Evidence to date has focused on assessing the individual prevalence and impact of comorbidities in patients with coronavirus disease (COVID-19) [1]. We aimed to investigate the pattern of the most prevalent combinations of multimorbidity (i.e. presence of two or more pre-existing chronic diseases) in those infected with SARS-CoV-2.
UK Biobank (https://www.ukbiobank.ac.uk/) is a large prospective cohort of middle-aged adults. Assessments were conducted between 2006 and 2010. Self-reported medical information based on physician diagnosis was included to determine long-term cardiovascular, non-cardiovascular, or mental health conditions. Three sources were used to select conditions; first: the Quality and Outcomes Framework reports the most common diseases in the UK [2]; second: a large UK based study containing 40 recommended disorders [3]; third: a systematic review on multimorbidity indices including 17 conditions [4]. Based on these we selected 36 chronic conditions (supplementary). The ten most prevalent co-occurring chronic conditions from these 36 (threshold ≥5 participants) are presented. SARS-CoV-2 test results from Public Health England were linked to UK Biobank database [5]. Data was available between March 16 and May 03, 2020. Descriptive analyses were performed.
From 502,543 UK Biobank participants, 3002 have been tested for SARS-CoV-2 infection in England, of which 1073 (36%) tested positive; median age was 70 (interquartile range 59–76) years, 54% were males, 85% were white, 5% South Asian, 6% black, and 4% other ethnicity.
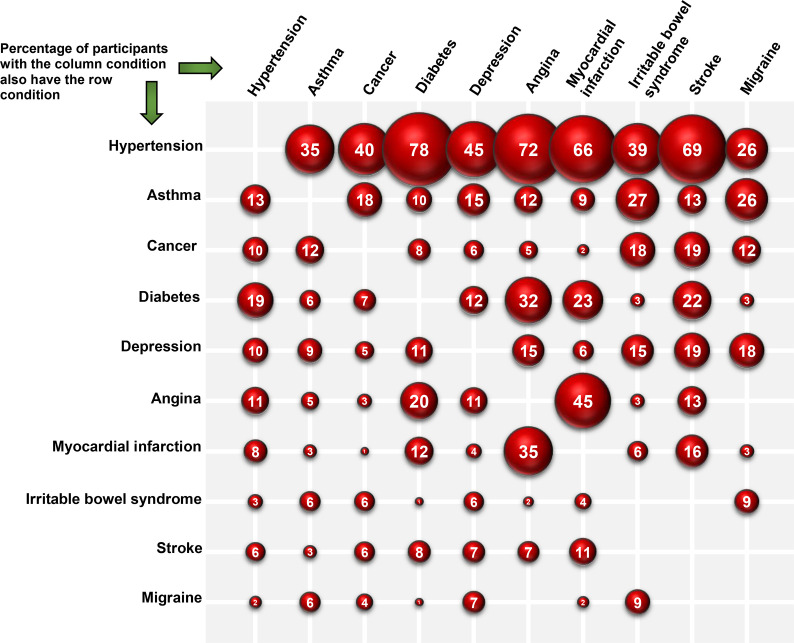
At baseline, 31% (n = 329) had multimorbidity (two or more pre-existing chronic conditions). The most prevalent combinations of multimorbidity were predominantly clustered around cardiometabolic conditions: diabetes and hypertension (78% of participants with diabetes had hypertension), angina and hypertension (72% of participants with angina), stroke and hypertension (69% of participants with stroke), myocardial infarction (MI) and hypertension (66% of participants with MI), depression and hypertension (45% of participants with depression), MI and angina (45% of participants with MI). Within non-cardiovascular diseases, common combinations included irritable bowel syndrome (IBS) and asthma (27% of participants with IBS), migraine and asthma, and mental-ill health (particularly depression) in combination with cardiometabolic conditions, Fig. 1 .
Fig. 1.
The most common co-occurring chronic diseases at baseline assessment of UK Biobank participants with multimorbidity and tested positive for SARS-CoV-2 infection (n = 329), between March 16 and May 03, 2020.
A limitation of this analysis is that data on pre-existing chronic diseases was collected at baseline, and participants may have since developed other chronic conditions; and possible selection bias. However, these results are important as they provide better understanding of the number and type of chronic disease combinations most commonly found in those testing positive for SARS-CoV-2 infection. As more data emerges on those with multimorbidity, it is crucial to clarify the burden of severity and mortality in people with COVID-19.
Funding/support
The National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC-EM). Data was analysed using UK Biobank application number 36371.
Ethical approval and informed consent
All participants gave written informed consent prior to data collection. UK Biobank has full ethical approval from the NHS National Research Ethics Service (16/NW/0274).
Data access and responsibility
The data that support the findings of this study are available from UK Biobank project site, subject to registration and application process. Further details can be found at https://www.ukbiobank.ac.uk.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dsx.2020.06.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doran T., Kontopantelis E., Reeves D., Sutton M., Ryan A.M. Setting performance targets in pay for performance programmes: what can we learn from QOF? BMJ Br Med J (Clin Res Ed) 2014:348. doi: 10.1136/bmj.g1595. [DOI] [PubMed] [Google Scholar]
- 3.Barnett K., Mercer S.W., Norbury M., Watt G., Wyke S., Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 4.Diederichs C., Berger K., Bartels D.B. The measurement of multiple chronic diseases—a systematic review on existing multimorbidity indices. J. Gerontol. Series A: Biol. Sci. Med. Sci. 2011;66(3):301–311. doi: 10.1093/gerona/glq208. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong J., Rudkin J., Allen N., Crook D., Wilson D., Wyllie D. Dynamic linkage of COVID-19 test results between public health england’s second generation surveillance system and UK Biobank. Microbial Genomics. 2020 doi: 10.1099/mgen.0.000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.