To the editor,
Asymptomatic people with SARS-CoV-2 infection are of great concern as they undermine control interventions that rely on identifying symptomatic cases. However, current reports of asymptomatic infections were mostly cross-sectional case reports [[1], [2], [3], [4], [5]]. Do they develop symptoms later? Is an asymptomatic period a part of the natural course of coronavirus disease 2019 (COVID-19), or a chronic condition? Is the asymptomatic patient in an incubation period or a subclinical infection, or are they a chronic asymptomatic carrier of SARS-CoV-2 like Typhoid Mary? These questions are of great significance for understanding the spectrum, natural history and epidemiology of COVID-19. Therefore, we followed up virologically confirmed COVID-19 patients in Shanghai Public Health Centre who had no subjective symptoms on admission.
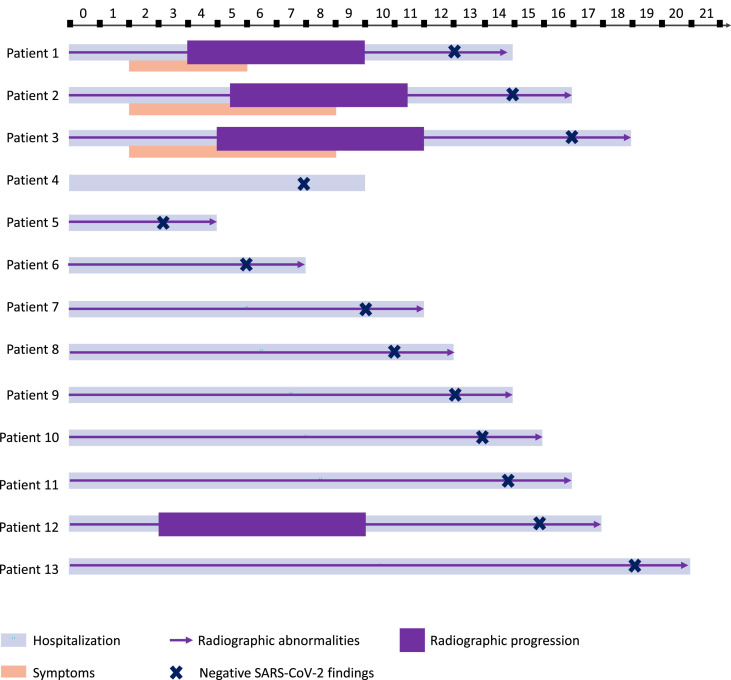
As of March 4th, 2020, a total of 328 adults were diagnosed with COVID-19 in Shanghai. Among them, 13 patients were asymptomatic at the diagnosis (Fig. 1 ). They also had no subjective symptoms within 2 weeks before admission. Their oral temperature was no more than 37.3°C on admission. All of them were close contacts of the confirmed cases and were admitted to Shanghai Public Health Clinic Centre within 48 h after diagnosis was established. Their mean age was 51.8 years (range: 25–80 years). Six of them were male. On admission, patients revealed slight laboratory abnormalities. Leucocytes were below the normal range in two patients (15.4%). Ten patients (76.9%) had differing degrees of elevation of the erythrocyte sedimentation rate. Liver function, renal function, and coagulation function were within the normal range, as were the levels of lactate dehydrogenase and procalcitonin.
Fig. 1.
Chronology of symptoms, radiographic findings, and identification of positive SARS-CoV-2 findings on qRT-PCR among asymptomatic patients in Shanghai. The numbers on the top indicate the number of days since admission. qRT-PCR, quantitative RT-PCR.
During follow-up, three patients developed symptoms at the second day of hospitalization, including sore throat, non-productive cough, chest distress, and diarrhoea (patients 1–3). The other ten patients remained asymptomatic. All patients underwent chest CT scan at admission and were followed up every 3 days. Twelve of them showed multiple ground-glass opacities that characterized SARS-CoV-2 pneumonia on admission (patients 1–3, 5–13), and four of these showed radiographic progression during hospitalization, but all showed improvement before discharge (patients 1–3 and 12). Patient 4 remained asymptomatic and had no evidence of radiographic abnormalities consistent with COVID-19. All patients tested SARS-CoV-2-RT-PCR-negative at a median time of 13 days (range 3–19 days).
When we find an RT-PCR-positive patient with no subjective symptoms, there are several possibilities. First, the patient is in the incubation period. The incubation period occurs in an acute disease, and is the time between the moment of exposure to an infectious agent and the appearance of signs and symptoms of the disease. In other words, this patient will develop symptoms or signs later, but has not yet done so. Second, the patient has developed signs, such as pneumonia on chest CT, but has not yet had subjective symptoms. This patient is actually in the period of illness. This is the case for our patients 5–13, and also for patients 1–3 before their symptom onset. Third, if this patient turns RT-PCR-negative later and has never experienced symptoms or signs, this patient should be regarded as having a subclinical infection, like patient 4 in our cohort. Fourth, if this patient continues to be asymptomatic and has no signs, and the RT-PCR remains positive for a long time, then this patient is an asymptomatic chronic carrier. No such cases were found in our cohort as all patients turned RT-PCR-negative in 3 weeks.
These four types of asymptomatic patients have completely different significance for the disease spectrum and natural history of COVID-19. If we can make a diagnosis early enough, we should be able to detect patients in the incubation period. In our cohort, three patients (patients 1–3) developed symptoms later and became typical COVID-19 patients. We also found that 2.7% of patients (9/328) continued asymptomatic even with pulmonary involvement (patients 5–13). Although they underwent the pathological process of pneumonia, like most COVID-19 patients, they were blind spots for control interventions based on symptomatic case screening because they never developed symptoms. We did not find chronic asymptomatic carriers in our cohort. There have been no previous cases of human chronic carriers of coronaviruses, including SARS-CoV and MERS-CoV. We think that there is probably no chronic carrier state for SARS-CoV-2. Although subclinical infections accounted for only 0.3% of our cohort (1/328, patient 4), it represents only the tip of the iceberg. The proportion of subclinical infections should be derived from future serological studies. A positive nasopharyngeal-swab or throat-swab RT-PCR for SARS-CoV-2 in an asymptomatic patient suggests that they may have the potential to infect others. However, the viral loads and infectivity of these patients may vary widely. Due to limited resources, we did not perform these tests. Further investigations are needed to determine the potential for and mode of contagion of asymptomatic patients to develop more scientific control strategies.
Author contributions
XZ and YL contributed equally to this work. Conception or design of the work: XZ, YL, WZ. Data collection and patient care: TL, WZ. Data analysis and drafting the article: XZ, YL. Critical revision of the article: WZ. Final approval of the version for publication: all of the authors.
Transparency declaration
The authors declare no competing interests. No funding was received for this work.
Acknowledgements
We thank all physicians who participated in this study for patient enrolment and follow-up, and show the greatest appreciation to all people, especially health workers, for their valuable input into disease control.
Editor: L. Leibovici
References
- 1.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan J.F., Yuan S., Kok K., To K.K.W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan X., Chen D., Xia Y., Wu X., Li T., Ou X. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020;20:410–411. doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. (epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang R., Xia J., Chen Y., Shan C., Wu C. A family cluster of SARS-CoV-2 infection involving 11 patients in Nanjing, China. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30147-X. (epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]