Abstract
The COVID-19 pandemic has raised ethical questions for the cardiovascular leader and practitioner. Attention has been redirected from a system that focuses on individual patient benefit toward one that focuses on protecting society as a whole. Challenging resource allocation questions highlight the need for a clearly articulated ethics framework that integrates principled decision making into how different cardiovascular care services are prioritized. A practical application of the principles of harm minimisation, fairness, proportionality, respect, reciprocity, flexibility, and procedural justice is provided, and a model for prioritisation of the restoration of cardiovascular services is outlined. The prioritisation model may be used to determine how and when cardiovascular services should be continued or restored. There should be a focus on an iterative and responsive approach to broader health care system needs, such as other disease groups and local outbreaks.
Résumé
La pandémie de COVID-19 soulève des questions éthiques pour les dirigeants et les praticiens du domaine cardiovasculaire. En effet, nous sommes passés d’un système axé sur les bienfaits pour les patients individuels à un contexte où il faut protéger l’ensemble de la population. Les questions difficiles d’allocation des ressources qui se posent font ressortir la nécessité d’un cadre éthique clair intégrant un processus décisionnel fondé sur des principes pour l’établissement de la priorité des différents services de soins cardiovasculaires. Les auteurs proposent une application pratique des principes de réduction des méfaits, d’équité, de proportionnalité, de respect, de réciprocité, de souplesse et de justice procédurale, ainsi qu’un modèle pour établir les priorités en matière de rétablissement des services de soins cardiovasculaires. Ce modèle d’établissement des priorités peut servir à déterminer comment et quand les services de soins cardiovasculaires doivent être maintenus ou rétablis. L’accent devrait être mis sur une approche itérative et réactive pour répondre aux besoins plus larges du système de soins de santé, par exemple en ce qui concerne les autres groupes de maladies et les flambées locales.
The Problem
The COVID-19 pandemic has presented unprecedented ethical challenges over the past several months. Ethicists nationwide face calls and e-mails from health care system administrators, department heads, and individual practitioners requesting guidance around morally fraught, sometimes heart-wrenching, decisions. These enquiries are unique and varied, evolving as the pandemic response transitions between stages. Difficult questions that have been repeatedly raised include:
-
•
What constitutes urgent?
-
•
Which patient should come first?
-
•
How should we ration scarce resources, such as testing kits and personal protective equipment (PPE)?
-
•
What is our duty to provide care in the face of inadequate PPE?
-
•
Is it reasonable to refuse being redeployed to a high-risk unit?
-
•
When, if ever, is it permissible to deny provision of life-saving care that is usually readily available?
-
•
How should we prioritise restoration of services and procedures as capacity is reinstated?
For the cardiovascular practitioner and leader, resource allocation during the COVID-19 pandemic amounts to managing 2 simultaneous threats: disease burden from COVID-19 itself, and the danger of increased non-COVID cardiac mortality. For example, an approximately 40% drop in ST-segment-elevation myocardial infarction–related cardiac catheterisation lab activation was reported during initial pandemic response stages.1 The long-term effects of decreased elective outpatient cardiac procedural volumes remains unclear, but will foreseeably result in a backlog that may take years to clear, with resulting excess morbidity and mortality.
These questions, arising at all levels in the health care system, highlight the need for a clearly articulated ethics framework in decision making. Decisions must be robust (well considered), reasonable (grounded in evidence and based on relevant factors), transparent (clear and open decisions and decision-making process), and just (resources are distributed equitably).2 The focus shifts from a traditional autonomy-based clinical ethics practice to one that applies a public health lens. Attention must be redirected from a system prioritising individual patient benefit and choice toward one geared toward society as a whole—a move from autonomy to solidarity. Consequently, service delivery is altered, ultimately affecting some clinical areas more significantly than others.
Tension also exists between the overarching public health perspective and the cardiovascular healthcare provider community. This is exemplified by the deferral of elective cardiovascular care in the interest of the public health imperative. Deferral, and gradual resumption of services at significantly lower volume, forces providers and leaders to make unbiased decisions concerning patient and procedural urgency. Eventually, another shift in priority will occur as the pandemic abates and services are restored in the interest of public cardiovascular health.
In the coming months, there exists the potential for an asymmetric impact in cardiovascular care provision, as some services may be deemed more essential than others. Decisions must be made on service reintroduction, despite insufficient quantitative estimates of consequences. Services will be restored with varying timing and priority, resulting in differential burden and impact on certain groups, including longer waits and limited access to some services. This creates doubt and stress, especially if the evidence or process by which decisions are made is not robust.
The Ethical Framework
To ensure that any impact on the public, patients and families, providers, and the healthcare system is just and reasonable, clarity regarding ethical principles relevant to public health and resource allocation decision making is warranted. These principles are not high-level theoretical concepts. Rather, they should be considered and applied at all levels of decision making during the pandemic, including at the governmental, health care system, and individual practitioner levels. The principles are not hierarchic, instead their relative importance is determined according to the question at hand. Table 1 outlines these principles and provides examples of their application in the cardiovascular setting during the COVID-19 pandemic.
Table 1.
Ethical principles and their application in the cardiac setting during COVID-19
| Principle | Definition | Application | Example |
|---|---|---|---|
| Minimize harm (non-maleficence/ beneficence) | Society should take steps to protect the public from harm and minimize physical, psychological, social, and economic impacts of a pandemic | Ensure there exists reserve capacity in critical care settings to accommodate any surge related to future waves of disease transmission | Cardiac surgery volumes should be balanced by weighing patient acuity and waiting lists against the need for critical care beds and ventilators |
| Fairness (distributive justice) | Persons matter equally and should have equal access to resources. However, those with greater needs and who stand to gain the most (utility), as well as services that provide the greatest benefit to the greatest numbers (efficiency), should be prioritized. Care must be taken to avoid placing undue burden on particular segments of the population or further perpetuating systemic or structural inequities | Surgeries, invasive and noninvasive interventions, as well as diagnostic testing, that are likely to benefit more people to a greater degree are prioritized over procedures that will benefit fewer people to a lesser degree | The resource investment required to operate high-volume ambulatory heart failure clinics should be balanced against those required for aggressive therapies, such as mechanical circulatory support or cardiac transplant, which greatly benefit a few |
| Respect for persons (autonomy) | Autonomous, informed choice, as well as cultural safety, privacy, and confidentiality, must be respected and promoted | Explore individual patients’ perspective, including goals and assessment of quality of life | Those patients who do not want to attend a recommended procedure or test due to concerns over COVID-19 transmission and infection should not be prejudiced against either for acute care during the pandemic, or for regular care once the pandemic abates |
| Proportionality | Decisions should be proportional to balance potential benefits of an activity against risks of harm. These calculations must be evidence-based and data-driven, wherever possible | Risks of exacerbating nosocomial COVID-19 spread and precipitating an unmanageable increase in pressure on healthcare resources should be considered | Exposing an elderly patient or a patient with significant comorbid disease burden to a COVID-rich environment, where adequate risk mitigation cannot be achieved, must be balanced by the potential benefit of the proposed procedure or test |
| Reciprocity | Those who are asked to take increased risks, or face undue burdens, should be supported in doing so, and harms mitigated as much as possible | Patient and provider safety should be considered when deliberating on available treatment options | Decision to perform an aerosol-generating medical procedure is balanced by sustainable access to PPE |
| Flexibility | Plans should be iterative and adapt to new evidence and public health directives | Proposals increasing access to services and associated communications must acknowledge the possibility of, and be responsive to, the ebb and flow of future COVID-19 surges | Patients and providers must be prepared for services to be abruptly altered, and the resultant reduction may not be consistent across all therapeutic areas |
| Procedural justice | Decisions should be accountable to a fair and transparent process throughout the planning and implementation stages. Stakeholders should be engaged, and decisions should be applied in a consistent manner with open communication | The decision on how to reintroduce service capacity and where resources will be allocated should be deliberate and informed by all stakeholders | The allocation of operation and procedural room access should be governed by an established set of principles |
An ethics framework is key to robust and defensible decision making. This necessitates thorough consideration of relevant ethical principles as outlined above, clear articulation of the values in tension, justification for their ranking, and adequate stakeholder engagement wherever possible.
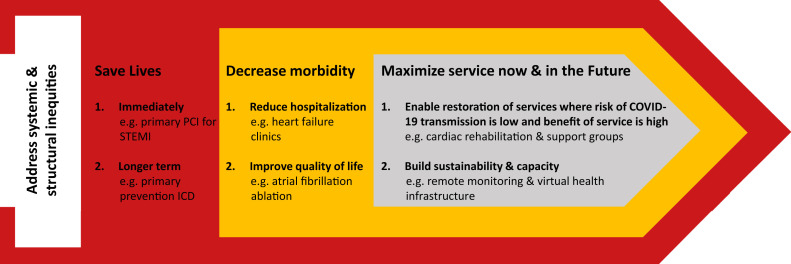
There is a strong ethically grounded rationale for prioritisation of services as the pandemic progresses. Consideration should be given to application of these principles to service restoration (Fig. 1 ). Of note, there may be overlap within prioritisation levels because some interventions result in impact at several levels. An exhaustive review of cardiac interventions and categorisation based on the type and magnitude of benefit conferred is beyond the scope of the present paper. The Canadian Cardiovascular Society (CCS) and several of its affiliate leaders created a consensus guidance document on resumption of services, jointly supported by 15 North America–based societies, that outlines a pragmatic staged approach to this challenge.3 CCS practice guidelines provide a rich source of guidance across all cardiac subspecialty domains (https://www.ccs.ca/en/guidelines/guidelines-library). They are methodologically rigorous in development, based on the highest quality data sources, and contextualised for Canadian practice. These guideline recommendations specifically attribute mortality, morbidity, quality of life, and symptomatic benefits to the full spectrum of cardiovascular interventions and are thus an important tool to inform prioritisation as outlined in Figure 1.
Figure 1.
An ethical framework for the prioritization of cardiac services during the COVID-19 pandemic.
Leadership should use the prioritisation model to determine how and when cardiovascular services should be continued or restored. This also requires transparent communication. Once implemented, the process needs to be iterative and responsive to broader health care system needs, such as other disease groups and local outbreaks. Data on the impact of delay for elective care must be quickly integrated into decision making, such that foreseen and unforeseen consequences are considered and addressed.4 This includes local and dynamic factors, such as access to testing, PPE availability, the possibility of future outbreaks, and site-specific limitations such as availability of physical infrastructure and human resources.
In the cardiovascular setting, there are already emerging data and empirically based approaches on how to quickly and safely adapt workflow and service while minimizing risks to individual patients and the broader health care system.4 , 5 These lessons must be capitalised and built on. Resource allocation policies and resultant approaches that are not attuned to these carefully considered principles will not withstand public scrutiny and may quickly become indefensible. For example, extreme caution should be used in proposing potentially discriminatory triage criteria that seek to maximize benefits by focusing purely on prioritising “healthy life years,” excluding individuals purely based on age or differential ability. Attention must be focused on minimising harm by saving lives, regardless of the perceived value or worth of that life.
Forward Facing
COVID-19 has inexorably altered health care access and utilization. It is anticipated that this will remain the case for the foreseeable future, with a corresponding impact on cardiovascular and other health outcomes. This effect will be unevenly distributed across both patient and health care provider communities. Questions regarding a clinician’s duty to provide care during a pandemic, as well as what aspects of cardiovascular care should be prioritised, need to be made using an ethical framework. In planning and case management, practitioners should be aware of local ethics resources. Ensuring transparency and impartiality in the adjudication of ethical quandaries, as systemic response evolves from the “sprint” to the “marathon” stage of COVID-19, requires broad stakeholder engagement, with clearly established processes.
Wherever possible, it is essential that patients and families, as appropriate, are involved in these decisions. In addition to being directly affected by illness, as members of the public they may also be indirectly affected by financial and other ripple effects of these decisions. Particular attention to include traditionally marginalised and underserved voices in these conversations, such as those from indigenous communities, is essential to avoid further perpetuation of systemic and structural inequities. Other key stakeholders to engage in these discussions include site and regional leaders with knowledge of cardiovascular and other specialty plans and needs, infection control experts, those with knowledge of important logistical concerns such as COVID-19 testing capacity, PPE, and pharmaceutical supply, and provincial cardiovascular care coordination bodies. Overarching operational considerations for health systems are presented in Supplemental Table S1, but the specifics of reopening must be managed at the local level, given the heterogeneity of service provision (cardiac and noncardiac) across various Canadian jurisdictions. In this regard, a highly prescriptive approach is not feasible and will not serve regional variability and context.
Decisions must also be made in alignment with public health officers and regional health authorities, such that cardiovascular care is coordinated and contextualized within the broader health system and considers the medical needs of other patient groups. Cardiovascular care is unique in that many offered services provide short-, medium-, and long-term mortality benefits. Advocacy is necessary to ensure that cardiovascular patients awaiting care are triaged with the use of appropriate decision-making frameworks. In addition, ethics frameworks and prioritisation decisions must be applied across the health care system, because consistency is key to fair and equitable service provision to engender public trust. Finally, these principles, while highlighted in the context of the pandemic, are relevant to all health care delivery during non–COVID-19 times. Ethics is not reserved for crisis situations, but should guide decision making and resource allocation even as the health system embarks on the new normal.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1316 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.06.002.
Supplementary Material
References
- 1.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Persad G., Wertheimer A., Emanuel E.J. Principles for allocation of scarce medical interventions. Lancet. 2009;373:423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 3.Wood D.A., Mahmud E., Thourani V.H. Safe reintroduction of cardiovascular services during the COVID-19 pandemic: from the North American society leadership. Can J Cardiol. 2020;36:971–976. doi: 10.1016/j.cjca.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenbaum L. The untold toll—the pandemic’s effects on patients without COVID-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 5.Hassan A., Arora R.C., Adams C. Cardiac surgery in Canada during the COVID-19 pandemic: a guidance statement from the Canadian Society of Cardiac Surgeons. Can J Cardiol. 2020;36:952–955. doi: 10.1016/j.cjca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.