Dear Editor:
Taiwanese anesthesiologist Dr. Hsien Yung Lai published his design for an aerosol box on 3/21/20. It was designed to keep physicians working in clinical environments safe during intubation, a known aerosol generating procedure, despite limited personal protective equipment (PPE) [[1], [2], [3]]. Dr. Lai shared world-wide via a Creative Commons License [1]. He designed the box two months earlier, during the COVID-19 outbreak in Wuhan, China, and found renewed interest from US physicians as surges of COVID-19 patients presented and PPE was scarce [2].
Dr. Lai's design was rapidly shared via social media and gained notoriety among US anesthesiologists. Canelli et al. demonstrated with fluorescent dye that the box was effective at trapping cough droplets, and theorized it would also protect against aerosols [4]. We discussed building aerosol boxes for our anesthesia team members on 3/23/20, built our first prototype 3/25/20, and conducted simulation testing 3/26/20. Our modifications addressed these design issues: (a) limited access for intubation assistance; (b) lack of negative pressure evacuation from the box; (c) lack of arm/sleeve protection; (d) instability on the OR table; and (e) the possibility that aerosolized virus particles could escape the box on the open/caudal end.
We modified the Taiwanese aerosol box (see Fig. 1 ). Access for another healthcare provider to manually assist during intubation was created with a side access port. We drilled a hole for a 6.5 mm endotracheal tube connector to permit suction from inside the box to the waste gas scavenger system via standard suction tubing, which can be used with/without a viricidal/bactericidal filter. Toilet flanges were added to all arm ports so sterile OR gown sleeves could be added as an extra layer of protection. Additionally, a plastic sheet, clear trash bag, cut C-arm drape, etc. can be secured with adhesive tape to the open end of the box.
Fig. 1.
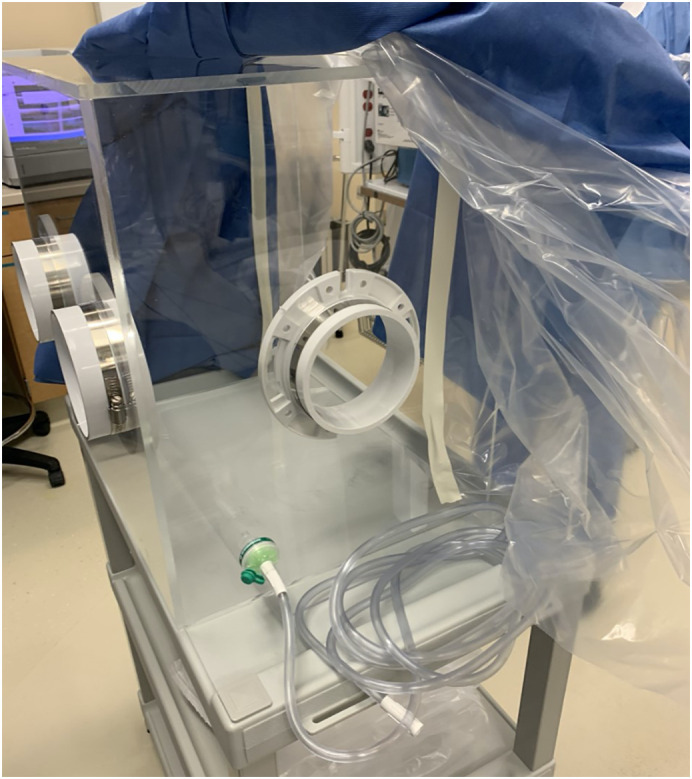
Rapid prototype of an improved aerosol box.
During the rapid improvement cycle, we switched from retail ¼″ acrylic to ⅜″ thick industrial grade. Gorilla Glue plastic epoxy was used on the prototype, creating a mechanical bond. This was not strong enough to allow the box to be moved and cleaned, and repeatedly used. To increase durability, we applied SCIGRIP Weld-on 3, which chemically bonds the acrylic pieces [5]. This product is intended for industrial use only and requires proper filtration and PPE. Thicker acrylic provided more stability; the boxes fit snugly to the OR table foam mattress headpiece and metal bars rails.
Intubations with an airway task trainer demonstrated our modifications enhanced the user experience to meet the needs of the anesthesia team, and aligned with everyday practice of anesthesiology in the US. Thus, the aerosol box did not inhibit routine airway management. It is common in our academic anesthesiology practice for someone to hand the endotracheal tube to the laryngoscopist. Adding a suction port and plastic sheet to the open-end reduced anxiety of anesthesiologists concerned with spreading aerosolized virus throughout positive pressure airflow ORs. Many anesthesiologists did not anticipate the need to wear OR gown sleeves, although they did agree it may offer an extra layer of protection. Everyone deemed the box stable on the OR table.
Prototype boxes deteriorated after 3–5 uses. Thicker acrylic boxes with industrial adhesive have endured eight weeks of clinical use. Modified boxes have been deployed to several hospitals, used successfully, and received positive feedback from end-users.
Dr. Lai created an innovative aerosol box that has been used to protect physicians around the world. Our modifications increased user satisfaction and safety by providing stability, negative pressure suction, intubation assistance port, and optional arm protection. We offer our modifications to assist colleagues manufacturing these boxes and to facilitate iterative design improvements for intubation and airway management.
Author contribution
JC and MH were instrumental in the conceptualization of the modifications and validation of rapid prototyping of the aerosol box. JC, TB, MH, RA, and SM contributed to the methodology, composition, and editing of the article, and approval of the final article for publication.
Funding statement
There is no funding nor grant for the this project.
Declaration of competing interest
There are no competing interests for any author.
Acknowledgement
We would like to acknowledge Eli Lilly & Company for their generous contribution of materials and personnel in the development of this rapid prototype in order to help protect healthcare workers around the world.
References
- 1.Lai HY. Aerosol box: Protects healthcare providers during endotracheal intubation [internet]. Hua Lian, Taiwan: Department of Anesthesiology, Mennonite Christian Hospital. Available from: https://sites.google.com/view/aerosolbox/design.
- 2.Everington K. Taiwan News. 2020. Taiwanese doctor invents device to protect US doctors against coronavirus.https://www.taiwannews.com.tw/en/news/3902435 Mar 23. Available from: [Google Scholar]
- 3.Hsien-Feng L., Lim E. Focus Taiwan. 2020. Coronavirus/Taiwanese doctor creates cheap protective device amid virus crisis.https://focustaiwan.tw/society/202003220009 Mar 22. Available from. [Google Scholar]
- 4.Canelli R., Connor C.W., Gonzalez M., Nozari A., Ortega R. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020:1–2. doi: 10.1056/NEJMc2007589. Apr 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IPS Corporation; Compton, CA: 2016. SCIGRIP weld-on 3 acrylic plastic cement. Available from https://www.tapplastics.com/uploads/pdf/PB-IPS3.pdf. [Google Scholar]


