Abstract
Background
The epidemic potential of coronavirus infection is now a reality. Since the first case detected in late 2019 in China, a fast worldwide expansion confirms it. The vascular patient is at a higher risk of developing a severe form of the disease because of its nature associating several comorbid states, and thus, some vascular surgery communities from many countries have tried to stratify patients into those requiring care during these uncertain times.
Methods
This is an observational study describing the current daily vascular surgery practice at one tertiary academic hospital in Madrid region, Spain—one of the most affected regions worldwide due to the COVID-19 outbreak. We analyzed our surgical practice since March 14th when the lockdown was declared up to date, May 14th (2 months).
Procedural surgical practice, organizational issues, early outcomes, and all the troubles encountered during this new situation are described.
Results
Our department is composed of 10 vascular surgeons and 4 trainees. Surgical practice has been reduced to only urgent care, totaling 50 repairs on 45 patients during the period. Five surgeries were performed on 3 COVID-19-positive patients. Sixty percent were due to critical limb ischemia, 45% of them performed by complete endovascular approach, whereas less than 10% of repairs were aorta related. We were allocated to use a total of 5 surgical rooms in different locations, none our usual, as it was converted into an ICU room while performing 50% of those repairs with unusual nursery staff.
Conclusions
The COVID-19 outbreak has dramatically changed our organization and practice in favor of urgent or semiurgent surgical care alone. The lack of in-hospital/ICU beds and changing nursery staff changed the whole availability organization at our hospital and was a key factor in surgical decision-making in some cases.
Introduction
The epidemic potential of coronavirus infection is now a reality. Since the first case detected in late 2019 in China, a fast worldwide expansion confirms it. The current knowledge of the disease describes mostly on a severe acute respiratory syndrome (SARS-CoV-2) while many other clinical descriptions of the disease have also been reported, such as peripheral arterial thrombosis,1 , 2 myocarditis, or central nervous system affections.
The first reported case in Spain was on January 31st, and since then, the rapid spread of the virus has been demonstrated as the numbers of confirmed diagnosis (231,000) and deaths (27,650) have dramatically increased daily, with the last week reaching the smaller number of deaths per day (less than 100).
The vascular patient due to its nature associating several comorbid states should be considered at higher risk when compared with other populations.3 Some vascular surgery communities have tried to stratify patients into those requiring urgent care during this pandemic situation, that is, > 70 mm abdominal aortic aneurysms or ruptured abdominal aortic aneurysms, critical limb ischemia (CLI), and symptomatic carotid disease.4 Hospital organization strictly depends on the pandemic situation, as in-hospital and intensive care unit (ICU) beds availability, surgical room disposals, and nursery staff.
Methods
This is an observational study describing the current daily practice at one tertiary academic hospital in Madrid region, Spain—one of the most affected regions worldwide due to the COVID-19 outbreak. We analyzed our surgical practice since March 14th when the lockdown was declared up to date (8 weeks).
Procedural surgical practice, organizational issues, early outcomes and all the troubles encountered during this new situation are described.
Results
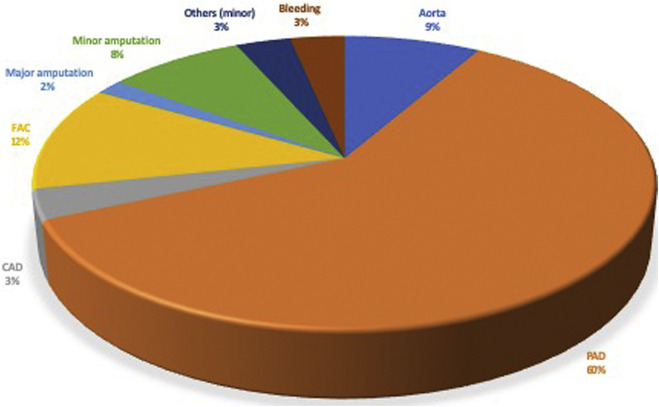
Our surgical activity has dramatically been reduced to minimums. We only provided surgical care for urgent cases, and during the last two weeks, as the COVID-19 situation improved and more in-hospital beds and resources are available, we started to provide care to patients requiring a vascular access, limb ischemia with rest pain and one carotid with severe stenosis with unstable plaque. Figure 1 shows a pie-chart with those procedures performed during the study period, describing on 60 interventions performed in 50 patients.
Fig. 1.
Distribution of surgical repairs during the study period.
All surgical procedures were performed outside our usual surgical room. We have changed our surgical room 5 times (like nearly all the other surgical departments), whereas up to 50% of repairs have been performed without our usual nursery staff.
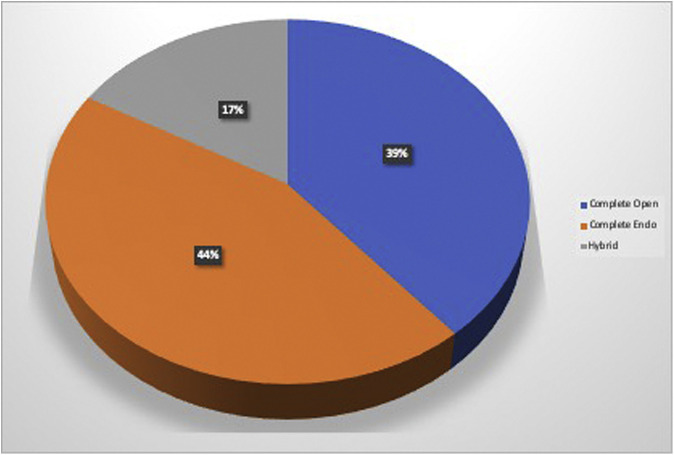
The vast majority of interventions were related to CLI revascularization (60%), where nearly 40% where performed by open means, as shown in Figure 2 .
Fig. 2.
Type of revascularization for patients with critical limb ischemia.
Aorta-related disease was required for 5 patients. One patient receiving an axillofemoral bypass due to aortic-graft thrombosis, was tested positive for COVID-19 and after two reinterventions (one explantation and contralateral axillofemoral revascularization and one other for acute axillar stump bleeding) died of acute respiratory distress syndrome (ARDS).
Three patients received successful TEVAR treatment for acute aortic syndromes, one case with symptomatic thoracic aortic ulcer, one with intramural hematoma (IMH) and the other with postdissection symptomatic aneurysm.
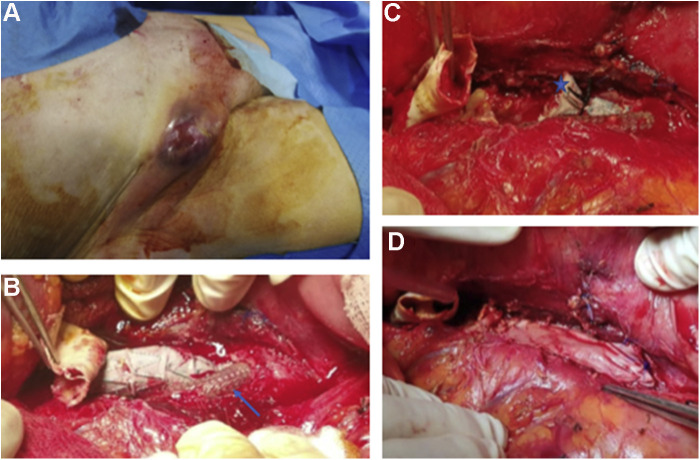
One case was previously published by this author5 where an EVAR with a hypogastric chimney precluded a highly possible fatal ischemic colitis in a patient with a previous open graft repair. He was treated afterward with an axillofemoral bypass due to open graft and endograft thrombosis and presented to the urgency room with a painful and tender mass in the groin associating fever. The CT scan confirmed infection of the axillofemoral and open-graft bypass. Figure 3 summarizes the case, where complete axillofemoral and aortic open graft explantation were performed and partial endograft explantation, maintaining the patent Viabahn in place and suturing a pericardial patch all around the aortic wall “hole” plus direct sutures in the duodenum. A new silver graft axillofemoral bypass was performed to maintain limb perfusion while patient remains good after one month of repair with specific (Staphylococcus viridans) antibiotics.
Fig. 3.
A, Infected groin; B, blue arrow showing patent Viabahn as chimney to hypogastric artery; C, blue star at partial explantation of the endograft and already explanted open surgical graft; D, pericardial patch used to cover the aorta (within the endograft and patent Viabahn).
Besides our surgical waiting list, we have 2 patients with aneurysmal disease (8 cm juxtarenal and 5 cm iliac) awaiting repair diagnosed during these COVID-19 outbreak (both tested positive and on recovery of pulmonary disease).
Discussion
Organization and surgical practice have changed dramatically during these pandemic times.6 Some countries dealing with this extreme situation as ours have been organized into surgical hubs as to hypothetically provide “the possible best care” for the whole process (diagnosis, treatment, and follow-up).7 This actually works as centralization of the vascular pathology for certain regions. Some other groups have provided COVID-19-adapted organization strategies to provide appropriate vascular care.
Madrid region has been especially hit by the coronavirus outbreak, with 6 million people (47 million for Spain) it encounters 12.7% of the country's population. The severity of the affection is demonstrated in the very high proportion of deaths, as Madrid encounters 30% of the national deaths.
Our hospital, a tertiary academic one, reaches between 500 and 550 thousand people. Since March 14th the lockdown was declared, at that time the curve of infections and deaths started to increase until reaching the sad peak of nearly 1,000 deaths/day on April 4th. The administration urgently converted nearly all surgical rooms into new ICU beds, increasing in 200% of our usual availability and reaching 95% of occupation at some point.
The challenge, as vascular surgeons, was the trouble in decision-making on who and how to operate, as we were dealing with our worst situation in terms of lack of resources (limitation of ICU beds, in-hospital beds, anesthesia team treating COVID-19 patients, nurse staff in other labors, etc.).8 Referral was not an option as this same situation was clearly evident for all private and public hospitals in the region.
Fortunately, in our center, every patient requiring urgent care did receive it at last, with lot of troubles due to a constant change in surgical rooms and nursery team.
At the peak of the outbreak, our department was split in two groups, where half of it was in COVID-19 attention and the remaining on specific vascular surgery care. This organization being dynamic depending on in-hospital COVID-19 and/or vascular care needs.
At the very beginning of the outbreak, we dealt with a disturbing lack of tests for patients and health care professionals. At some point, and this is already established, every patient requiring hospitalization received a pharyngeal swab test for diagnosis. If one needing surgical care was tested positive, one dedicated COVID-19 surgical room was provided.
During these 8 weeks, we have performed 60 operations in 50 patients. As shown in Figure 1, those were mainly for CLI representing 60% of our practice. As described previously, COVID-19 patients can associate a procoagulant state which can lead either to deep vein thrombosis (DVT) and/or peripheral arterial thrombosis. These patients with acute limb ischemia required most of the times urgent surgery, a situation we dealt with in two cases. Pertaining DVT, a previous description of 23% incidence for COVID-19 patients in ICU and 8% not requiring ventilator demonstrated the importance of such situation in these patients.7 A national registry (NCT04361981) is currently starting to better understand this situation and provide accurate data in the near future.
Interestingly, from those treated for CLI, 40% were treated by open revascularization techniques in our department. This in part due to the aforementioned limitations related to organization as the recommendations standards given by other vascular communities is directed toward total endovascular approach. We also treated 5 patients with aortic diseases, and one of them would have received a different treatment in normal conditions. The decision to perform an axillofemoral bypass was due to the risk of visceral embolization and absolute lack of ICU bed. Three other patients received TEVAR for IMH, thoracic penetrating aortic ulcer, and enlarging symptomatic thoracic aortic aneurysm, respectively, despite the limitations, as the open options were extremely risky. The benefits of EVAR/TEVAR during the COVID-19 outbreak have been described.9 , 10
Two patients were treated for carotid disease, with conventional patch endarterectomy, and 7 patients for hemodialysis access (fistula creation) by open means as well.
Although endovascular procedures are highly recommended during these times being less invasive and needing less in-hospital resources, we needed to adapt our decisions and surgical actions to the changing reality in our hospital, where lack of ICU beds and changes in surgical rooms and nursery staffs had a clear incidence in our decisions.
Finally, from those with positive test for COVID-19, 2 were CLI with successful repair and the remaining, the abovementioned case of aortic graft thrombosis who unfortunately died of ARDS. The increased risk of fatality for a surgical repair in COVID-19 patients is previously described.11
We are now into the “going back to the normal” process; however, a considerable grade of uncertainty comes for the future where our weakened health system will need to deal with an unprecedented scenario that might surpass again our available resources.
Conclusions
The COVID-19 outbreak has dramatically changed our organization and practice in favor of urgent or semiurgent surgical care alone. The lack for in-hospital/ICU beds and changing nursery staff changed the whole availability organization at our hospital and was a key factor in surgical decision-making in some cases.
Footnotes
Conflict of interests: None.
Funding: None.
References
- 1.Valdivia A.R., Olmos C.G., Guaita J.O. Cardiovascular examination should also include peripheral arterial evaluation for COVID-19 patients. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellosta R., Luzzani L., Natalini G. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inciardi R.M., Adamo M., Lupi L. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forbes T.L. Vascular surgery activity condition is a common language for uncommon times. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reyes Valdivia A., Santos A.D., Guaita J.O. Hypogastric chimney patency in aortic monoiliacal endograft thrombosis: a life saved by collateral pelvic circulation. Int J Angiol. 2018;27:46–49. doi: 10.1055/s-0037-1602373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ben Abdallah I., Coscas R., Javerliat I. Early experience in paris with the impact of the covid-19 pandemic on vascular surgery. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melissano G., Mascia D., Baccellieri D. Pattern of vascular disease in lombardia (Italy) during the first month of the COVID-19 outbreak. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reyes Valdivia A., Gandarias Zuniga C., Riambau V. Vascular life during the COVID-19 pandemic reminds us to prepare for the unexpected. Eur J Vasc Endovasc Surg. 2020 doi: 10.1016/j.ejvs.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rinaldi L.F., Marazzi G., Marone E.M. Endovascular treatment of a ruptured pararenal abdominal aortic aneurysm in a COVID-19 patient: suggestions and case report. Ann Vasc Surg. 2020 doi: 10.1016/j.avsg.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griffin C.L., Sharma V., Sarfati M.R. Aortic disease in the time of COVID: repercussions on patient care at an academic aortic center. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aminian A., Safari S., Razeghian-Jahromi A. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]