As of April 1, 2020, more than 800 000 cases of coronavirus disease 2019 (COVID-19) had been confirmed worldwide. The death toll in Italy is approaching 12 000 people, with Spain not far behind. The USA has reported more than 164 000 cases of the disease, including more than 38 000 cases in New York City alone. There are concerns that the COVID-19 could overwhelm health-care systems worldwide. Many nations have reported a shortage of ventilators.
The UK is one of several countries to have suspended elective surgery. On March 26, Gethin Williams, a colorectal surgeon at the Royal Gwent Hospital in Newport, Wales, warned that his institution was under severe strain, with operating theatres turned into intensive care units to accommodate the influx of patients with COVID-19. “The rate at which COVID-19 is going through the Royal Gwent, there'll be no colorectal surgery for the foreseeable future”, he said. “Without treatment, some cancers could obstruct, others could metastasise.”
Oncology societies and national authorities have been quick to issue guidelines on cancer care during the pandemic. Giuseppe Curigliano (European Institute of Oncology, Milan, Italy) is a council member of the European Society for Medical Oncology (ESMO). “ESMO is taking this very seriously”, he said. “They are offering guidance to medical oncologists and giving training on how to manage patients with cancer while this pandemic goes on.” According to an analysis of Italian patients published in March, 20% of those who died from COVID-19 in the country had active cancer.
The ESMO website includes general information on COVID-19, a Q&A section, and links to useful resources. ESMO recommends that oncologists remain ready to adjust their routines. It suggests bolstering telemedicine services, reducing clinic visits, and switching to subcutaneous or oral therapies, rather than intravenous ones, when possible. There is also advice on supporting patients and on infection control.
In its guidance for managing patients with cancer requiring acute treatment, NHS England warned that certain groups are particularly vulnerable to serious illness if they become infected with severe acute respiratory syndrome coronavirus 2. These groups include individuals who are undergoing active chemotherapy or radical radiotherapy for lung cancer, and patients with cancers of the blood or bone marrow. “Different cancers produce immune suppression to different extents”, explains Richard Schilsky, chief medical officer of the American Society of Clinical Oncology (ASCO). “The blood cancers often directly compromise the immune system, so those patients are probably most at risk, whereas cancers such as colon cancer, breast cancer, and lung cancer do not typically cause immune suppression that is not treatment-related.”
Schilsky notes that standard chemotherapy regimens for most solid tumours mainly cause transient immune suppression that manifests in low white blood cell counts. “You can prop up the white blood cells using colony-stimulating factors, so these patients are probably at lower risk than the blood cancer patients”, he told The Lancet Oncology.
The pandemic poses several challenges for oncology services. Caregivers have to think about how to minimise their patients' exposure to health-care facilities. “We are seeing systems adapt to this now, with telephone and telehealth consultations, people receiving laboratory testing at facilities closer to their homes, and some evaluations being delayed”, said Schilsky. NHS England's guidance lists several possible options, including home delivery of oral medications and repeat prescriptions.
Then there are issues associated with infection. Oncologists are accustomed to dealing with such complications, but the problem with COVID-19 is that there is no specific treatment. “The risk–benefit calculus is tricky”, said Schilsky. “On the one hand, a patient might be at high risk of contracting the infection and dying from it; on the other hand, the patient might be at high risk of the cancer progressing or causing death if it is not treated appropriately.” Physicians have to assess whether treatment plans should be initiated on schedule or delayed, and if so, for how long?
NHS England stresses that individual patient decisions have to be made by multidisciplinary teams. Its guidance establishes priority groups for surgery, systemic anticancer treatments, and radiotherapy. For systemic treatments, NHS England sets out six priority levels. Patients who are in line for curative therapy with a greater than 50% chance of success are in the highest level. Patients who are awaiting non-curative therapy that is unlikely to offer palliation, tumour control, or more than 1 year's extension of life are assigned the lowest priority level. For radiotherapy, there are five levels of priority, patients with rapidly proliferating tumours with little scope for delay are in the highest group.
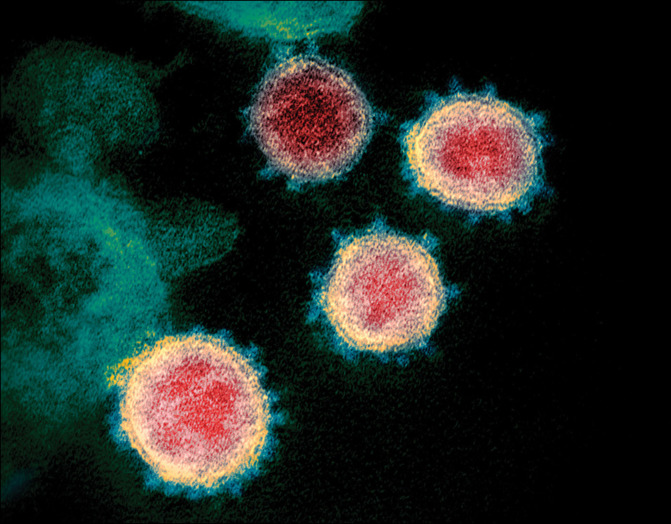
© 2020 NIAID-RML/National Institues of Health/Science Photo Library
Several other cancer societies have issued some guidance. The Society of Surgical Oncology website includes disease-site specific resources to help guide decisions in the era of COVID-19, as well as a series of podcasts from different specialists. There are information sheets on a range of malignancies, including breast cancer, colorectal cancer, endocrine cancer, and melanoma, with each subdivided into disease types, when appropriate.
In a statement issued on COVID-19, the European Society of Surgical Oncology (ESSO) advised against seeing patients older than 70 years in the clinic, unless urgent. ESSO also emphasised the importance of ensuring that the workforce does not burn out. “Rest and recuperation, as well as psychological support should be factored into planning”, the statement concluded.
The ASCO website also assembles a great deal of information on patient care and COVID-19, along with links to guidance from organisations such as the US Centers for Disease Control and Prevention and several oncology societies. ASCO has produced guidance on how practices should ready themselves for the virus; advice can be found on staffing, clinical preparedness, infection prevention and control, and patient scheduling. There are also mental health resources. Practitioners can find the tips on enhancing coping useful. The suggestions include avoiding information overload and taking a break from news and social media related to COVID-19. There is also a set of tips for enhancing mental and physical health—one suggested exercise is mindful handwashing, which could be a neat way to combine hygiene and wellbeing.
The American Society for Radiation Oncology website contains a large section on COVID-19. The organisation is putting together specific recommendations for its membership, based on the findings of a dedicated workgroup. Its website contains frequently asked questions, several of which are directly relevant to clinical decision making, and links to journal articles and relevant websites.
The American Society for Transplantation and Cellular Therapy and the European Society for Blood and Marrow Transplantation (EBMT) have both issued guidelines for COVID-19 management. The EBMT warns that the travel restrictions imposed in Europe are likely to have a serious effect on transplant activities both on the continent and beyond. “Due to the rapidly changing situation, access to a stem cell donor might be restricted either due to the donor becoming infected, logistical reasons at the harvest centres in the middle of a strained health-care system, or travel restrictions across international borders”, note the EBMT guidelines. “It is therefore strongly recommended to have secured stem cell product access by freezing the product before start of conditioning and, in situations when this is not possible, to have an alternative donor as a back-up.”
On the regulatory side, the US Food and Drug Administration has issued guidance on managing clinical trials during the time of COVID-19, as have the US National Cancer Institute and the European Medicines Agency (EMA). The EMA document outlines the changes and adaptations that might be required over the course of the pandemic, for example, if trial participants need to be isolated, access to public places is limited, or health-care professionals have to take up different duties. It suggested that trial organisers consider suspensions, extensions, and postponements, depending on circumstances. The UK National Institute for Health and Care Excellence has issued guidance on delivering radiotherapy and systemic cancer therapies, which draws from NHS England's guidance.
Finally, the Global Radiation Oncology Targeted Response emerged from an online discussion involving 121 contributors in March, 2020. The paper explores subjects such as infection prevention, rationalisation of working practices, and specific issues related to radiation oncology. Advice on specific diseases is offered, and the authors list radiotherapy treatments that could be omitted. But they also point out that although deferring radical treatment for diseases with favourable biology “might seem immediately preferable, it might have unintended consequence in creating a further unmanageable surge in activity when the crisis has passed.”
It is too early to tell what shape this pandemic will take. But it is worth noting that the epidemic in China appears to be slowing down. Yi-Long Wu (Guangdong Lung Cancer Institute, Guangdong, China) points out that the major disruption to cancer care in the country occurred during the first two weeks of February. “From late February, everywhere except for Hubei province, we were able to start giving patients surgery, chemotherapy, and radiotherapy again”, he told The Lancet Oncology. “Now we are coming back to normal.”