The efficacy of digital mental health (DMH) services is well established. DMH services are comprised of the technology, service protocol, and ideally, implementation plan to support delivery. Like their traditional in-person treatment counterparts, DMH services have been developed and are being studied to target the behavioral, cognitive, and/or affective mechanisms that impact functioning (e.g., decreasing avoidance via a digital anxiety intervention). However, when DMH services move from controlled research settings to deployment in real-world healthcare settings, engagement is an acute problem.1 Implementation attempts often show low rates of service use and retention among patients (i.e., failure for individual-level engagement), and DMH services fail to be integrated successfully within their targeted systems of care (i.e., failure for systems-level engagement among providers/organizations). For example, a large-scale attempt to implement commercially-available and free-to-use digital depression services in primary care failed.2 Several factors impede successful implementation of evidence-based interventions into care, such as organizational, sociopolitical, and economic policies (e.g., reimbursement challenges) and failed understanding of mechanisms by which implementation strategies improve outcomes. Another critical factor impacting low engagement is the failure to adequately incorporate end-users (e.g., patients, providers, and care systems) in the design of DMH services.
To rectify these failures, our field needs methods to study and improve treatment design and delivery for DMH. The National Institute of Mental Health’s (NIMH) National Advisory Mental Health Council report on developing information technologies recommended research on “the design and evaluation of interventions in real-world environments with input from end-users (consumers, clinicians, administrators).”3 We propose here the integration of user-centered design (UCD) methods to improve engagement by patients and providers, along with adaptation of NIMH’s Research Domain Criteria (RDoC) framework4 to study these mechanisms.
Improving Engagement through Attention to Design
The underlying principle by which DMH services are intended to be successful (i.e., how they “operate”) is by integrating into the fabric of people’s lives so that these services are used in the moments and contexts when they are needed throughout peoples’ daily routines. However, if DMH service designs are not engaging, people will stop using them. Additionally, there has been little attention to fitting DMH services into healthcare organizations and the workflows of providers who are expected to deliver them. As a result, even a service that is firmly grounded in an evidence-based therapy will fail to produce clinical improvements if the service does not account for how people engage with it.
UCD is a methodology for optimizing technologies and services to enhance engagement through iterative design that is grounded in information from the stakeholders who will be using the services and the contexts in which they will be implemented. Rather than relying on experts to design what users should receive (i.e., typical approach to date for DMH), UCD engages deeply with end-users to understand what they need, how they interact with the devices through which interventions are delivered, and the workflows to deliver the service. As a result, UCD produces solutions that are more likely to be perceived by end-users as useful, usable, and desirable, and that lead to greater engagement. However, systematic efforts linking UCD to these and clinical outcomes in healthcare are lacking.5
Engagement as a Mechanism
We also need research methods that provide more generalizable information about DMH services. UCD largely is a qualitative endeavor focused on discovery, in which the voices of a few individuals are assumed to speak for the broader population. Clinical research requires quantitative methods that protect stakeholders through validation and generate translational information about the mechanisms that drive how and why individuals engage (i.e., adopt and interact) with DMH services. Experimental therapeutics aims to establish a generalizable understanding of mechanisms that drive human functioning to establish more effective interventions.4 The RDoC framework operationalizes experimental therapeutics by defining constructs through which interventions effect problems or diseases. To date, RDoC domains (e.g., positive and negative valence systems, cognitive systems) have primarily measured constructs at the individual level using molecular, genetic, neurocircuit, and behavioral units of analysis. To adapt experimental therapeutics for DMH, we need an informed conceptualization of the domains and constructs through which exogenous variables impact the potency of DMH services.
Targeting engagement (the product of UCD) as a mechanism of DMH is critical to understanding how to design DMH services that produce changes in symptomatology. Figure 1 presents a conceptual model showing the relationship between engagement as a mechanism and clinical outcomes for a hypothetical intervention. Engagement is operationalized through several constructs and measured through subjective and objective units of analysis.6,7 Subjective assessments focus on whether stakeholders perceive DMH services as useful (helps stakeholders achieve their goal or complete tasks), usable (is easy to use, learn, and understand), and satisfying (enhances stakeholder experiences). We also can assess engagement through objective means, such as interactions with the technology or contacts with the health system. These subjective and objective engagement constructs can be evaluated as mediating factors that influence users’ response to digital interventions.
Figure 1.
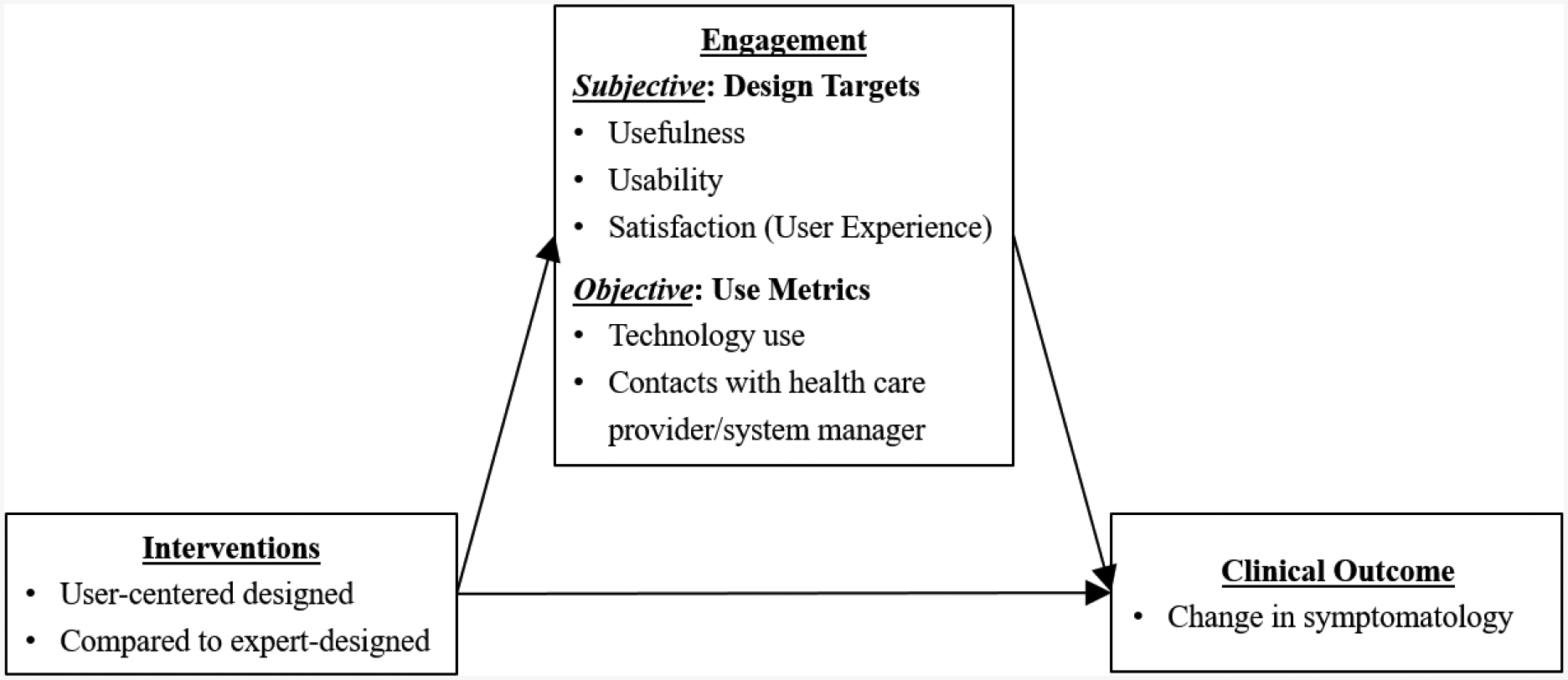
Conceptual model for experimental therapeutics for digital mental health: targeting engagement as a mediating mechanism
Conclusion
We advocate for expanding the experimental therapeutics framework beyond the individual to define and study engagement, which can inform our understanding of human functioning, in this case, how individuals interact with DMH services in their everyday, real-world settings. Targeting and measuring engagement can validate the results of UCD efforts and improve our capacity to create effective DMH services. The RDoC framework provides a useful paradigm for evaluating the importance of engagement variables. RDoC began as a flexible framework and has since been adapted to embrace diverse research approaches. To make progress in DMH, we need to understand how a person interacts with the technologies and services. This can be measured both subjectively, for example through perceptions of usefulness, usability, and satisfaction, as well as objectively through trace data from digital technologies, such as use logs or contacts. Updating RDoC, and experimental therapeutics frameworks more broadly, to integrate a domain that reflects engagement with DMH services would support and drive research that is critical to overcoming the research-to-practice gap, which if validated, would strongly support a fundamental shift in our approach to DMH research.
Funding/Support:
This work was supported by grants from the National Institutes of Health (K08 MH112878; K01 DK116925).
Footnotes
Conflict of Interest Disclosures: None to report.
References
- 1.Mohr DC, Riper H, Schueller SM. A Solution-Focused Research Approach to Achieve an Implementable Revolution in Digital Mental Health. JAMA Psychiatry. 2018;75(2):113–114. [DOI] [PubMed] [Google Scholar]
- 2.Gilbody S, Littlewood E, Hewitt C, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ. 2015;351:h5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health and Human Services NIoH, National Institute of Mental Health, National Advisory Mental Health Council. Opportunities and Challenges of Developing Information Technologies on Behavioral and Social Science Clinical Research. 2017. [Google Scholar]
- 4.National Institute of Mental Health. Strategic Plan for Research. Bethesda, MD: National Institute of Mental Health;2015. [Google Scholar]
- 5.Altman M, Huang TTK, Breland JY. Design Thinking in Health Care. Prev Chronic Dis. 2018;15:E117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doherty K, Doherty G. Engagement in HCI: Conception, Theory and Measurement. ACM Comput Surv. 2018;51(5):1–39. [Google Scholar]
- 7.Yardley L, Spring BJ, Riper H, et al. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am J Prev Med. 2016;51(5):833–842. [DOI] [PubMed] [Google Scholar]


