. Laboratory findings showed that young ACS patients had lower high-density lipoprotein (HDL) cholesterol levels and higher triglyceride levels than elderly ACS patients, which was consistent with the results of a previous study (12). The EPA/AA ratio was also a contributor to ACS in young patients, and almost all young ACS patients (96.8%) showed an EPA/AA ratio ≤0.3. Several epidemiologic studies have shown that a lower EPA/AA ratio was associated with unstable plaque composition (13-15), cardiovascular events (including ACS) (16-18) and fatal arrhythmic events in the early phase of AMI (19). EPA has beneficial effects on multiple atherosclerotic processes, from protecting against endothelial dysfunction to reducing plaque formation, inflammation, and vulnerability (20-23). In the present study, elderly ACS patients also showed low EPA/AA ratios [0.25 (0.18-0.37)], while young ACS patients showed still lower EPA/AA ratios [0.17 (0.12-0.25)], representing an even higher risk of ACS in young patients. The EPA/AA ratio generally increases with age (24) due to differences in the consumption of dietary fish and age-related changes in serum fatty acid metabolism (25). Therefore, we cannot rule out the possibility that a lower EPA/AA ratio in young ACS patients represents the general findings in young people. This result is in line with the findings of a previous study that showed a reduced EPA/AA ratio as a contributor to the early onset of ACS (26).
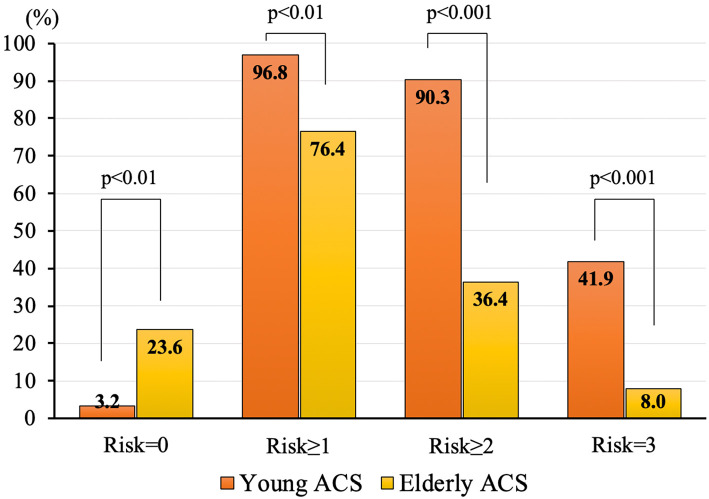
Ultimately, the present study extracted three modifiable risk factors (current smoking, being overweight and a low EPA/AA ratio) as distinctive features of young ACS patients. The prevalence of these three cumulative risk factors is indicated in Fig. 3. It is noteworthy that about 90% of young ACS patients had multiple risk factors, while only 40% of elderly ACS patients had multiple risk factors. From a practical point of view, our results suggest that the modification of these risk factors can be expected to prevent the onset of ACS in younger populations. This hypothesis needs to be investigated through prospective interventional trials in the future.
Figure 3.
Prevalence of cumulative three risk factors (current smoking, overweight and EPA/AA ≤0.3). The prevalence of three cumulative risk factors (current smoking, overweight and EPA/AA ≤0.3) in both young ACS patients and elderly ACS patients is shown. Patients with two or more risk factors accounted for 90.3% of young ACS patients and 36.4% of elderly ACS patients. Conversely, patients with no risk factors accounted for only 3.2% of young ACS patients. ACS: acute coronary syndrome, EPA: eicosapentaenoic acid, AA: arachidonic acid
Despite the number of coronary lesions being fewer, a higher Killip class and a higher prevalence of CPA and PCPS use were observed in young ACS patients than in older patients. Previous studies have shown a younger age to be significantly associated with the occurrence of life-threatening arrhythmia in the setting of acute myocardial infarction (27,28). The absence of angina before the onset of ACS, which is a characteristic finding in young ACS patients (29), is also associated with life-threatening arrhythmia (27).
Study limitations
Several limitations associated with the present study warrant mention. This was a single-center study with a relatively small population, which might have resulted in the lack of statistical power. Consequently, the present study might have missed important features of young ACS patients. In addition, this was a post-hoc analysis; the results are therefore hypothesis-generating. Larger prospective studies are warranted to validate our results.
Conclusion
Young ACS patients present with markedly different features from those seen in elderly ACS patients. In young ACS patients, smoking, being overweight, and a low EPA/AA ratio were distinctive risk factors, and more serious clinical presentations were observed at the onset of ACS.
The authors state that they have no Conflict of Interest (COI).
Supplementary Materials
Of the 361 ACS patients, 37 were young ACS patients, accounting for 10.2% of total ACS patients, and the remaining 324 (89.8%) were elderly ACS patients. The proportion of men among young ACS patients was 94.6%, and that among elderly ACS patients was 73.8%. ACS = acute coronary syndrome.
Acknowledgement
We thank the patients who participated in the present study.
References
- 1. Roth GA, Johnson C, Abajobir A, et al. . Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 70: 1-25, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cui Y, Hao K, Takahashi J, et al. . Age-specific trends in the incidence and in-hospital mortality of acute myocardial infarction over 30 years in Japan- report from the Miyagi AMI registry study. Circ J 81: 520-528, 2017. [DOI] [PubMed] [Google Scholar]
- 3. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894: i-xii, 1-253, 2000. [PubMed] [Google Scholar]
- 4. Mozaffarian D, Benjamin EJ, Go AS, et al. . Executive summary: heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 133: 447-454, 2016. [DOI] [PubMed] [Google Scholar]
- 5. Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med 311: 1144-1147, 1984. [DOI] [PubMed] [Google Scholar]
- 6. Yagi H, Komukai K, Hashimoto K, et al. . Difference in risk factors between acute coronary syndrome and stable angina pectoris in the Japanese: smoking as a crucial risk factor of acute coronary syndrome. J Cardiol 55: 345-353, 2010. [DOI] [PubMed] [Google Scholar]
- 7. JCS Joint Working Group, Japanese Society for Oral Health, Japanese Society of Oral and Maxillofacial Surgeons, et al. Guidelines for Smoking Cessation (JCS 2010)-digest version. Circ J 76: 1024-1043, 2012. [DOI] [PubMed] [Google Scholar]
- 8. Chalon S, Moreno H Jr, Benowitz NL, Hoffman BB, Blaschke TF. Nicotine impairs endothelium-dependent dilatation in human veins in vivo. Clin Pharmacol Ther 67: 391-397, 2000. [DOI] [PubMed] [Google Scholar]
- 9. Kumagai S, Amano T, Takashima H, et al. . Impact of cigarette smoking on coronary plaque composition. Coron Artery Dis 26: 60-65, 2015. [DOI] [PubMed] [Google Scholar]
- 10. JT's annual survey finds 17.9% of Japanese adults are smokers [Internet]. [cited 2019 Nov 1]. Available from: https://www.jt.com/media/news/2018/pdf/20180730_02.pdf
- 11. McGill HC Jr, McMahan CA, Herderick EE, et al. . Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 105: 2712-2718, 2002. [DOI] [PubMed] [Google Scholar]
- 12. Lipids and lipoproteins in symptomatic coronary heart disease. Distribution, intercorrelations, and significance for risk classification in 6,700 men and 1,500 women. The Bezafibrate Infarction Prevention (BIP) Study Group, Israel. Circulation 86: 839-848, 1992. [DOI] [PubMed] [Google Scholar]
- 13. Amano T, Matsubara T, Uetani T, et al. . Impact of omega-3 polyunsaturated fatty acids on coronary plaque instability: an integrated backscatter intravascular ultrasound study. Atherosclerosis 218: 110-116, 2011. [DOI] [PubMed] [Google Scholar]
- 14. Suzuki A, Ando H, Takashima H, et al. . Effects of polyunsaturated fatty acids on periprocedural myocardial infarction after elective percutaneous coronary intervention. EuroIntervention 10: 792-798, 2014. [DOI] [PubMed] [Google Scholar]
- 15. Wakabayashi Y, Funayama H, Ugata Y, et al. . Low eicosapentaenoic acid to arachidonic acid ratio is associated with thin-cap fibroatheroma determined by optical coherence tomography. J Cardiol 66: 482-488, 2015. [DOI] [PubMed] [Google Scholar]
- 16. Amano T, Matsubara T, Uetani T, et al. . Lipid-rich plaques predict non-target-lesion ischemic events in patients undergoing percutaneous coronary intervention. Circ J 75: 157-166, 2011. [DOI] [PubMed] [Google Scholar]
- 17. Domei T, Yokoi H, Kuramitsu S, et al. . Ratio of serum n-3 to n-6 polyunsaturated fatty acids and the incidence of major adverse cardiac events in patients undergoing percutaneous coronary intervention. Circ J 76: 423-429, 2012. [DOI] [PubMed] [Google Scholar]
- 18. Nishizaki Y, Shimada K, Tani S, et al. . Significance of imbalance in the ratio of serum n-3 to n-6 polyunsaturated fatty acids in patients with acute coronary syndrome. Am J Cardiol 113: 441-445, 2014. [DOI] [PubMed] [Google Scholar]
- 19. Hashimoto T, Ako J, Nakao K, et al. . A lower eicosapentaenoic acid/arachidonic acid ratio is associated with in-hospital fatal arrhythmic events in patients with acute myocardial infarction: a J-MINUET substudy. Heart Vessels 33: 481-488, 2018. [DOI] [PubMed] [Google Scholar]
- 20. Kurita A, Takashima H, Ando H, et al. . Effects of eicosapentaenoic acid on peri-procedural (type IVa) myocardial infarction following elective coronary stenting. J Cardiol 66: 114-119, 2015. [DOI] [PubMed] [Google Scholar]
- 21. Yamano T, Kubo T, Shiono Y, et al. . Impact of eicosapentaenoic acid treatment on the fibrous cap thickness in patients with coronary atherosclerotic plaque: an optical coherence tomography study. J Atheroscler Thromb 22: 52-61, 2015. [DOI] [PubMed] [Google Scholar]
- 22. Doi M, Nosaka K, Miyoshi T, et al. . Early eicosapentaenoic acid treatment after percutaneous coronary intervention reduces acute inflammatory responses and ventricular arrhythmias in patients with acute myocardial infarction: a randomized, controlled study. Int J Cardiol 176: 577-582, 2014. [DOI] [PubMed] [Google Scholar]
- 23. Endo J, Arita M. Cardioprotective mechanism of omega-3 polyunsaturated fatty acids. J Cardiol 67: 22-27, 2016. [DOI] [PubMed] [Google Scholar]
- 24. Otsuka R, Kato Y, Imai T, Ando F, Shimokata H. Higher serum EPA or DHA, and lower ARA compositions with age independent fatty acid intake in Japanese aged 40 to 79. Lipids 48: 719-727, 2013. [DOI] [PubMed] [Google Scholar]
- 25. Rees D, Miles EA, Banerjee T, et al. . Dose-related effects of eicosapentaenoic acid on innate immune function in healthy humans: a comparison of young and older men. Am J Clin Nutr 83: 331-342, 2006. [DOI] [PubMed] [Google Scholar]
- 26. Yagi S, Aihara K-i, Fukuda D, et al. . Reduced ratio of eicosapentaenoic acid and docosahexaenoic acid to arachidonic acid is associated with early onset of acute coronary syndrome. Nutr J 14: 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jabbari R, Engstrøm T, Glinge C, et al. . Incidence and risk factors of ventricular fibrillation before primary angioplasty in patients with first ST-elevation myocardial infarction: a nationwide study in Denmark. J Am Heart Assoc 4: e000738, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bougouin W, Marijon E, Puymirat E, et al. . Incidence of sudden cardiac death after ventricular fibrillation complicating acute myocardial infarction: a 5-year cause-of-death analysis of the FAST-MI 2005 registry. Eur Heart J 35: 116-122, 2014. [DOI] [PubMed] [Google Scholar]
- 29. Doughty M, Mehta R, Bruckman D, et al. . Acute myocardial infarction in the young-The University of Michigan experience. Am Heart J 143: 56-62, 2002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Of the 361 ACS patients, 37 were young ACS patients, accounting for 10.2% of total ACS patients, and the remaining 324 (89.8%) were elderly ACS patients. The proportion of men among young ACS patients was 94.6%, and that among elderly ACS patients was 73.8%. ACS = acute coronary syndrome.