Abstract
Gallbladder tuberculosis (GT) is an extremely rare disease entity, even in our country Morocco known for being an endemic area. The lack of pathognomonic clinical presentation and radiological features of GT makes preoperative diagnosis unlikely and poses a diagnostic dilemma regarding gallbladder carcinoma (GC). The diagnosis is usually made by histological examination after cholecystectomy, highlighting the importance of sending every gallbladder specimen to pathology. We report an exceedingly rare case of GT mimicking GC and refer to a recent review of the literature to discuss the clinical and radiological features of GT.
Keywords: gallbladder tuberculosis, tuberculosis, gallbladder carcinoma, cholecystectomy, surgery, case report, scare
Introduction
Gallbladder tuberculosis (GT) is an extremely rare clinical entity that represents only 1% of abdominal tuberculosis cases [1]. The clinical presentation and the radiological findings are not specific, thereby making preoperative diagnosis difficult, and it is usually misdiagnosed as gallbladder carcinoma (GC) [2]. The diagnosis is usually made upon histological examination after cholecystectomy. We report an uncommon case of GT mimicking GC, and refer to a recent review of the literature to discuss the clinical and radiological features of GT. This case has been reported following the SCARE criteria [3].
Case presentation
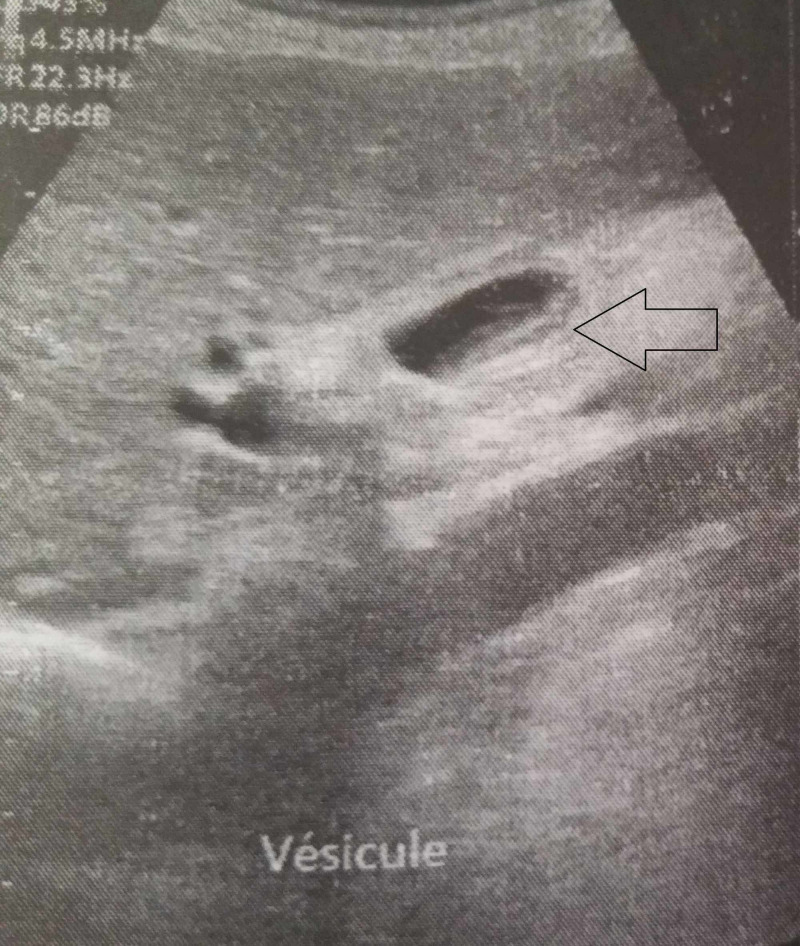
A 71-year-old male patient, a former miner, was diagnosed with silicosis 30 years ago. The patient presented with complaints of vague, dull pain in the right upper quadrant with a significant loss of weight and appetite. There was no history of tuberculosis. Physical examination found a right hypochondrial tenderness. Laboratory investigations and chest X-rays were normal. Ultrasonography showed a gallbladder with a large gallstone and an irregularly thickened wall with dilatation of the intrahepatic bile ducts (IHBD) and the common bile duct (CBD) (Figure 1).
Figure 1. Ultrasonography showing thickened gallbladder wall (black arrow).
A CT scan with intravenous contrast reported a suspicious irregular thickening of the gallbladder wall with the presence of a large calculus of 18 mm in the gallbladder, with dilatation of the CBD (Figure 2A,B).
Figure 2. (A and B) Computed tomography scan showing irregular thickening of the gallbladder wall (black arrow) with the presence of a large calculus in the gallbladder (blue arrow), with dilatation of the common bile duct (star).
Bili-MRI also revealed a thickened irregular gallbladder wall with dilatation of the CBD (14 mm) and IHBD, making GC the most likely diagnosis (Figure 3).
Figure 3. Bili-Magnetic resonance imaging showing suspicious irregular thickening of the gallbladder wall (black arrow).
Surgical exploration of the presumptive diagnosis of GC was done. Intraoperatively, we found a hard gallbladder with a thickened wall and contiguous infiltration into segment 4b of the liver. The patient underwent radical cholecystectomy. The histopathological examination revealed an ulcerated mucosa surrounded by epithelioid cells mixed with rare giant Langhans cells without caseous necrosis (Figure 4A,B).
Figure 4. (A) Microphotograph showing an epithelioid granuloma (black arrow) (HE 40×). (B) Microphotograph showing an epithelioid cell granuloma with rare giant cells without caseous necrosis (HE 400×).
HE: Hematoxylin and eosin
The diagnosis of GT was established in front of a bundle of clinical, radiological, and histological arguments.
On postoperative day nine, the patient became febrile and complained of abdominal pain and vomiting. An abdominal examination revealed diffuse rebound tenderness. Bile was noted in the drain. An urgent abdominal CT objectified fluid collections in the perihepatic space and at the cul-de-sac of Douglas, suggesting biliary peritonitis. The patient benefited from lavage and drainage of the peritoneal cavity and had a satisfactory recovery before being discharged from the hospital on day 15.
A complete course of anti-tubercular treatment was administered for six months [four drugs for two months: isoniazid (5 mg/kg), rifampicin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg), and then two drugs for the next four months: isoniazid and rifampicin]. The patient remained asymptomatic after a six-month follow-up.
Discussion
Isolated GT is an extremely rare clinical entity that was originally described for the first time by Gaucher in 1870 [4]. Only around 120 cases have been reported in the literature [1]. GT occurs most commonly in women over 30 years of age [1, 5]. Cholelithiasis and cystic duct obstruction are considered the most important factors in the development of GT [6]. According to Kapoor et al., all patients presented gallstone disease [5], however, Saluja et al. did not find any gallstone disease associated with GT in their cases [7].
The rarity of tuberculosis in the gallbladder is possibly due to the hypovascularity of the gallbladder sac and the alkaline nature of gallbladder bile, which has an inhibitory effect on Mycobacterium [8].
The clinical presentation of GT is varied and nonspecific, making the preoperative diagnosis of GT difficult; the most frequent clinical signs and symptoms are abdominal pain, loss of weight, and loss of appetite, according to the series of GT published in the literature, as seen in our case (Table 1).
Table 1. Comparison of the symptoms and clinical signs of GT between the series published in the literature and our case.
GT, gallbladder tuberculosis
| Author (year) | Kumar et al. (2000) [9] | Kapoor et al. (2006) [5] | Saluja et al. (2007) [7] | Govindasamy et al. (2011) [10] | Xu et al. (2011) [1] | Krishnamurthy et al. (2016) [2] | Our case |
| Number of patients | 5 | 5 | 3 | 3 | 7 | 3 | 1 |
| Abdominal pain | 5 | 4 | 2 | 3 | 7 | 3 | 1 |
| Loss of weight and appetite | 1 | 1 | 1 | 2 | 3 | 2 | 1 |
| Fever | 1 | 0 | 1 | 2 | 2 | 1 | 0 |
| Abdominal mass | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Jaundice | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
Only a few papers on the radiological findings of GT are found in the literature. Xu et al. [1] revealed three types of CT morphology features of GT. The most common presentation is the thickened-wall type which can be frequently misdiagnosed as GC, or cholecystitis. Sometimes CT scans can differentiate between GT and GC by showing the “halo” of the edema of GT. The mass-forming type CT findings are similar to GC; however, the presence of a large mass with multicentric necrosis on enhanced CT, or a large mass with multiple flecked calcifications, may be helpful to make the diagnosis of GT. The micronodular type is nonspecific.
According to Govindasamy et al., the MRI morphology features of GT were identical to GC [10]. To summarize, there are no specific investigations for GT.
The diagnosis is usually made upon histological examination after cholecystectomy [11] highlighting the importance of sending every gallbladder specimen to pathology.
The treatment of GT is based on anti-tubercular chemotherapy based on a two-month attack treatment plan involving isoniazid (5 mg/kg), rifampicin (10 mg/kg), pyrazinamide (25-30 mg/kg), and ethambutol (20 mg/kg), followed by maintenance therapy for four months of isoniazid and rifampicin [12].
Conclusions
There is no pathognomonic presentation of GT, and it is usually misdiagnosed as GC. As the preoperative diagnosis is difficult, all resected cholecystectomy specimens should be sent for histopathological examination for evidence of tuberculosis. A well-managed anti-tuberculosis treatment allows healing.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Gallbladder tuberculosis: CT findings with histopathologic correlation. Xu XF, Yu RS, Qiu LL, Shen J, Dong F, Chen Y. Kor J Radiol. 2011;12:196–202. doi: 10.3348/kjr.2011.12.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallbladder tuberculosis camouflaging as gallbladder cancer - case series and review focussing on treatment. Krishnamurthy G, Singh H, Rajendranet J, et al. Ther Adv Infect Dis. 2016;3:152–157. doi: 10.1177/2049936116678589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, Orgill DP, for the SCARE group. Int J Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 4.Tuberculosis of the gall-bladder. Bergdahl L, Boquist L. Br J Surg. 1972;59:289–292. doi: 10.1002/bjs.1800590411. [DOI] [PubMed] [Google Scholar]
- 5.Myriad presentations of gall bladder tuberculosis. Kapoor S, Sewkani A, Naik S, Sharma S, Jain A, Varshney S. https://www.ncbi.nlm.nih.gov/pubmed/16763349. Indian J Gastroenterol. 2006;25:103–104. [PubMed] [Google Scholar]
- 6.Tuberculosis of the gall bladder. Goyal SC, Goyal R, Malhotra V, Kaushik K. http://europepmc.org/article/MED/9695395. Indian J Gastroenterol. 1998;17:108. [PubMed] [Google Scholar]
- 7.Hepatobiliary and pancreatic tuberculosis: a two decade experience. Saluja SS, Ray S, Pal S, Kukeraja M, Srivastava DN, Sahni P, Chattopadhyay TK. BMC Surg. 2007;7:10. doi: 10.1186/1471-2482-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gallbladder tuberculosis (case report and review of the literature) Abu-Zidan FM, Zayat I. https://www.ncbi.nlm.nih.gov/pubmed/10576349. Hepatogastroenterology. 1999;46:2804–2806. [PubMed] [Google Scholar]
- 9.Tuberculosis of the gallbladder. Kumar K, Ayub M, Kumar M, Keswani N, Shukla H. HPB Surg. 2000;11:401–404. doi: 10.1155/2000/21392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biliary tract tuberculosis - a diagnostic dilemma. Govindasamy M, Srinivasan T, Varma V, Mehta N, Yadav A, Kumaran V, Nundy S. J Gastrointest Surg. 2011;15:2172–2177. doi: 10.1007/s11605-011-1685-5. [DOI] [PubMed] [Google Scholar]
- 11.Tuberculosis of the cystic duct lymph node. De Melo VA, De Melo GB, Silva RL, Piva N, Almeida ML. Braz J Infect Dis. 2004;8:112–114. doi: 10.1590/s1413-86702004000100009. [DOI] [PubMed] [Google Scholar]
- 12.Gallbladder tuberculosis (Article in French) El Malki HO, Benkabbou A, Mohsine R, Ifrine L, Belkouchi A, Balafrej S. http://europepmc.org/article/MED/16630427. Can J Surg. 2006;49:135–136. [PMC free article] [PubMed] [Google Scholar]