Abstract
Background
Convalescent plasma and hyperimmune immunoglobulin may reduce mortality in patients with respiratory virus diseases, and are currently being investigated in trials as a potential therapy for coronavirus disease 2019 (COVID‐19). A thorough understanding of the current body of evidence regarding the benefits and risks is required.
Objectives
To assess whether convalescent plasma or hyperimmune immunoglobulin transfusion is effective and safe in the treatment of people with COVID‐19.
Search methods
The protocol was pre‐published with the Center for Open Science and can be accessed here: osf.io/dwf53
We searched the World Health Organization (WHO) COVID‐19 Global Research Database, MEDLINE, Embase, Cochrane COVID‐19 Study Register, Centers for Disease Control and Prevention COVID‐19 Research Article Database and trials registries to identify ongoing studies and results of completed studies on 23 April 2020 for case‐series, cohort, prospectively planned, and randomised controlled trials (RCTs).
Selection criteria
We followed standard Cochrane methodology and performed all steps regarding study selection in duplicate by two independent review authors (in contrast to the recommendations of the Cochrane Rapid Reviews Methods Group).
We included studies evaluating convalescent plasma or hyperimmune immunoglobulin for people with COVID‐19, irrespective of disease severity, age, gender or ethnicity.
We excluded studies including populations with other coronavirus diseases (severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS)) and studies evaluating standard immunoglobulins.
Data collection and analysis
We followed recommendations of the Cochrane Rapid Reviews Methods Group regarding data extraction and assessment.
To assess bias in included studies, we used the assessment criteria tool for observational studies, provided by Cochrane Childhood Cancer. We rated the certainty of evidence using the GRADE approach for the following outcomes: all‐cause mortality at hospital discharge, improvement of clinical symptoms (7, 15, and 30 days after transfusion), grade 3 and 4 adverse events, and serious adverse events.
Main results
We included eight studies (seven case‐series, one prospectively planned, single‐arm intervention study) with 32 participants, and identified a further 48 ongoing studies evaluating convalescent plasma (47 studies) or hyperimmune immunoglobulin (one study), of which 22 are randomised.
Overall risk of bias of the eight included studies was high, due to: study design; small number of participants; poor reporting within studies; and varied type of participants with different severities of disease, comorbidities, and types of previous or concurrent treatments, including antivirals, antifungals or antibiotics, corticosteroids, hydroxychloroquine and respiratory support.
We rated all outcomes as very low certainty, and we were unable to summarise numerical data in any meaningful way. As we identified case‐series studies only, we reported results narratively.
Effectiveness of convalescent plasma for people with COVID‐19
The following reported outcomes could all be related to the underlying natural history of the disease or other concomitant treatment, rather than convalescent plasma.
All‐cause mortality at hospital discharge
All studies reported mortality. All participants were alive at the end of the reporting period, but not all participants had been discharged from hospital by the end of the study (15 participants discharged, 6 still hospitalised, 11 unclear). Follow‐up ranged from 3 days to 37 days post‐transfusion. We do not know whether convalescent plasma therapy affects mortality (very low‐certainty evidence).
Improvement of clinical symptoms (assessed by respiratory support)
Six studies, including 28 participants, reported the level of respiratory support required; most participants required respiratory support at baseline. All studies reported improvement in clinical symptoms in at least some participants. We do not know whether convalescent plasma improves clinical symptoms (very low‐certainty evidence).
Time to discharge from hospital
Six studies reported time to discharge from hospital for at least some participants, which ranged from four to 35 days after convalescent plasma therapy.
Admission on the intensive care unit (ICU)
Six studies included patients who were critically ill. At final follow‐up the majority of these patients were no longer on the ICU or no longer required mechanical ventilation.
Length of stay on the ICU
Only one study (1 participant) reported length of stay on the ICU. The individual was discharged from the ICU 11 days after plasma transfusion.
Safety of convalescent plasma for people with COVID‐19
Grade 3 or 4 adverse events
The studies did not report the grade of adverse events after convalescent plasma transfusion. Two studies reported data relating to participants who had experienced adverse events, that were presumably grade 3 or 4. One case study reported a participant who had moderate fever (38.9 °C). Another study (3 participants) reported a case of severe anaphylactic shock. Four studies reported the absence of moderate or severe adverse events (19 participants). We are very uncertain whether or not convalescent plasma therapy affects the risk of moderate to severe adverse events (very low‐certainty evidence).
Serious adverse events
One study (3 participants) reported one serious adverse event. As described above, this individual had severe anaphylactic shock after receiving convalescent plasma. Six studies reported that no serious adverse events occurred. We are very uncertain whether or not convalescent plasma therapy affects the risk of serious adverse events (very low‐certainty evidence).
Authors' conclusions
We identified eight studies (seven case‐series and one prospectively planned single‐arm intervention study) with a total of 32 participants (range 1 to 10). Most studies assessed the risks of the intervention; reporting two adverse events (potentially grade 3 or 4), one of which was a serious adverse event. We are very uncertain whether convalescent plasma is effective for people admitted to hospital with COVID‐19 as studies reported results inconsistently, making it difficult to compare results and to draw conclusions. We identified very low‐certainty evidence on the effectiveness and safety of convalescent plasma therapy for people with COVID‐19; all studies were at high risk of bias and reporting quality was low.
No RCTs or controlled non‐randomised studies evaluating benefits and harms of convalescent plasma have been completed. There are 47 ongoing studies evaluating convalescent plasma, of which 22 are RCTs, and one trial evaluating hyperimmune immunoglobulin. We will update this review as a living systematic review, based on monthly searches in the above mentioned databases and registries. These updates are likely to show different results to those reported here.
Plain language summary
Plasma from people who have recovered from COVID‐19 to treat individuals with COVID‐19
Background
Coronavirus (COVID‐19) is a highly infectious respiratory illness caused by a new strain of virus. The outbreak has spread rapidly on a global scale. People infected with this virus may not show signs of the disease, others may develop symptoms, including fever, cough, shortness of breath and sore throat. In some people the infection is more severe and can cause severe breathing difficulties, leading to hospitalisation, admission to intensive care or death. Currently, no vaccine or specific treatment is available.
People who have recovered from COVID‐19 develop natural defences to the disease in their blood (antibodies). Antibodies are found in part of the blood called plasma. Plasma from blood donated from recovered patients, which contains COVID‐19 antibodies, can be used to make two preparations. Firstly, convalescent plasma, which is plasma that contains these antibodies. Secondly, hyperimmune immunoglobulin, which is more concentrated, and therefore contains more antibodies.
Convalescent plasma and hyperimmune immunoglobulin have been used successfully to treat other respiratory viruses. These treatments (given by a drip or injection) are generally well‐tolerated, but unwanted effects can occur.
What did we want to find?
We wanted to know whether plasma from people who have recovered from COVID‐19 is an effective treatment for people with COVID‐19, and whether this treatment causes any unwanted effects.
Our methods
We searched major medical databases for clinical studies on treatment with convalescent plasma or hyperimmune immunoglobulin for people with COVID‐19. Studies could be conducted anywhere in the world and include participants of any age, gender or ethnicity, with mild, moderate or severe COVID‐19.
COVID‐19 is spreading rapidly, so we needed to answer this question quickly. This meant that we shortened some steps of the normal Cochrane Review process ‐ only one review author extracted data from studies and assessed study quality; normally two review authors would do this.
Key results
We included eight completed studies, with 32 participants who received convalescent plasma. None of the studies randomly allocated participants to different treatments (randomised trials produce the best evidence). None of the studies included a group of people who did not receive convalescent plasma, as a comparison group.
All participants in the studies were alive at the end of follow‐up, but not all had been discharged from hospital. Follow‐up varied from 3 to 37 days after treatment with convalescent plasma.
Six studies used the level of breathing support that participants required as a measure of recovery. Breathing support included oxygen therapy, mechanical ventilation and the need for a special machine that oxygenates the blood. All six studies reported clinical improvement in at least some of their participants, but it remains uncertain whether this improvement was related to convalescent plasma, another treatment, or the natural progression of the disease.
Six studies reported time to discharge from hospital for some of their participants, all of whom received convalescent plasma. The time to discharge ranged from 4 to 35 days after convalescent plasma treatment.
Six studies included participants with severe COVID‐19. Most had improved at final follow‐up, but this improvement may have been due to another treatment, the natural progression of the disease or convalescent plasma treatment.
Two participants reported unwanted effects related to convalescent plasma. One participant developed a fever, and a second participant experienced anaphylactic shock (severe allergic reaction) early on in the transfusion.
Certainty of the evidence
Our certainty (confidence) in the evidence was very limited because the studies were not randomised and did not use reliable methods to measure their results. Furthermore, they had only a small number of participants, who received various treatments alongside convalescent plasma, and some had underlying health problems.
Conclusion
We are very uncertain whether plasma from people who have recovered from COVID‐19 is an effective treatment for people with COVID‐19. The completed studies we found were poor quality and their results could be related to the natural progression of the disease, other treatments that the participants received, or to convalescent plasma. However, our searches found 48 ongoing studies: 47 evaluating convalescent plasma and 1 evaluating hyperimmune immunoglobulin, of which 22 are randomised. We will update this review with their results when these studies are completed.
Background
Description of the condition
The clinical syndrome coronavirus disease 2019 (COVID‐19) is a new, rapidly emerging zoonotic infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2; WHO 2020a). On 11 March 2020, the World Health Organization (WHO) declared the current COVID‐19 outbreak a pandemic, with the outbreak resulting in almost 3.5 million cases and over 239,000 deaths worldwide (WHO 2020b; WHO 2020c). Although there are similarities with historic coronavirus epidemics, with severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) responsible for 813 and 858 deaths respectively, the scale and impact of the COVID‐19 pandemic presents unprecedented challenges to health facilities and healthcare workers all over the world (WHO 2007; WHO 2019).
With a preliminary hospitalisation rate of 12.3 patients per 100,000 population in the USA, COVID‐19 has taken a toll on healthcare capacity, and especially on intensive care unit (ICU) capacity (CDC 2020a). Early reports of the case fatality rate suggest that it ranges between of 0.7% to 4%, with higher rates also reported (WHO 2020a; WHO 2020c). However, these numbers should be interpreted with great care due to the data pertaining to the early emergency response, which due to shortage of test kits has led to selective testing of people with severe disease, underreporting of cases and delays from confirmation of a case to time of death (Kim 2020). The median incubation period of SARS‐CoV‐2 was reported to be five days, with 97.5% of cases developing symptoms within 11.5 days of infection (Lauer 2020). Common signs and symptoms can include fever, dry cough, fatigue and sputum production (WHO 2020a). Other, less commonly reported signs and symptoms are shortness of breath, sore throat, headache, myalgia or arthralgia, chills, nausea or vomiting, nasal congestion, diarrhoea, haemoptysis and conjunctival congestion (WHO 2020a). Of the reported cases, 80% are estimated to have a mild or asymptomatic course of infection, and an estimated 5% of cases are admitted to the ICU with acute respiratory distress syndrome (ARDS), septic shock or multiple organ failure, or both (Team 2020; WHO 2020a). A risk factor for developing infection and progressing to severe disease is old age, with people aged over 80 years at highest risk of mortality. Other risk factors are cardiovascular disease, obesity, hypertension, diabetes, chronic respiratory disease, cancer and compromised immune status (Chen 2020; Huang 2020; Liang 2020; WHO 2020a; Wu 2020a).
SARS‐CoV‐2 is a positive‐sense, single‐stranded RNA (ribonucleic acid) virus with a large RNA genome. Although not much is known about the specific mechanisms underlying severe disease in COVID‐19, there are indications that the virus is capable of inducing an excessive immune reaction in the host, with highly activated but decreased numbers of CD4+ and CD8+ T cells detected in the peripheral blood of people with COVID‐19 (Xu 2020). Early reports also showed that people critically ill with COVID‐19 frequently exhibit a hypercoagulable state and endothelial inflammation, which is hypothesised to lead to the high burden of thromboembolic events seen in this population (Driggin 2020). Preliminary reports into the pathophysiology of SARS‐CoV‐2 have further indicated that the observed decrease in human angiotensin‐converting enzyme 2 (ACE2) activity may play a role in causing the rapid deterioration of patient lung function (Tolouian 2020; Van de Veerdonk 2020). ACE2 is a protein that functions as the receptor facilitating entry of SARS‐CoV‐2 into the host cell, and is most abundant on type II alveolar cells in the lungs.
Description of the intervention
Convalescent plasma, convalescent serum and hyperimmune immunoglobulin prepared from convalescent plasma, are interventions that have been used in the past to treat conditions when no vaccine or pharmacological interventions were available. Diphtheria, pneumococcal pneumonia, hepatitis A and B, mumps, polio, measles and rabies are conditions where convalescent plasma has been shown to be effective (Eibl 2008).
A systematic review has shown that convalescent plasma may have clinical benefit for people with influenza and SARS (Mair‐Jenkins 2015). This systematic review included observational studies and randomised controlled trials (RCTs) investigating the use of convalescent plasma, serum or hyperimmune immunoglobulin for treating severe acute respiratory infections of laboratory‐confirmed or suspected viral aetiology, and included investigations with patients of any age and sex. Control interventions consisted of sham, or placebo, therapy and no therapy. The authors concluded that, although the included studies were generally small and of low quality, with a moderate to high risk of bias, the use of convalescent plasma may reduce mortality and appears safe (Mair‐Jenkins 2015). The authors also suggested that the effectiveness of convalescent plasma in reducing hospital length of stay is dependent on early administration of the therapy, and use as prophylaxis is more likely to be beneficial than treating severe disease. However, the optimal timing and dosage of convalescent plasma therapy is unknown.
There is conflicting evidence about the effect of convalescent plasma or hyperimmune immunoglobulin for treating severe acute respiratory infections. Studies investigating the effectiveness of hyperimmune immunoglobulin for influenza have been contradictory, with some RCTs showing effectiveness (Hung 2013), whereas others show no benefit (Beigel 2017; Beigel 2019; Davey 2019).
Although convalescent plasma is generally thought to be a safe and well‐tolerated therapy, adverse events can occur. Limited information is available about specific adverse events related to convalescent plasma therapy, but symptoms that have been reported are similar to those for other types of plasma blood components, including fever or chills, allergic reactions, and transfusion‐related acute lung injury (TRALI; Beigel 2019; Chun 2016; Luke 2006). Furthermore, the transfer of coagulation factors present in plasma products is potentially harmful for people with COVID‐19, who are already at an increased risk of thromboembolic events (Driggin 2020). Plasma transfusions are also known to cause transfusion‐associated circulatory overload (TACO). TACO and TRALI are especially important to consider, because COVID‐19 patients with comorbidities, who might be eligible for experimental treatment with convalescent plasma therapy, are at an increased risk of these adverse events. There are risk‐mitigation strategies that can be implemented to prevent TRALI. These include limiting donations from female donors, especially those with a history of pregnancy, and screening of donors for antibodies that are implicated in TRALI (Otrock 2017). In addition to the aforementioned adverse events, transfusion‐transmitted infections, red blood cell alloimmunisation and haemolytic transfusion reactions have also been described following plasma transfusion, although they are less common (Pandey 2012). Pathogen inactivation can be implemented to decrease the risk of transmitting infections by transfusion (Rock 2011).
When compared to convalescent plasma, hyperimmune immunoglobulin has the advantage of preventing transfer of potentially harmful coagulation factors that are present in plasma products. The amount and antibody concentration can be more accurately dosed compared to convalescent plasma, and hyperimmune immunoglobulin can be prepared in a consistent manner (Hung 2013). Not many studies have reported on adverse events of hyperimmune immunoglobulin, but the safety profile of standard intravenous immunoglobulin is known and the adverse events reported here are also likely to occur in hyperimmune immunoglobulin therapy. Common adverse events of intravenous immunoglobulin that occur immediately after administration are: infusion site pain; swelling and erythaema; and immediate systemic reactions, such as head and body aches, chills and fever (Stiehm 2013). Other, less common early adverse reactions to immunoglobulin therapy are pulmonary complications, such as pulmonary embolism, pulmonary oedema and pleural effusion, with TRALI also reported (Baudel 2020; Stiehm 2013). Anaphylactic and anaphylactoid reactions to immunoglobulin therapy are rare (Brennan 2003; Stiehm 2013). Delayed adverse events of immunoglobulin therapy, which occur within hours to days of initiation of immunoglobulin therapy, are persistent headaches (common), aseptic meningitis, renal failure, thromboembolic events, and haemolytic reactions (Sekul 1994; Stiehm 2013). Transmission of infectious agents has been described after administration of intravenous immunoglobulin, but this risk is considered to be low (Stiehm 2013). Other, severe adverse events that occur late after administration are lung disease, enteritis and dermatological disorders (Stiehm 2013).
A theoretical risk related to virus‐specific antibodies, which are transferred with convalescent plasma and hyperimmune immunoglobulin administration, is antibody‐dependent enhancement of infection (Morens 1994). Here, virus‐binding antibodies facilitate the entry and replication of virus particles into monocytes, macrophages and granulocytic cells and thereby increase the risk of more severe disease in the infected host. Although antibody‐dependent enhancement has not been demonstrated in COVID‐19, it has been seen with previous coronavirus infections when the antibodies given targeted a different serotype of the virus (Wan 2020; Wang 2014). A mechanism for antibody‐dependent enhancement in COVID‐19 has recently been proposed, with non‐neutralising antibodies to variable S domains potentially enabling an alternative infection pathway via Fc receptor‐mediated uptake (Ricke 2020). Antibody‐dependent enhancement is therefore a potentially harmful consequence of convalescent plasma and hyperimmune immunoglobulin therapy for COVID‐19.
In summary, the benefits of the intervention, both for convalescent plasma or hyperimmune immunoglobulin, should be carefully considered in view of the risks of adverse events.
How the intervention might work
Convalescent plasma contains pathogen‐specific neutralising antibodies, which can neutralise viral particles, and treatment with convalescent plasma or hyperimmune immunoglobulins confers passive immunity to recipients. The duration of conferred protection can differ depending on the timing of administration, ranging from weeks to months after treatment (Casadevall 2020).
By neutralising SARS‐CoV‐2 particles, early treatment with convalescent plasma is postulated to increase the patient’s own capacity to clear the initial inoculum (Casadevall 2020; Robbins 1995). This could lead to a reduction in mortality and fewer hospitalised patients progressing to the ICU. Furthermore, convalescent plasma may reduce the length of ICU stay in critically ill patients (Mair‐Jenkins 2015), thus helping to lift pressure from global healthcare systems and increasing ICU capacity.
Preliminary evidence in humans and rhesus macaques has shown that reinfection with SARS‐CoV‐2 is not likely, with most (but not all) patients who recovered from COVID‐19 producing sufficient amounts of neutralising antibodies to protect against reinfection (Bao 2020; Wu 2020b). This implies that convalescent plasma from people who have recovered from SARS‐CoV‐2 infection is capable of conferring passive immunity. A recently reported case series also indicated sufficient neutralising antibody titres in convalescent plasma to neutralise SARS‐CoV‐2 in five COVID‐19 patients, who all recovered after treatment (Shen 2020). It is important to note, however, that research in other coronavirus species has shown that immunity may not be long‐lasting, with two to three years of protection estimated from work with SARS and MERS (Mo 2006; Payne 2016). Furthermore, there are indications that the severity of infection has an impact on antibody titres, with less severe disease leading to lower neutralising antibody response in people with SARS and COVID‐19 (Ho 2005; Zhao 2020).
Why it is important to do this review
There is a clear, urgent need for more information to guide clinical decision‐making for COVID‐19 patients. Pharmacological interventions have not yet proven to be effective, and current treatment consists of supportive care with extracorporeal membrane oxygenation in severe cases and oxygen supply in mild cases (CDC 2020b; WHO 2020d). A vaccine could aid in inducing immunity in the population and preventing transmission to those who are at risk for severe disease, but no vaccine is currently available, although multiple candidate vaccines are in development. Until these vaccines are available and distributed, convalescent plasma is a potential therapy for COVID‐19 patients. Convalescent plasma, and hyperimmune immunoglobulin to a certain extent, can be prepared and made rapidly available by blood banks and hospitals when enough potential donors have recovered from the infection, using readily available materials and methods (Bloch 2020). However, its safety and efficacy are not well characterised, and there are costs associated with pursuing the use of convalescent plasma for treatment of COVID‐19.
A multitude of clinical trials investigating the safety and effectiveness of convalescent plasma or hyperimmune immunoglobulins have been announced, and their results will need to be interpreted with care. Thus, there needs to be a thorough understanding of the current body of evidence regarding the use of convalescent plasma for people with COVID‐19, and an extensive review of the available literature is required.
Objectives
To assess whether convalescent plasma or hyperimmune immunoglobulin transfusion is effective and safe in the treatment of people with COVID‐19.
Methods
Criteria for considering studies for this review
Types of studies
The protocol for this review was registered with the Center for Open Science (Piechotta 2020).
As planned at the protocol stage, we included prospective non‐comparative study designs (e.g. case series), because there was no evidence from randomised controlled trials (RCTs), non‐randomised studies of interventions (NRSIs), and only one prospective observational study available (please find further explanations in Appendix 1). We followed the suggestions specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019a), as far as possible, and applied the methodology outlined in the following sections. We considered studies including one or more participant(s) with coronavirus disease 2019 (COVID‐19).
We included full‐text publications, abstract publications, and results published in trials registries, if sufficient information was available on study design, characteristics of participants, interventions and outcomes. We did not apply any limitation with respect to the length of follow‐up.
Types of participants
We included individuals with a confirmed diagnosis of COVID‐19, with no age, gender or ethnicity restrictions.
We excluded studies including populations with other coronavirus diseases (severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS)). We also excluded studies including populations with mixed virus diseases (e.g. influenza), unless the trial authors provided subgroup data for people with COVID‐19.
Types of interventions
We included the following interventions.
Convalescent plasma from people who recovered from SARS‐CoV‐2 infection
Hyperimmune immunoglobulin therapy
We did not include studies on standard immunoglobulin.
In future updates we plan to include the following comparisons for studies with a control arm.
Convalescent plasma versus standard care or placebo
Convalescent plasma therapy versus control treatment, for example, drug treatments (including but not limited to hydroxychloroquine, remdesivir). Co‐interventions will be allowed, but must be comparable between intervention groups.
Convalescent plasma therapy versus hyperimmune immunoglobulin
Hyperimmune immunoglobulin versus standard care or placebo
Hyperimmune immunoglobulin versus control treatment, for example, drug treatments (including but not limited to hydroxychloroquine, remdesivir). Co‐interventions will be allowed, but must be comparable between intervention groups.
Types of outcome measures
We evaluated core outcomes as pre‐defined by the Core Outcome Measures in Effectiveness Trials Initiative for Covid‐19 patients (COMET 2020).
Primary outcomes
Effectiveness of convalescent plasma for people with COVID‐19
All‐cause mortality at hospital discharge
Time to death
Secondary outcomes
Effectiveness of convalescent plasma for people with COVID‐19
-
Improvement of clinical symptoms, assessed by need for respiratory support at up to 7 days; 8 to 15 days; 16 to 30 days:
oxygen by mask or nasal prongs
oxygen by non‐invasive ventilation (NIV) or high‐flow
intubation and mechanical ventilation
mechanical ventilation plus high‐flow oxygen
extracorporeal membrane oxygenation (ECMO)
30‐day and 90‐day mortality
Time to discharge from hospital
Admission on the ICU
Length of stay on the ICU
Safety of convalescent plasma for people with COVID‐19
Number of participants with grade 3 and grade 4 adverse events, including potential relationship between intervention and adverse reaction (e.g. transfusion‐related acute lung injury (TRALI), transfusion‐transmitted infection, transfusion‐associated circulatory overload (TACO), transfusion‐associated dyspnoea (TAD), acute transfusion reactions)
Number of participants with serious adverse events
Timing of outcome measurement
For time‐to‐event outcomes, such as mortality, discharge from hospital, and improvement of clinical symptoms, we included outcome measures representing the longest follow‐up time available.
We included all other outcome categories for the observational periods that the study publications reported. We included those adverse events occurring during active treatment and had planned to include long‐term adverse events as well. If sufficient data had been available, we planned to group the measurement time points of eligible outcomes, for example, adverse events and serious adverse events, into those measured directly after treatment (up to seven days after treatment), medium‐term outcomes (15 days after treatment) and longer‐term outcomes (over 30 days after treatment).
Search methods for identification of studies
We searched for studies in all languages in order to limit language bias. However, we prioritised articles in languages that our review team could accommodate (these are English, Dutch, German, French, Italian, Malay and Spanish). We did not seek translators for this version of the review. We tagged all references in additional languages as 'awaiting classification' and will seek translators via Cochrane TaskExchange in an update of this review.
Electronic searches
We designed and tested search strategies for electronic databases according to methods suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2019), CD developed them and Cochrane Haematology's Information Specialist (IM) peer reviewed them. In this emerging field, we expected that at least the abstract would be in English. If studies are published in other languages than those our review team could accommodate (English, Dutch, German, French, Italian, Malay and Spanish), we plan to involve Cochrane TaskExchange to identify people within Cochrane to translate these studies for an update of this review.
As publication bias might influence all subsequent analyses and conclusions, we searched all potential relevant trials registries in detail to detect ongoing as well as completed studies, but not yet published studies. Nowadays, it is mandatory to provide results at least in the trials registry. In case results were not published elsewhere, we had planned to extract and analyse these data. However, no outcome data have yet been added to the trials registries (also stated in Differences between protocol and review).
We searched the following databases and sources, from 1 January 2019 to 23 April 2020.
-
Databases of medical literature
WHO COVID‐19 Global Research Database (search.bvsalud.org/global-research-on-novel-coronavirus-2019-ncov/advanced/?lang=en), searched 23 April 2020; Appendix 2
MEDLINE (Ovid, 1 January 2019 to 23 April 2020), Appendix 3
Embase (Ovid, 1 January 2019 to 23 April 2020), Appendix 4
PubMed (for epublications ahead of print only; searched 23 April 2020), Appendix 5
Center for Disease Control and Prevention COVID‐19 Research Article Database (www.cdc.gov/library/researchguides/2019novelcoronavirus/databasesjournals.html; downloaded 22 April 2020), Appendix 6
Cochrane COVID‐19 Study Register (covid-19.cochrane.org; searched 23 April 2020), Appendix 7
-
Trials registries and registry platforms to identify ongoing studies and results of completed studies
ClinicalTrials.gov ‐ COVID‐19 Subset (clinicaltrials.gov/ct2/results?cond=COVID-19; searched 23 April 2020), Appendix 8
WHO International Clinical Trials Registry Platform (ICTRP) ‐ COVID‐19 Subset (www.who.int/ictrp/en); searched 23 April 2020), Appendix 9
Searching other resources
In an update of this rapid review we plan to:
handsearch the reference lists of all identified studies, relevant review articles and current treatment guidelines for further literature; and
contact experts in the field, drug manufacturers and regulatory agencies in order to retrieve information on unpublished studies.
Data collection and analysis
Selection of studies
Two out of four review authors (SJV, KLC, VP, NS) independently screened the results of the search strategies for eligibility for this review by reading the abstracts using Covidence software. We coded the abstracts as either 'retrieve' or 'do not retrieve'. In the case of disagreement or if it was unclear whether we should retrieve the abstract or not, we obtained the full‐text publication for further discussion. Two review authors assessed the full‐text articles of selected studies. If the two review authors were unable to reach a consensus, they consulted a third review author to reach a final decision.
We documented the study selection process in a flow chart, as recommended in the PRISMA statement (Moher 2009), and show the total numbers of retrieved references and the numbers of included and excluded studies. We list all articles that we excluded after full‐text assessment and the reasons for their exclusion in the Characteristics of excluded studies table.
Data extraction and management
One review author (SJV or KLC) performed all data extractions and assessments. Two other review authors (VP, NS) verified the accuracy and (where applicable) the plausibility of extractions and assessment.
One review author (VP or NS) assessed eligible studies obtained in the process of study selection (as described above) for methodological quality and risk of bias, the other review author verified the 'Risk of bias' assessment.
One review author (SJV or KLC) extracted data using a customised data extraction form developed in Microsoft Excel (Microsoft Corporation 2018); please see Differences between protocol and review). Another review author (NS) verified the accuracy and (where applicable) the plausibility of extractions and assessment. We conducted data extraction according to the guidelines proposed by Cochrane (Li 2019). If the review authors were unable to reach a consensus, we consulted a third review author (VP).
We collated multiple reports of one study so that the study, and not the report, is the unit of analysis.
We extracted the following information.
General information: author, title, source, publication date, country, language, duplicate publications
Quality assessment: study design, confounding, definition of risk estimates, selection bias, attrition bias, detection bias, reporting bias
Study characteristics: trial design, setting and dates, source of participants, inclusion/exclusion criteria, comparability of groups, treatment cross‐overs, compliance with assigned treatment, length of follow‐up
Participant characteristics: age, gender, ethnicity, number of participants recruited/allocated/evaluated, disease, severity of disease, additional diagnoses, previous treatments (e.g. experimental drug therapies, oxygen therapy, ventilation)
-
Interventions: convalescent plasma therapy or hyperimmune immunoglobulin therapy, concomitant therapy, duration of follow‐up
For studies including a control group: comparator (type)
-
Outcomes
-
Effectiveness of convalescent plasma for people with COVID‐19:
all‐cause mortality at hospital discharge
time to death
improvement of clinical symptoms, assessed through need for respiratory support at up to 7 days; 8 to 15 days; 16 to 30 days
30‐day and 90‐day mortality
time to discharge from hospital
admission on the ICU
length of stay on the ICU
-
Safety of convalescent plasma for people with COVID‐19:
number of participants with grade 3 and grade 4 adverse events, including potential relationship between intervention and adverse reaction (e.g. TRALI, transfusion‐transmitted infection, TACO, TAD, acute transfusion reactions)
number of participants with serious adverse events
-
Assessment of risk of bias in included studies
If RCT data had been available, we had planned to use the Risk of Bias 2.0 (RoB 2) tool to analyse the risk of bias in the underlying study results (Sterne 2019). If non‐randomised studies of interventions (NRSIs) data had been available, we had planned to use the Risk Of Bias in Non‐randomised Studies ‐ of Interventions (ROBINS‐I) tool (Sterne 2016). Please refer to Appendix 1 for detailed information regarding how we had planned to assess the risk of bias of RCTs and NRSIs.
Non‐controlled, prospectively planned studies
As specified in the Types of studies section we only included non‐controlled prospective studies because we did not identify any controlled studies.
One review author (VP or NS) assessed eligible studies for methodological quality and risk of bias (using the 'Risk of bias' assessment criteria for observational studies tool provided by Cochrane Childhood Cancer (see Table 1; Mulder 2019). A second review author (VP or NS) verified the accuracy and the plausibility. Any 'Risk of bias' judgements were performed and presented per outcome per study.
1. 'Risk of bias' assessment criteria for observational studies.
| Heading | Internal validity | External validity |
| Study group |
Selection bias (representative: yes/no)
or
|
Reporting bias (well defined: yes/no)
and
|
| Follow‐up |
Attrition bias (adequate: yes/no)
or
|
Reporting bias (well defined: yes/no)
|
| Outcome |
Detection bias (blind: yes/no)
|
Reporting bias (well defined: yes/no)
|
| Risk estimation |
Confounding (adjustment for other factors: yes/no)
|
Analyses (well defined: yes/no)
|
The quality assessment strongly depends upon information on the design, conduct and analysis of the trial. The two review authors (VP, NS) resolved any disagreements regarding the quality assessments by discussion, in case of disagreement they would have consulted a third review author (SJV or KLC).
We assessed the following domains of bias.
-
Internal validity
Unrepresentative study group (selection bias)
Incomplete outcome assessment/follow‐up (attrition bias)
Outcome assessors unblinded to investigated determinant (detection bias)
Important prognostic factors or follow‐up not taken adequately into account (confounding)
-
External validity
Poorly defined study group (reporting bias)
Poorly defined follow‐up (reporting bias)
Poorly defined outcome (reporting bias)
Poorly defined risk estimates (analyses)
For every criterion, we made a judgement using one of three response options.
High risk of bias
Low risk of bias
Unclear risk of bias
Measures of treatment effect
Please refer to Appendix 1 for information regarding how we had planned to measure the treatment effects of RCTs and NRSIs.
Uncontrolled studies
For uncontrolled studies we did not carry out an analysis using quantitative data from indirect controls, as we are aware of the difficulties of indirect comparisons of participant groups with varying baseline characteristics, especially in the absence of individual patient data. Because authors of one‐arm, non‐comparative studies, often discuss their findings using information from other intervention and observational studies as implicit controls, we discussed our findings extensively in the context of what is known about the outcome of 'comparable' patients receiving other experimental treatments but not convalescent plasma therapy or hyperimmune immunoglobulin therapy. We did not meta‐analyse the data but provided information from individual studies within tables.
Unit of analysis issues
As we identified uncontrolled studies only, meta‐analysis was not appropriate. Instead, we narratively described and presented results per study in tables.
Please refer to Appendix 1 for information regarding how we had planned to combine studies with multiple treatment groups.
Dealing with missing data
Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions suggests a number of potential sources for missing data, which we will need to take into account: at study level, at outcome level and at summary data level (Higgins 2019b). In the first instance, it is of the utmost importance to differentiate between data 'missing at random' and 'not missing at random'.
We will request missing data from the study authors in an update of this review. If, after this, data are still missing, we will have to make explicit assumptions of any methods the included studies used. For example, we will assume that the data were missing at random or we will assume that missing values had a particular value, such as a poor outcome.
Assessment of heterogeneity
As we identified uncontrolled studies only, meta‐analysis was not appropriate. Instead, we narratively described and presented results per study in tables.
Please refer to Appendix 1 for information regarding how we had planned to assess heterogeneity.
Assessment of reporting biases
As mentioned above, we searched trials registries to identify completed studies that have not been published elsewhere, to minimise or determine publication bias.
In an update of this review, we intend to explore potential publication bias by generating a funnel plot and statistically testing this by conducting a linear regression test (Sterne 2019), for meta‐analyses involving at least 10 studies. We will consider P < 0.1 as significant for this test.
Data synthesis
Please refer to Appendix 1 for information regarding how we had planned to synthesise data from RCTs and NRSIs.
We did not meta‐analyse data from uncontrolled trials, as there might be no additional benefit in meta‐analysing data without a control group. We reported outcome data of each included trial within tables.
As data did not allow quantitative assessment, we presented outcome data individually per study within tables.
Subgroup analysis and investigation of heterogeneity
In an update of this review, we plan to perform subgroup analyses of the following characteristics.
Age of participants (divided into applicable age groups, e.g. children; 18 to 65 years, 65 years and older)
Severity of condition
Pre‐existing conditions (diabetes, respiratory disease, hypertension, immunosuppression)
We will use the tests for interaction to test for differences between subgroup results.
Sensitivity analysis
In an update of this review, we will perform only one sensitivity analysis for the following.
'Risk of bias' assessment components (low risk of bias versus high risk of bias)
To assess the influence of study quality on an outcome, we will perform sensitivity analyses per outcome, comparing studies with at least one domain of high risk of bias to those without high risk of bias.
Influence of completed, but not published studies
Influence of premature termination of studies
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of the evidence for the following outcomes (please find the rationale for the amendment of graded outcomes in the Differences between protocol and review).
All‐cause mortality at hospital discharge
Time to death
-
Clinical improvement (assessed by need for respiratory support) at the following time points
7 days post‐convalescent plasma transfusion
15 days post‐convalescent plasma transfusion
30 days post‐convalescent plasma transfusion
Grade 3 and 4 adverse events
Serious adverse events
We used GRADEpro GDT software to create an 'evidence profile'. We will also use the GRADEpro GDT software to create a 'Summary of findings' table, as suggested in the Cochrane Handbook for Systematic Reviews of Interventions when results of controlled trials are available (Schünemann 2019).
Results
Description of studies
Results of the search
We identified 1267 potentially relevant references. After removing duplicates, we screened 1039 references based on their titles and abstracts, and we excluded 956 references that were irrelevant because they did not meet the prespecified inclusion criteria. We evaluated the remaining 83 references and screened the full texts, or, if these were not available, abstract publications or trials registry entries. Of these, we classified two studies as awaiting classification for this review (Qiu 2020; Tu 2020).
We identified 56 potentially eligible studies within 57 citations: eight completed studies (Ahn 2020; Duan 2020; Pei 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), and 48 ongoing studies (ChiCTR2000029757; ChiCTR2000029850; ChiCTR2000030010; ChiCTR2000030039; ChiCTR2000030179; ChiCTR2000030627; ChiCTR2000030702; ChiCTR2000030841; ChiCTR2000030929; ChiCTR2000031501; EUCTR2020‐001310‐38; IRCT20151228025732N53; IRCT20200310046736N1; IRCT20200325046860N1; IRCT20200404046948N1; IRCT20200409047007N1; IRCT20200413047056N1; NCT04264858; NCT04292340; NCT04321421; NCT04327349; NCT04332380; NCT04332835; NCT04333251; NCT04333355; NCT04338360; NCT04340050; NCT04342182; NCT04343261; NCT04343755; NCT04344535; NCT04345289; NCT04345523; NCT04345679; NCT04345991; NCT04346446; NCT04346589; NCT04347681; NCT04348656; NCT04348877; NCT04352751; NCT04353206; NCT04354831; NCT04355767; NCT04355897; NCT04356482; NCT04356534; NCT04357106). See PRISMA flow diagram (Figure 1; Moher 2009).
1.
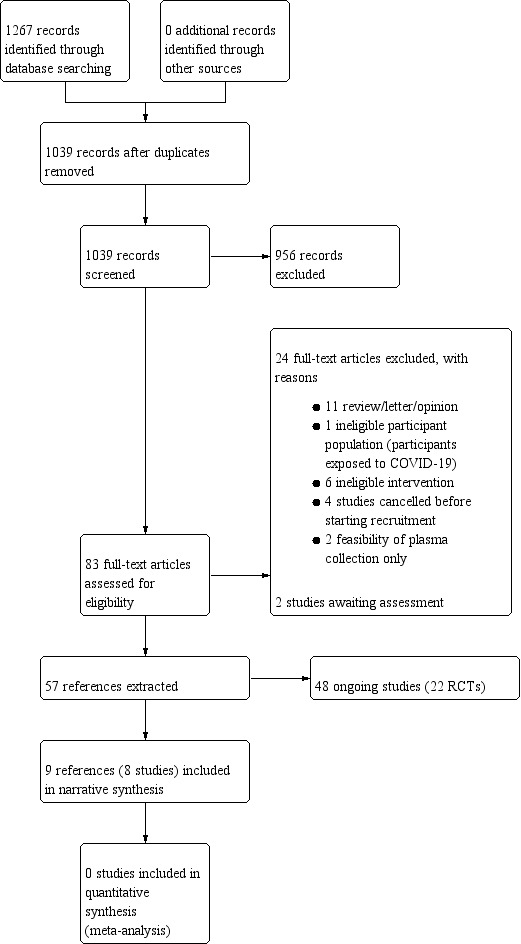
Study flow diagram
Included studies
We included eight studies describing 32 participants in this review (Ahn 2020; Duan 2020; Pei 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b). The eight included studies were all uncontrolled studies, seven studies were case series (Ahn 2020; Pei 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), and one was a prospectively registered single‐arm intervention study (Duan 2020). Of the eight included studies, seven originated from China (Duan 2020; Pei 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), and one from South Korea (Ahn 2020). In seven of the eight studies, convalescent plasma was transfused in critically ill individuals (Ahn 2020; Duan 2020; Pei 2020; Shen 2020; Ye 2020; Zhang 2020a; Zhang 2020b). One study described a person with moderate disease severity (Pei 2020), and one study described a hospitalised participant with moderate disease severity (Tan 2020).
The dose, volume and timing of convalescent plasma varied greatly between studies. The total volume of convalescent plasma transfused varied between 200 mL and 2400 mL, with participants receiving between one to eight doses of plasma. Antibody titres were reported in four studies (Duan 2020; Pei 2020; Shen 2020; Zhang 2020b). Characteristics of the donors of convalescent plasma also varied between studies, although reporting was not complete. Out of the eight studies, only six reported information on plasma donors (Ahn 2020; Duan 2020; Pei 2020; Shen 2020; Ye 2020; Zhang 2020b). Most donors were male, but Pei 2020 included a female donor with a previous history of pregnancy. The age of the donors varied: Ahn 2020 included donors in their twenties; Shen 2020 included donors aged between 18 and 60 years; Duan 2020 included donors with a median age of 42 years; and Zhang 2020b included donors aged between 30 and 50. Some studies provided information on previously reported symptoms and disease severity of convalescent plasma donors (Ahn 2020; Duan 2020; Zhang 2020b). Ahn 2020 reported that the two included donors had been admitted to hospital with fever, cough and pneumonia. Duan 2020 reported that donors had been admitted to hospital, but no other information on severity of illness was available. Zhang 2020b reported that all six donors had fever and cough during the course of disease and were admitted to the hospital. In the five studies that reported assessment of donor recovery, all donors were symptom‐free and completely recovered from coronavirus disease 2019 (COVID‐19) prior to donating plasma (Ahn 2020; Duan 2020; Shen 2020; Ye 2020; Zhang 2020b). Four studies required a negative severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) reverse transcription polymerase chain reaction (RT‐PCR) test prior to convalescent plasma donation (Duan 2020; Shen 2020; Ye 2020; Zhang 2020b), with three studies requiring two consecutive negative results as a requirement for donation (Duan 2020; Ye 2020; Zhang 2020b). Four studies used an enzyme‐linked immunosorbent assay (ELISA) to quantify neutralising antibodies (Duan 2020; Pei 2020; Shen 2020; Zhang 2020b), with limited information available on the type of ELISA that was used. One study additionally used a plaque reduction neutralisation assay to assess the neutralising activity of the plasma (Duan 2020).
We had also planned to include studies on hyperimmune immunoglobulin therapy in this rapid review. However we did not identify any eligible studies.
Please refer to the Characteristics of included studies for more detailed information.
Ongoing studies
Of the 48 ongoing studies, 22 are RCTs (ChiCTR2000029757; ChiCTR2000030010; ChiCTR2000030179; ChiCTR2000030627; ChiCTR2000030702; ChiCTR2000030929; EUCTR2020‐001310‐38; IRCT20200310046736N1; IRCT20200404046948N1; IRCT20200409047007N1; IRCT20200413047056N1; NCT04332835; NCT04333251; NCT04342182; NCT04344535; NCT04345289; NCT04345991; NCT04345523; NCT04355767; NCT04346446; NCT04348656; NCT04356534).
Of these, 16 are expected to be completed in 2020 (ChiCTR2000030010; ChiCTR2000030179; ChiCTR2000030627; ChiCTR2000030702; ChiCTR2000030929; IRCT20200310046736N1; IRCT20200404046948N1; IRCT20200409047007N1; IRCT20200413047056N1; NCT04332835; NCT04342182; NCT04345523; NCT04345991; NCT04346446; NCT04348656; NCT04356534), and plan to evaluate between 15 and 1200 participants.
Two further large RCTs are planned to be completed in 2021: NCT04344535, randomising 500 participants and NCT04345289, evaluating 1500 participants.
Please refer to Characteristics of ongoing studies for more detailed information.
Excluded studies
We excluded 24 studies that did not match our inclusion criteria:
11 were a review of the literature, a letter or an opinion (Bloch 2020; Casadevall 2020; Chen 2020; Jawhara 2020; Roback 2020; Syal 2020; Tanne 2020; Tiberghien 2020; Wong 2020; Yoo 2020; Zhao 2020b);
six studies were performed with an intervention other than convalescent plasma or hyperimmune immunoglobulin (Cao 2020; Díez 2020; Hu 2020; NCT04261426; Shi 2020; Xie 2020);
four studies were cancelled by the investigator before recruiting participants into the study (ChiCTR2000030312; ChiCTR2000030381; ChiCTR2000030442; NCT04325672);
two studies pertained to feasibility of collection of convalescent plasma only (NCT04344015; NCT04344977);
one study included the wrong participant population (participants exposed to COVID‐19; NCT04323800).
Risk of bias in included studies
Overall, we rated the risk of bias within and across studies to be serious. In addition to the high risk of bias due to the non‐randomised study design, we assessed the internal and external validity as outlined in the 'Risk of bias' assessment criteria for observational studies tool provided by the Cochrane Childhood Cancer Group (see Table 1; Mulder 2019). The full judgement per trial and category is presented in Figure 2 and the support for judgement in the Characteristics of included studies.
2.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study
Allocation
All studies were at high risk of selection bias. We considered study groups not to be representative, as all studies included low numbers of participants (1 to 10 participants) with no control groups.
Blinding
All studies were unblinded and therefore at high risk of performance and detection bias for subjective outcomes. All outcomes apart from all‐cause mortality are subjective to a greater or lesser extent and therefore at risk of bias.
Incomplete outcome data
We assessed attrition bias in terms of whether studies (equally) assessed outcomes for all participants. We evaluated attrition bias for three outcome categories.
Mortality
All studies assessed this outcome until discharge from hospital or the latest point of follow‐up. We judged the risk for attrition bias to be unclear for seven studies (Ahn 2020; Duan 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), because some participants were either still hospitalised or it was unclear whether participants had been discharged. Therefore the outcome for these participants is unknown.
We judged the risk for attrition bias to be low for one study (Pei 2020), as all participants had been free of disease and were discharged from the hospital.
Adverse events
We judged the risk of attrition bias to be low for four studies (Ahn 2020; Duan 2020; Ye 2020; Zhang 2020b), because they assessed and reported adverse events for all participants.
We judged the risk of attrition bias to be unclear for the other four studies (Pei 2020; Shen 2020; Tan 2020; Zhang 2020a), because it was unclear whether they had assessed adverse events for all participants or whether they had selectively reported outcomes. Pei 2020 reported one serious adverse event occurring in one participant, however did not report whether they had assessed or observed other adverse events. Shen 2020 did not provide any information regarding the safety of plasma transfusion. Tan 2020 reported that their participant experienced moderate fever after the transfusion, however did not report whether other adverse events occurred. Zhang 2020a described that they had observed no adverse events for one of their participants after plasma transfusion, but did not provide any information regarding the occurrence of adverse events for the other participants. They stated in the conclusions that they had not observed any serious adverse events.
Clinical improvements
We judged the risk of bias to be low for six studies (Ahn 2020; Duan 2020; Shen 2020; Ye 2020; Zhang 2020a; Zhang 2020b), because they assessed and reported clinical improvements for all participants.
We judged the risk of attrition bias to be high for one study (Tan 2020), because it was unclear why the participant was still hospitalised and they did not report clinical improvements.
Pei 2020 did not report the course of disease after convalescent plasma transfusion so we judged it at unclear risk of bias for this domain.
Selective reporting
We assessed reporting bias in terms of whether the study group and intervention were well‐defined and whether the outcomes were equally reported for all participants and the length of follow‐up was mentioned.
Well‐defined study group and intervention
We judged the risk of reporting bias to be low for four studies (Ahn 2020; Duan 2020; Shen 2020; Ye 2020), because both the study population and intervention were well described.
Zhang 2020a described the study population, but reported only limited information on the intervention. Zhang 2020b provided clear information on the intervention, but scarcely described the participant. We therefore judged the risk of reporting bias to be unclear for these two studies.
We judged the risk of bias to be high for two studies (Pei 2020; Tan 2020), which only reported limited information on the study population and the intervention. However, Pei 2020 was a preprint only, and claimed that the patient characteristics would be provided in the supplementary material once published.
Well‐defined outcomes
We evaluated reporting bias for three outcome categories.
Mortality
We judged the risk for reporting bias to be low for seven studies (Ahn 2020; Pei 2020; Shen 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), because all reported information for this outcome per participant until discharge from hospital or the latest point of follow‐up.
We judged the risk for reporting bias to be high for Duan 2020 because the follow‐up was unclear and it was unclear whether all participants were free of disease and discharged.
Adverse events
We judged the risk of reporting bias to be low for two studies (Ye 2020; Zhang 2020b), because observation period and results were reported for all participants.
We judged the risk of reporting bias to be high for the other six studies (Ahn 2020; Duan 2020; Pei 2020; Shen 2020; Tan 2020; Zhang 2020a), because it was unclear whether adverse events had not been (equally) assessed for all participants or whether outcomes were selectively reported. Pei 2020 reported one serious adverse event occurring in one participant, however did not report whether they had assessed or observed other adverse events. Shen 2020 did not provide any information regarding the safety of plasma transfusion. Tan 2020 reported that their participant experienced moderate fever after the transfusion, however did not report whether other adverse events occurred. Zhang 2020a described they had not observed any adverse events for one of their participants after plasma transfusion, but did not provide any information regarding the occurrence of adverse events for the other participants. They stated in the conclusions that they had not observed any serious adverse events.
Clinical improvements
Reporting of clinical improvements was very heterogeneous across studies.
We judged the risk of reporting bias to be low for three studies (Duan 2020; Ye 2020; Zhang 2020a), which clearly described clinical improvements and periods of follow‐up per participant.
We judged the risk of reporting bias to be unclear for three studies (Ahn 2020; Shen 2020; Zhang 2020b), because of the following reasons. Reporting and follow‐up was unclear for one participant of Ahn 2020, two participants of Shen 2020 probably were still on the intensive care unit (ICU) but it was unclear, and Zhang 2020b did not provide details but the participant was transferred to another ward.
We judged the risk of reporting bias to be high for Tan 2020 because neither clinical symptoms nor clinical improvement were reported in detail, but the participant was still in hospital.
Pei 2020 did not report the course of disease after convalescent plasma transfusion so we judged it at unclear risk of bias for this domain.
Other potential sources of bias
We further considered confounding and poorly‐defined risk estimates as potential sources of bias.
Confounding
All studies were at high risk of confounding because none of the studies adjusted for confounding factors, including concomitant treatments.
Poorly‐defined risk estimates
None of the studies performed any analyses.
Effects of interventions
In the 'Evidence profile' (Table 2), we present certainty of the evidence for the outcomes that were prioritised in the protocol (Piechotta 2020).
2. Certainty of evidence ratings for the effectiveness and safety of convalescent plasma therapy for people with COVID‐19.
|
Patients or population: people with COVID‐19 Settings: inpatient Intervention: convalescent plasma transfusion Comparison: not applicable; observational studies only | ||||||
| Outcome | Risk of bias | Indirectness | Imprecision | Inconsistency | Other considerations | Certainty of the evidence (GRADE) |
| All‐cause mortality at hospital discharge | Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
|
Improvement of clinical symptoms Assessed by respiratory support Follow‐up: 7 days |
Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
|
Improvement of clinical symptoms Assessed by respiratory support Follow‐up: 15 days |
Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
|
Improvement of clinical symptoms Assessed by respiratory support Follow‐up: 30 days |
Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
| Grade 3‐4 adverse eventse | Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
| Serious adverse events | Very seriousa | Direct | Very impreciseb | Inconsistentc | Study designd | ⊕⊝⊝⊝ Very low |
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aRisk of bias within and across studies is serious, so we downgraded two points for risk of bias. We included observational studies only, so we started assessment from 'low' certainty evidence. bWe downgraded two points for imprecision because of the very small information size and nonexisting control group; effect estimates cannot be calculated. cWe identified clinical heterogeneity among participants (different severity of disease, comorbidities, different number and type of previous treatments), so we downgraded one point for inconsistency. dWe included observational studies only, so we started assessment from low‐certainty evidence and did not summarise outcome data across studies. eWe assume these adverse events are grade 3‐4; studies did not report grading of adverse events.
Effectiveness of convalescent plasma for people with COVID‐19
As no RCTs or well conducted non‐randomised studies evaluating benefits and harms of convalescent plasma have yet been completed, we are not sure if the following results are related to convalescent plasma therapy; they could also be related to the underlying natural history of the disease or other concomitant treatments.
All‐cause mortality at hospital discharge
All‐cause mortality at hospital discharge cannot be fully evaluated, as not all of the participants had been discharged at the end of follow‐up. None of the studies reported any deaths during their study periods, meaning that all 32 participants were alive at the end of follow‐up. Participants were followed until discharge from hospital or from three (Duan 2020), to 37 days (Shen 2020), after transfusion. Two participants of Shen 2020 and one participant each of Ahn 2020, Ye 2020, Zhang 2020a, and Zhang 2020b were still hospitalised. The participant in Zhang 2020a still remained on the ICU. Further, it was unclear, whether all 11 participants of Duan 2020 and Tan 2020 had been discharged from hospital.
Time to death
All participants were alive at the end of follow‐up (3 to 37 days).
Improvement of clinical symptoms (assessed by need for respiratory support)
The effect of convalescent plasma on improvement of clinical symptoms was reported in six included studies (Ahn 2020; Duan 2020; Shen 2020; Ye 2020; Zhang 2020a; Zhang 2020b), including 24 participants on respiratory support at baseline, and four participants who did not require respiratory support. The results of these studies can be found in Table 3. We grouped them according to the prespecified time points; day 7, day 15, and day 30 after the plasma transfusion, and summarised baseline information and clinical status at the longest time of follow‐up for each study.
3. Improvement of clinical symptoms (assessed by need for respiratory support).
| Studya | Number of participants | Convalescent plasma given | ||||
| at baseline | at day 7 | at day 15 | up to day 30 | from baseline to longest follow‐up | ||
| Ahn 2020 | 2 |
|
|
|
|
Longest follow‐up: 16 and 18 days (2/2 participants with clinical improvement)
|
|
|
|
||||
| Duan 2020 | 10 |
|
|
|
|
Longest follow‐up: 3 days after transfusion (3/8 participants with clinical improvement)
|
| ||||||
| Shen 2020 | 5 |
|
|
|
|
Longest follow‐up: up to 37 days after first transfusion or until discharge (5/5 participants with clinical improvement)
|
|
|
|
||||
| Ye 2020 | 6 |
|
|
|
|
Longest follow‐up: up to 13 days after first transfusion or until discharge (4/4 participants with clinical improvement)
|
|
|
|||||
| Zhang 2020a | 4 |
|
|
|
|
Longest follow‐up: up to 36 days after first transfusion or until discharge (3/4 participants with clinical improvement, 1 unclear)
|
|
|
|
||||
| Zhang 2020b | 1 |
|
|
|
|
Longest follow‐up: 11 days after first transfusion until end of ICU stay (1/1 with clinical improvement)
|
|
|
|||||
| CP: convalescent plasma; ECMO: extracorporeal membrane oxygenation; NIV: non‐invasive ventilation; NR: not reported | ||||||
Six studies reported on improvement of clinical symptoms, but we could not extract all information about timing of improvement and types of respiratory support from all the studies.
Ahn 2020 described two critically ill people with COVID‐19 requiring intubation and mechanical ventilation. The two participants received a tracheotomy and one participant was reportedly successfully weaned from the ventilator by day 18 after convalescent plasma therapy. For the other participant, the date of cessation of respiratory support was not evident from the publication, but tracheotomy and weaning from mechanical ventilation were reported during the study period.
Duan 2020 reported decreased need for respiratory support in four out of 10 participants within three days of convalescent plasma transfusion. One other participant was reported to require only intermittent oxygenation after previously receiving continuous low‐flow oxygenation via nasal cannula. The study also reported on two individuals who required no respiratory support preceding convalescent plasma therapy. No information on improvement of clinical symptoms for other time points was available.
Shen 2020 reported a case series that included five participants who were described as critically ill at baseline, with four participants in need of mechanical ventilation and intubation and one participant receiving extracorporeal membrane oxygenation (ECMO). Of these five participants, three were discharged from hospital at the end of the study period, and two were in a stable condition, intubated and receiving mechanical ventilation.
Ye 2020 included six participants, four of whom required oxygen at baseline (one via nasal cannula, with the other modes not specified in the publication). Two individuals did not require respiratory support before convalescent plasma was administered. All four participants previously requiring respiratory support experienced alleviation of symptoms after convalescent plasma therapy, with none of them requiring respiratory support at the end of the study follow‐up. The study reports information on respiratory support but lacks information on the type of support received by the participants, and the timing of this outcome is not part of the presented data for all participants.
Zhang 2020a reported in detail the clinical characteristics and timing of convalescent plasma therapy for four people with COVID‐19. One participant was on non‐invasive ventilation (NIV) and high‐flow oxygenation, one participant was mechanically ventilated and intubated at baseline, and two participants received ECMO. Three out of the four participants were discharged at the end of the study period, and all participants were reported to have recovered from the infection eventually. For one participant it was unclear whether oxygen support was still required by the end of the study period.
Zhang 2020b described one participant who was mechanically ventilated and intubated before receiving convalescent plasma therapy. At day 11 after convalescent plasma therapy, the participant was removed from mechanical ventilation. Whether the participant required other types of respiratory support was not reported.
30‐day and 90‐day mortality
All participants were alive at the end of follow‐up. Participants were followed until discharge from hospital or three (Duan 2020), to 37 days (Shen 2020), after transfusion.
Time to discharge from hospital
The time to discharge was reported for at least some of the participants in six studies (Ahn 2020; Pei 2020; Shen 2020; Ye 2020; Zhang 2020a; Zhang 2020b). The day of discharge after convalescent plasma therapy ranged from 4 days to 35 days. Only one study (3 participants) reported time to discharge from hospital for all participants (Pei 2020). Please refer to Table 4 for further information regarding each trial and participant.
4. Hospital discharge.
| Study | Number of participants | Number of participants discharged at end of follow‐up | Day of discharge (after convalescent plasma) |
| Ahn 2020 | 2 | 1 | Day 18 |
| Duan 2020 | 10 | Not reported | Not reported |
| Pei 2020 | 3 | 3 | Day 6 Day 14 Day 23 |
| Shen 2020 | 5 | 3 | Day 32 Day 33 Day 35 |
| Tan 2020 | 1 | 0 | Not applicable |
| Ye 2020 | 6 | 5 1 unclear | Day 4 Day 6 Day 6 Day 10 1 unclear |
| Zhang 2020a | 4 | 3 | Day 7 Day 25 Day 27 |
| Zhang 2020b | 1 | 0 | Not applicable |
It was unclear, whether all participants of Duan 2020 and Tan 2020 had been discharged from the hospital.
Admission on the ICU
This outcome was not reported in a consistent way in the included studies. Ye 2020, Zhang 2020a and Zhang 2020b reported the number of participants on the ICU at baseline (Table 5). These were none of six (Ye 2020), four of four (Zhang 2020a), and one of one (Zhang 2020b), respectively. The other studies did not report the number of participants on the ICU at baseline, however Ahn 2020, Duan 2020, Pei 2020, and Shen 2020 reported the number of participants that were mechanically ventilated, and so presumably on the ICU (please see Table 5). The participant reported in Tan 2020 presented with moderate symptoms only, and so presumably was not on the ICU.
5. Intensive care unit (ICU) stay after convalescent plasma.
| Study | Number of participants | Baseline: number of participants on ICU | End of follow‐up: number of participants on ICU |
| Ahn 2020 | 2 | NR (probably 2) | NR (probably 1; 1 discharged) |
| Duan 2020 | 10 | NR (probably 3) | NR (probably 1) |
| Pei 2020 | 3 | NR (probably 2) | 0; all discharged |
| Shen 2020 | 5 | NR (probably 5) | NR (probably 2, 3 discharged) |
| Tan 2020 | 1 | NR (probably 0) | NR (probably 0) |
| Ye 2020 | 6 | 0 | 0; 5 discharged |
| Zhang 2020a | 4 | 4 | 1; 3 discharged |
| Zhang 2020b | 1 | 1 | 0 |
| ICU: intensive care unit; NR: not reported | |||
Length of stay on the ICU
We could not evaluate the length of stay on the ICU as none of the included studies reported this outcome in a consistent way. Zhang 2020a reported that one participant was still on the ICU at the end of follow‐up, the other three participants had been discharged from the ICU. Zhang 2020b reported that their participant could be released from the ICU 11 days after plasma transfusion to a general ward; 18 days after admission on the ICU. Based on the reported clinical course of disease presumably one participant of Ahn 2020 and two participants of Shen 2020 were also still on the ICU at the end of follow‐up (please see Table 5). However, this was not clearly reported.
Safety of convalescent plasma for people with COVID‐19
Number of participants with adverse events of possibly grade 3 or grade 4 severity
Seven studies reported assessment of adverse events (Ahn 2020; Duan 2020; Pei 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b), however, Zhang 2020a only reported for one of their participants that no adverse event had been observed. It was unclear whether the other three participants did or did not experience any adverse events.
Six studies therefore reported the presence or absence of adverse events for all participants. Two studies reported adverse events that were possibly grade 3 or 4 severity but they did not report the degree of severity (see Table 6). Tan 2020, a case study, reported that their participant experienced moderate fever (38.9 °C) after convalescent plasma transfusion. One of the three participants in Pei 2020 had severe anaphylactic shock after receiving 30 mL of plasma from a female donor with a history of pregnancy. Four other studies reported no adverse events that were possibly of grade 3 or grade 4 severity (19 participants; Ahn 2020; Duan 2020; Ye 2020; Zhang 2020b).
6. Adverse events: grade 3 or 4.
| Study | Number of participants | Grade 3 or 4 adverse eventsa |
| Ahn 2020 | 2 | 0 |
| Duan 2020b | 10 | 0 |
| Pei 2020 | 3 | 1 (anaphylactic shock) |
| Shen 2020c | 5 | Not reported |
| Tan 2020 | 1 | 1 (fever) |
| Ye 2020 | 6 | 0 |
| Zhang 2020ad | 4 | 0 |
| Zhang 2020b | 1 | 0 |
aWe assume that these adverse events were grade 3 or 4, but the studies did not specify the degree of severity. bOne participant with evanescent red face (grade unclear). cShen 2020 did not report whether they assessed or observed adverse events. dAssessment of adverse events only reported for one individual. Unclear information provided for the other three participants.
Number of participants with serious adverse events
Seven studies assessed and reported serious adverse events (Ahn 2020; Duan 2020; Pei 2020; Tan 2020; Ye 2020; Zhang 2020a; Zhang 2020b). One participant in Pei 2020 (3 participants) experienced a serious adverse event (see Table 7). As described above, this individual had severe anaphylactic shock after receiving convalescent plasma from a female donor with a history of pregnancy. No serious adverse events occurred in six studies (24 participants).
7. Serious adverse events.
| Study | Number of participants | Serious adverse events |
| Ahn 2020 | 2 | 0 |
| Duan 2020 | 10 | 0 |
| Pei 2020 | 3 | 1 (anaphylactic shock) |
| Shen 2020a | 5 | Not reported |
| Tan 2020 | 1 | 0 |
| Ye 2020 | 6 | 0 |
| Zhang 2020a | 4 | 0 |
| Zhang 2020b | 1 | 0 |
aShen 2020 did not report whether they assessed or observed serious adverse events.
Discussion
Summary of main results
The aim of this review was to assess the effectiveness and safety of convalescent plasma and hyperimmune immunoglobulin in the treatment of coronavirus disease 2019 (COVID‐19) illness.
We included eight studies in this review ‐ seven case‐series and one prospectively planned, single‐arm intervention study, all evaluating convalescent plasma (32 participants in total). There were no completed studies evaluating hyperimmune immunoglobulin. We identified 47 ongoing studies evaluating convalescent plasma and one ongoing study evaluating hyperimmune immunoglobulin. Twenty‐two of the ongoing studies on convalescent plasma are randomised.
Effectiveness of convalescent plasma for people with COVID‐19
As no RCTs or high‐quality, non‐randomised studies evaluating benefits and harms of convalescent plasma are completed yet, we do not know whether the following results are related to the underlying natural history of the disease, other concomitant treatment, or convalescent plasma.
All‐cause mortality at hospital discharge
All studies reported mortality, and all participants were alive at the end of reporting, but not all of the participants had been discharged from hospital at the end of follow‐up. We do not know whether convalescent plasma has any effect on all‐cause mortality (very low‐certainty evidence).
Improvement of clinical symptoms (as assessed by respiratory support)
Six studies reported on the level of respiratory support required in participants; most participants required respiratory support at baseline. All studies reported improvement in clinical symptoms in at least some of their participants. We do not know whether convalescent plasma improves clinical symptoms or whether this improvement was due to other interventions, or the natural history of the disease (very low‐certainty evidence).
Time to discharge from the hospital
Six studies reported time to discharge from hospital for at least some of their participants. The day of discharge after convalescent plasma therapy ranged from 4 to 35 days.
Admission on the intensive care unit (ICU)
Six studies included participants who were critically ill. The majority of these participants were no longer on the ICU or no longer required mechanical ventilation at final follow‐up.
Length of stay on the ICU
None of the studies clearly reported this outcome.
Safety of convalescent plasma for people with COVID‐19
Adverse events
Two studies reported participants who had experienced adverse events, presumably of grade 3 or 4 (they did not report degree of severity). One case study reported a participant who had moderate fever (38.9 °C) after the transfusion of convalescent plasma. The other study (3 participants) reported a case of severe anaphylactic shock after convalescent plasma transfusion. Four studies reported that no participants experienced moderate or severe adverse events (19 participants). We are very uncertain whether convalescent plasma therapy affects the risk of moderate to severe adverse events (very low‐certainty evidence).
Serious adverse events
One study with three participants reported one serious adverse event. This participant had severe anaphylactic shock after receiving convalescent plasma. Six studies reported that no serious adverse events occurred. We are very uncertain whether convalescent plasma therapy affects the risk of serious adverse events (very low‐certainty evidence).
Overall completeness and applicability of evidence
We found eight published non‐randomised, uncontrolled studies (seven case‐series, one prospectively planned study) evaluating convalescent plasma in adults, most with severe COVID‐19. These studies included 32 participants (ranging from 1 to 10 participants). Most of these participants had already received different treatment options either solely or in combination. These included antivirals, antifungals or antibiotics, corticosteroids, hydroxychloroquine and respiratory support (extracorporeal membrane oxygenation (ECMO), mechanical ventilation or oxygen). Therefore, the participant population might have been too small and heterogeneous to generalise results.
We identified 48 ongoing studies, of which 22 are designed as RCTs. Of these ongoing studies, 47 evaluate convalescent plasma and one evaluates hyperimmune immunoglobulin. Sixteen RCTs are planned to be completed in 2020. The publication of the results of these studies will necessitate an update of this review. The conclusions of the updated review could differ from those of the present review, and may allow for a better judgement regarding the effectiveness and safety of convalescent plasma therapy.
Certainty of the evidence
It is important to note that the outcome measures are heterogeneous with wide variation in reporting across the included studies. Only one study was prospectively planned (Duan 2020), a non‐randomised and uncontrolled study, evaluating 10 participants. However, this study reported a very short follow‐up only (three days after convalescent plasma was given). The other seven small case‐series studies were not registered. These study designs lead to high risk of bias, both in terms of selection and detection bias. Studies were not adjusted for potential confounders (e.g. severity of disease, comorbidities, previous or concomitant COVID‐19 treatment). Currently, there is no standard instrument available to assess risk of bias for this type of study. We used the form developed by the Cochrane Childhood Cancer Group (Table 1; Mulder 2019).
As we included eight small observational studies only (32 participants altogether), the results are very imprecise and very inconsistent, with very high risk of bias. Therefore, the certainty of the evidence is very low for all prioritised outcomes.
Potential biases in the review process
To avoid potential bias in the review, we had planned to include the best available evidence. However, as COVID‐19 is a novel disease, results from RCTs and non‐RCTs are not yet available. In fact, we could only identify uncontrolled studies, reporting on a small number of participants. To increase the informative value of our review, we are tracking all registered trials and will update this review on a monthly basis as more evidence becomes available.
Two experienced Information Specialists developed a sensitive search strategy, to identify all ongoing and completed studies. We searched all relevant databases and trials registries, and in contrast to the recommendations of the Cochrane Rapid Reviews Methods Group, we decided to conduct all review steps regarding the study selection in duplicate by two independent review authors. We are confident that we identified all relevant published and ongoing studies and will monitor them closely in the future.
Unlike standard Cochrane methodology, only one review author performed data extraction and 'Risk of bias' and GRADE assessments for this rapid review. To minimise bias in these steps, at least one other review author verified the accuracy and (where applicable) the plausibility of extractions and assessment.
Although we have very limited confidence in the available evidence, we are not aware of any deficiencies in our review process. However, we are certain that the results are likely to be substantially different and conclusions may change as soon as high‐certainty evidence becomes available.
Agreements and disagreements with other studies or reviews
This systematic review identified very low‐certainty evidence on the safety and effectiveness of convalescent plasma for people with COVID‐19.
A recent systematic review and meta‐analysis found low‐certainty evidence for the use of convalescent plasma for treating people with infections with different aetiologies (Mair‐Jenkins 2015). The authors reported a systematic review and meta‐analysis of the literature on the use of convalescent plasma and hyperimmune immunoglobulin in treating severe acute respiratory infections of viral aetiology, and found that this treatment is likely to be both safe and effective in preventing mortality. The study identified a 75% reduction in the odds of mortality in their exploratory post hoc meta‐analysis across all viral aetiologies. The studies included in this review were performed with people treated with convalescent plasma for severe acute respiratory syndrome (SARS) and influenza. The limited number of identified studies and the low quality of included, mainly uncontrolled studies restricted the authors’ ability to analyse extensively the risks and benefits of convalescent plasma therapy. Recommendations from the authors were to investigate the use of convalescent plasma and hyperimmune immunoglobulin in large, well‐designed clinical trials or other formal evaluations to obtain better‐certainty evidence, and to evaluate the optimal treatment regimen.
Results from several large RCTs on the use of convalescent plasma and hyperimmune immunoglobulin in treating severe influenza have recently been made public (Beigel 2017; Beigel 2019; Davey 2019; Hung 2013). However, the results from these studies are inconsistent, with some studies showing a beneficial effect of convalescent plasma for treating people with severe influenza, whereas other studies show no benefit. The studies were well designed and reported in detail the timing of the intervention and relevant outcomes. One trial reported effectiveness of hyperimmune immunoglobulin, but only in a post hoc analysis of a subgroup of participants treated within five days of symptom onset (Hung 2013). In a different trial, for the subgroup analysis of people with influenza B, the effect of hyperimmune immunoglobulin also resulted in a demonstrable clinical and virological benefit (Davey 2019). Different mechanisms in the human immune system and their role in responding to different circulating influenza strains might further explain why the results of clinical trials of convalescent plasma and hyperimmune immunoglobulin for influenza varied (Davey 2019). Influenza A immunity is reported to carry over to the next years, known as heterosubtypic immunity (Kreijtz 2011), and the current outbreak of COVID‐19 can, in that sense, not be compared with seasonal influenza. Notwithstanding these dissimilarities which might explain why the aforementioned influenza studies were not successful in clearly demonstrating benefit, the possibility of a null effect of convalescent plasma over a suitable comparator cannot be ruled out with the currently available evidence on COVID‐19.
The adverse events associated with plasma transfusions are well characterised. Critically ill patients receiving plasma transfusions have an especially high risk of transfusion‐associated circulatory overload (TACO), which is the leading cause of transfusion‐related mortality (Pandey 2012). Many countries have now introduced risk mitigation strategies to decrease the risk of transfusion‐related acute lung injury (TRALI). In the UK in 2018 there was only one confirmed case of TRALI.
In this systematic review of the literature, which mainly identified studies that included people with COVID‐19 with critical illness, we identified one potentially grade 3 adverse event and one potentially grade 4 adverse event (which also qualified as a serious adverse event). With the information available at this moment from published trials registry entries, it is apparent that the majority of clinical trials are enrolling people with COVID‐19 who have progressed to moderate or severe disease. Despite there being some evidence from other infectious diseases that early therapy might be more effective (Mair‐Jenkins 2015), targeting this population is justifiable given the evident lack of effective interventions for COVID‐19. The population that is eligible for treatment in these trials with convalescent plasma is potentially at high risk of transfusion reactions, and when treating critically ill people with COVID‐19, their status should be carefully monitored.
Authors' conclusions
Implications for practice.
The currently available evidence on the safety and effectiveness of convalescent plasma and hyperimmune immunoglobulin for treatment of people with COVID‐19 is of very low certainty. Thus, any conclusions that are drawn based on these data are of limited value and these conclusions are subject to change as more reliable results become available. For the primary outcomes, the included studies reported that all participants were alive at the end of follow‐up. Clinical improvement assessed through the need for respiratory support was reported by most studies, but details on timing and type of respiratory support were not clear for all studies. Other outcomes that were reported in a subset of the included studies were length of stay on the intensive care unit (ICU) and time to discharge from hospital, but reporting of these outcomes was not complete. Two studies reported adverse events that were potentially grade 3 and grade 4, of which one was a serious adverse event. More thorough investigations, preferably well‐designed clinical trials, are needed in order to assess the benefits and risks of convalescent plasma therapy for people with COVID‐19.
Implications for research.
In this systematic review of the literature, we identified seven case‐series studies and one prospectively planned, single‐arm intervention study. We encountered difficulties while extracting data from these studies because there were major differences in the way these studies reported participant characteristics, details on the intervention, and outcomes. Future publications could benefit from more standardised reporting, especially of timing of intervention and clinically relevant outcomes, like days until discharge from hospital and improvement of clinical symptoms. We support the adoption of a reporting guideline in this rapidly evolving field of research.
Randomised controlled trials (RCTs) or at least non‐randomised trials with a control group are needed to confirm the findings of this review. As there are 47 ongoing studies evaluating convalescent plasma and one ongoing study evaluating hyperimmune immunoglobulin, of which 22 are randomised, we will screen search results monthly and publish updates as a living systematic review in the near future. It might well be that this update will show different results than those published in this rapid review.
History
Review first published: Issue 5, 2020
Acknowledgements
This review was published in collaboration with the Cochrane Editorial and Methods Department. We particularly thank Sarah Hodgkinson (Associate Editor, Editorial and Methods Dept), Analysis of Review Group Output (ARGO) for their comments on the Abstract, Clare Dooley (Managing Editor), and Denise Mitchell (Copy Editor) for their excellent support. Thanks also to the Cochrane Editorial and Methods Department team, for their valuable comments on the review and timely management of the editorial process.
We thank Robin Featherstone (Information Specialist, Editorial and Methods Department) for commenting on the search strategy and Gerald Gartlehner and Adrienne Stevens for their advice on rapid review methodology. We thank Susan J Brunskill for her support in identifying included and ongoing studies.
We thank all external peer reviewers who read and commented on this review. We thank Miquel Lozano (MD, PhD Clinic University Hospital, University of Barcelona, Spain), and Michael James Ankcorn (Virology Department, Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, UK), who greatly helped to improve this review.
Appendices
Appendix 1. Planned methodology for randomised controlled trials (RCTs) and non‐randomised studies of interventions (NRSIs)
Types of studies
To assess the benefits and safety of convalescent plasma for the therapy of COVID‐19 we had planned to include randomised controlled trials (RCTs) only, as such studies, if performed appropriately, currently give the best evidence for experimental therapies in highly controlled therapeutic settings. If RCT data had been available, we would have used the methods recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019a), as specified in the description of the methods.
In case of insufficient evidence (very low‐certainty evidence or no evidence) available from RCTs to answer this review's questions we had planned to include prospective controlled non‐randomised studies of interventions (NRSIs), including quasi‐randomised controlled trials (e.g. assignment to treatment by alternation or by date of birth), controlled before‐and‐after (CBA) studies, and interrupted time series (ITS) studies. In that case, we would have used the methods proposed in the Cochrane Handbook for Systematic Reviews of Interventions for the inclusion of NRSIs in systematic reviews (Reeves 2019).
In case of insufficient evidence (very low‐certainty evidence or no evidence) available from RCTs and NRSIs we had planned to include prospective observational studies with a control group and would have adapted the methods for the inclusion of NRSIs in systematic reviews as specified by the Cochrane Handbook for Systematic Reviews of Interventions as well (Reeves 2019).
As there was no evidence from RCTs, NRSIs, and only one prospective observational study available, we included prospective non‐comparative study designs (e.g. case series) and followed the methodology as specified in the protocol (Piechotta 2020).
Data extraction and management
Assessment of risk of bias in included studies
Randomised controlled trials
We had planned to use the Risk of Bias 2.0 (RoB 2) tool to analyse the risk of bias in the underlying study results (Sterne 2019). Of interest for this review was the effect of the assignment to the intervention (the intention‐to‐treat (ITT) effect) and we would have performed all assessments with RoB 2 on this effect. The outcomes that we would have addressed are those specified for inclusion in the 'Evidence profile' (Table 2). Accordingly, the outcomes had been prioritised according to the Core Outcome Measures in Effectiveness Trials Initiative for Covid‐19 patients (COMET 2020).
One review author would have assessed the risk of bias for each study result. A second review author would have verified the accuracy and the plausibility. In case of discrepancies among their judgements or inability to reach consensus, we had planned to consult a third review author to reach a final decision. We would have assessed the following types of bias as outlined in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019a).
Bias arising from the randomisation process
Bias due to deviations from the intended interventions
Bias due to missing outcome data
Bias in measurement of the outcome
Bias in selection of the reported result
To address these types of bias we had planned to use the signalling questions recommended in RoB 2 and make a judgement using the following options:
'yes': if there is firm evidence that the question is fulfilled in the study (i.e. the study is at low or high risk of bias for the given the direction of the question);
'probably yes': a judgement has been made that the question is fulfilled in the study (i.e. the study is at low or high risk of bias given the direction of the question);
'no': if there is firm evidence that the question is unfilled in the study (i.e. the study is at low or high risk of bias for the given the direction of the question);
'probably no': a judgement has been made that the question is unfilled in the study (i.e. the study is at low or high risk of bias given the direction of the question);
'no information' if the study report does not provide sufficient information to allow any judgement.
We had planned to use the algorithms proposed by RoB 2 to assign each domain one of the following levels of bias:
low risk of bias;
some concerns;
high risk of bias.
Subsequently we had planned to derive a 'Risk of bias' rating for each prespecified outcome in each study in accordance with the following suggestions.
'Low risk of bias': the trial is judged to be at low risk of bias for all domains for this result.
'Some concerns': the trial is judged to raise some concerns in at least one domain for this result, but not to be at high risk of bias for any domain.
'High risk of bias': the trial is judged to be at high risk of bias in at least one domain for the result or the trial is judged to have some concerns for multiple domains in a way that substantially lowers confidence in the results.
Non‐randomised controlled studies
As reported above, we had planned to include non‐randomised studies if there were insufficient evidence from RCTs.
One review author would have assessed eligible studies for methodological quality and risk of bias (using the Risk Of Bias in Non‐randomised Studies ‐ of Interventions (ROBINS‐I) tool; Sterne 2016). A second review author would have verified the accuracy and the plausibility. The quality assessment strongly depends upon information on the design, conduct and analysis of the trial. The two review authors would have resolved any disagreements regarding the quality assessments by consulting a third review author until they reached a consensus.
We had planned to assess the following domains of bias.
Bias due to confounding
Bias in selection of participants into the study
Bias in classification of interventions
Bias due to deviations from intended interventions
Bias due to missing data
Bias in measurement of outcomes
Bias in selection of the reported result
For every criterion we had planned to make a judgement using one of five response options.
Yes
Probably yes
Probably no
No
No information
Measures of treatment effect
Randomised controlled trials
For continuous outcomes, we had planned to record the mean, standard deviation and total number of participants in both the treatment and control groups. For dichotomous outcomes, we had planned to record the number of events and total number of participants in both the treatment and control groups.
For continuous outcomes using the same scale we had planned to perform analyses using the mean difference (MD) with 95% confidence intervals (CIs). For continuous outcomes measured with different scales we had planned to perform analyses using the standardised mean difference (SMD). For interpreting SMDs, we had planned to re‐express it in the original units of a particular scale with the most clinical relevance and impact.
If available, we had planned to extract and report hazard ratios (HRs) for time‐to‐event outcomes (overall survival, progression‐free survival). If HRs had not been available, we had planned to make every effort to estimate as accurately as possible the HR using the available data and a purpose‐built method based on the Parmar and Tierney approach (Parmar 1998; Tierney 2007), in an update of this review. If sufficient studies had provided HRs, we had planned to use HRs rather than RRs or MDs in a meta‐analysis.
For dichotomous outcomes, we had planned to report the pooled risk ratio (RR) with a 95% CI (Deeks 2019). If the number of observed events had been small (less than 5% of sample per group), and if studies had balanced treatment groups, we had planned to report the Peto odds ratio (OR) with 95% CI (Deeks 2019).
For cluster‐randomised trials, we had planned to extract and report direct estimates of the effect measure (e.g. RR with a 95% CI) from an analysis that accounts for the clustered design. We had planned to obtain statistical advice to ensure the analysis was appropriate. If appropriate analyses had not been available, we would have made every effort to approximate the analysis following the recommendations in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019b), in an update of this review.
Non‐randomised controlled studies
For dichotomous outcomes, if available we had planned to extract and report the RR with a 95% CI from statistical analyses adjusting for baseline differences (such as Poisson regressions or logistic regressions) or the ratio of RRs (i.e. the RR post‐intervention/RR pre‐intervention).
For continuous variables, if available, we had planned to extract and report the absolute change from a statistical analysis adjusting for baseline differences (such as regression models, mixed models or hierarchical models), or the relative change adjusted for baseline differences in the outcome measures (i.e. the absolute post‐intervention difference between the intervention and control groups, as well as the absolute pre‐intervention difference between the intervention and control groups/the post‐intervention level in the control group; EPOC 2017).
Unit of analysis issues
Studies with multiple treatment groups
As recommended in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019b), for studies with multiple treatment groups we had planned to combine arms as long as they could be regarded as subtypes of the same intervention.
When arms could not be pooled this way, we would have compared each arm with the common comparator separately. For pair‐wise meta‐analysis, we would have split the ‘shared’ group into two or more groups with smaller sample size, and included two or more (reasonably independent) comparisons. For this purpose, for dichotomous outcomes, both the number of events and the total number of participants would have been divided up, and for continuous outcomes, the total number of participants would have been divided up with unchanged means and SDs.
Assessment of heterogeneity
We had planned to assess heterogeneity of treatment effects between studies using a Chi2 test with a significance level at P < 0.1. We had planned to use the I2 statistic (Higgins 2003), to quantify possible heterogeneity (I2 statistic > 30% to signify moderate heterogeneity, I2 statistic > 75% to signify considerable heterogeneity; Deeks 2019). If heterogeneity were above 80%, we had planned to explore potential causes through sensitivity and subgroup analyses. If we could not find a reason for heterogeneity, we would not have performed a meta‐analysis, but had planned to comment on results from all studies and present these in tables.
Data synthesis
If the clinical and methodological characteristics of individual studies were sufficiently homogeneous, we had planned to pool the data in meta‐analysis. We had planned to perform analyses according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2019). We would not have conducted meta‐analyses that involved both RCTs and non‐RCTs. We had planned to conduct separate meta‐analyses for each comparison.
We had planned to use the Review Manager Web software for analyses (Review Manager Web). One review author would have entered the data into the software, and a second review author would have checked the data for accuracy.
We had planned to use the random‐effects model for all analyses as we anticipate that true effects will be related but will not be the same for included studies. If we could not perform a meta‐analysis, we had planned to comment on the results as a narrative with the results from all studies presented in tables.
For RCTs, when meta‐analysis had been feasible, we had planned to use the random‐effects model for pooling the data. For binary outcomes, we had planned to base the estimation of the between‐study variance using the Mantel‐Haenszel method. We had planned to use the inverse variance method for continuous outcomes, outcomes that include data from cluster‐RCTs, or outcomes where HRs are available. We planned to explore heterogeneity above 80% with subgroup analyses. If we could not find a cause for the heterogeneity then we had planned not to perform a meta‐analysis, but comment on the results as a narrative with the results from all studies presented in tables.
If a meta‐analysis had been feasible for non‐RCTs, CBA studies, ITS studies, and cohort studies, we had planned to analyse the different types of studies separately. We had planned to only analyse outcomes with adjusted effect estimates if these were adjusted for the same factors using the inverse‐variance method as recommended in Chapter 24 of the Cochrane Handbook for Systematic Reviews of Interventions (Reeves 2019).
Appendix 2. Search strategy WHO COVID‐19 Database
plasma OR hyperimmune OR hyper‐immune OR IVIG OR immunoglobulin OR globulin OR immune‐globulin OR gamma‐globulin OR γ‐Globulin OR hyper‐Ig OR immunoglobulins OR globulins OR donor OR donation OR donors OR donating OR donations OR donated
Appendix 3. Search strategy MEDLINE
1. Coronavirus Infections/
2. Coronavirus/
3. "Betacoronavirus"/
4. ((corona* or corono*) adj1 (virus* or viral* or virinae*)).tw,kf.
5. (coronavirus* or coronovirus* or coronavirinae* or "2019‐nCoV" or 2019nCoV or 2019‐CoV or nCoV2019 or "nCoV‐2019" or "COVID‐19" or COVID19 or "CORVID‐19" or CORVID19 or "WN‐CoV" or WNCoV or "HCoV‐19" or HCoV19 or CoV or "2019 novel*" or Ncov or "n‐cov" or "SARS‐CoV‐2" or "SARSCoV‐2" or "SARSCoV2" or "SARS‐CoV2" or SARSCov19 or "SARS‐Cov19" or "SARSCov‐19" or "SARS‐Cov‐19" or SARSr‐cov or Ncovor or Ncorona* or Ncorono* or NcovWuhan* or NcovHubei* or NcovChina* or NcovChinese*).tw,kf.
6. (((respiratory* adj2 (acute* or symptom* or disease* or illness* or condition*)) or "seafood market*" or "food market*") adj10 (Wuhan* or Hubei* or China* or Chinese* or Huanan*)).tw,kf.
7. ((outbreak* or wildlife* or pandemic* or epidemic*) adj3 (Wuhan* or Hubei* or China* or Chinese* or Huanan*)).tw,kf.
8. (anti‐flu* or anti‐influenza* or antiflu* or antinfluenza*).tw,kf.
9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
10. Plasma/
11. Immunoglobulins/
12. Immunoglobulins, Intravenous/
13. Immune Sera/
14. ((convalesc* or recovered or cured or rehabilitat* or survivor* or survived or virus‐positive or virus neutrali* or virus inactivated or antibod* or high‐titre* or high‐titer*) adj6 (plasma or blood or serum or sera)).mp.
15. ((plasma adj1 therap*) or gamma‐globulin* or "γ‐Globulin" or hyper‐Ig).tw,kf.
16. ((hyperimmune or hyper‐immune or high‐dos*) adj3 (plasma or immunoglobulin* or IVIG* or immune globulin* or globulin* or IgG)).tw,kf.
17. (plasma adj5 (immun* or antibod* or exchange* or donor* or donat* or transfus* or infus*)).mp.
18. ((convalesc* or recovered or cured or rehabilitat* or survivor* or survived or virus‐positive or virus inactivated or antibody‐positive) adj5 (donor* or donat*)).mp.
19. 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
20. 9 and 19
21. (Flu‐IVIG or ((anti‐flu* or anti‐influenza* or antiflu* or antinfluenza*) adj5 plasma)).mp.
22. 20 or 21
23. (exp Animals/ or exp Animal Experimentation/ or exp Models, Animal/) not Humans/
24. 22 not 23
25. limit 24 to yr="2019 ‐Current"
Appendix 4. Search strategy Embase
1. Sars‐related Coronavirus/
2. "Coronavirus Infections"/ or "Coronavirus Infection"/
3. Coronavirinae/
4. Coronavirus/
5. ((corona* or corono*) adj1 (virus* or viral* or virinae*)).tw,kw.
6. (coronavirus* or coronovirus* or coronavirinae* or "2019‐nCoV" or 2019nCoV or 2019‐CoV or nCoV2019 or "nCoV‐2019" or "COVID‐19" or COVID19 or "CORVID‐19" or CORVID19 or "WN‐CoV" or WNCoV or "HCoV‐19" or HCoV19 or CoV or "2019 novel*" or Ncov or "n‐cov" or "SARS‐CoV‐2" or "SARSCoV‐2" or "SARSCoV2" or "SARS‐CoV2" or SARSCov19 or "SARS‐Cov19" or "SARSCov‐19" or "SARS‐Cov‐19" or SARSr‐cov or Ncovor or Ncorona* or Ncorono* or NcovWuhan* or NcovHubei* or NcovChina* or NcovChinese*).tw,kw.
7. (((respiratory* adj2 (acute* or symptom* or disease* or illness* or condition*)) or "seafood market*" or "food market*") adj10 (Wuhan* or Hubei* or China* or Chinese* or Huanan*)).tw,kw.
8. ((outbreak* or wildlife* or pandemic* or epidemic*) adj3 (Wuhan* or Hubei* or China* or Chinese* or Huanan*)).tw,kw.
9. (anti‐flu* or anti‐influenza* or antiflu* or antinfluenza*).tw,kw.
10. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
11. Plasma Transfusion/
12. exp Immunoglobulin/
13. ((convalesc* or recovered or cured or survivor* or survived or rehabilitat* or virus‐positive or virus neutrali* or virus inactivated or antibody‐rich or high‐titre* or high‐titer*) adj6 (plasma or blood or serum or sera)).mp.
14. ((plasma adj1 therap*) or gamma‐globulin* or "γ‐Globulin" or hyper‐Ig).tw,kw.
15. ((hyperimmune or hyper‐immune or high‐dos*) adj3 (plasma or immunoglobulin* or IVIG* or immune globulin* or globulin* or IgG)).tw,kw.
16. (plasma adj5 (immun* or antibod* or exchange* or donor* or donat* or transfus* or infus*)).mp.
17. ((convalesc* or recovered or cured or survivor* or rehabilitat* or survived or virus‐positive or virus inactivated or antibody‐positive) adj5 (donor* or donat*)).mp.
18. 11 or 12 or 13 or 14 or 15 or 16 or 17
19. 10 and 18
20. (Flu‐IVIG or ((anti‐flu* or anti‐influenza* or antiflu* or antinfluenza*) adj5 plasma)).mp.
21. 19 or 20
22. (exp animal/ or nonhuman/) not exp human/
23. Animal experiment/ not (human experiment/ or human/)
24. 22 or 23
25. 21 not 24
26. limit 25 to yr="2019 ‐Current"
Appendix 5. Search strategy PubMed
#1 (corona‐virus* OR corono‐virus* OR coronavirus* OR coronovirus* OR coronavirinae* OR Wuhan* OR Hubei* OR Huanan OR "2019 nCoV" OR 2019nCoV OR 2019 CoV OR nCoV2019 OR "nCoV 2019" OR "COVID 19" OR COVID19 OR "CORVID 19" OR CORVID19 OR "WN CoV" OR WNCoV OR "HCoV 19" OR HCoV19 OR CoV OR "2019 novel*" OR Ncov OR "n cov" OR "SARS CoV 2" OR "SARSCoV 2" OR "SARS‐CoV‐2" OR "SARSCoV‐2" OR "SARSCoV2" OR "SARS CoV2" OR SARSCov19 OR "SARS Cov19" OR "SARSCov 19" OR "SARS Cov 19" OR Ncovor OR Ncorona* OR Ncorono* OR NcovWuhan* OR NcovHubei* OR NcovChina* OR NcovChinese* OR SARSr‐cov)
#2 (((respiratory* AND (symptom* OR disease OR diseases OR diseased OR illness* OR condition*)) OR "seafood market*" OR "food market*") AND (Wuhan* OR Hubei* OR China OR "China’s" OR Chinese* OR Huanan*))
#3 ((outbreak* OR wildlife* OR pandemic* OR epidemic*) AND (China OR "China’s" OR Chinese* OR Huanan* OR Wuhan OR Hubei*))
#4 (anti‐flu* OR anti‐influenza* OR antiflu* OR antinfluenza*)
#5 #1 OR #2 OR #3 OR #4
#7 ((convalesc*[TIAB] OR recovered[TIAB] OR cured[TIAB] OR survivor*[TIAB] OR survived[TIAB] OR virus‐positive[TIAB] OR virus‐neutrali*[TIAB] OR "virus inactivated"[TIAB] OR antibod*[TIAB] OR high‐titre*[TIAB] OR high‐titer*) AND (plasma[TIAB] OR blood[TIAB] OR donor*[TIAB] OR donat*[TIAB]))
#8 ("therapeutic plasma" OR "plasma therapy" OR "immune plasma" OR "plasma exchange" OR gamma‐globulin* or "γ‐Globulin" or hyper‐Ig)
#9 (plasma[TI] AND (immun*[TIAB] OR transfus*[TIAB] OR infus*[TIAB]))
#10 ((hyperimmune OR hyper‐immune OR high‐dos*) AND (plasma OR immunoglobulin* OR IVIG* OR immune globulin* OR globulin*))
#11 #7 OR #8 OR #9 OR #10
#12 #6 AND #11
#13 (Flu‐IVIG OR ((anti‐flu* or anti‐influenza* or antiflu* or antinfluenza*) AND plasma))
#14 #12 OR #13
#15 (publisher[sb] OR inprocess[sb] OR pubmednotmedline[sb]) #16 #13 AND #15: Publication date from 2019/11/01 to present
Appendix 6. Search strategy CDC COVID‐19 Database (for searching in Endnote)
Any Field: plasma OR hyperimmune OR hyper‐immune OR IVIG OR immunoglobulin OR globulin OR immune‐globulin OR gamma‐globulin OR γ‐Globulin OR hyper‐Ig OR immunoglobulins OR globulins
Appendix 7. Search strategy Cochrane COVID‐19 Study Register
plasma OR hyperimmune OR hyper‐immune OR IVIG OR immunoglobulin OR globulin OR gamma‐globulin OR γ‐Globulin OR hyper‐Ig OR serum OR sera OR donor OR donation
Appendix 8. Search strategy ClinicalTrials.gov
COVID‐19 SUBSET
AND
Intervention: "convalescent plasma" OR "hyperimmune IVIG" OR "hyperimmune immunoglobulin" OR "plasma therapy" OR "immune plasma" OR "hyperimmune plasma" OR plasma OR IVIG OR immunoglobulin OR globulin OR immune‐globulin OR gamma‐globulin OR γ‐Globulin OR hyper‐Ig OR serum OR sera OR donor OR donation
Appendix 9. Search strategy WHO ICTRP (for searching in EndNote)
COVID‐19 SUBSET
AND
Any Field: plasma OR hyperimmune OR hyper‐immune OR IVIG OR immunoglobulin OR globulin OR gamma‐globulin OR γ‐Globulin OR hyper‐Ig OR serum OR sera OR donor OR donat
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahn 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 2 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | Both cases of SARS‐CoV‐2 negative at the time of publication, case 1 still hospitalised |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Low risk | Assessed and reported for both cases |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Assessed and reported for both cases |
| Well‐defined study group (reporting bias) | Low risk | Population and intervention are well described |
| Well‐defined outcome (reporting bias) Mortality | Low risk | Both cases of SARS‐CoV‐2 negative at the time of publication, case 1 still hospitalised |
| Well‐defined outcome (reporting bias) Adverse events | High risk | No adverse reaction occurred after the administration of CP in both cases. Observation period NR |
| Well‐defined outcome (reporting bias) Clinical improvement | Unclear risk | Improvement of symptoms described until the time of publication, case 1 still hospitalised |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Duan 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 10 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | Unclear whether all participants free of disease and discharged |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Low risk | Assessed for all participants over study period |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Assessed for all participants over study period |
| Well‐defined study group (reporting bias) | Low risk | Study population and intervention is well described |
| Well‐defined outcome (reporting bias) Mortality | High risk | Follow‐up not described |
| Well‐defined outcome (reporting bias) Adverse events | High risk | Follow‐up not described |
| Well‐defined outcome (reporting bias) Clinical improvement | Low risk | Clinical improvement described for all participants until day 4 post‐transfusion |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Pei 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants | (Preprint only, participant characteristics will be described in the supplementary material; not accessible yet)
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 3 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Low risk | Assessed for all participants until hospital discharge |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Unclear risk | SAE reported for 1 participant, not reported whether other participants experienced any AEs |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Unclear risk | Course of disease after convalescent plasma transfusion not reported |
| Well‐defined study group (reporting bias) | High risk | Study population and intervention insufficiently described |
| Well‐defined outcome (reporting bias) Mortality | Low risk | Followed until hospital discharge |
| Well‐defined outcome (reporting bias) Adverse events | High risk | Observation period not described |
| Well‐defined outcome (reporting bias) Clinical improvement | Unclear risk | Course of disease after convalescent plasma transfusion not reported |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Comorbidities and disease presentation and course not clearly reported; not adjusted for confounding factors |
Shen 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 5 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes. Data on clinical improvement taken from hospital computer medical system |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | Not all participants discharged |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Unclear risk | Unclear whether AEs occurred; outcome NR |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Reported for all 5 participants |
| Well‐defined study group (reporting bias) | Low risk | Study population well described, clear inclusion criteria |
| Well‐defined outcome (reporting bias) Mortality | Low risk | All participants alive, 2 still hospitalised |
| Well‐defined outcome (reporting bias) Adverse events | High risk | Outcome NR, unclear whether AEs occurred |
| Well‐defined outcome (reporting bias) Clinical improvement | Unclear risk | Probably still 2 participants on ICU, but unclear |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Tan 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 1 participant only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, but awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | Participant alive at last follow‐up, in hospital |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Unclear risk | Only fever reported, not reported whether other AEs occurred |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | High risk | Unclear why participant is still in hospital, clinical improvement not reported |
| Well‐defined study group (reporting bias) | High risk | 1 participant only, not much information (e.g. age, comorbidities, clinical symptoms), intervention not described in detail |
| Well‐defined outcome (reporting bias) Mortality | Low risk | 1 participant is still in hospital |
| Well‐defined outcome (reporting bias) Adverse events | High risk | Only fever reported, not reported whether other AEs occurred |
| Well‐defined outcome (reporting bias) Clinical improvement | High risk | Neither clinical symptoms nor clinical improvement reported in detail, but participant still in hospital |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Ye 2020.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 6 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, but awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | All participants alive (1 participant further monitored) |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Low risk | None occurred (3‐day follow‐up) |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Reported for all participants |
| Well‐defined study group (reporting bias) | Low risk | Study population and intervention well described |
| Well‐defined outcome (reporting bias) Mortality | Low risk | All alive (1 participant further monitored) |
| Well‐defined outcome (reporting bias) Adverse events | Low risk | 3‐day follow‐up |
| Well‐defined outcome (reporting bias) Clinical improvement | Low risk | Reported until considered cured or discharged |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Zhang 2020a.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 4 participants only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, but awareness of intervention can bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | All participants alive, 1 still on ICU |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Unclear risk | Clinical course reported, but not whether AEs occurred |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Reported for all 4 participants |
| Well‐defined study group (reporting bias) | Unclear risk | Study group well described but not intervention |
| Well‐defined outcome (reporting bias) Mortality | Low risk | All participants alive, 1 still hospitalised |
| Well‐defined outcome (reporting bias) Adverse events | High risk | Not described in detail, unclear whether AEs occurred |
| Well‐defined outcome (reporting bias) Clinical improvement | Low risk | Well defined |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
Zhang 2020b.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Representative study group (selection bias) | High risk | 1 participant only |
| Outcome detectors blinded to intervention (detection bias) Objective outcomes (e.g. mortality) | Low risk | Not blinded, but awareness of intervention cannot bias assessment of objective outcomes |
| Outcome detectors blinded to intervention (detection bias) Subjective outcomes | High risk | Not blinded, awareness of intervention cannot bias assessment of subjective outcomes |
| Complete outcome assessment/follow up (attrition bias) Mortality | Unclear risk | Alive but transferred to another ward |
| Complete outcome assessment/follow up (attrition bias) Adverse events | Low risk | Reported that no TRALIs were observed |
| Complete outcome assessment/follow up (attrition bias) Clinical improvement | Low risk | Clinical course assessed and briefly reported |
| Well‐defined study group (reporting bias) | Unclear risk | Participant not described in detail |
| Well‐defined outcome (reporting bias) Mortality | Low risk | Participant alive and transferred to general ward |
| Well‐defined outcome (reporting bias) Adverse events | Low risk | No AEs occurred |
| Well‐defined outcome (reporting bias) Clinical improvement | Unclear risk | Not described in detail; transferred to another ward |
| Important prognostic factors or follow‐up taken adequately into account (confounding) | High risk | Not adjusted for confounding factors |
AE: adverse event; ARDS: acute respiratory distress syndrome; COI: conflict of interest; COPD: chronic obstructive pulmonary disease; CP: convalescent plasma; CPK: creatine phosphokinase; CRP: C‐reactive protein; CT: computed tomography; ECMO: extracorporeal membrane oxygenation; ELISA: enzyme‐linked immunosorbent assay; FiO2: fractional inspired oxygen; GI: gastrointestinal; HBV/HCV: hepatitis B/C; ICU: intensive care unit; IgA (B/G/M): immunoglobulin A (B/G/M); IL‐6: interleukin‐6; IQR: interquartile range; IRB: Institutional Review Board; IV: intravenous; IVIG: intravenous immunoglobulin; LDH: lactate dehydrogenase; MODS: multiple organ dysfunction syndrome; NR: not reported; PaO2: arterial blood oxygen partial pressure; PCR: polymerase chain reaction; RNA: ribonucleic acid; RT‐PCR: reverse transcription polymerase chain reaction; SAE: serious adverse event; SARS: severe acute respiratory syndrome; TACO: transfusion‐associated circulatory overload; TAD: transfusion‐associated dyspnoea; TRALI: transfusion‐related acute lung injury
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bloch 2020 | Review |
| Cao 2020 | Ineligible intervention |
| Casadevall 2020 | Review |
| Chen 2020 | Review |
| ChiCTR2000030312 | Study cancelled before starting recruitment |
| ChiCTR2000030381 | Study cancelled before starting recruitment |
| ChiCTR2000030442 | Study cancelled before starting recruitment |
| Díez 2020 | Ineligible intervention |
| Hu 2020 | Ineligible intervention |
| Jawhara 2020 | Review |
| NCT04261426 | Ineligible intervention |
| NCT04323800 | Ineligible participant population (participants exposed to COVID‐19) |
| NCT04325672 | Study cancelled before starting recruitment |
| NCT04344015 | Feasibility of plasma collection only |
| NCT04344977 | Feasibility of plasma collection only |
| Roback 2020 | Review |
| Shi 2020 | Ineligible intervention |
| Syal 2020 | Review |
| Tanne 2020 | Review |
| Tiberghien 2020 | Review |
| Wong 2020 | Review |
| Xie 2020 | Ineligible intervention |
| Yoo 2020 | Review |
| Zhao 2020b | Review |
Characteristics of studies awaiting classification [ordered by study ID]
Qiu 2020.
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Notes |
|
Tu 2020.
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Notes |
|
AE: adverse event; COI: conflict of interest; CP: convalescent plasma; ICU: intensive care unit; IV: intravenous; NR: not reported; SAE: serious adverse event; TACO: transfusion‐associated circulatory overload; TAD: transfusion‐associated dyspnoea; TRALI: transfusion‐related acute lung injury
Characteristics of ongoing studies [ordered by study ID]
ChiCTR2000029757.
| Study name | Convalescent plasma for the treatment of severe and critical novel coronavirus pneumonia (COVID‐19): a prospective randomized controlled trial |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 14 February 2020 |
| Contact information | Liu Zhong Institute of Blood Transfusion, Chinese Academy of Medical Sciences, 26 Huacai Road, Chenghua District, Chengdu, Sichuan, 610000, Liuz@ibt.pumc.edu.cn Cao Bin Cherry Blossom Garden East Street, Chaoyang District, Beijing, 100029, caobin_ben@163.com |
| Notes |
|
ChiCTR2000029850.
| Study name | Study on convalescent plasma treatment for severe patients with novel coronavirus pneumonia (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 15 February 2020 |
| Contact information | Liang Yu The First Affiliated Hospital of Zhejiang University, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Disease, 79 Qingchun Road, Shangcheng District, Hangzhou, Zhejiang, 310003, yu‐liang@zju.edu.cn Xiaowei Xu 79 Qingchun Road, Shangcheng District, Hangzhou, Zhejiang, China, 310003, xxw69@126.com |
| Notes |
|
ChiCTR2000030010.
| Study name | A randomized, double‐blind, parallel‐controlled, trial to evaluate the efficacy and safety of anti‐SARS‐CoV‐2 virus inactivated plasma in the treatment of severe novel coronavirus pneumonia patients (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 19 February 2020 |
| Contact information | Liu Ying Wuhan Jinyintan Hospital (Wuhan Infectious Diseases Hospital) , 1 Yintan Road, Dongxihu District, Wuhan, Hubei, China , 430023, whsjytyy_gcp@163.com Zhang Dingyu 1 Yintan Road, Dongxihu District, Wuhan, Hubei, China, 430023, 1813886398@qq.com |
| Notes |
|
ChiCTR2000030039.
| Study name | Clinical study for infusing convalescent plasma to treat patients with new coronavirus pneumonia (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 February 2020 |
| Contact information | Liping Wang Affiliated Hospital of Xuzhou Medical University, 9 Kunpeng Road, Gulou District, Xuzhou, Jiangsu, 163wangliping@163.com China Xuebing Yan 9 Kunpeng Road, Gulou District, Xuzhou, Jiangsu, China, yxbxuzhou@126.com |
| Notes |
|
ChiCTR2000030179.
| Study name | Experimental study of novel coronavirus pneumonia rehabilitation plasma therapy severe novel coronavirus pneumonia (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 24 February 2020 |
| Contact information | Liu Wei The First Affiliated Hospital of Nanchang University, 17 Yongwai Main Street, Nanchang, Jiangxi, China, 330006, cdyfyliuwei@163.com Le Aiping 17 Yongwai Main Street, Nanchang, Jiangxi, China, 330006, leaiping@126.com |
| Notes |
|
ChiCTR2000030627.
| Study name | Study for using the healed novel coronavirus pneumonia (COVID‐19) patients plasma in the treatment of severe critical cases |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 February 2020 |
| Contact information | Guojun Zhang The First Affiliated Hospital of Zhengzhou University, 1 Jianshe Road East, Zhengzhou, He'nan, China, zlgj‐001@126.com Guojun Zhang 1 Jianshe Road East, Zhengzhou, He'nan, China, zlgj‐001@126.com |
| Notes |
|
ChiCTR2000030702.
| Study name | Plasma of the convalescent in the treatment of novel coronavirus pneumonia (COVID‐19) common patient: a prospective clinical trial |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 15 February 2020 |
| Contact information | Liu Zhong Institute of Blood Transfusion, Chinese Academy of Medical Sciences, 26 Huacai Road, Chenghua District, Chengdu, Sichuan, China, 610000, Liuz@ibt.pumc.edu.cn Cao Bin 2 Yinghua Street East, Chaoyang District, Beijing, China, 100029, caobin_ben@163.com |
| Notes |
|
ChiCTR2000030841.
| Study name | Exploratory study for immunoglobulin from cured COVID‐19 patients in the treatment of acute severe novel coronavirus pneuvirus (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 17 February 2020 |
| Contact information | Xiang Cheng nathancx@hust.edu.cn Union hospital of Tongji Medical College, Huazhong University of Science and Technology 1277 Jiefang Avenue, Jianghan District, Wuhan, Hubei, China |
| Notes |
|
ChiCTR2000030929.
| Study name | A randomized, double‐blind, parallel‐controlled trial to evaluate the efficacy and safety of anti‐SARS‐CoV‐2 virus inactivated plasma in the treatment of severe novel coronavirus pneumonia (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 17 March 2020 |
| Contact information | Lianghao Zhang 11443556@qq.com Sinopharm Wuhan Blood Products Co., Ltd. 1 Golden Industrial Park Road, Zhengdian, Jiangxia District, Wuhan, Hubei, China |
| Notes |
|
ChiCTR2000031501.
| Study name | The efficacy of convalescent plasma in patients with critical novel coronavirus pneumonia (COVID‐19): a pragmatic, prospective cohort study |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 17 March 2020 |
| Contact information | Weiqin LI liweiqindr@vip.163.com Eastern Theater General Hospital 305 Zhongshandong road, Xuanwu district, Nanjing, Jiangsu, China |
| Notes |
|
EUCTR2020‐001310‐38.
| Study name | A randomized, prospective, open label clinical trial on the use of convalescent plasma compared to best supportive care in patients with severe COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions | Interventions
|
| Outcomes |
|
| Starting date | 6 April 2020 |
| Contact information | Sixten Körper, IKT Ulm, 89081 Ulm, Germany; s.koerper@blutspende.de |
| Notes |
|
IRCT20151228025732N53.
| Study name | Evaluation of the therapeutic effects of convalescent plasma (CP) of recovered people from COVID‐19 in improving clinical and laboratory symptoms of hospitalised patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 20 April 2020 |
| Contact information | Alireza Emadi Semnan University of Medical Sciences, Semnan, Iran +98 23 3345 1336 are20935@semums.ac.ir |
| Notes |
|
IRCT20200310046736N1.
| Study name | Comparison of the therapeutic effect of convalescent plasma and plasma‐derived immunoglobulin‐enriched solution on COVID‐19 patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 24 March 2020 |
| Contact information | Parastoo Moradi Choghakabodi, Iran (Islamic Republic of); parastoomoradi40@yahoo.com |
| Notes |
|
IRCT20200325046860N1.
| Study name | Evaluation of convalescent plasma therapy in the treatment of patients with COVID‐19 disease |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 15 March 2020 |
| Contact information | Hassan Abolghasemi +98 21 8126 3166 h.abolghasemi.ha@gmail.com |
| Notes |
|
IRCT20200404046948N1.
| Study name | Randomized, parallel‐controlled and multi‐center clinical study evaluating the efficacy and safety of convalescent plasma, in the treatment of patients with severe SARS‐CoV‐2 infection (COVID‐19) |
| Methods |
|
| Participants | Participants
|
| Interventions |
|
| Outcomes |
|
| Starting date | 13 April 2020 |
| Contact information | Ramin Hamidi Farahani, Artesh University of Medical Sciences, Tehran, Iran; Amir.salarian@gmail.com |
| Notes |
|
IRCT20200409047007N1.
| Study name | The effect of plasma administration of COVID‐19 survivors in patients with acute respiratory distress syndrome due to COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 13 April 2020 |
| Contact information | Dr Mohsen Seddigh Shamsi, Mashhad University of Medical Sciences, Department of Internal Medicine, Taqi Abad Square, Mashhad, Iran |
| Notes |
|
IRCT20200413047056N1.
| Study name | Comparison between the efficacy of intravenous immunoglobulin and convalescent plasma in improving the condition of patients with COVID‐19: a randomized clinical trial |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 18 April 2020 |
| Contact information | Malihe Zangoue, Birjand University of Medical Sciences, Birjadn, Iran; mzangoue@yahoo.com |
| Notes |
|
NCT04264858.
| Study name | Treatment of acute severe 2019‐nCoV pneumonia with immunoglobulin from cured patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 17 March 2020 |
| Contact information | Xiang Cheng Department of Cardiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology Wuhan, Hubei, China, 430022 |
| Notes |
|
NCT04292340.
| Study name | The efficacy and safety of anti‐SARS‐CoV‐2 inactivated convalescent plasma in the treatment of novel coronavirus pneumonia patient (COVID‐19): an observational study |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 February 2020 |
| Contact information | Hongzhou Lu, Ph.D+86‐021‐37990333 ext 3222luhongzhou@fudan.edu.cn Shanghai Public Health Clinical Center Shanghai, Shanghai, China, 201508 |
| Notes |
|
NCT04321421.
| Study name | Plasma from donors recovered from new coronavirus 2019 as therapy for critical patients with Covid‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 17 March 2020 |
| Contact information | Catherine KlersyPavia, PV, Italy, 27100 Principal Investigator: Cesare Perotti, MDFoundation IRCCS San Matteo Hospital |
| Notes |
|
NCT04327349.
| Study name | Investigating effect of convalescent plasma on COVID‐19 patients outcome: a clinical trial |
| Methods |
|
| Participants |
|
| Interventions |
Treatment cross‐overs: not applicable |
| Outcomes |
|
| Starting date | 28 March 2020 |
| Contact information | NR |
| Notes |
|
NCT04332380.
| Study name | Convalescent plasma for patients with COVID‐19: a pilot study (CP‐COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 April 2020 |
| Contact information | Juan M Anaya Cabrera, MD, PhD ; +57 321 233 9828; anayajm@gmail.com Manuel E Rojas Quintana, MD, MSc; +57 315 459 9951; manuel_9316@hotmail.com |
| Notes |
|
NCT04332835.
| Study name | Convalescent plasma for patients with COVID‐19: a randomized, open label, parallel, controlled clinical study (CP‐COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 April 2020 |
| Contact information | Juan M Anaya Cabrera, MD, PhD; +57 321 233 9828; anayajm@gmail.com Manuel E Rojas Quintana, MD, MSc; +57 315 459 9951; manuel_9316@hotmail.com |
| Notes |
|
NCT04333251.
| Study name | Study testing convalescent plasma vs best supportive care |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 April 2020 |
| Contact information | NR |
| Notes |
|
NCT04333355.
| Study name | Safety in convalescent plasma transfusion to COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 15 April 2020 |
| Contact information | Servando Cardona‐Huerta, MD., Ph.D; +5218112121946; servandocardona@tec.mx Sylvia De la Rosa, MD; +5218111832730; sylvia.delarosa@tec.mx |
| Notes |
|
NCT04338360.
| Study name | Expanded access to convalescent plasma for the treatment of patients with COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | NR |
| Contact information | Michael Joyner, MD; 507‐255‐4288; USCOVIDplasma@mayo.edu |
| Notes |
|
NCT04340050.
| Study name | COVID‐19 convalescent plasma |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 10 April 2020 |
| Contact information | Maria Lucia Madariaga, MD; 773‐270‐2004; mlmadariaga@bsd.uchicago.edu |
| Notes |
|
NCT04342182.
| Study name | Convalescent plasma therapy from recovered COVID‐19 patients as therapy for hospitalized patients with COVID‐19 (CONCOVID Study) (ConCoVid‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 8 April 2020 |
| Contact information | Bart Rijnders, MD, PhD+31107033510; b.rijnders@erasmusmc.nl |
| Notes |
|
NCT04343261.
| Study name | Convalescent plasma in the treatment of COVID 19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 10 April 2020 |
| Contact information | Contact: Latha Dulipsingh, MD860‐714‐4402; Latha.Dulipsingh@trinityhealthofne.org |
| Notes |
|
NCT04343755.
| Study name | Convalescent plasma as treatment for hospitalized subjects with COVID‐19 infection |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 9 April 2020 |
| Contact information |
|
| Notes |
|
NCT04344535.
| Study name | Convalescent plasma to reduce complications associated with COVID‐19 infection: a randomized trial comparing the efficacy and safety of high‐titre anti‐SARS‐CoV‐2 plasma vs. standard plasma in hospitalized patients with COVID‐19 infection |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 8 April 2020 |
| Contact information | Contact information not shared Responsible party: Elliott Bennett‐Guerrero, Professor of Anesthesiology, Stony Brook University |
| Notes |
|
NCT04345289.
| Study name | Efficacy and safety of novel treatment options for adults with COVID‐19 pneumonia. A double‐blinded, randomized, multi‐stage, 6‐armed placebo‐controlled trial in the framework of an adaptive trial platform |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 20 April 2020 |
| Contact information | Contact: Thomas Benfield, MD, DMSc+45 38622302 thomas.lars.benfield@regionh.dk |
| Notes |
|
NCT04345523.
| Study name | Multi‐center, randomized clinical trial of convalescent plasma therapy versus standard of care for the treatment of COVID‐19 in hospitalized patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 3 April 2020 |
| Contact information | Cristina Avendaño Solá, MD, PhD +34 91 191 64 79 cavendano@salud.madrid.org |
| Notes |
|
NCT04345679.
| Study name | Anti COVID‐19 convalescent plasma therapy |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 14 April 2020 |
| Contact information |
|
| Notes |
|
NCT04345991.
| Study name | Cohort multiple randomized controlled trials open‐label of immune modulatory drugs and other treatments in covid‐19 patients ‐ CORIMUNO‐CORIPLASM: efficacy of convalescent plasma to treat SARS‐CoV2 infected patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 14 April 2020 |
| Contact information | Karine LACOMBE, PU‐PH +33 149283196 karine.lacombe2@aphp.fr |
| Notes |
|
NCT04346446.
| Study name | Efficacy of convalescent plasma therapy in severely sick COVID‐19 patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 14 April 2020 |
| Contact information | Dr Meenu Bajpai, MD, Institute of Liver and Biliary Sciences, India mailto:meenubajpai%40hotmail.com?subject=NCT04346446, ILBS‐COVID‐02, Efficacy of Convalescent Plasma Therapy in Severely Sick COVID‐19 Patients |
| Notes |
|
NCT04346589.
| Study name | A pilot study to explore the efficacy and safety of rescue therapy with antibodies from convalescent patients obtained with double ‐filtration plasmapheresis (DFPP) and infused in critically ill ventilated patients with coronavirus disease 2019 (COVID‐19) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | April 2020 |
| Contact information | Piero Luigi Ruggenenti, MD; 0039 035 267 ext 3814; pruggenenti@asst-pg23.it |
| Notes |
|
NCT04347681.
| Study name | A national collaborative multicenter phase II study for potential efficacy of convalescent plasma to treat severe COVID‐19 and patients at high risk of developing severe COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 12 April 2020 |
| Contact information | Hani AL‐Hashmi, MD; 00966564773377; hanih.hashmi@kfsh.med.sa Mahammad Awadallah, MSc; 00966545032312; mahammad.awadalla@kfsh.med.sa |
| Notes |
|
NCT04348656.
| Study name | A randomized open‐label trial of CONvalenscent plasma for hospitalized adults with acute COVID‐19 respiratory illness (CONCOR‐1) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 27 April 2020 |
| Contact information | Donald M Arnold, MD, McMaster University, Hamilton, Canada arnold@mcmaster.ca |
| Notes |
|
NCT04348877.
| Study name | Plasma rich antibodies from recovered patients from COVID19 (PRA‐001) |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 20 April 2020 |
| Contact information | Hossam Fahmy, Professor of Faculty of Medicine, Ain Shams University |
| Notes |
|
NCT04352751.
| Study name | Experimental use of convalescent plasma for passive immunization in current COVID‐19 pandemic in Pakistan in 2020 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | April 2020 |
| Contact information | Contact: Dr. Arshi Naz, PhD,Diplab; 00923232234376; labarshi@yahoo.com Contact: Dr. Neeta Maheshwary, MBBS M.Phil; 00923208247773; drneeta@hiltonpharma.com |
| Notes |
|
NCT04353206.
| Study name | A feasibility study assessing the safety of multiple doses of anti‐SARS‐CoV‐2 plasma in mechanically ventilated intubated patients with respiratory failure due to COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | May 2020 |
| Contact information | Noah Merin, MD PhD; 310‐423‐1160; Noah.Merin@cshs.org David Hager, MD PhD; dhager1@jhmi.edu |
| Notes |
|
NCT04354831.
| Study name | An open label, phase 2 study evaluating the efficacy and safety of high‐titre anti‐SARS‐CoV‐2 plasma in hospitalized patients with COVID‐19 infection |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 1 May 2020 |
| Contact information | Mary Beth Graham, MD, Medical College of Wisconsin, USA mailto:mbgraham%40mcw.edu?subject=NCT04354831, PRO00037712, A Study Evaluating the Efficacy and Safety of High‐Titer Anti‐SARS‐CoV‐2 Plasma in Hospitalized Patients With COVID‐19 Infection |
| Notes |
|
NCT04355767.
| Study name | Convalescent plasma to limit coronavirus associated complications: a randomized double‐blind, phase 2 study comparing the efficacy and safety of high‐titer anti‐SARS‐CoV‐2 plasma vs. placebo in emergency room patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | May 2020 |
| Contact information | Study team; 650‐724‐7186; jcunning@stanford.edu |
| Notes |
|
NCT04355897.
| Study name | CoVID‐19 plasma in treatment of COVID‐19 patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | NR |
| Contact information | Dean J Kereiakes, MD; 513‐585‐1777; lindnermd@thechristhospital.com |
| Notes |
|
NCT04356482.
| Study name | Determination of the dose and effectiveness of convalescent plasma in severely and very severely ill patients by COVID‐19 |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | May 2020 |
| Contact information | Luis M Villela, MD; +526624756529; luisvillela@yahoo.com Diego Espinoza, MD; +526623862375; dr.espinoza.peralta@gmail.com |
| Notes |
|
NCT04356534.
| Study name | Convalescent plasma trial in COVID ‐19 patients |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 19 April 2020 |
| Contact information | Manaf Al Qahtani, Dr. Royal College of Surgeons in Ireland ‐ Bahrain; mailto:mqahtani%40rcsi‐mub.com?subject=NCT04356534, BDF/R&REC/2020‐423, Convalescent Plasma Trial in COVID ‐19 Patients |
| Notes |
|
NCT04357106.
| Study name | COPLA Study: treatment of severe forms of coronavirus infection with convalescent plasma |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 13 April 2020 |
| Contact information | Juan Carlos Olivares‐Gazca, MD, MPH; 2222438100; jolivares@hsctmexico.com José Manuel Priesca‐Marin, MD; 2222438100; mpriesca@hsctmexico.com |
| Notes |
|
AE: adverse event; ALT: alanine transaminase; ARDS: acute respiratory distress syndrome; AST: aspartate transaminase; BAL: bronchoalveolar lavage; BMI: body mass index; CDC: Centers for Disease Control and Prevention; COI: conflict of interest; COPD: chronic obstructive pulmonary disease; CP: convalescent plasma; CPAP: continuous positive airway pressure; CPK: creatine phosphokinase; CRP: C‐reactive protein; CT: computed tomography; ECMO: extracorporeal membrane oxygenation; ED: emergency department; FDA: US Food and Drug Administration; FiO2: fractional inspired oxygen; GFR: glomerular filtration rate; HBV/HCV: hepatitis B/C; HCPOA: healthcare power of attorney; ICU: intensive care unit; IgA (B/G/M): immunoglobulin A (B/G/M); IL‐6: interleukin‐6; IV: intravenous; IVIG: intravenous immunoglobulin; LAR: legal authorised representative; LDH: lactate dehydrogenase; NR: not reported; NYHA: New York Heart Association; PaO2: arterial blood oxygen partial pressure; PCR: polymerase chain reaction; RCT: randomised controlled trial; RNA: ribonucleic acid; RT‐PCR: reverse transcription polymerase chain reaction; SAE: serious adverse event; SARS: severe acute respiratory syndrome; SC: subcutaneous; SOFA: Sequential Organ Failure Assessment; SpO2: peripheral capillary oxygen saturation; TACO: transfusion‐associated circulatory overload; TAD: transfusion‐associated dyspnoea; TB: tuberculosis; TRALI: transfusion‐related acute lung injury; TTP: thrombotic thrombocytopenic purpura; UIP: usual interstitial pneumonia; ULN: upper limit of normal; WHO: World Health Organization
Differences between protocol and review
Types of outcome measures
We revised the secondary outcome 'Improvement of clinical symptoms, assessed through need for respiratory support at up to 7 days; 8 to 15 days; 16 to 30 days' and added to the fourth bullet point: 'plus high‐flow oxygen', to differentiate from the third bullet point. It now reads:
Improvement of clinical symptoms, assessed by need for respiratory support at up to 7 days; 8 to 15 days; 16 to 30 days:
oxygen by mask or nasal prongs
oxygen by NIV (non‐invasive ventilation) or high flow
intubation and mechanical ventilation
mechanical ventilation plus high‐flow oxygen
extracorporeal membrane oxygenation (ECMO)
Electronic searches
As publication bias might influence all subsequent analyses and conclusions, we searched all potential relevant trials registries in detail to detect ongoing as well as completed studies, but not yet published studies. Nowadays, it is mandatory to provide results at least in the trials registry. In case results were not published elsewhere, we had planned to extract and analyse these data. However, no outcome data had yet been added to the trials registries.
Data extraction and management
We had planned to extract data using a standardised data extraction form developed in Covidence. However, we could not adapt the standardised form to our needs. Therefore we generated a customised data extraction form in Microsoft Excel (Microsoft Corporation 2018).
Summary of findings and assessment of the certainty of the evidence
At protocol stage we had planned to assess the certainty of the evidence for our primary outcomes (all‐cause mortality at hospital discharge and time to death), only. However, as none of the included studies reported any deaths during their study periods, we decided to assess the certainty of the evidence also for prioritised secondary outcomes (clinical improvement, grade 3 and 4 adverse events, and serious adverse events) to increase the informative value on effectiveness and safety of convalescent plasma therapy.
Some passages in this protocol, especially in the methods section, are from the standard template of Cochrane Haematology.
Contributions of authors
SJV: clinical expertise and conception and writing of the review
VP: methodological expertise and conception and writing of the review
KLC: clinical expertise and conception and writing of the review
CD: development of the search strategy
IM: development of the search strategy
EMW: clinical expertise and advice
AL: clinical expertise and advice
CK: clinical expertise and advice
ZM: clinical expertise and advice
CS‐O: clinical expertise and advice
LJE: clinical and methodological expertise and conception and writing of the review
NS: methodological expertise and advice and conception and writing of the review
Sources of support
Internal sources
-
Sanquin Blood Supply, Netherlands
Center for Clinical Transfusion Research
-
University Hospital of Cologne, Germany
Cochrane Cancer, Department I of Internal Medicine
-
Monash University, Australia
Transfusion Research Unit, Department of Epidemiology and Preventive Medicine
-
NHS Blood and Transplant, UK
NHS Blood and Transplant
External sources
No sources of support supplied
Declarations of interest
SJV: none known
VP: none known
KLC: HSANZ Leukaemia Foundation PhD scholarship to support studies at Monash University. This is not related to the work in this review.
CD: none known
IM: none known
EMW: I have sought funding support from Australian Medical Research Future Fund for a trial of convalescent plasma. I will not be involved in bias assessment, data extraction or interpretation, but will serve as a content expert.
AL: none known
CK: none known
ZM: I have sought funding support from Australian Medical Research Future Fund for a trial of convalescent plasma. I will not be involved in bias assessment, data extraction or interpretation, but will serve as a content expert.
CS‐O: is a member of the BEST Collaborative Clinical Study Group. I will not be involved in bias assessment, data extraction or interpretation, but will serve as a content expert.
LJE: co‐lead of the COVID‐19 immunoglobulin domain of the REMAP‐CAP trial. I will not be involved in bias assessment, data extraction or interpretation, but will serve as a content expert.
NS: none known
contributed equally
contributed equally
contributed equally
New
References
References to studies included in this review
Ahn 2020 {published data only}
- Ahn JY, Sohn Y, Lee SH, Cho Y, Hyun JH, Baek YJ, et al. Use of convalescent plasma therapy in two COVID-19 patients with acute respiratory distress syndrome in Korea. Journal of Korean Medical Science 2020; 35(14):e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duan 2020 {published data only}
- Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. In: National Academy of Sciences of the United States of America. Vol. 202004168. 2020. [DOI: 10.1073/pnas.2004168117] [DOI] [PMC free article] [PubMed]
- Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, et al. The feasibility of convalescent plasma therapy in severe COVID-19 patients: a pilot study. medRxiv 2020. [DOI: ]
Pei 2020 {published data only}
- Pei S, Yuan X, Zhimin ZZ, Run YR, Xie Y, Minxue SM, et al. Convalescent plasma to treat COVID-19: Chinese strategy and experiences. medRxiv 2020. [DOI: 10.1101/2020.04.07.20056440] [DOI]
Shen 2020 {published data only}
- Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 2020. [DOI: 10.1001/jama.2020.4783] [DOI] [PMC free article] [PubMed]
Tan 2020 {published data only}
- Tan L, Kang X, Zhang B, Zheng S, Liu B, Yu T, et al. A special case of COVID-19 with long duration of viral shedding for 49 days. medRxiv 2020. [DOI: 10.1101/2020.03.22.20040071] [DOI] [PMC free article] [PubMed]
Ye 2020 {published data only}
- Ye M, Fu D, Ren Y, Wang F, Wang D, Zhang F, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. Journal of Medical Virology 2020. [DOI: 10.1002/jmv.25882] [DOI] [PMC free article] [PubMed]
Zhang 2020a {published data only}
- Zhang B, Liu S, Tan T, Huang W, Dong Y, Chen L, et al. Treatment with convalescent plasma for critically ill patients with SARS-CoV-2 infection. Chest 2020 Mar 31 [Epub ahead of print]. [DOI: 10.1016/j.chest.2020.03.039] [DOI] [PMC free article] [PubMed]
Zhang 2020b {published data only}
- Zhang L, Pang R, Xue X, Bao J, Ye S, Dai Y, et al. Anti-SARS-CoV-2 virus antibody levels in convalescent plasma of six donors who have recovered from COVID-19. Aging 2020 Apr 22 [Epub ahead of print];12. [DOI: 10.18632/aging.103102] [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
Bloch 2020 {published data only}
- Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. Journal of Clinical Investigation 2020. [DOI: 10.1172/JCI138745] [DOI] [PMC free article] [PubMed]
Cao 2020 {published data only}
- Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infectious Diseases 2020; 7(3):ofaa102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casadevall 2020 {published data only}
- Casadevall A, Pirofski L A. The convalescent sera option for containing COVID-19. Journal of Clinical Investigation 2020; 130(4):1545-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2020 {published data only}
- Chen L, Xiong J, Bao L, Shi Y. Convalescent plasma as a potential therapy for COVID-19. Lancet Infectious Diseases 2020; 27:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
ChiCTR2000030312 {published data only}
- ChiCTR2000030312. Cancelled, due to modify the protocol A single-center, open-label and single arm trial to evaluate the efficacy and safety of anti-SARS-CoV-2 inactivated convalescent plasma in the treatment& [A single-center, open-label and single arm trial to evaluate the efficacy and safety of anti-SARS-CoV-2 inactivated convalescent plasma in the treatment of novel coronavirus pneumonia (COVID-19) patient]. www.chictr.org.cn/showproj.aspx?proj=50258 (first received 23 April 2020).
ChiCTR2000030381 {published data only}
- ChiCTR2000030381. Cancelled by investigator A randomized, open-label, controlled and single-center trial to evaluate the efficacy and safety of anti-SARS-CoV-2 inactivated convalescent plasma in the treatment of novel coronavirus pneumonia (COVID-19) patient [A randomized, open-label, controlled and single-center trial to evaluate the efficacy and safety of anti-SARS-CoV-2 inactivated convalescent plasma in the treatment of novel coronavirus pneumonia (COVID-19) patient]. www.chictr.org.cn/showproj.aspx?proj=50290 (first received 23 April 2020).
ChiCTR2000030442 {published data only}
- ChiCTR2000030442. Combination of tocilizumab, IVIG and CRRT in severe patients with novel coronavirus pneumonia (COVID-19). www.chictr.org.cn/showproj.aspx?proj=50380 (first received 23 April 2020).
Díez 2020 {published data only}
- Díez JM, Romero C, Gajardo R. Currently available intravenous immunoglobulin (Gamunex-C and Flebogamma© DIF) contains antibodies reacting against SARS-CoV-2 antigens. bioRxiv 2020. [DOI: 10.1101/2020.04.07.029017] [DOI] [PMC free article] [PubMed]
Hu 2020 {published data only}
- Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. European Heart Journal 2020; 16:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jawhara 2020 {published data only}
- Jawhara S. Could intravenous immunoglobulin collected from recovered coronavirus patients protect against COVID-19 and strengthen the immune system of new patients? International Journal of Molecular Sciences 2020; 21(7):2272. [DOI: 10.3390/ijms21072272] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT04261426 {published data only}
- NCT04261426. The efficacy of intravenous immunoglobulin therapy for severe 2019-nCoV infected pneumonia. clinicaltrials.gov/ct2/show/NCT04261426 (first received 23 April 2020).
NCT04323800 {published data only}
- NCT04323800. Convalescent plasma to stem coronavirus: a randomized, blinded phase 2 study comparing the efficacy and safety human coronavirus immune plasma (HCIP) vs. control (SARS-CoV-2 non-immune plasma) among adults exposed to COVID-19. clinicaltrials.gov/show/NCT04323800 (first received 23 April 2020).
NCT04325672 {published data only}
- NCT04325672. Convalescent plasma to limit coronavirus associated complications: an open label, phase 2A study of high-titer anti-SARS-CoV-2 plasma in hospitalized patients with COVID-19. clinicaltrials.gov/show/NCT04325672 (first received 23 April 2020).
NCT04344015 {published data only}
- NCT04344015. COVID-19 plasma collection. ClinicalTrials.gov/show/NCT04344015 (first received 23 April 2020).
NCT04344977 {published data only}
- NCT04344977. COVID-19 plasma collection. clinicaltrials.gov/ct2/show/NCT04344977 (first received 23 April 2020).
Roback 2020 {published data only}
Shi 2020 {published data only}
- Shi H, Zhou C, He P, Huang S, Duan Y, Wang X, et al. Successful treatment of plasma exchange followed by intravenous immunoglobulin in a critically ill patient with 2019 novel coronavirus infection. International Journal of Antimicrobial Agents 2020:105974. [DOI] [PMC free article] [PubMed]
Syal 2020 {published data only}
- Syal K. COVID-19: herd immunity and convalescent plasma transfer therapy. Journal of Medical Virology 2020; 13:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanne 2020 {published data only}
- Tanne JH. Covid-19: FDA approves use of convalescent plasma to treat critically ill patients. BMJ 2020; 368:m1256. [DOI] [PubMed] [Google Scholar]
Tiberghien 2020 {published data only}
Wong 2020 {published data only}
- Wong HK, Lee CK. Pivotal role of convalescent plasma in managing emerging infectious diseases. Vox Sanguinis 2020. [DOI: 10.1111/vox.12927] [DOI] [PMC free article] [PubMed]
Xie 2020 {published data only}
- Xie Y, Cao S, Li Q, Chen E, Dong H, Zhang W, et al. Effect of regular intravenous immunoglobulin therapy on prognosis of severe pneumonia in patients with COVID-19. Journal of Infection 2020:S0163-4453(20)30172-9. [DOI] [PMC free article] [PubMed]
Yoo 2020 {published data only}
- Yoo JH. Convalescent plasma therapy for corona virus disease 2019: a long way to go but worth trying. Journal of Korean Medical Science 2020; 35(14):e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhao 2020b {published data only}
- Zhao Q, He Y. Challenges of convalescent plasma therapy on COVID-19. Journal of Clinical Virology 2020; 127:104358. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Qiu 2020 {published data only}
- Qiu T, Wang J, Zhou J, Zou J, Chen Z, Ma X, et al. The report of two cases infection with novel coronavirus (2019-ncov) after kidney transplantation and the association literature analyzation. Chinese Journal of Organ Transplantation 2020; 41(0):E004. [Google Scholar]
Tu 2020 {published data only}
- Tu Y, Wu X, Liu F, Wang J, Luo Y, Cai Z, et al. Two clinical cases of novel coronavirus pneumonia (NCP) in renal transplant recipients. Chinese Journal of Organ Transplantation 2020; 41(0):E005. [Google Scholar]
References to ongoing studies
ChiCTR2000029757 {published data only}
- ChiCTR2000029757. Convalescent plasma for the treatment of severe and critical novel coronavirus pneumonia (COVID-19): a prospective randomized controlled trial. www.chictr.org.cn/showproj.aspx?proj=49081 (first received 12 February 2020).
ChiCTR2000029850 {published data only}
- ChiCTR2000029850. Effecacy and safety of convalescent plasma treatment for severe patients with novel coronavirus pneumonia (COVID-19): a prospective cohort study. www.chictr.org.cn/showproj.aspx?proj=49533 (first received 15 February 2020).
ChiCTR2000030010 {published data only}
- ChiCTR2000030010. A randomized, double-blind, parallel-controlled, trial to evaluate the efficacy and safety of anti-SARS-CoV-2 virus inactivated plasma in the treatment of severe novel coronavirus pneumonia patients (COVID-19). www.chictr.org.cn/showproj.aspx?proj=49777 (first received 19 February 2020).
ChiCTR2000030039 {published data only}
- ChiCTR2000030039. Clinical study for infusing convalescent plasma to treat patients with new coronavirus pneumonia (COVID-19). www.chictr.org.cn/showproj.aspx?proj=49544 (first received 21 February 2020).
ChiCTR2000030179 {published data only}
- ChiCTR2000030179. Experimental study of novel coronavirus pneumonia rehabilitation plasma therapy severe novel coronavirus pneumonia (COVID-19). www.chictr.org.cn/showproj.aspx?proj=50059 (first received 24 February 2020).
ChiCTR2000030627 {published data only}
- ChiCTR2000030627. Study on the application of convalescent plasma therapy in severe COVID-19. www.chictr.org.cn/showproj.aspx?proj=50727 (first received 8 March 2020).
ChiCTR2000030702 {published data only}
- ChiCTR2000030702. Convalescent plasma for the treatment of common COVID-19: a prospective randomized controlled trial. www.chictr.org.cn/showproj.aspx?proj=50537 (first received 10 March 2020).
ChiCTR2000030841 {published data only}
- ChiCTR2000030841. Treatment of acute severe COVID-19 with immunoglobulin from cured COVID-19 patients. www.chictr.org.cn/showproj.aspx?proj=51072 (first received 15 March 2020).
ChiCTR2000030929 {published data only}
- ChiCTR2000030929. A randomized, double-blind, parallel-controlled trial to evaluate the efficacy and safety of anti-SARS-CoV-2 virus inactivated plasma in the treatment of severe novel coronavirus pneumonia (COVID-19). www.chictr.org.cn/showproj.aspx?proj=50696 (first received 17 March 2020).
ChiCTR2000031501 {published data only}
- ChiCTR2000031501. The efficacy of convalescent plasma in patients with critical novel coronavirus pneumonia (COVID-19): a pragmatic, prospective cohort study. www.chictr.org.cn/showproj.aspx?proj=50254 (first received 2 April 2020).
EUCTR2020‐001310‐38 {published data only}
- EUCTR2020-001310-38. A randomized, prospective, open label clinical trial on the use of convalescent plasma compared to best supportive care in patients with severe COVID-19. www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2020-001310-38 (first received 23 April 2020).
IRCT20151228025732N53 {published data only}
- IRCT20151228025732N53. Therapeutic effects of plasma of recovered people from COVID-19 on hospitalized patients with this disease. en.irct.ir/trial/46931 (first received 10 April 2020).
IRCT20200310046736N1 {published data only}
- IRCT20200310046736N1. Comparison of the therapeutic effect of convalescent plasma and plasma-derived immunoglobulin-enriched solution on COVID-19 patients. en.irct.ir/trial/46424 (first received 1 April 2020).
IRCT20200325046860N1 {published data only}
- IRCT20200325046860N1. Convalescent plasma therapy for COVID-19 patients. en.irct.ir/trial/46759 (first received 30 March 2020).
IRCT20200404046948N1 {published data only}
- IRCT20200404046948N1. Efficacy and safety of convalescent plasma in the treatment of COVID-19. en.irct.ir/trial/46973 (first received 15 April 2020).
IRCT20200409047007N1 {published data only}
- IRCT20200409047007N1. Effect of COVID 19 survivors plasma in COVID 19 patients with ARDS. en.irct.ir/trial/47058 (first received 12 April 2020).
IRCT20200413047056N1 {published data only}
- IRCT20200413047056N1. Comparison between the efficacy of intravenous immunoglobulin and convalescent plasma in COVID-19. en.irct.ir/trial/47212 (first received 17 April 2020).
NCT04264858 {published data only}
- NCT04264858. An exploratory clinical study on the treatment of acute severe 2019-nCoV pneumonia with immunoglobulin from cured 2019-nCoV pneumonia patients. clinicaltrials.gov/show/NCT04264858 (first received 11 February 2020).
NCT04292340 {published data only}
- NCT04292340. The efficacy and safety of anti-SARS-CoV-2 inactivated convalescent plasma in the treatment of novel coronavirus pneumonia patient (COVID-19): an observational study. clinicaltrials.gov/show/NCT04292340 (first received 3 March 2020).
NCT04321421 {published data only}
- NCT04321421. Plasma from donors recovered from new coronavirus 2019 as therapy for critical patients with COVID-19. clinicaltrials.gov/show/NCT04321421 (first received 25 March 2020).
NCT04327349 {published data only}
- NCT04327349. Investigating effect of convalescent plasma on COVID-19 patients outcome: a clinical trial. clinicaltrials.gov/show/NCT04327349 (first received 31 March 2020).
NCT04332380 {published data only}
- NCT04332380. Convalescent plasma for patients with COVID-19: a pilot study. clinicaltrials.gov/show/NCT04332380 (first received 2 April 2020).
NCT04332835 {published data only}
- NCT04332835. Convalescent plasma for patients with COVID-19: a randomized, open label, parallel, controlled clinical study. clinicaltrials.gov/show/NCT04332835 (first received 3 April 2020).
NCT04333251 {published data only}
- NCT04333251. Evaluating convalescent plasma to decrease coronavirus associated complications. A phase I study comparing the efficacy and safety of high-titer anti-Sars-CoV-2 plasma vs best supportive care in hospitalized patients with interstitial pneumonia due to COVID-19. clinicaltrials.gov/show/NCT04333251 (first received 3 April 2020).
NCT04333355 {published data only}
- NCT04333355. Phase 1 study to evaluate the safety of convalescent plasma as an adjuvant therapy in patients with SARS-CoV-2 infection. clinicaltrials.gov/show/NCT04333355 (first received 3 April 2020).
NCT04338360 {published data only}
- NCT04338360. Expanded access to convalescent plasma for the treatment of patients with COVID-19. ClinicalTrials.gov/show/NCT04338360 (first received 8 April 2020).
NCT04340050 {published data only}
- NCT04340050. COVID-19 convalescent plasma. ClinicalTrials.gov/show/NCT04340050 (first received 9 April 2020).
NCT04342182 {published data only}
- NCT04342182. Convalescent plasma as therapy for Covid-19 severe SARS-CoV-2 disease (CONCOVID Study) (ConCoVid-19). ClinicalTrials.gov/show/NCT04342182 (first received 10 April 2020).
NCT04343261 {published data only}
- NCT04343261. Convalescent plasma in the treatment of COVID 19. ClinicalTrials.gov/show/NCT04343261 (first received 13 April 2020).
NCT04343755 {published data only}
- NCT04343755. Convalescent plasma as treatment for hospitalized subjects with COVID-19 infection. ClinicalTrials.gov/show/NCT04343755 (first received 13 April 2020).
NCT04344535 {published data only}
- NCT04344535. Convalescent plasma vs. standard plasma for COVID-19. ClinicalTrials.gov/show/NCT04344535 (first received 14 April 2020).
NCT04345289 {published data only}
- EUCTR2020-001367-88-DK. Efficacy and safety of novel treatment options for adults with COVID-19 pneumonia. apps.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2020-001367-88-DK (first received 14 April 2020).
- NCT04345289. Efficacy and safety of novel treatment options for adults with COVID-19 pneumonia (CCAP). ClinicalTrials.gov/show/NCT04345289 (first received 14 April 2020).
NCT04345523 {published data only}
- NCT04345523. Convalescent plasma therapy vs. SOC for the treatment of COVID19 in hospitalized patients (ConPlas-19). ClinicalTrials.gov/show/NCT04345523 (first received 14 April 2020).
NCT04345679 {published data only}
- NCT04345679. Anti COVID-19 convalescent plasma therapy. ClinicalTrials.gov/show/NCT04345679 (first received 14 April 2020).
NCT04345991 {published data only}
- NCT04345991. Efficacy of convalescent plasma to treat COVID-19 patients, a nested trial in the CORIMUNO-19 cohort. ClinicalTrials.gov/show/NCT04345991 (first received 15 April 2020).
NCT04346446 {published data only}
- NCT04346446. Efficacy of convalescent plasma therapy in severely sick COVID-19 patients. ClinicalTrials.gov/show/NCT04346446 (first received 15 April 2020).
NCT04346589 {published data only}
- NCT04346589. Convalescent antibodies infusion in critically ill COVID 19 patients. clinicaltrials.gov/ct2/show/NCT04346589 (first received 15 April 2020).
NCT04347681 {published data only}
- NCT04347681. Potential efficacy of convalescent plasma to treat severe COVID-19 and patients at high risk of developing severe COVID-19. ClinicalTrials.gov/show/NCT04347681 (first received 15 April 2020).
NCT04348656 {published data only}
- NCT04348656. Convalescent plasma for hospitalized adults with COVID-19 respiratory illness (CONCOR-1). ClinicalTrials.gov/show/NCT04348656 (first received 16 April 2020).
NCT04348877 {published data only}
- NCT04348877. Plasma rich antibodies from recovered patients from COVID19. ClinicalTrials.gov/show/NCT04348877 (first received 16 April 2020).
NCT04352751 {published data only}
- NCT04352751. Experimental use of convalescent plasma for passive immunization in current COVID-19 pandemic in Pakistan in 2020. ClinicalTrials.gov/show/NCT04352751 (first received 20 April 2020).
NCT04353206 {published data only}
- NCT04353206. Convalescent plasma in ICU patients with COVID-19-induced respiratory failure. ClinicalTrials.gov/show/NCT04353206 (first received 20 April 2020).
NCT04354831 {published data only}
- NCT04354831. A study evaluating the efficacy and safety of high-titer anti-SARS-CoV-2 plasma in hospitalized patients with COVID-19 infection. clinicaltrials.gov/ct2/show/NCT04354831 (first received 21 April 2020).
NCT04355767 {published data only}
- NCT04355767. Convalescent plasma vs. placebo in emergency room patients with COVID-19. clinicaltrials.gov/ct2/show/NCT04355767 (first received 21 April 2020).
NCT04355897 {published data only}
- NCT04355897. CoVID-19 plasma in treatment of COVID-19 patients. clinicaltrials.gov/ct2/show/NCT04355897 (first received 21 April 2020).
NCT04356482 {published data only}
- NCT04356482. Convalescent plasma for ill patients by COVID-19. ClinicalTrials.gov/show/NCT04356482 (first received 22 April 2020).
NCT04356534 {published data only}
- NCT04356534. Convalescent plasma trial in COVID -19 patients. ClinicalTrials.gov/show/NCT04356534 (first received 22 April 2020).
NCT04357106 {published data only}
- NCT04357106. COPLA study: treatment of severe forms of coronavirus infection with convalescent plasma. ClinicalTrials.gov/show/NCT04357106 (first received 22 April 2020).
Additional references
Bao 2020
- Bao L, Deng W, Gao H, Xiao C, Liu J, Xue J, et al. Reinfection could not occur in SARS-CoV-2 infected rhesus macaques. bioRxiv (accessed 13 April 2020). [DOI: 10.1101/2020.03.13.990226] [DOI]
Baudel 2020
- Baudel JL, Vigneron C, Pras-Landre V, Joffre J, Marjot F, Ait-Oufella H, et al. Transfusion-related acute lung injury (TRALI) after intravenous immunoglobulins: French multicentre study and literature review. Clinical Rheumatology 2020; 39(2):541-6. [DOI] [PubMed] [Google Scholar]
Beigel 2017
- Beigel JH, Tebas P, Elie-Turenne MC, Bajwa E, Bell TE, Cairns B, et al. Immune plasma for the treatment of severe influenza: an open-label, multicentre, phase 2 randomised study. Lancet Respiratory Medicine 2017; 5(6):500-11. [DOI: 10.1016/S2213-2600(17)30174-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beigel 2019
- Beigel JH, Aga E, Elie-Turenne M-C, Cho J, Tebas P, Clark CL, et al. Anti-influenza immune plasma for the treatment of patients with severe influenza A: a randomised, double-blind, phase 3 trial. Lancet Respiratory Medicine 2019; 7(11):941-50. [DOI: 10.1016/S2213-2600(19)30199-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brennan 2003
- Brennan VM, Salomé-Bentley NJ, Chapel HM, Immunology Nurses Study. Prospective audit of adverse reactions occurring in 459 primary antibody-deficient patients receiving intravenous immunoglobulin. Clinical and Experimental Immunology 2003; 133(2):247-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2020a
- Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 (COVID-19). www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html (accessed 13 April 2020).
CDC 2020b
- Centers for Disease Control and Prevention (CDC). Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html (last accessed 26 April 2020).
Chun 2016
- Chun S, Chung CR, Ha YE, Han TH, Ki CS, Kang ES, et al. Possible transfusion-related acute lung injury following convalescent plasma transfusion in a patient with Middle East respiratory syndrome. Annals of Laboratory Medicine 2016; 36(4):393-5. [DOI: 10.3343/alm.2016.36.4.393] [DOI] [PMC free article] [PubMed] [Google Scholar]
COMET 2020
- Core outcome set developers’ response to COVID-19 (2nd April 2020). www.comet-initiative.org/Studies/Details/1538 (accessed 9 April 2020).
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed 20 April 2020. Melbourne, Australia: Veritas Health Innovation.Available at covidence.org.
Davey 2019
- Davey RT Jr, Fernández-Cruz E, Markowitz N, Pett S, Babiker AG, Wentworth D, et al. Anti-influenza hyperimmune intravenous immunoglobulin for adults with influenza A or B infection (FLU-IVIG): a double-blind, randomised, placebo-controlled trial. Lancet Respiratory Medicine 2019; 7(11):951-63. [DOI: 10.1016/S2213-2600(19)30253-X] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG, editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Driggin 2020
- Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. Journal of the American College of Cardiology 2020; 75(18):2352-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eibl 2008
- Eibl MM. History of immunoglobulin replacement. Immunology and Allergy Clinics of North America 2008; 28(4):737-64. [DOI: 10.1016/j.iac.2008.06.004] [DOI] [PubMed] [Google Scholar]
EPOC 2017
- Cochrane Effective Practice and Organisation of Care (EPOC). What study designs can be considered for inclusion in an EPOC review and what should they be called? EPOC Resources for review authors. Available from epoc.cochrane.org/resources/epoc-resources-review-authors (accessed 23 April 2019).
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 20 April 2020. Hamilton (ON): McMaster University (developed by Evidence Prime).Available at gradepro.org.
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2019a
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Higgins 2019b
- Higgins JP, Deeks JJ, editor(s). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Ho 2005
- Ho MS, Chen WJ, Chen HY, Lin SF, Wang MC, Di J, et al. Neutralizing antibody response and SARS severity. Emerging Infectious Diseases 2005; 11(11):1730-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2020
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223):497-506. [DOI: 10.1016/S0140-6736(20)30183-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hung 2013
- Hung IF, To KK, Lee CK, Lee KL, Yan WW, Chan K, et al. Hyperimmune IV immunoglobulin treatment: a multicenter double-blind randomized controlled trial for patients with severe 2009 influenza A(H1N1) infection. Chest 2013; 144(2):464-73. [DOI: 10.1378/chest.12-2907] [DOI] [PubMed] [Google Scholar]
Kim 2020
- Kim D-H, Choe YJ, Jeong J-Y. Understanding and interpretation of case fatality rate of coronavirus disease 2019. Journal of Korean Medical Science 2020; 35(12):e137. [DOI: 10.3346/jkms.2020.35.e137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kreijtz 2011
- Kreijtz JH, Fouchier RA, Rimmelzwaan GF. Immune responses to influenza virus infection. Virus Research 2011; 162(1-2):19-30. [DOI: 10.1016/j.virusres.2011.09.022] [DOI] [PubMed] [Google Scholar]
Lauer 2020
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Annals of Internal Medicine 2020. [DOI: 10.7326/M20-0504] [DOI] [PMC free article] [PubMed]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf MI, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Li 2019
- Li T, Higgins JP, Deeks JJ, editor(s). Chapter 5: Collecting data. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Liang 2020
- Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncology 2020; 21(3):335-7. [DOI: 10.1016/S1470-2045(20)30096-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luke 2006
- Luke TC, Kilbane EM, Jackson JL, Hoffman SL. Meta-analysis: convalescent blood products for Spanish influenza pneumonia: a future H5N1 treatment? Annals of Internal Medicine 2006; 145(8):599-609. [DOI] [PubMed] [Google Scholar]
Mair‐Jenkins 2015
- Mair-Jenkins J, Saavedra-Campos M, Baillie JK, Cleary P, Khaw FM, Lim WS, et al. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis. Journal of Infectious Diseases 2015; 211(1):80-90. [DOI: 10.1093/infdis/jiu396] [DOI] [PMC free article] [PubMed] [Google Scholar]
Microsoft Corporation 2018 [Computer program]
- Microsoft Corporation, available at: office.microsoft.com/excel Mircosoft Excel. Microsoft Corporation. Microsoft Corporation, available at: office.microsoft.com/excel, 2018.
Mo 2006
- Mo H, Zeng G, Ren X, Li H, Ke C, Tan Y, et al. Longitudinal profile of antibodies against SARS-coronavirus in SARS patients and their clinical significance. Respirology 2006; 11(1):49-53. [DOI: 10.1111/j.1440-1843.2006.00783.x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology 2009; 62(10):1006-12. [DOI] [PubMed] [Google Scholar]
Morens 1994
- Morens DM. Antibody-dependent enhancement of infection and the pathogenesis of viral disease. Clinical Infectious Diseases 1994; 19(3):500-12. [DOI] [PubMed] [Google Scholar]
Mulder 2019
- Mulder RL, Bresters D, Van den Hof M, Koot BG, Castellino SM, Loke YK, et al. Hepatic late adverse effects after antineoplastic treatment for childhood cancer. Cochrane Database of Systematic Reviews 2019, Issue 4. [DOI: 10.1002/14651858.CD008205.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Otrock 2017
- Otrock ZK, Liu C, Grossman BJ. Transfusion‐related acute lung injury risk mitigation: an update. Vox Sanguinis 2017; 112(8):694-703. [DOI] [PubMed] [Google Scholar]
Pandey 2012
- Pandey S, Vyas GN. Adverse effects of plasma transfusion. Transfusion 2012; 52 Suppl 1:65S-79S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parmar 1998
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine 1998; 17(24):2815-34. [DOI] [PubMed] [Google Scholar]
Payne 2016
- Payne DC, Iblan I, Rha B, Algasrawi S, Hin A, Al Nsour M, et al. Persistence of antibodies against Middle East respiratory syndrome coronavirus. Emerging Infectious Disease Journal 2016; 22(10):1824-6. [DOI: 10.3201/eid2210.160706] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reeves 2019
- Reeves BC, Deeks JJ, Higgins JP, Shea B, Tugwell P, Wells GA. Chapter 24: Including non-randomized studies on intervention effects. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Review Manager Web [Computer program]
- The Cochrane Collaboration Review Manager Web (RevMan Web). The Cochrane Collaboration, 2019.Available from revman.cochrane.org.
Ricke 2020
- Ricke D, Malone R. Medical countermeasures analysis of 2019-nCoV and vaccine risks for antibody-dependent enhancement (ADE). www.preprints.org/manuscript/202003.0138/v1 2020; 2020030138. [DOI: 10.20944/preprints202003.0138.v1] [DOI]
Robbins 1995
- Robbins JB, Schneerson R, Szu SC. Perspective: hypothesis: serum IgG antibody is sufficient to confer protection against infectious diseases by inactivating the inoculum. Journal of Infectious Diseases 1995; 171(6):1387-98. [DOI] [PubMed] [Google Scholar]
Rock 2011
- Rock G. A comparison of methods of pathogen inactivation of FFP. Vox Sanguinis 2011; 100(2):169-78. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s) Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Sekul 1994
- Sekul EA, Cupler EJ, Dalakas MC. Aseptic meningitis associated with high-dose intravenous immunoglobulin therapy: frequency and risk factors. Annals of Internal Medicine 1994; 121(4):259-62. [DOI] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JA, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366:l4898. [DOI] [PubMed] [Google Scholar]
Stiehm 2013
- Stiehm ER. Adverse effects of human immunoglobulin therapy. Transfusion Medicine Reviews 2013; 27(3):171-8. [DOI] [PubMed] [Google Scholar]
Team 2020
- Team NCPERE . Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China. China CDC Weekly 2020; 2(8):113-22. [DOI: 10.3760/cma.j.issn.0254-6450.2020.02.003] [DOI] [PMC free article] [PubMed]
Tierney 2007
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007; 8:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tolouian 2020
- Tolouian R, Vahed SZ, Ghiyasvand S, Tolouian A, Ardalan M. COVID-19 interactions with angiotensin-converting enzyme 2 (ACE2) and the kinin system; looking at a potential treatment. Journal of Renal Injury Prevention 2020; 9(2):e19. [DOI: 10.34172/jrip.2020.19] [DOI] [Google Scholar]
Van de Veerdonk 2020
- Van de Veerdonk F, Netea MG, Van Deuren M, Van der Meer JW, De Mast Q, Bruggemann RJ, et al. Kinins and cytokines in COVID-19: a comprehensive pathophysiological approach. Preprints 2020 (accessed 13 April 2020);2020040023. [DOI: 10.20944/preprints202004.0023.v1] [DOI] [Google Scholar]
Wan 2020
- Wan Y, Shang J, Sun S, Tai W, Chen J, Geng Q, et al. Molecular mechanism for antibody-dependent enhancement of coronavirus entry. Journal of Virology 2020; 94(5):e02015-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2014
- Wang S-F, Tseng S-P, Yen C-H, Yang J-Y, Tsao C-H, Shen C-W, et al. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochemical and Biophysical Research Communications 2014; 451(2):208-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2007
- World Health Organization (WHO). Cumulative number of reported probable cases of SARS. www.who.int/csr/sars/country/2003_07_11/en/ (accessed 13 April 2020).
WHO 2019
- World Health Organization (WHO). Middle East respiratory syndrome coronavirus (MERS-CoV). www.who.int/emergencies/mers-cov/en/ (accessed 13 April 2020).
WHO 2020a
- World Health Organization (WHO). Report of the WHO‐China Joint Mission on coronavirus disease 2019 (COVID‐19); February 2020. Available at www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.
WHO 2020b
- World Health Organization (WHO). Rolling updates on coronavirus diseases (COVID‐19). www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 13 April 2020).
WHO 2020c
- World Health Organization (WHO). Coronavirus disease (COVID-2019) situation report-105; 4 May 2020. Available at www.who.int/docs/default-source/coronaviruse/situation-reports/20200504-covid-19-sitrep-105.pdf.
WHO 2020d
- World Health Organization (WHO). Clinical management of severe acute respiratory infection (SARI) when COVID19 disease is suspected: interim guidance. World Health Organization 2020; WHO/2019-nCoV/clinical/2020.4.
Wu 2020a
- Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Internal Medicine 2020. [DOI: 10.1001/jamainternmed.2020.0994] [DOI] [PMC free article] [PubMed]
Wu 2020b
- Wu F, Wang A, Liu M, Wang Q, Chen J, Xia S, et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. medRxiv (accessed 13 April 2020). [DOI: ]
Xu 2020
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respiratory Medicine 2020; 8(4):420-2. [DOI: 10.1016/S2213-2600(20)30076-X] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhao 2020
- Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y, et al. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. medRxiv 2020. [DOI: 10.1101/2020.03.02.20030189] [DOI] [PMC free article] [PubMed]
References to other published versions of this review
Piechotta 2020
- Piechotta V, Valk SJ, Chai KL, Wood EM, Lamikanra A, Kimber C, et al. Safety and effectiveness of convalescent plasma or hyperimmune globulin for people with COVID-19: a rapid review. available at: doi.org/10.17605/OSF.IO/DWF53.


