Abstract
Significance.
We sought to identify baseline and clinical factors that were predictive of the response to amblyopia treatment. We report that binocular amblyopia treatment may be especially effective for moderate amblyopia in orthotropic children.
Purpose.
We previously reported results from the primary cohort (n=28) enrolled in a randomized clinical trial (NCT02365090), which found that binocular amblyopia treatment was more effective than patching. Enrollment of an additional 20 children was pre-planned to provide the opportunity to examine factors that may be predictive of response to amblyopia treatment.
Methods.
48 children (4-10 y) were enrolled, with 24 randomized to contrast-rebalanced binocular game treatment (1 hour/day, 5 days/week) and 24 to patching treatment (2 hours/day, 7 days/week). The primary outcome was change in amblyopic eye best-corrected visual acuity at the 2-week visit. Baseline factors examined were age at enrollment, visual acuity, stereoacuity, and suppression. Clinical factors were etiology, age at diagnosis, prior treatment, and ocular alignment.
Results.
At 2 weeks, visual acuity improvement was significantly greater with the binocular game than patching. Children with moderate amblyopia and orthotropia had more visual acuity improvement with binocular game play than those with severe amblyopia. In addition, children who spent more time playing the binocular game had more improvement. We were not able to confidently identify any baseline or clinical factors that were associated with response to patching treatment.
Conclusions.
Binocular amblyopia treatment was more effective among orthotropic children with moderate amblyopia than among children with microtropia or severe amblyopia.
We previously reported results from our primary cohort (n=28) enrolled in a randomized clinical trial of contrast re-balanced binocular amblyopia treatment with the Dig Rush game on an iPad versus patching (NCT02365090).1 The Dig Rush game was dichoptic and had reduced contrast for components of the game display seen by the fellow eye (contrast rebalancing) to allow the child to overcome interocular suppression and experience binocular vision while playing the game. Dig Rush was effective in treating childhood amblyopia and the visual acuity improvement achieved with Dig Rush was significantly greater than with patching.1 Completion of enrollment into our preplanned secondary cohort combined with the primary cohort (n=48), has provided a sufficient opportunity to identify baseline and clinical factors that may be predictive of response to binocular and patching treatment.
METHODS
The research protocol observed the tenets of the Declaration of Helsinki, was approved by the Institutional Review Board of the University of Texas Southwestern Medical Center and conformed to the requirements of the United States Health Insurance Portability and Privacy Act. Informed consent was obtained from a parent or legal guardian prior to testing and after explanation of the nature and possible consequences of the study. Assent was obtained from participants age 10 years and older.
From February 20, 2015 through July 2, 2018, eligible children 4-10 years of age diagnosed with amblyopia due to strabismus, anisometropia, or both were referred to the Retina Foundation of the Southwest by pediatric ophthalmologists in the Dallas-Fort Worth area. Eligible children had amblyopic eye best-corrected visual acuity of 0.3-0.8 logMAR (20/40-20/125) and fellow eye amblyopic eye best-corrected visual acuity of 0.1 logMAR (20/25) or better (0.2 logMAR or better for 4-year-olds), and an interocular difference of ≥0.3 logMAR (≥3 lines). In addition, eligible children were required to have been wearing their glasses for at least 8 weeks to be eligible for enrollment. Strabismic children were initially diagnosed with esotropia, but were aligned with surgery and/or spectacle correction to within 4 prism diopters of orthotropia at distance and near. None of the children were born <32 weeks postmenstrual age or had co–existing ocular or systemic disease, congenital infections/malformations, or developmental delay. Medical records were obtained from referring ophthalmologists to extract diagnosis, current alignment, cycloplegic refraction, and prior treatment.
This study was a randomized clinical trial (NCT02365090) with the goal of enrolling two pre-planned two cohorts1: 1) Primary Cohort: 28 children to determine the effectiveness of the binocular game as amblyopia treatment, and whether it is more effective than patching, and 2) an additional 20 children to be combined with the primary cohort to allow evaluation of factors that may affect treatment outcomes including baseline factors (age, amblyopic eye best-corrected visual acuity, stereoacuity, and suppression) and clinical factors (etiology, age at initial diagnosis, prior amblyopia treatment, and current alignment). Data from the primary cohort of 28 children have been reported previously.1 Here, we report results from analysis of baseline and clinical factors based on the combined cohorts (n=48). The trial protocol and statistical analysis plan are available on clinicaltrials.gov (NCT02365090).
Randomization was performed by a statistician who provided individual sealed sequentially numbered envelopes. Two randomization schedules were created: one for children with prior amblyopia treatment (patching, atropine), and one for children with no prior treatment. Randomization (1:1) was prepared in permuted blocks of 4 or 6. After confirming eligibility and obtaining informed consent, an investigator opened the envelope, enrolled the child and assigned the child to the appropriate treatment.
Children randomized to binocular game treatment were loaned an iPad with Dig Rush, a contrast-rebalanced dichoptic game.1 Children were asked to play the game at home for 1 hour a day, 5 days a week for 2 weeks (10 hours total binocular treatment). During game play, children wore red-green anaglyphic glasses that separate game images seen by each eye, so that reduced contrast components of the game screens were seen by the fellow eye, while high contrast components of the game screen were seen by the amblyopic eye. Background images were high contrast and seen by both eyes. Both eyes must see their respective game components for successful game play. Amblyopic eye contrast remained at 100% contrast, while fellow eye contrast started at 20% but increased gradually with game success. The patching protocol was the current standard-of-care for amblyopia treatment.2 Children were provided with Ortopad® eye patches and asked to patch their fellow eye 2 hours a day, 7 days a week for 2 weeks (28 hours total patching treatment). Children randomized to the patching group were offered the opportunity to play the binocular game after they completed the 2-week primary outcome visit.
For both groups, vision assessments were conducted at baseline and at 2 weeks, and included: 1) Crowded monocular amblyopic eye best-corrected visual acuity using the e-ETDRS protocol3 for children ≥7 years of age at the baseline visit, or the Amblyopia Treatment Study HOTV protocol for children <7 years of age at the baseline visit,4 2) stereoacuity using the Randot Preschool Stereoacuity and Stereo Butterfly Tests (Stereo Optical Co., Inc., Chicago, IL, USA), and 3) extent of suppression scotoma using the Worth 4-dot test at 7 different distances.5
Parents or legal guardians were provided a personalized calendar to record the number of minutes per day their child played the game or patched the fellow eye. A log file was also obtained from the iPad that contained the number of minutes played and the fellow eye contrast for each play session.
Statistical Analyses
The primary outcome was change in amblyopic eye best-corrected visual acuity at the 2-week visit. In an intent-to-treat analysis, an independent t-test was conducted to determine whether improvement in visual acuity differed between the binocular game and patching groups at the 2-week visit. For analyses of predictive factors, baseline and clinical variables were dichotomized, based on criteria commonly used in clinical treatment trials for amblyopia6-12: age at enrollment (4.0-6.9 years vs 7.0-10.9 years), amblyopic eye best-corrected visual acuity (moderate amblyopia, 0.3-0.6 logMAR vs severe amblyopia, 0.7-0.8 logMAR), stereoacuity (40-800 arcsec vs nil), suppression (foveal/macular fusion vs peripheral/nil fusion), etiology (anisometropic vs strabismic/combined), age at initial diagnosis (<4 years vs 4-8 years), prior amblyopia treatment (none vs patching/atropine), and current alignment (ortho vs tropic). Independent t-tests were conducted to evaluate whether each was associated with visual acuity improvement. Because 8 baseline variables and 4 clinical variables were evaluated, only P≤ .006 were considered statistically significant (Bonferroni correction for multiple comparisons). A Pearson correlation was conducted to examine the relationship between hours of binocular game play and the amount of visual acuity improvement observed at the 2-week visit. All analyses were conducted with an intent-to-treat approach.
RESULTS
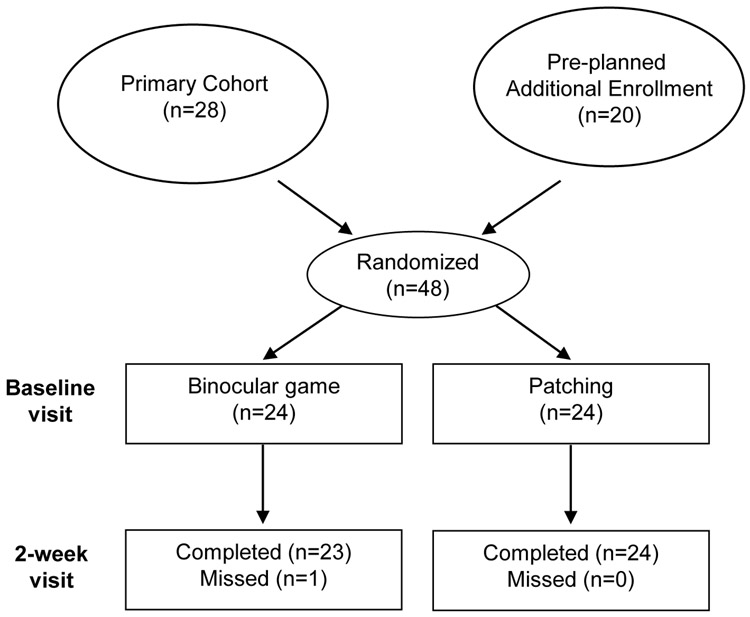
Between February 2015 and March 2019, 48 patients were enrolled in the study; 24 were randomized to binocular game treatment and 24 to patching treatment. The 2-week outcome visit was completed by 47/48 children (Appendix Figure A1, available at [LWW insert link]); one child was unable to complete the 2-week visit due to illness. Baseline characteristics are provided in Appendix Table 1, available at [LWW insert link]. Twenty-seven (56%) children were diagnosed with anisometropic amblyopia and 21 (44%) with strabismic or combined mechanism amblyopia. The mean±standard deviation (SD) age was 6.8±1.8 years, range=4.3–10.8 years. Mean amblyopic eye best-corrected visual acuity ±SD at enrollment was 0.49±0.16 logMAR (~20/63±1.6 lines), range=0.3–0.8 logMAR (20/40–20/125). Visual acuity was 0.3–0.6 logMAR (20/40–20/80) in 38 (79%) children and 0.7–0.8 logMAR (20/100–20/125) in 10 (21%) children. Twenty-eight (58%) children received prior amblyopia treatment with patching, atropine, or both.
Adherence to Protocol
Compliance using the personalized calendar was similar to the iPad log, but the parents overestimated the time spent playing the game by 13% (1.3±3.0 hours). In all reported analyses, the iPad log was used. Compliance for patching was tabulated using the personalized calendar. Children assigned to the binocular game completed 10.3±3.0 hours (103% prescribed treatment time). Fellow eye contrast for children assigned to the binocular game was 50±19% at the 2-week visit. Children assigned to patching reported that they completed 27.7±2.6 hours (99% prescribed treatment time).
Primary Outcome
At the 2-week primary outcome visit, a larger improvement in amblyopic eye best-corrected visual acuity was found with binocular game compared with patching (0.15 vs 0.07 logMAR; CI95% difference = 0.03-0.13; t45 = 3.05, P =.004; Figure 1). For the binocular game group, improvement ranged from 0.0 to 0.4 logMAR; 21 children (87.5%, CI95%=69%–96%) improved by 0.1 logMAR or more [2 improved 0.3-0.4 logMAR, 10 improved 0.2 logMAR, 9 improved 0.1 logMAR], and 3 children did not improve (12.5%, CI95%=4%–31%). For the patching group, improvement ranged from −0.1 to 0.2 logMAR; 12 children (50%, 95%CI=31%–69%) improved by 0.1 logMAR or more [5 improved 0.2 logMAR, 7 improved 0.1 logMAR], and 11 children (46%, CI95%=28%–65%) did not improve, and 1 child (4%, CI95%=1%–20%) decreased by −0.1 logMAR].
Figure 1.
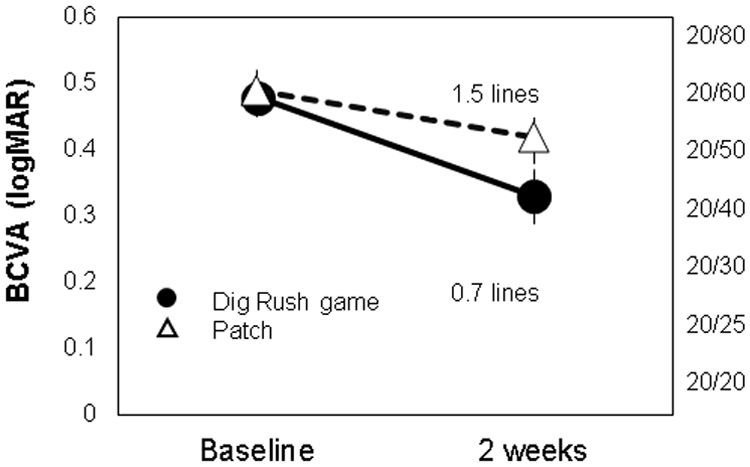
Best-corrected visual acuity (BCVA) for the amblyopic eye at baseline and after 2 weeks of playing a contrast re-balanced binocular iPad game (1 hr/day 5 days/wk) or patching the fellow eye (2 hr/day 7 days/wk). A larger improvement occurred for children randomized to play the binocular game compared with children who were randomized to patching.
At the 2-week visit, 35% (95%CI: 19% - 55%) of children playing the binocular game had recovered normal visual acuity for age (≤0.2 logMAR; 20/32 or better). Only 8% (CI95%=2% - 26%) of the children in the patching group had recovered normal visual acuity for age at the 2-week visit.
Baseline Factors
Baseline factors included age at enrollment, baseline amblyopic eye best-corrected visual acuity, baseline fusion, and baseline stereoacuity. In the binocular game group (Figure 2), only baseline visual acuity was associated with response to amblyopia treatment. Children with moderate amblyopia had more improvement than children with severe amblyopia (0.15 vs 0.07 logMAR; CI95% difference = 0.06-0.08; t22=15.40, P <0.001). In the patching group (Figure 3), we were unable to confidently identify any association between baseline factors and response to amblyopia treatment (P-values ranged from 0.12 to 0.50 for the 4 factors evaluated).
Figure 2.
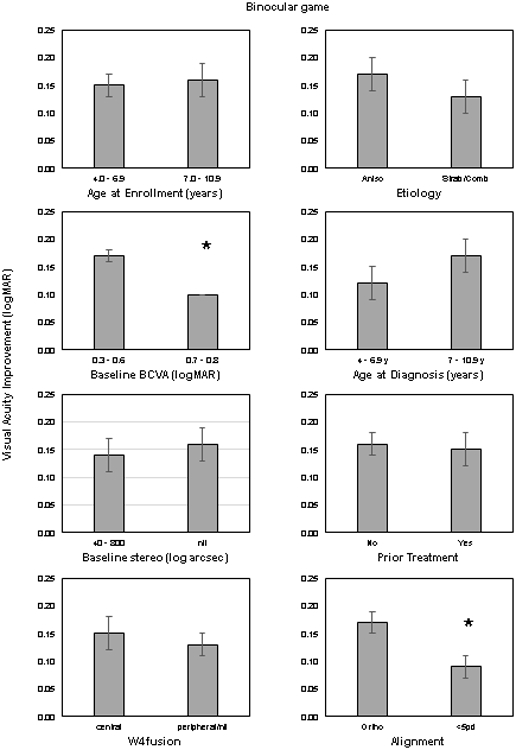
Amount of best-corrected visual acuity (BCVA) improvement for the amblyopic eye for subgroups of children who were playing the contrast re-balanced binocular iPad game. Baseline (left) and clinical variables (right) were dichotomized, based on criteria commonly used in clinical treatment trials for amblyopia.6-12 Binocular amblyopia treatment was more effective among orthotropic children with moderate amblyopia than among children with microtropia or severe amblyopia.
Figure 3.
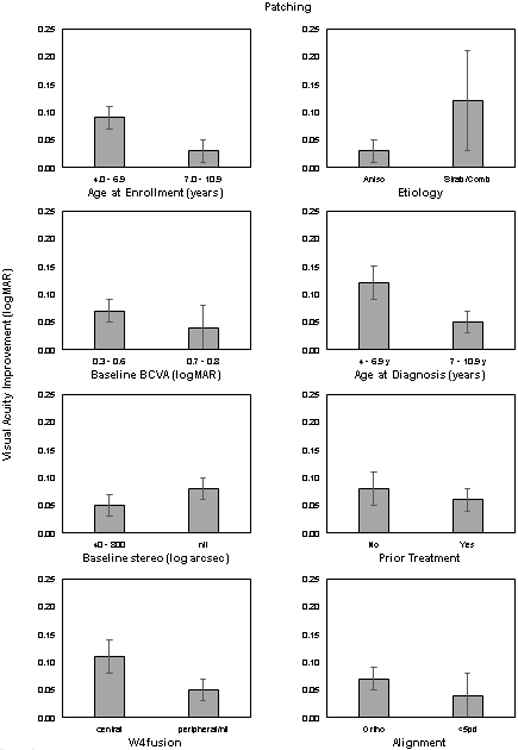
Amount of best-corrected visual acuity (BCVA) improvement for the amblyopic eye for subgroups of children who were patching. Baseline (left) and clinical variables (right) were dichotomized, based on criteria commonly used in clinical treatment trials for amblyopia.6-12 We were not able to confidently identify any baseline or clinical factors that were associated with response to patching treatment.
Clinical Factors
Clinical factors included etiology, age at diagnosis, prior treatment, and ocular alignment. In the binocular game group (Figure 2), only ocular alignment was associated with response to amblyopia treatment. Orthotropic children had significantly more visual acuity improvement than children with esotropia <5pd (0.17 vs 0.09 logMAR; CI95% difference = 0.06-0.10; t22=7.96, P<.001). In the patching group (Figure 3), we were unable to confidently identify any association between clinical factors and response to amblyopia treatment (P-values ranged from 0.09 to 0.57 for the 4 factors evaluated).
Dose-Response
In the binocular game group (Figure 4, top), there was a moderate linear relationship between hours of binocular game play with fellow eye contrast <100% and the amount of visual acuity improvement observed (r = 0.545; CI95%=0.17 – 0.78). Based on the linear best-fit, children who played 5 hours (50% adherence) improved about 0.1 logMAR (1 line), those who played 10 hours (100% adherence) improved about 0.18 logMAR (1.8 lines), and those who played 15 hours (150% adherence) improved about 0.26 logMAR (2.6 lines).
Figure 4.
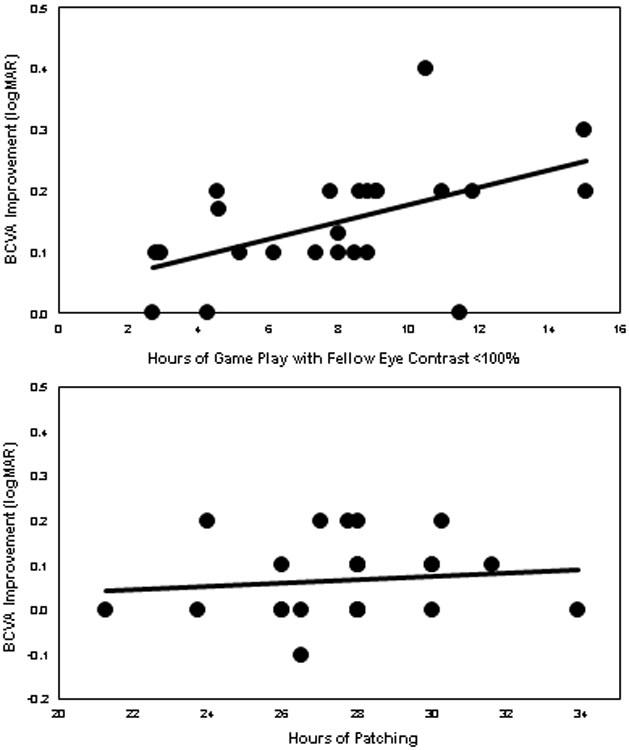
Amount of best-corrected visual acuity (BCVA) improvement for the amblyopic eye as a function of the number of hours of treatment for children randomized to play the binocular game (top) and children who were randomized to patching (bottom). There was a moderate linear relationship between hours of binocular game play and the amount of BCVA improvement observed. In the patching group, we were unable to confidently identify a relationship between hours of patching and the amount of AE BCVA improvement observed.
In the patching group (Figure 4, bottom), we were unable to confidently identify a relationship between hours of patching and the amount of visual acuity improvement observed.
Stability of Visual Acuity Gains
In the binocular game group, most children returned to patching treatment following completion of the study. However, 8 children had no treatment other than glasses for 3-6 months following study participation. In this subset of participants, there had been a mean improvement in visual acuity of 0.19 logMAR.
DISCUSSION
The contrast re-balanced Dig Rush game was effective in treating amblyopia in children ages 4-10 years, improving visual acuity by 1.5 lines with 10 hours of game play over 2 weeks. With baseline visual acuity of 0.3 to 0.8 logMAR, 35% of children in the binocular game group achieved visual acuity of 0.2 or better at 2 weeks compared with only 8% in the patching group. Baseline visual acuity, ocular alignment, and adherence to the treatment protocol were associated with binocular amblyopia treatment success. The 1.5 lines improvement in visual acuity observed at 2 weeks (10 hours of game play) compares favorably with recent studies of 16 weeks (224 hours) of 2 hours per day patching treatment for amblyopia. Specifically, in recent studies that required spectacle wear for a sufficient period to establish stable visual acuity prior to enrollment, 16 weeks of patching has resulted in 1.3 – 2.3 lines of visual acuity improvement.13-16
There remains substantial controversy about whether binocular amblyopia treatment is effective. Table 1 highlights some differences among the randomized clinical trials that have been reported in the literature. First, note the decreasing amount of visual acuity improvement among the various studies as a function of the average age of those enrolled. Participants in this study (shown in the first row) were younger than those enrolled in other studies. Our focus was on enrolling young children, not children who had abandoned treatment and were judged to have intractable residual amblyopia. Our cohort included only 4 children who had prior patching but had stopped patching due to lack of visual acuity improvement prior to enrolling in our study. The remaining children had either no prior patching or took a break from patching to participate in this randomized clinical trial. Compare that to the older participants in other randomized clinical trials in the table, where most participants had abandoned patching, had intractable residual amblyopia, and sought an experimental treatment because all other options (spectacles, patching, atropine) had failed.
Table 1.
Randomized clinical trials of contrast-rebalanced binocular games.
| Study | Game | Lines improved |
Age | >7 years | No prior patching |
Not orthotropic |
|---|---|---|---|---|---|---|
| Birch et al (2019)a Kelly et al (2016)b |
Dig Rush | 1.8 | 6.8 y | 25% | 42% | 21% 1-4pd |
| Holmes et al. (2016)c | Tetris | 1.1 | 8.4 y | 77% | 24% | 26% 1-9 and ≥10pd |
| PEDIG, et al. (2019)d | Dig Rush | 0.5 | 9.6 y | 100% | 6% | 32% 1-9 and ≥10pd |
| Manh et al. (2018)e | Tetris | 0.7 | 14.3 y | 100% | 23% | 38% 1-9 and ≥10pd |
| Gao et al. (2018)f | Tetris | 0.1 | 22 y | 100% | 20% | 55% 1-9 and ≥10pd |
y = years old; pd = prism diopters
Current study
Kelly KR, Jost RM, Dao L, et al. Binocular Ipad Game Vs Patching for Treatment of Amblyopia in Children: A Randomized Clinical Trial. Pediatric Eye Disease Investigator Group. JAMA Ophthalmol 2016;134:1402-8.
Holmes JM, Manh VM, Lazar EL, et al. Effect of a Binocular IPad Game vs. Part-Time Patching in Children Aged 5 to 12 Years with Amblyopia: A Randomized Clinical Trial. Pediatric Eye Disease Investigator Group. JAMA Ophthalmol 2016;134:1391-400.
Pediatric Eye Disease Investigator Group, Holmes JM, Manny RE, et al. A Randomized Trial of Binocular Dig Rush Game Treatment for Amblyopia in Children Aged 7 to 12 Years. Ophthalmology 2019;126:456-66.
Manh VM, Holmes JM, Lazar EL, et al. A Randomized Trial of a Binocular IPad Game versus Part-Time Patching in Children Aged 13 to 16 Years with Amblyopia. Pediatric Eye Disease Investigator Group. Am J Ophthalmol 2018;186:104-15.
Gao TY, Guo CX, Babu RJ, et al. Effectiveness of a Binocular Video Game vs. Placebo Video Game for Improving Visual Functions in Older Children, Teenagers, and Adults with Amblyopia: A Randomized Clinical Trial. BRAVO Study Team. JAMA Ophthalmol 2018;136:172-81.
In our cohort, even small angle deviations up to 4pd appeared to limit the benefit of binocular treatment. The 4pd limit was chosen for inclusion based on research showing that strabismus of 4pd or less was compatible with stereoacuity.17 Nonetheless, we found that even small angles of ocular misalignment of 1-4 pd were associated with less benefit of binocular amblyopia treatment compared with orthotropia. Perhaps this is a consequence of the anti-suppression approach; children with small angle tropia may suppress the amblyopic eye when not engaged in contrast-rebalanced game play to avoid diplopia. Orthotropic children may maintain the release from suppression experienced during game play, so that it persists beyond the game. Overall, only 21% of children in the present study had 1-4pd tropia, while other randomized clinical trials had 26-55% with strabismus, including some with tropia >4 pd.
There are several limitations of our study. This was a single site, small cohort randomized clinical trial. The inclusion/exclusion criteria may limit generalization to other groups of amblyopic children. Visual acuity testing was not masked but we did utilize a computer visual acuity test system designed to minimize the role of the tester. While the sample size was sufficient to examine baseline and clinical variables in a dichotomous manner, we are not able to look at the relationship between these variables and visual acuity outcome in finer detail. In addition, our results may be dependent on the criteria chosen to dichotomize each variable. The brief duration of the study may have limited the amount of visual acuity improvement observed. While the iPad did provide an objective log of the number of minutes of game play per day, it is possible that children did not wear their red-green glasses for all periods of game play. We were not able to monitor the number of hours of patching objectively, and relied on a calendar log completed by the parents.
CONCLUSIONS
Binocular amblyopia treatment was effective in treating childhood amblyopia, especially among orthotropic children with moderate amblyopia who had more game play time.
ACKNOWLEDGMENTS
Trial Registration: NCT02365090. Registration Date: February 18, 2015.
The authors thank Bryan De La Cruz and Sarah Morale for their help with data collection. This study was conducted at the Retina Foundation of the Southwest and was presented at the annual AAPOS 2019 meeting. National Eye Institute (EY02313). Dig Rush was developed in collaboration with Robert Hess at McGill University (Montréal, Québec), Amblyotech (Atlanta, Georgia) and UbiSoft (Montréal, Québec). None of the authors have a financial conflict of interest with any of the material presented in the manuscript. Eileen E Birch had full access to all of the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
This research was conducted in the Crystal Charity Ball Pediatric Vision Laboratory at the Retina Foundation of the Southwest.
Appendix
Appendix figure A1. -.
Birch et al. Optometry and Vision Science, May 2020
Appendix Table A1.
Baseline characteristics.
| Total (N=48) |
Binocular game (n=24) |
Patching (n=24) |
|
|---|---|---|---|
| Sex: F | 16 | 8 | 8 |
| Age, years | |||
| 4–6 | 28 | 14 | 14 |
| 7–10 | 20 | 10 | 10 |
| Mean±SD, years | 6.83±1.78 | 6.71±1.83 | 6.95±1.77 |
| Prior amblyopia treatment | |||
| None | 20 | 10 | 10 |
| Patching | 17 | 9 | 8 |
| Atropine | 2 | 1 | 1 |
| Patching + atropine | 9 | 4 | 5 |
| Weeks in glasses | |||
| 8–13 | 10 | 4 | 6 |
| >13–26 | 7 | 4 | 3 |
| >26 | 31 | 16 | 15 |
| Cause of amblyopia | |||
| Anisometropia | 27 | 13 | 14 |
| Strabismus/Combined mechanism | 21 | 11 | 10 |
| AE BCVA, logMAR (Snellen equivalent) | |||
| 0.3–0.6 (20/40–20/80) | 38 | 19 | 19 |
| 0.7–0.8 (20/100–20/125) | 10 | 5 | 5 |
| Mean±SD, logMAR | 0.49±0.16 | 0.48±0.17 | 0.49±0.15 |
| (20/63±1.4 lines) | (20/63±1.4 lines) | (20/63±1.5 lines) | |
| FE BCVA, logMAR (Snellen equivalent) | |||
| −0.1 (20/16) | 10 | 5 | 5 |
| 0.0 (20/20) | 19 | 10 | 9 |
| 0.1 (20/25) | 17 | 8 | 9 |
| 0.2 (20/30) | 2 | 1 | 1 |
| Mean±SD, logMAR | 0.02±0.08 | 0.03±0.08 | 0.03±0.08 |
| (20/20±0.8 line) | (20/20±0.8 line) | (20/20±0.8 line) |
Footnotes
Presented at the 2019 Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus (San Diego).
Contributor Information
Eileen E. Birch, Retina Foundation of the Southwest, Dallas, Texas; Department of Ophthalmology, UT Southwestern Medical Center, Dallas, Texas.
Reed M. Jost, Retina Foundation of the Southwest, Dallas, Texas.
Krista R. Kelly, Retina Foundation of the Southwest, Dallas, Texas.
Joel N. Leffler, Children’s Eye Care of North Texas, PA, Plano, Texas.
Lori Dao, ABC Eyes Pediatric Ophthalmology, PA, Dallas, Texas.
Cynthia L. Beauchamp, ABC Eyes Pediatric Ophthalmology, PA, Dallas, Texas.
REFERENCES
- 1.Kelly KR, Jost RM, Dao L, et al. Binocular iPad Game Vs Patching for Treatment of Amblyopia in Children: A Randomized Clinical Trial. JAMA Ophthalmol 2016;134:1402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallace DK, Repka MX, Lee KA, et al. Amblyopia Preferred Practice Pattern(R). Ophthalmology 2018;125:P105–42. [DOI] [PubMed] [Google Scholar]
- 3.Beck RW, Moke PS, Turpin AH, et al. A Computerized Method of Visual Acuity Testing: Adaptation of the Early Treatment of Diabetic Retinopathy Study Testing Protocol. Am J Ophthalmol 2003;135:194–205. [DOI] [PubMed] [Google Scholar]
- 4.Holmes JM, Beck RW, Repka MX, et al. The Amblyopia Treatment Study Visual Acuity Testing Protocol. Arch Ophthalmol 2001;119:1345–53. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum AL, Santiago AP. Clinical Strabismus Management : Principles and Surgical Techniques. Philadelphia: Saunders; 1999. [Google Scholar]
- 6.Holmes JM, Lazar EL, Melia BM, et al. Effect of Age on Response to Amblyopia Treatment in Children. Arch Ophthalmol 2011;129:1451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pediatric Eye Disease Investigator Group. A Randomized Trial of Patching Regimens for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol 2003;121:603–11. [DOI] [PubMed] [Google Scholar]
- 8.Pediatric Eye Disease Investigator Group. A Randomized Trial of Prescribed Patching Regimens for Treatment of Severe Amblyopia in Children. Ophthalmology 2003;110:2075–87. [DOI] [PubMed] [Google Scholar]
- 9.Repka MX, Kraker RT, Beck RW, et al. Treatment of Severe Amblyopia with Weekend Atropine: Results from 2 Randomized Clinical Trials. J AAPOS 2009;13(3):258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Repka MX, Cotter SA, Beck RW, et al. A Randomized Trial of Atropine Regimens for Treatment of Moderate Amblyopia in Children. Ophthalmology 2004;111(11):2076–85. [DOI] [PubMed] [Google Scholar]
- 11.Stewart CE, Stephens DA, Fielder AR, Moseley MJ. Objectively Monitored Patching Regimens for Treatment of Amblyopia: Randomised Trial. BMJ 2007;335:707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart CE, Stephens DA, Fielder AR, Moseley MJ. Treatment of Unilateral Amblyopia: Factors Influencing Visual Outcome. Invest Ophthalmol Vis Sci 2005. September;46:3152–60 [DOI] [PubMed] [Google Scholar]
- 13.Holmes JM, Manh VM, Lazar EL, et al. Effect of a Binocular ipad Game vs Part-Time Patching in Children Aged 5 to 12 Years with Amblyopia: A Randomized Clinical Trial. JAMA Ophthalmol 2016;134:1391–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pediatric Eye Disease Investigator Group. A Randomized Trial Comparing Bangerter Filters and Patching for the Treatment of Moderate Amblyopia in Children. Ophthalmology 2010;117:998–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J, Neely DE, Galli J, et al. A Pilot Randomized Clinical Trial of Intermittent Occlusion Therapy Liquid Crystal Glasses Versus Traditional Patching for Treatment of Moderate Unilateral Amblyopia. J AAPOS 2016;20:326–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart CE, Moseley MJ, Stephens DA, Fielder AR. Treatment Dose-Response in Amblyopia Therapy: the Monitored Occlusion Treatment of Amblyopia Study (MOTAS). Invest Ophthalmol Vis Sci 2004;45:3048–54. [DOI] [PubMed] [Google Scholar]
- 17.Leske DA, Holmes JM. Maximum Angle of Horizontal Strabismus Consistent with True Stereopsis. J AAPOS 2004;8:28–34. [DOI] [PubMed] [Google Scholar]