Abstract
Background
Sleep is a natural, restorative, physiological process that is characterized by perceptual disengagement from and unresponsiveness to whatever going around, which is reversible. Sleep quality refers to a sense of being rested and refreshed after waking up from sleep. People living with HIV/AIDS (PLWHA) are vulnerable to poor sleep quality as they suffer from social stigma and Anti-Retroviral drug side effects. The study aimed to examine the quality of sleep and its associated factors among people living with HIV/AIDS attending Anti-Retroviral Therapy (ART) clinic at Hawassa University comprehensive specialized hospital.
Method
Institutional based cross-sectional study was conducted among PLWHA attending ART clinic at Hawassa University comprehensive specialized hospital from May 1–30, 2019. A systematic random sampling technique was used to select an estimated 422 study participants and data was collected using interviewer-administered technique. Sleep Quality was assessed using the Pittsburgh Sleep Quality Index (PSQI). Data were entered and analyzed using SPSS 22 software. Bivariable and multivariable logistic regression model was fitted to identify factors associated with quality of sleep. An adjusted odds ratio with a 95% confidence interval was computed to determine the level of significance with P-value less than 0.05.
Result
Out of 422 respondents, 389 participated in the study giving a response rate of 92.1%. The prevalence of poor quality of sleep among study participants was found to be 57.6% (95% CI: 54.72, 60.48). 31.9% (124) and 30.6% (119) of study participants had anxiety and depression respectively. Being between the age of 55–64 years (AOR = 5.7, 95% CI (1.9, 17.8), Age ≥ 65 (AOR:6.6, 95% CI (1.2, 36.9), Monthly income <1656 Ethiopian Birr (ETB) (AOR = 2.17, 95% CI (1.06, 4.4), having anxiety (AOR = 4.4, 95% CI (2.12, 9.2), having depression (AOR = 4.97, 95% CI (2.28, 10) and poor social support (AOR = 2.9, 95% CI (1.16, 7.3) were factors associated with poor quality of sleep.
Conclusion
The prevalence of poor quality of sleep among PLWHA was significantly high. Average monthly income, age, anxiety, depression, and social support were found to be significantly associated with poor sleep quality. Health care professionals working at the ART clinic need to assess the sleep pattern of ART clients, give psychoeducation on the prevention and management of sleep pattern problems.
Background
Sleep is a natural, restorative, physiological process that is characterized by perceptual disengagement from and unresponsiveness to whatever going around, which must be reversible [1]. During sleep, most of the body’s systems are in an anabolic state, helping to restore the immune, nervous, skeletal and muscular systems, which are vital processes that maintain mood, memory and cognitive function, and play important roles in daily functions [2, 3].
Sleep quality refers to how long an individual sleeps each night and how well he/she sleeps. Also, it includes how difficult it is for an individual to fall asleep, remain slumbering, and how many times he/she wakes up during the night. Moreover, it is a sense of being rested and refreshed after waking up from sleep [4].
Having a good sleep quality is an indicator of wellbeing whereas poor sleep quality results in increased co-morbidity, mortality, health care costs and poor quality of life of PLWHA [5]. Furthermore, poor sleep quality can cause an individual to feel tired the next day and may even be associated with long term risk of Alzheimer’s disease [6].
Sleep disturbances impair the quality of life, cognitive function, and emotion of PLWHA that could lead to poor medication adherence [7]. It can induce various adverse outcomes in peoples living with HIV/AIDS (PLWHA), including diminished health-related quality of life, excessive day time sleepiness, and cognitive impairment [8]. In the HIV infected population, poor quality of sleep has been associated with, disease progression, side effects of medication, financial concerns, unemployment and inadequate knowledge about behaviors enhancing good sleep [9].
HIV/AIDS is a chronic, potentially life-threatening condition caused by the human immunodeficiency virus (HIV), which interferes with the body’s ability to fight against disease causing organisms [10]. It is one of the most devastating illnesses that human beings ever faced [11]. As of 2017, approximately 36.9 million peoples worldwide are living with HIV/AIDS. Sub-Saharan Africa is the most affected region, in 2017, an estimated 66% of new HIV infections occurred in this region [12]. Ethiopia is one of Sub-Saharan counties, reported a prevalence of 1.1% HIV/AIDS infection in 2016 among individuals aged between 15–49 [13].
In the United States of America, 50–70 million adults are suffering from sleeping problems [14]. Among them, insomnia and sleep apnea commonly dominate with a prevalence of 6%-10% and 10–25% respectively [15]. Sleep disturbances are thought to be common among HIV infected individuals in the US [16] and have a 40 to 70% prevalence of sleep disturbance and Patients with HIV were found to have a higher risk of sleep disturbances than the general population [17].
PLWHA are vulnerable to poor sleep quality as they suffer from the social stigma of the disease, unpleasant side effects of ARV medications including increased risk for metabolic syndromes [18]. Depression often considered as a logical outcome in peoples living with HIV/AIDS and consequently may lead to and exacerbates sleep disturbance [19]. Also, addictive drug use is associated with sleep disturbances in persons living with HIV/AIDS [20]. There is a controversy regarding the association of duration since HIV diagnosis with sleep quality, in which some studies state that short duration since diagnosis is negatively associated with sleep quality [17]; whereas others discussed that individuals with long durations since HIV status known are more likely to have diminished sleep quality [21, 22].
Despite all the above evidence in developed and middle-income countries, little is known in low-income countries, especially in Ethiopia. So, the current study tried to fill this gap and examined the prevalence and associated factors of poor quality of sleep among people living with HIV/AIDS attending ART clinic at Hawassa University Comprehensive Specialized Hospital.
Methods
Study design and setting
An institutional-based cross-sectional study was conducted to examine the prevalence and associated factors of poor quality of sleep among PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital (HUCSH) from May1-30, 2019. Hawassa University Comprehensive Specialized hospital is located in Hawassa city, SNNPR, which is 275 km far from Addis Ababa. Beyond other inpatient and outpatient medical services, the hospital provides ART services for PLWHA.
Population
All PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital were source population. PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital ART clinic during the data collection period were the study population. Individual ART client attending ART clinic at Hawassa University Comprehensive Specialized Hospital was the study unit.
PLWHA attending Hawassa University Comprehensive Specialized Hospital ART clinic with age 18 years and above were included in the study but those with a severe medical condition (unconscious or critically ill) and unable to communicate due to hearing difficulty were excluded from the study.
Sample size and sampling technique
The sample size was determined using a single population proportion formula considering assumption (Z = 1.96, d = 0.05, and P = 50%). Then, adding a 10% non-response rate, the final estimated sample size was 422. Among the total ART clients currently being enrolled in ART service, 422 study participants were selected through systematic random sampling technique using sampling fraction; K = 6. The sampling fraction (K) was obtained by dividing the total ART clients who have follow-up at Hawassa University comprehensive specialized hospital (n = 2533) by the sample size, 2533/422 which is 6. The first individual was selected using a lottery method, and the rest were selected at a regular interval (every 6th).
Measurements and data collection technique
Data were collected by four psychiatry nurses using interviewer administered technique. During data collection daily base supervision was conducted by one MSc psychiatry professional to check for completeness of data collection tool.
Sleep quality was assessed by using the Pittsburgh Sleep Quality Index (PSQI), a 19-item self-rated scale which examined Sleep Quality and disturbances over a 1 month time interval. The tool mainly addresses seven sleep components: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of hypnotics, and daytime dysfunction during the last month. The total PSQI score is then calculated by summing-up the seven component scores, giving an overall score ranging from 0 to 21. The score >5 points indicates poor sleep quality [23]. For the current study the internal consistency of PSQI was found Cronbach’s alpha α = 0.76.
The hospital anxiety and depression scale (HADS) was used to assess anxiety and depression. It has been validated in Ethiopia and its internal consistency was α = 0.78 for anxiety, α = 0.76 for depression subscales and α = 0.87 for full scale. It has two subscales: the anxiety subscale (HADS-A) and the depression subscale (HADS-D). Each subscale contains seven items, giving a total of 14 items in the HADS. It has cutoff point ≥ 8 for each subscale suggestive of depression and anxiety [24]. For the current study the internal consistency was Cronbach’s alpha α = 0.81 for full scale.
Social support was measured by using 3 items Oslo social support scale (OSS-3) which is classified as poor social support (3–8 OSS score), intermediate social support (9–11 OSS score), and strong social support (12–14 OSS score) [25]. For the current study the internal consistency of OSS-3 was Cronbach’s alpha α = 0.73. Current substance use: assessing the use of any substance (alcohol, tobacco, cigarette and other) in the last 3 months. Ever use of the substance was assessed if a study participant used any substance (alcohol, tobacco, cigarette and other) at least once in his lifetime.
Monthly income was categorized using the 2015 World Bank poverty line classification. World Bank re-established the international poverty line; from 1.25 US $- 1.9 US $ (1.9*29.06*30 = 1656 Ethiopian birr (ETB)) monthly income considered as the poverty line. Below poverty line: < 1656 ETB and above poverty line: ≥ 1656 ETB [26].
Variables and data analysis
The dependent variable was quality of sleep (poor/good) and the independent variables were sociodemographic factors (age, sex, marital status, occupation, religion, educational status, income), clinical factors (CD4 count, WHO clinical stage of HIV/AIDS, duration since HIV/AIDS diagnosis, ART drug type, presence of co-morbid medical illness), Substance use (ever use/current use), psychosocial factors (depression, anxiety, social support) and environmental factors (noise disturbance).
Data entry and analysis was conducted using SPSS 22 software. Bivariable logistic regression analysis was conducted to identify independent factors associated with poor quality of sleep. Possible confounding (important variable which have a hidden effect on the outcome) variables were entered into a multivariable logistic regression model to identify the association of each independent variable with poor quality of sleep. In the final model, variables with a p-value of less than 0.05 declared as statistically significant, and AOR with 95% CI was calculated to determine the strength of association. Model fitness was checked using the Hosmer and Lemeshow test, and it was found to be 0.71. Multi-collinearity was checked by the variance inflation factor (VIF) and tolerance.
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board (IRB) of Hawassa University, college of medicine and health sciences. The data collectors clearly explained the aim of the study for every study participant. Written consent was sought from individual ART client who agreed to participate. Participants who can’t read and write gave a fingerprint to indicate consent. Each participant was informed that they have the right to refuse or discontinue participation at any time they want. All participants were randomly selected without any discrimination on any ground. Filled out questionnaires were carefully handled, and all access to results was kept strictly within the members of the research team.
Results
Socio-demographic characteristics
Out of 422 estimated study participants, 389 were included in the analysis, making a response rate of 92.2%. The mean age of respondents was 38.2 (±9.7) years. From the total study participants, 231 (59.4%) were females and 261 (67%) were married. The mean estimated monthly income of patients was 1612.7 (±1349) Ethiopian birr (ETB) (Table 1).
Table 1. Socio-demographic characteristics of PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital, SNNPR, Ethiopia, 2019 (n = 389).
| Variable | Category | Frequency (%) |
|---|---|---|
| Age | 18–24 | 53 (13.6) |
| 25–54 | 233 (59.9) | |
| 55–64 | 85(21.9) | |
| >65 | 18(4.6) | |
| Sex | Male | 158 (40.6) |
| Female | 231 (59.4) | |
| Religion | Orthodox | 177 (45.5) |
| Protestant | 155 (39.8) | |
| Muslim | 51 (13.1) | |
| Others | 6 (1.5) | |
| Marital status | Married | 261 (67) |
| Single | 46 (11.8) | |
| Divorced | 38 (9.8) | |
| Widowed | 44 (11.3) | |
| Educational status | Unable to read and write | 49 (12.6) |
| Primary | 164 (42.2) | |
| Secondary | 110 (28.3) | |
| College/University | 66 (17) | |
| Occupation | Civil servant | 58 (14.9) |
| Merchant | 109 (28) | |
| Day worker | 107 (27.5) | |
| Student | 16 (4.1) | |
| House wife | 66 (17) | |
| Unemployed | 23 (5.9) | |
| Others | 10 (2.6) | |
| Monthly income | <1656ETB | 245 (63) |
| ≥1656 ETB | 144 (37) |
Clinical characteristics
Out of 389 respondents, 267 (68.6%) were in stage I for WHO clinical staging. Regarding the time since HIV diagnosis, 314 (80.7%) have a duration above 1 year and 259 (66.6%) of respondents have CD4 count ≥500 cells/ml. 209 (53.7%) study participants used EFV based combination ART drug type, and 106(27.2%) have a co-morbid medical illness (Table 2).
Table 2. Clinical characteristics of PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital, SNNPR, Ethiopia, 2019 (n = 389).
| Clinical factors | Frequency and (%) |
|---|---|
| WHO clinical stages | |
| Stage I | 267 (68.6) |
| Stage II | 96 (24.7) |
| Stage III | 20 (5.1) |
| Stage IV | 6 (1.5) |
| Time since HIV diagnosis | |
| ≤1 year | 75 (19.3) |
| >1 year | 314 (80.7) |
| CD4 count | |
| <200 cells/ml | 11 (2.8) |
| 200–499 cells/ml | 119 (30.6) |
| ≥500 cells/ml | 259 (66.6) |
| ART drug Type | |
| EFV-based | 209 (53.7) |
| Non-EFV | 180 (46.3) |
| Presence of any comorbid chronic medical illness (DM, Ca, HTN or other) | |
| No | 283 (72.8) |
| Yes | 106 (27.2) |
Abbreviation: DM: Diabetes Mellitus, Ca: Cancer, HTN: Hypertension, ART: Antiretroviral Therapy, EFV: Efavirenz
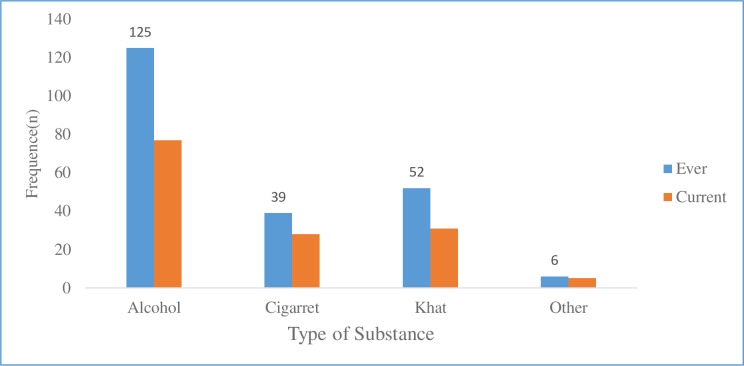
Substance use
Out of 389 respondents, 156 (40.1%) and 102 (26.2%) used at least one substance in their lifetime and within the last 3 months respectively (Fig 1).
Fig 1. Types of substances used by study participants attending ART clinic at HUCSH, SNNPR, Ethiopia, 2019 (n = 389).
Psychosocial and environmental factors
Based on the Hospital Anxiety and Depression Scale, 124(31.9%) and 119(30.6%) of respondents had anxiety and depression respectively. 167(42.9%) of participants received poor social support. Out of the total respondents, 66(17%) complained about the experience of noise disturbance during their sleeping time.
Quality of sleep
The prevalence of poor quality of sleep among PLWHA was 57.6%. The mean total PSQI score of individuals with poor quality of sleep was 8.43(±2.74) as compared to 3.21 (±1.47) of those with good quality of sleep (S1 Table).
Factors associated with poor quality of sleep
From the total variables included in the multivariable logistic regression analysis, five variables were found to be statistically significant (P<0.05). Accordingly, age (55–64 and >64), average monthly income (<1656 ETB), having anxiety, having depression and poor social support were found to be significantly associated with poor sleep quality (Table 3).
Table 3. Bivariable and multivariable logistic regression of factors associated with poor quality of sleep among PLWHA attending ART clinic at Hawassa University Comprehensive Specialized Hospital, SNNPR, Ethiopia, 2019 (n = 389).
| Variable | Category | Poor Sleep Quality | COR (95%CI) | AOR (95%CI) | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age | 18–24 | 23 | 30 | 1 | 1 |
| 25–54 | 114 | 119 | 1.25 (0.69,2.3) | 1.4 (0.6, 3.4) | |
| 55–64 | 72 | 13 | 7.2 (3.2, 16.1) | 5.7(1.9, 17.8)* | |
| ≥ 65 | 15 | 3 | 6.5(1.6, 25.2) | 6.6(1.2, 36.9)* | |
| Marital status | Married | 142 | 121 | 1 | 1 |
| Single | 29 | 15 | 1.6(0.86, 3.27) | 1.6 (0.5, 5.0) | |
| Divorced | 26 | 12 | 2.1(1.01, 4.46) | 1.1(0.4, 3.0) | |
| Widowed | 27 | 17 | 1.37(0.7, 2.64) | 0.9(0.34, 2.2) | |
| Educational status | Unable to read & write | 36 | 13 | 2.8(1.25,6.14) | 0.5(0.13, 1.6) |
| Primary | 101 | 63 | 1.56(0.8,2.78) | 0.6(0.26, 1.7) | |
| Secondary | 54 | 56 | 1.0(0.54,1.84) | 0.8(0.35, 2.2) | |
| College/university | 33 | 33 | 1 | 1 | |
| Occupation | Civil servant | 19 | 39 | 1 | 1 |
| Merchant | 59 | 50 | 2.4 (1.24, 4.7) | 2.7(1.01, 7.3) | |
| Day worker | 71 | 34 | 4.29(2.16,8.5) | 1.83(0.57,5.8) | |
| Student | 11 | 5 | 4.5(1.37,14.9) | 2.28(0.32,16.2) | |
| House wife | 36 | 30 | 2.46 (1.2, 5.1) | 1.27(0.37,4.3) | |
| Unemployed | 19 | 6 | 6.5 (2.2, 18.9) | 3.4 (0.9, 13.2) | |
| Others | 9 | 1 | 18.5(2.1,25.6) | 5.6 (0.3, 9.6) | |
| Monthly income | <1656 ETB | 163 | 82 | 2.7(1.77,4.13) | 2.17(1.06,4.4)* |
| ≥1656 ETB | 61 | 83 | 1 | 1 | |
| Anxiety | No | 116 | 149 | 1 | 1 |
| Yes | 108 | 16 | 8.6(4.86,15.4) | 4.4(2.12, 9.2)** | |
| Depression | No | 119 | 151 | 1 | 1 |
| Yes | 105 | 14 | 9.5(5.19,17.4) | 4.97 (2.28, 10)** | |
| WHO stages of HIV/AIDS | Stage I | 131 | 136 | 1 | 1 |
| Stage II | 74 | 22 | 3.49(2.05,5.9) | 0.77(0.18, 3.4) | |
| Stage III & IV | 19 | 7 | 2.82(1.14, 6.9) | 0.17(0.03, 1.2) | |
| Duration since HIV diagnosis | ≤1 year | 39 | 36 | 1 | 1 |
| >1 year | 185 | 129 | 1.41(0.85, 2.3) | 0.86(0.43, 1.7) | |
| CD4 count | <200 cells/ml | 9 | 2 | 5.1(1.07,23.8) | 1.9 (0.22, 18.2) |
| 200–499 cells /ml | 93 | 26 | 4.01(2.44, 6.6) | 3.0 (0.7, 13.2) | |
| ≥500 cells/ml | 122 | 137 | 1 | 1 | |
| ART drug type | EFV-based | 136 | 73 | 1.86 (1.24,2.8) | 1.7 (0.9, 3.04) |
| Non EFV-based | 88 | 92 | 1 | 1 | |
| Chronic medical illness | No | 147 | 136 | 1 | 1 |
| Yes | 77 | 29 | 2.45(1.5, 3.99) | 1.6 (0.8, 3.3) | |
| Lifetime substance use | No | 120 | 113 | 1 | 1 |
| Yes | 104 | 52 | 1.88(1.2, 2.87) | 1.3(0.6, 2.8) | |
| Current substance use | No | 151 | 136 | 1 | 1 |
| Yes | 73 | 29 | 2.27(1.4, 3.7) | 1.03(0.4, 2.6) | |
| Social support | Poor | 127 | 40 | 5.8(3.02,11.3) | 2.9(1.16, 7.3)* |
| Moderate | 77 | 90 | 1.57(0.8, 2.97) | 1.2(0.5, 2.8) | |
| Good | 19 | 35 | 1 | 1 | |
*Significant association (P-value <0.05)
**Significant association (P-value <0.01), Abbreviation: COR: Crudes Odds Ratio, AOR: Adjusted Odds Ratio, CI: Confidence Interval, ART: Anti-Retroviral Therapy, ETB: Ethiopian Birr
Discussion
In the current study, the prevalence of poor sleep quality was 57.6% (95% CI: 54.72, 60.48). The result is somewhat in agreement with the result reported from Mexico which is 58.9% [22]. However, the prevalence in the current study was lower than the study conducted in Nigeria which is 59.3% [17]. The finding in the current study was higher than the result reported from South Africa which showed that the prevalence of poor sleep quality was 52% [27], 46.2% in University of Calabar teaching Hospital, South Nigeria [28], Iran 47.5% [29], China 43.1% [30], Brazil 46.7% [31], France 47% [21], Southern US 40% [32], John Hopkins Medical Institution USA 56% [33], another study in USA 46.1% [16] and Taiwan 27.4% [34]. These discrepancies might be due to various factors including differences in the geographical area, socio-cultural variation, characteristics of study participants and the inclusion and exclusion criteria used.
An individual living with HIV/AIDS age between 55–64 years was 5.7 times more likely to experience poor sleep quality compared to the younger (18–24 years) individual. Also, study participants with age ≥ 65 were 6.6 times more likely to experience poor quality of sleep compared with those with younger age groups. This implication might be related to various factors including age-related immunity deterioration, dropping of growth hormone levels, which is known to facilitate deep sleep, psychological and socio-economic factors including retirement from jobs result in a poor quality of sleep. Also, as an individual gets older, the neurological receptors that connect with sleep signaling chemicals weaken, which results in the brain face a long time figuring out when individuals are tired [35]. The current finding was consistent with the study conducted in China [36].
Individuals below the poverty line (<1656 ETB) were 2 times more likely to experience poor quality of sleep compared with those above poverty lines. This might be related to some negative emotions posed by survival pressure over low-income earners might result in a poor quality of sleep. Also, individuals with higher socioeconomic status have been hypothesized to get positive social, psychological, and economic skills that protect against the effect of hardship [37] which would protect sleep problems. This finding is in agreement with the study reported in China [36].
Our study also revealed that the presence of both anxiety and depression increases the possibility of experiencing poor quality of sleep compared with their counterpart. This might be due to the linkages between sleep, emotional regulation and alteration in the Hypothalamic-pituitary-adrenal axis implication of psychopathology and sleep-wake cycle. Also, the presence of insomnia symptoms was higher among individuals who have anxiety and depression which results in poor sleep quality [38]. The result is in agreement with the studies conducted in the USA [16], Mexico [21] and Iran [39].
Lastly, our study result suggested, individuals who received poor social support to be 2.9 times more likely to develop poor quality of sleep. Social support is thought to promote sleep quality by providing a safe context in which close family or friends protect sleepers from enemies or other threats [40]. The current finding was in line with the study conducted in Mexico [21].
Limitation of the study
One limitation of our study is that it’s cross-sectional nature, which is weak to evaluate the cause-effect relationship. Lack of a control group limited our study’s ability to characterize the sleep pattern of people with HIV/AIDS in contrast to the general population. Also, since only 1.5% of the samples in the current study were classified as stage IV, the finding can’t be generalized for study participants at severe HIV stage.
Conclusion
The prevalence of poor quality of sleep among PLWHA was high (57.6%), which indicates desperate life of individuals living with HIV/AIDS in Ethiopia. Average monthly income, age, anxiety, depression, and social support were found to be significantly associated with poor sleep quality. Health care professionals working at the ART clinic need to regularly assess the sleep pattern of ART clients, give psychoeducation on prevention and management of sleep pattern problems. Special consideration has to be given to those with age >55 years, having poor social support, having depression and anxiety, and individuals living below the poverty line.
Supporting information
(DOCX)
Acknowledgments
We would like to thank study participants, data collectors, and supervisors for their unreserved contribution during data collection. Also, we would like to forward our gratitude to Hawassa University comprehensive specialized hospital ART clinic health care providers for their genuine support during data collection.
List of abbreviations
- ART
Anti Retro-viral Therapy
- CBE
Community Based Education
- COP/ROP
Country/Regional Operational Plan
- EFV
Efavirenz
- HAART
Highly Active Anti-retroviral Therapy
- HADS-A
Hospital Anxiety and Depression Scale-anxiety component
- HADS-D
Hospital Anxiety and Depression Scale-depression component
- HIV/AIDS
Human immunodeficiency virus or Acquired Immune deficiency syndrome
- HUCSH
Hawassa University Comprehensive Specialized Hospital
- NVP
Nevirapine
- OSS-3
3 Item Oslo social support scale
- PLWHA
People Living With HIV/AIDS
- PSQI
Pittsburgh Sleep Quality Index
- SNNPR
Southern Nations, Nationalities and Peoples’ Region
- SPSS
Statistical Package for Social Sciences
- UNAIDS
United Nations program on HIV/AIDS
- USA
United States of America
- WHO
World Health Organization
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Carckadon MA, Dement WC (2005). Monitoring and Staging of human sleep. Principles and practices of sleep medicine. 10.1016/s1389-9457(05)80005-x [DOI] [Google Scholar]
- 2.Barlow DH (2014). Clinical handbook of psychological disorders: A step-by-step treatment manual. Guilford publications [Google Scholar]
- 3.National sleep foundation (2006) Sleep-wake cycle: its physiology and impact on health.
- 4.Christopher M. Barnes and Christopher Drake (2015) Prioritizing Sleep Health: Public health policy recommendations. 10 (6): 733–737 [DOI] [PubMed] [Google Scholar]
- 5.Garbarino S., Lanteri P, Durando P., Magnavita N., &Sannita W. G. (2016): Co-Morbidity, Mortality, Quality of life and the healthcare/welfare/social costs of disordered sleep: A Rapid Review. International Journal of Environmental Research and Public Health, 13(8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National sleep foundation (2019) Sleep and Alzheimer’s disease: more evidence on their relationship. Cognitive Vitality
- 7.Babson KA, Heinz AJ, Bonn-Miller MO (2013): HIV Meditation adherence and HIV symptom severity: The roles of sleep quality and memory. AIDS patient care STDs. 27(10):544–552 10.1089/apc.2013.0221 [DOI] [PubMed] [Google Scholar]
- 8.Tedaldi E. M, Minniti N. L., & Fischer T. (2015): HIV-associated neuro-cognitive disorders: the relationship of HIV infection with physical and social co-morbidities. BioMed Research International, 641913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irwin M. R., Olmstead R., & Carroll J. E. (2016): Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biological Psychiatry, 80(1), 40–52 10.1016/j.biopsych.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnston L, O'Malley P, Bachman J, Schulenberg J, Patrick M, Miech R. (2017) HIV/AIDS: Risk & protective behaviors among adults ages 21 to 40 in the USA [Google Scholar]
- 11.Bhatia M.S. and SahilMunjal (2014): Prevalence of depression in people living with HIV/AIDS undergoing ART and factors associated with it. Journal of clinical and Diagnostic Research 8 (10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.UNAIDS (2018): Global HIV &AIDS statistics: 2018 fact sheet
- 13.Country/Regional Operational Plan (2017): Strategic Direction Summary. Ethiopia
- 14.Centers for Disease Control and Prevention (2015): Insufficient sleep is a public health problem. http://www.cdc.gov/features/dsleep/
- 15.Chai-Coetzer CL, Antic NA, McEvoy RD (2015): Identifying and managing sleep disorders in primary care. Lancet Respir Med.3:337–339 10.1016/S2213-2600(15)00141-1 [DOI] [PubMed] [Google Scholar]
- 16.Crum-cianflone NF, Roediger MP, Moore DJ, Hale B, Weintrob A, Ganesan A, et al. (2012). Prevalence and factors associated with sleep disturbances among early-treated HIV-infected persons. Clinical infectious diseases, 54(10):1485–1494 10.1093/cid/cis192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oshinaike O., Akinbami A., Ojelabi O., Dada A., Dosunmu A., & John Olabode S. (2014). Quality of sleep in an HIV population on Antiretroviral therapy at an urban tertiary centre in Lagos, Nigeria. Neurology Research International, 2014, 298703 10.1155/2014/298703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Araújo Márcio M, Uchôa Lilian Raquel A1, Oliveira Maria Da S, De Araújo Da Silva Antonio U,.et al. (2018). Poor Sleep Quality in Persons Living with HIV: A Systematic Review and Meta-Analysis. Research & Reviews: Journal of Nursing and Health Sciences. 4(2), 28–32. [Google Scholar]
- 19.Bernard Charlotte, Dabis Francois and de RE keneire Nathalie, (2017) Prevalence and factors associated with depression in people living with HIV in Sub-Saharan Africa: A systematic review and meta-analysis. Peer-reviewed, Open Access Journal 12(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahoney J. J., De La Garza R., Jackson B. J., Verrico C. D., Ho A., Iqbal T., et al. (2014). The relationship between sleep and drug use characteristics in participants with cocaine or methamphetamine use disorders. Psychiatry Research, 219(2), 367–37 10.1016/j.psychres.2014.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allavena C, Guimard, Billaud E, de la Tullaye S, Reliquet V, Pineau S, et al. (2016). Prevalence and risk factors of sleep disturbance in a large HIV-infected adult population. AIDS and Behavior, 20(2), 339–344. 10.1007/s10461-015-1160-5 [DOI] [PubMed] [Google Scholar]
- 22.Evelyn E, Maria candela I, Ana Fresan O, Gustavo Reyes. (2018) Factors associated with poor sleep quality among HIV-positive individuals in Mexico. [Google Scholar]
- 23.Buysse D.J., Reynolds III, C.F., Monk T.H., Berman S.R., & Kupfer D.J (1989): Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Journal of Psychiatric Research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- 24.Reda AA. (2011) Reliability and validity of Ethiopian version of hospital anxiety and depression scale in HIV infected patients. PLoS One. 6 (1): e16049 10.1371/journal.pone.0016049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalgard O (2009). social support: consequences for individual and society. EUPHIX
- 26.https://data.worldbank.org
- 27.Redman Kirsten (2016) Sleep quality and immune changes in HIV positive people in the first six months of starting Highly Active Antiretroviral Therapy. Wits Institutional Repository environment on Space [Google Scholar]
- 28.Bisong E: Predictors of sleep disorder among HIV out-patients in a Tertiary Hospital. Recent Adv Biol Med 2017, 3(2017): 2747. [Google Scholar]
- 29.Dabaghzadeh F, Khalili H, Ghaeli P, Alimadadi A (2013). Sleep quality and its correlates in HIV positive patients who are candidates for initiation of antiretroviral therapy. Iranian Journal of Psychiatry, 8(4), 160–164. [PMC free article] [PubMed] [Google Scholar]
- 30.Huang X., Li H., Meyers K., Xia W., Meng Z., Li C., et al. (2017). Burden of sleep disturbances and associated risk factors: A cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Scientific Reports, 7(1), 3657 10.1038/s41598-017-03968-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferraira LTK, Coelim MF (2012). Sleep quality in HIV-Positive Outpatients. Revista da Escola de Enfermagem da USP 46(4): 890–896. [DOI] [PubMed] [Google Scholar]
- 32.McDaniel Janelle (2011). Sleep quality and habits of adults with the Human Immunodeficiency Virus [Google Scholar]
- 33.Gamaldo CE, Gamaldo A, Creighton J, Salas RE, Selnes OA, David PM, et al. (2013). Sleep, function and HIV: A multi-method assessment. AIDS and behavior 17(8):2808–2815 10.1007/s10461-012-0401-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen YC, Lin CY, Strong C, et al. Sleep disturbances at the time of a new diagnosis: a comparative study of human immunodeficiency virus patients, cancer patients, and general population controls. Sleep Med. 2017;36:38‐43. 10.1016/j.sleep.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 35.Does It Seem Harder to Sleep as You Age? Sleep.org: www.sleep.org › articles › sleep-challenges-getting-older.
- 36.Wu Wenwen, Wang Wenru, Dong Zhuangzhuang, Xie Yaofei, Gu Yaohua, Zhang Yuting, et al. (2018): Sleep quality and Its associated factors among Low-income Adults in a Rural Area of China. International Journal of Environmental Research and Public Research, 15(9):2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992; 82:816–820. 10.2105/ajph.82.6.816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985; 42(3):225–232. 10.1001/archpsyc.1985.01790260019002 [DOI] [PubMed] [Google Scholar]
- 39.Afkham Ebrahimi Azizeh, Maryam Rasoulian, Taherifar Zahra and Zare Maryam (2010): The impact of anxiety on sleep: Medical Journal of Islamic Republic of Iran. 23(4), 144–188. [Google Scholar]
- 40.Dahl RE., & El-Sheikh M. (2007). Considering sleep in a family context: Introduction to the special issue. Journal of Family Psychology, 21(1), 1–3. 10.1037/0893-3200.21.1.1 [DOI] [PubMed] [Google Scholar]