Abstract
BACKGROUND AND AIM:
Given the prevalence of novel coronavirus disease 2019 (COVID-19) and the lack of information on coronavirus and pregnancy, the purpose of this study was to evaluate the association of COVID-19 and perinatal outcomes in pregnant women.
MATERIALS AND METHODS:
In the present review article, the search process was conducted on English and Persian scientific databases of PubMed, Scopus, Google Scholar, Magiran, Irandoc, Iranmedx, and SID as well as the websites of international organizations of World Health Organization and Centers for Disease Control and Prevention using the main keywords of “Pregnancy,” “Perinatal outcomes,” “Coronavirus,” “COVID-19,” “MERS-CoV,” “MERS,” “SARS-CoV-2,” and “SARS-CoV-1” and their Persian-equivalent keywords from inception until March 16 2020.
RESULTS:
The findings of studies on mothers with COVID-19 were limited, and insufficient information is available on the adverse pregnancy outcomes in pregnant women with COVID-19. In cases of infection with other coronaviruses such as Middle East respiratory syndrome and severe acute respiratory syndrome during pregnancy, there have been reports on adverse pregnancy outcomes such as miscarriage, stillbirth, preterm labor, low birth weight, and congenital malformations following high fever in the first trimester.
CONCLUSION:
Pregnant women may be more susceptible to viral respiratory infections, including COVID-19, due to immunological and physiological changes. Therefore, pregnant women should take routine preventive measures, such as washing their hands frequently and avoiding contact with infected people, to prevent infection.
Keywords: Coronavirus, coronavirus disease 2019, pregnancy, perinatal outcomes
Introduction
Coronaviruses are a family of RNA viruses, ranging from agents causing the common cold to severe acute respiratory syndrome (SARS). Most coronaviruses are not dangerous, but some of them can cause serious respiratory disorders. Middle East respiratory syndrome (MERS)- and SARS-related coronaviruses are responsible for respiratory complications.[1] The SARS disease appeared for the first time in 2003, whose outbreak claimed the lives of many victims. The MERS-related coronaviruses also appeared for the first time in 2012 and caused high mortality in countries in the Middle East, Africa, Asia, and Europe.[2] Recently, the World Health Organization (WHO) identified a novel coronavirus disease (COVID-19) called SARS-CoV-2 that was first reported from Wuhan, China, on December 31, 2019, which resulted in the deaths of many people.[2] The new coronavirus of SARS-CoV-2 is a new viral strain that is pathogenic to humans and causes novel coronavirus disease-2019 (COVID-19) in humans.[3] The outbreak of COVID-19 disease has become a main epidemic warning in the world. On January 30, 2020, the outbreak of COVID-19 was declared a Public Health Emergency of International Concern.[4] On March 16, 2020, the COVID-19 outbreak and coronavirus cases have been reported by more than 151 countries. According to the WHO report, China, Italy, Iran, the Republic of Korea, Spain, and France countries had the highest reported cases of the coronavirus disease.[5]
In a study by Lu et al., SARS-CoV-2 is genetically similar to two other coronaviruses: SARS-CoV-1 (about 79% of genomic similarity) and MERS (about 50% of genomic similarity).[5] Given that SARS-CoV-2 has a structure similar to SARS-CoV-1, the COVID-19 infection may have a pathogenesis similar to SARS-CoV-1 infection.[6,7]
Coronavirus causes respiratory symptoms such as cough, sore throat, runny nose, fever, and sometimes gastrointestinal symptoms such as abdominal pain and diarrhea. The incubation period of coronavirus is up to 14 days during which it can be infectious and transmissible.[8,9] The most common symptoms of COVID-19 infection are fever and cough, and the majority of patients have abnormal chest computed tomography (CT) scan. A number of patients also suffer from myalgia, fatigue, diarrhea, hemoptysis, headache, sore throat, shock, and acute respiratory syndrome. The most recent meta-analysis results in COVID-19 patients reported the presence of symptoms including fever (89.1%), cough (72.2%), fatigue (42.5%), acute respiratory syndrome (14.8%), abnormal chest CT scan (96.6%), very severe cases (18.1%), and an overall mortality rate of 4.3%.[10]
Because pregnant women are known to be at high risk for various diseases, and given the global prevalence of COVID-19, as well as the lack of information on coronavirus and pregnancy outcomes, this review study aimed to investigate the association between coronavirus and perinatal outcomes in pregnant women.
Materials and Methods
In the present review article, the search process on the published articles evaluating coronavirus and perinatal outcomes in pregnant women was conducted on English and Persian scientific databases of PubMed, Scopus, Google Scholar, Magiran, Irandoc, Iranmedx, and SID as well as the websites of international organizations of WHO and Centers for Disease Control and Prevention (CDC) using the main keywords of “Pregnancy”, “Perinatal outcomes,” “Coronavirus,” “COVID-19,” “MERS-CoV,” “SARS-CoV-2,” and “SARS-CoV-1” and their Persian-equivalent keywords from inception until March 16, 2020. Inclusion criteria were the insertion of the searched keywords in the title section and keywords of the articles. Many of the search efforts generated duplicate studies, or studies that were not linked to the study, which were not considered in this study. In addition, the reference section of relevant articles and systematic reviews was manually checked to identify additional articles missed by electronic search. In the process of extraction, one of the authors reviewed both the title of the articles and the abstract to determine its suitability for inclusion. Finally, the results of nine studies or guidelines with a focus on COVID-19 have been reported qualitatively [Figure 1].
Figure 1.
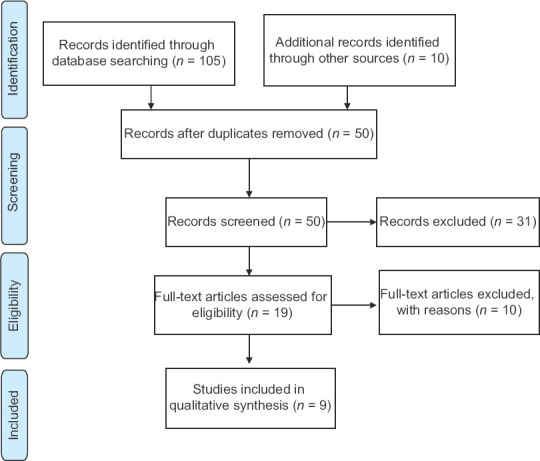
PRISMA flowchart of the study selection process
Results
Studies on COVID-19 included one study and recommendations for pregnant women by the CDC. Due to the <2 months after the outbreak of COVID-19, the findings of studies on mothers with COVID-19 were limited, so the findings of studies on other coronaviruses such as SARS are also reported.
In a study by Chen et al. on pregnant women with COVID-19, there was no evidence on the presence of SARS-CoV-2 in pregnancy products or in neonates of mothers with COVID-19. This study examined nine pregnant women with COVID-19 pneumonia at Zhongnan Hospital in Wuhan, China, who were admitted from January 20 to January 31, 2020, aimed at evaluating clinical symptoms in pregnancy and intrauterine infection caused by vertical transmission of COVID-19 infection. In this study, clinical signs of pregnant mothers, results of laboratory tests, and chest CT scan were retrospectively evaluated. The presence of SARS-CoV-2 virus was assessed in amniotic fluid, umbilical cord blood, and neonatal throat swab specimens. Breastmilk samples were also collected and tested after the first lactation. The findings of this study showed that all the nine patients had cesarean section in the third trimester, and seven of the nine mothers had a fever. Other symptoms included cough (n = 4), myalgia (n = 3), sore throat (n = 2), and weakness (n = 2). Five of the nine patients had lymphopenia. None of the patients had severe infection or death by February 4, 2020. No asphyxia was observed in the neonates, and the 1-min Apgar score of the nine infants was 8–9 and their 5-min Apgar score was 9–10. The samples of amniotic fluid, umbilical cord blood, and throat swabs from neonates and breastmilk of six patients were tested for SARS-CoV-2, and all samples showed negative results.[11]
According to the CDC, there is currently no information available on the susceptibility of pregnant women to COVID-19. Admittedly, pregnant women may be more susceptible to viral respiratory infections, including COVID-19, due to immunological and physiological changes. Pregnant women may also be exposed to more severe illness and morbidity and mortality than the general population, as they are more susceptible to other coronavirus infections, including SARS-CoV and MERS-CoV, and other viral respiratory infections, such as the flu.[12] The CDC also stated that no information was available on the adverse pregnancy outcomes in pregnant women with COVID-19. However, in cases of infection with other associated coronaviruses, such as SARS-CoV and MERS-CoV during pregnancy, the adverse pregnancy outcomes include miscarriage and stillbirth. Elevated fever in the first trimester of pregnancy can also increase the risk of congenital disorders.[11]
In a study, Wang et al. (2004) compared pregnancy and nonpregnancy outcomes in ten pregnant women and forty nonpregnant women with SARS who had positive SARS-CoV-1 results. The results showed that the pregnant women generally had worse outcomes than nonpregnant women. Among pregnant women, five were in the first trimester and five in the second and third trimesters (26–32 weeks), none of whom had any specific disease. Four patients experienced abortion, and four patients had preterm labor after the second trimester (26–33 weeks). None of the five newborns had SARS-CoV infection, but three had preterm complications. Clinical manifestations in two similar groups were fever and chills, nausea, restlessness, diarrhea, myalgia, headache, dyspnea, chest pain, sore throat, and cough. The prevalence of viral pneumonia in the pregnant women was higher than that in the general population. The pregnant women also had significant complications, including acute kidney failure, sepsis, and disseminated intravascular coagulation. The pregnant women needed more intensive care than nonpregnant women (60% vs. 17.5%), and 40% of the pregnant women and 12.5% of the nonpregnant women needed mechanical ventilation with positive end-expiratory pressure. There were three deaths in the pregnant women group. All women survived in the nonpregnant group. Duration of hospitalization in the pregnant women was longer than that in the nonpregnant women (27 days vs. 17.3 days).[13]
In Qiao's study, pregnant women were vulnerable to respiratory infections and pneumonia, which probably makes them more vulnerable to COVID-19 than the other people, especially if they have chronic disorder. For that reason, in strategies focusing on the management and prevention of COVID-19, pregnant women and their babies should be considered key at-risk persons.[14] Rasmussen et al. stated that health systems for managing pregnant women with COVID-19 infections need more information on pregnancy status and also prenatal and perinatal outcomes. They mentioned that in the context of the spread of the COVID-19, health systems must be alert and able to control outbreaks. In addition, the basic care for pregnant women with COVID-19 and acute respiratory disease needs to be implemented forceful in a team-based care model.[15]
The first reported case of COVID-19 in a pregnant woman was a case presentation by Wang et al. The case is a 28-year-old pregnant mother with COVID-19 who was 30-week pregnant. The mother was in severe atypical pneumonia based on chest CT scan finding. There was no variability of fetal heart rate during monitoring, and fetal movements decreased. She delivered a healthy baby by emergency cesarean section. A preterm baby was delivered with Apgar scores at 1 and 5 min of 9 and 10, respectively. The baby had no evidence of COVID-19.[16] In a study, Liu et al., COVID-19 cases were reported in pregnant women and their newborn infant in Wuhan, China. In their study, three pregnant women with COVID-19 infection in late pregnancy were described. Two mothers had cesarean section delivery in the third trimester. All women showed successful outcome. No newborns became infected during delivery or vertical transmission.[17]
In guidelines by Favre et al., for pregnant women with suspected SARS-CoV-2 infection, it was stated that infants delivered from mother who were infected by COVID-19 should be isolated for at least 14 days, and during this time, direct breastfeeding is not suggested.[18] Liu et al. reported the clinical manifestations of 15 pregnant women with COVID-19 pneumonia. The common symptoms were fever (13/15), cough (9/15), and lymphocytopenia (12/15). Successful delivery happened in 11 cases, and 4 cases are still in pregnancy. All newborns were healthy and no severe pneumonia occurred.[19]
Discussion
Given the limited studies available on COVID-19 during pregnancy, the CDC believes that being aware of the adverse consequences of other respiratory viral infections may be helpful. Other respiratory viral infections during pregnancy, such as acute respiratory syndrome and influenza, have been associated with neonatal side effects including low birth weight and preterm labor. In addition, the presence of cold or high fever flu in early pregnancy may increase the risk of congenital disorders in newborns. Infants of mothers with other coronavirus, SARS-CoV, and MERS-CoV infections are born premature and small for gestational age.[12]
The prevalence of viral pneumonia in pregnant women was higher than that in the general population.[20] The mortality rate in the 1918 epidemic influenza was 30%–50%.[21] The mortality rate of pregnant women was twice as high as that of nonpregnant women in the Asian flu outbreak of 1950.[22] The worse consequences for pregnant women can be due to the physiological changes in the immune and respiratory mechanisms in pregnancy. A reduction in cell-mediated immunity has been reported in pregnant women.[23,24] Maternal lymphocytes in the second and third trimesters of pregnancy show a marked decrease in response to stimulatory antigens. There is also a decrease in active natural killer cells. The association of the immunosuppressive system with pregnancy can be a stage for uncontrolled coronavirus proliferation.
In the second and third trimesters, the uterus raises the diaphragm up to 4 cm.[25] There is a decrease in expiratory reserve volume and residual volume in pregnancy and a 9.5%–25% reduction in functional residual capacity. Total lung capacity is also reduced throughout the term. In addition, the need for oxygen increases by 20%.[25] Thus, patients with coronavirus may have worsened maternal hypoxia, leading to premature labor and higher mortality in the affected women.[13]
Concerning mother-to-child vertical transmission of the virus infection, the COVID-19-related virus appears to be mainly transmitted through close contact with the infected person via respiratory droplets. Detailed information is unavailable on whether a pregnant woman with COVID-19 can transmit the virus to her fetus or newborns by other vertical transmission routes (before, during, or after delivery).[12] However, in a series of recent limited cases of neonates born to mothers with COVID-19 published in literature, a sample of neonatal throat swabs showed a virus-negative result.[11] Furthermore, the virus has not been detected in amniotic fluid or breastmilk samples. Limited information is available on the vertical transmission for other coronaviruses (MERS-CoV and SARS-CoV), and vertical transmission has not been reported for these infections.[12]
The CDC reports indicate that human-to-human transmission occurs through close contact with a patient with COVID-19, and is thought to be transmitted mainly through respiratory droplets, especially when the patient is coughing or sneezing. In the limited cases reported to date, no evidence of the virus has been found in the breastmilk of mothers with COVID-19, so there is no information on the transmission of COVID-19-related virus through breastmilk. In the limited reports of breastfeeding women with SARS-CoV, the virus has not been detected in the breastmilk. However, anti-SARS-CoV antibody was found in at least one sample.[12]
Preventive actions of coronavirus disease-19 for pregnant women
The CDC states that given that the interpersonal transmission of COVID-19-related virus has been observed in close contacts, pregnant women can avoid the risk of infection through routine preventive measures, such as washing their hands frequently and avoiding contact with affected people.[11] There is currently no vaccine to prevent COVID-19. The best strategy for disease prevention is to avoid exposure to the virus. However, as a reminder, the CDC always recommends daily preventive measures to prevent the spread of respiratory diseases, including washing hands with soap and water for at least 20 s; avoiding eye, nose, and mouth touch; and keeping a distance of at least 1 m (3 feet) between yourself and any person coughing or sneezing.[26,27]
Other preventive measures recommended by the WHO and CDC include covering mouth and nose mainly with disposable tissues or the inside of an elbow when coughing and sneezing. Just like the masks used, immediately put the used tissue into the trash can and wash your hands. The infected individuals will shed fewer viruses into the air around themselves by wearing masks, which potentially reduce the risk of others getting infected. For uninfected people, the effects of the mask are less pronounced because they usually are not sealed tight around the nose and mouth. Do not share foods, mugs, utensils, towels, or bedding with other people or pets in your home and wash all high-touch surfaces everyday by a spray cleaner, including counters, tabletops, doorknobs, bathroom fixtures, toilets, phones, keyboards, tablets, and bedside tables. Further, clean any surfaces that may have blood, stool, or body fluids on them. Use a household cleaning spray or wipe, according to the label instructions. Immediately seek medical care if you have fever, cough, and difficulty breathing.[26,27] However, limited information is available on COVID-19 infection because the disease is new. The results of this study could be a promising perspective on the care of pregnant women with this infection, given the widespread prevalence of the disease and the limited study on COVID-19, especially on pregnant women.
Conclusion
Limited information is available on pregnant women with COVID-19, but pregnant women may be more susceptible to viral respiratory infections, including COVID-19, due to immunological and physiological changes. Therefore, pregnant women should take routine preventive measures, such as washing their hands frequently and avoiding contact with infected people, to prevent infection.
Financial support and sponsorship
This study was financially supported by Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the authorities of Torbat Heydariyeh University of Medical Sciences for their comprehensive support for this study.
References
- 1.Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24:490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: The role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18:398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lorusso A, Calistri P, Petrini A, Savini G, Decaro N. Novel coronavirus (SARS-CoV-2) epidemic: A veterinary perspective. Vet Ital. 2020 Feb 12; doi: 10.12834/VetIt.2173.11599.1. [Epub ahead of print][Last accessed on March 16, 2020] [DOI] [PubMed] [Google Scholar]
- 4. [Last Accessed on March 16, 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen .
- 5. [Last Accessed on March 16, 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200316-sitrep-56-covid-19.pdf?sfvrsn=9fda7db2_2 .
- 6.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–74. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamming I, Timens W, Bulthuis M, Lely A, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rainer TH, Cameron PA, Smit D, Ong KL, Hung AN, Nin DC, et al. Evaluation of WHO criteria for identifying patients with severe acute respiratory syndrome out of hospital: Prospective observational study. BMJ. 2003;326:1354–8. doi: 10.1136/bmj.326.7403.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyer B, Müller MA, Corman VM, Reusken CB, Ritz D, Godeke GJ, et al. Antibodies against MERS coronavirus in dromedary camels, United Arab Emirates, 2003 and 2013. Emerg Infect Dis. 2014;20:552. doi: 10.3201/eid2004.131746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun P, Qie S, Liu Z, Ren J, Xi J. Clinical characteristics of 50466 patients with 2019-nCoV infection. [Last accessed on March 16, 2020];medRxiv. 2020 Jan 1; [Google Scholar]
- 11.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. [Last accessed on March 30, 2020];Lancet. 2020 Mar 7;:395. doi: 10.1016/S0140-6736(20)30360-3. (10226):809-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC. [Last update on 2020 Feb 25]. Available from: https://wwwcdcgov/coronavirus/2019-ncov/specific-groups/pregnancy-faqhtml .
- 13.Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191:292–7. doi: 10.1016/j.ajog.2003.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395:760–2. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. [Last accessed on March 30, 2020];Am J Obstet Gynecol. 2020 Feb 24; doi: 10.1016/j.ajog.2020.02.017. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020. Feb 28, [Last accessed on March 30, 2020]. Epub ahead of print. Available from: https://umsuacir/uploads/129pdf . [DOI] [PMC free article] [PubMed]
- 17.Liu W, Wang Q, Zhang Q, Chen L, Chen J, Zhang B, et al. Coronavirus disease 2019 (COVID-19) during pregnancy: A case series Preprints 2020, 2020020373. [Last accessed on March 30, 2020]. Available from: https://wwwpreprintsorg/manuscript/2020020373/v1 .
- 18.Favre G, Pomar L, Qi X, Nielsen-Saines K, Musso D, Baud D. Guidelines for pregnant women with suspected SARS-CoV-2 infection. Lancet Infect Dis. 2020. Mar 3, [Last accessed on March 16, 2020]. Available from: https://wwwthelancetcom/action/showPdfpii=S1473-3099%2820%2930157-2 . [DOI] [PMC free article] [PubMed]
- 19.Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: A preliminary analysis. [Last Accessed on March 30, 2020];AJR Am J Roentgenol. 2020 :1–6. doi: 10.2214/AJR.20.23072. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Ramsey PS, Ramin KD. Pneumonia in pregnancy. Obstet Gynecol Clin North Am. 2001;28:553–69. doi: 10.1016/s0889-8545(05)70217-5. [DOI] [PubMed] [Google Scholar]
- 21.Harris JW. Influenza occurring in pregnant women: a statistical study of thirteen hundred and fifty cases. J Am Med Assoc. 1919;72:978–80. [Google Scholar]
- 22.Greenberg M, Jacobziner H, Pakter J, Weisl BA. Maternal mortality in the epidemic of Asian influenza, New York City, 1957. Am J Obstet Gynecol. 1958;76:897–902. doi: 10.1016/0002-9378(58)90027-9. [DOI] [PubMed] [Google Scholar]
- 23.Knuttgen HG, Emerson K., Jr Physiological response to pregnancy at rest and during exercise. J Appl Physiol. 1974;36:549–53. doi: 10.1152/jappl.1974.36.5.549. [DOI] [PubMed] [Google Scholar]
- 24.Lederman MM. Cell-mediated immunity and pregnancy. Chest. 1984;86:6s–9s. doi: 10.1378/chest.86.3_supplement.6s. [DOI] [PubMed] [Google Scholar]
- 25.Alaily A, Carr K. Pulmonary ventilation in pregnancy. BJOG Int J Obstet Gynaecol. 1978;85:518–24. doi: 10.1111/j.1471-0528.1978.tb15626.x. [DOI] [PubMed] [Google Scholar]
- 26.WHO. [Last update on 2020 Feb 25]. Available from: https://wwwwhoint/emergencies/diseases/novel-coronavirus-2019/advice-for-public .
- 27.CDC. [Last Accessed on March 16, 2020]. Available from: https://wwwcdcgov/coronavirus/2019-ncov/hcp/guidance-prevent-spreadhtml .


