A recent meta-analysis reported that a higher neutrophil-to-lymphocyte ratio (NLR), i.e. a well-known marker of systemic inflammation integrating the detrimental effects of neutrophilia and lymphopenia, is strongly associated with poorer in-hospital outcomes in patients with coronavirus disease-2019 (COVID-19) [1]. Previous studies also reported a significant association between increased NLR and the histological severity of liver fibrosis in non-alcoholic fatty liver disease (recently renamed metabolic dysfunction-associated fatty liver disease (MAFLD) [2]) [3], [4]. We therefore postulated that MAFLD might contribute to the COVID-19-induced inflammatory “storm”, and that patients with MAFLD and increased NLR at hospital admission are at greater risk for severe COVID-19 illness.
We studied a multicentre cohort of 310 patients with laboratory-confirmed COVID-19, who were consecutively hospitalised at four sites in Whenzou, Zhejiang Province (China), between January and February 2020. These patients have been included in a prior study examining the relationship between MAFLD with increased non-invasive fibrosis scores and risk of COVID-19 severity [5]. Patients with viral hepatitis, excessive alcohol consumption, active cancers or chronic pulmonary diseases were excluded. Clinical and laboratory data were collected in all patients at hospital admission, including NLR that was calculated by dividing the absolute number of neutrophils by the absolute number of lymphocytes. Obesity was diagnosed as body mass index > 25 kg/m2. Pre-existing diabetes was defined as self-reported history of disease or use of glucose-lowering medications. All patients were screened for hepatic steatosis by computed tomography and subsequently diagnosed as MAFLD, according to the recently proposed diagnostic criteria [2]. The severity of COVID-19 was assessed during hospitalisation and classified as severe and non-severe based on the current management guideline [6]. The study protocol was approved by the local ethics committees of the four hospitals. The requirement for written informed consent was waived due to the retrospective and anonymous nature of the study design.
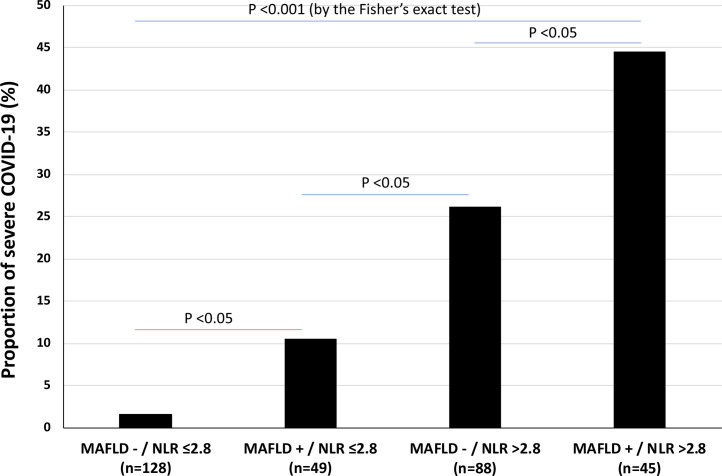
In our cohort of 310 (48.1% men; mean age 47 years) consecutive cases of COVID-19, the median values of NLR were 2.53 (inter-quartile range: 1.7–3.8), and 94 (30.3%) patients had imaging-defined MAFLD. We stratified our cohort of patients by both presence/absence of MAFLD and high/low values of NLR; we adopted a cut-point value of 2.80 that was found to be the optimal cut-point value of NLR in a ROC curve analysis, using the Youden's index, for predicting severe COVID-19 in the patient cohort.
After stratifying patients by both presence/absence of MAFLD and high/low NLR values at hospital admission, those with MAFLD and increased NLR were older and more likely to have diabetes, obesity and hypertension, and had higher serum liver enzymes, higher leucocyte and neutrophil counts, higher C-reactive protein, longer prothrombin time and higher D-dimer levels, as well as lower lymphocyte counts and lower high-density lipoprotein-cholesterol concentrations compared with their counterparts without MAFLD and normal NLR. Notably, as shown in Fig. 1 , the severity of COVID-19 illness markedly increased across the four groups of patients. Almost identical results were found when we used a different cut-off value of NLR for stratifying the COVID-19 cases, i.e., 3.2 that corresponds to the upper tertile of distribution of NLR values in the entire cohort of patients (data not shown).
Fig. 1.
Proportion of severe COVID-19 illness among patients, stratified by presence/absence of metabolic dysfunction-associated fatty liver disease (MAFLD) and values of neutrophil-to-lymphocyte ratio (NLR) at hospital admission.
In binary logistic regression analysis, compared to those without MAFLD and NLR ≤ 2.8 at hospital admission, patients with MAFLD and NLR ≤2.8 (adjusted-odds ratio [OR] 5.32, 95% confidence intervals [CI] 0.98–29.9, P = 0.053), those without MAFLD and NLR > 2.8 (adjusted-OR 17.7, 95%CI 3.89–80.6, P < 0.001), and those with MAFLD and NLR > 2.8 (adjusted-OR 25.9, 95%CI 5.32–127, P < 0.001) were associated with greater severity of COVID-19 illness, even after adjustment for age, sex, pre-existing diabetes, obesity and hypertension. In this multivariable regression model, older age (adjusted-OR 1.03, 95%CI 1.01–1.06, P < 0.05), male sex (adjusted-OR 2.63, 95%CI 1.22–5.01, P < 0.01) and hypertension (adjusted-OR 2.68, 95%CI 1.20–5.98, P < 0.01) were also independently associated with greater risk of having severe COVID-19.
Our study has some limitations, including the relatively modest sample size, the Asian ancestry of the cohort, and the lack of any data on lymphocyte subsets (by flow cytometry) and serial monitoring of NLR during the hospital stay. Despite these limitations, our study is the first to examine the differential effects of MAFLD and increased NLR on severity of COVID-19. It has been shown that increased NLR (and T lymphopenia) is strongly associated with poorer in-hospital outcomes amongst patients with COVID-19 [1], [7], and also predicts with reasonable accuracy the fibrosis stage and other histological features of MAFLD [3], [4].
Our multicentre preliminary analysis confirms the prognostic value of NLR in hospitalised patients with COVID-19, and shows for the first time that patients with imaging-defined MAFLD and increased NLR values on admission are at substantially higher risk of severe illness from COVID-19, irrespective of age, sex and metabolic comorbidities. It is possible that the presence of MAFLD with increased NLR exacerbates the virus-induced inflammatory “storm”, possibly through the hepatic release of several proinflammatory cytokines, thereby contributing mechanistically to severe COVID-19 illness. However, further studies in larger Asian and non-Asian cohorts of COVID-19 patients are needed to better elucidate the link between MAFLD and COVID-19 severity.
Funding Sources
MHZ is supported by grants from the National Natural Science Foundation of China (81500665). CDB is supported in part by the Southampton NIHR Biomedical Research Centre (IS-BRC-20004), UK. GT is supported in part by grants from the School of Medicine, University of Verona, Verona, Italy.
Author contributions
Ming-Hua Zheng contributed to the study concept, design and study supervision; Xiao-Bo Wang, Hua-Dong Yan, Qing-Feng Sun, Ke-Hua Pan, Kenneth I. Zheng, and Yong-Ping Chen all focused on the acquisition of data; Giovanni Targher contributed to the analysis and interpretation of data, and drafting of the manuscript; Alessandro Mantovani focused on both the analysis and interpretation of data and critical revision of the manuscript for important intellectual content, while Christopher D. Byrne, Mohammed Eslam, and Jacob George all contributed to the latter only.
Disclosure of interest
The authors declare that they have no competing interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.diabet.2020.06.001.
Appendix A. Supplementary data
References
- 1.Lagunas-Rangel F.A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. J Med Virol. 2020 doi: 10.1002/jmv.25819. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020 doi: 10.1016/j.jhep.2020.03.039. [Epub ahead of print; pii: S0168-8278(20)30201-4] [DOI] [PubMed] [Google Scholar]
- 3.Alkhouri N., Morris-Stiff G., Campbell C., Lopez R., Tamimi T.A., Yerian L. Neutrophil to lymphocyte ratio: a new marker for predicting steatohepatitis and fibrosis in patients with non-alcoholic fatty liver disease. Liver Int. 2012;32:297–302. doi: 10.1111/j.1478-3231.2011.02639.x. [DOI] [PubMed] [Google Scholar]
- 4.Peng Y., Li Y., He Y., Wei Q., Xie Q., Zhang L. The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: a systematic review. Expert Rev Gastroenterol Hepatol. 2018;12:503–513. doi: 10.1080/17474124.2018.1463158. [DOI] [PubMed] [Google Scholar]
- 5.Targher G., Mantovani A., Byrne C.D., Wang X.B., Yan H.D., Sun Q.F. Risk of severe illness from COVID-19 in patients with metabolic dysfunction-associated fatty liver disease and increased fibrosis scores. Gut. 2020 doi: 10.1136/gutjnl-2020-321611. [Online ahead of print; gutjnl-2020-321611] [DOI] [PubMed] [Google Scholar]
- 6.National Health Commission & State Administration of Traditional Chinese Medicine . 2020. Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7) [EB/OL; 2020.03.03] [Google Scholar]
- 7.Liu Y., Du X., Chen J., Jin Y., Peng L., Wang H.H.X. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalised patients with COVID-19. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.002. [pii: S0163-4453(20)30208-5; Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.