Abstract
Schizophrenia is a debilitating disorder affecting just under 1% of the population. While the symptoms of this disorder do not appear until late adolescence, pathological alterations likely occur earlier, during development in utero. While there is an increasing literature examining transcriptome alterations in patients, it is not possible to examine the changes in gene expression that occur during development in humans that will develop schizophrenia. Here we utilize three distinct rodent developmental disruption models of schizophrenia to examine potential overlapping alterations in the transcriptome, with a specific focus on markers of interneuron development. Specifically, we administered either methylazoxymethanol acetate (MAM), Polyinosinic:polycytidylic acid (Poly I:C), or chronic protein malnutrition, on GD 17 and examined mRNA expression in the developing hippocampus of the offspring 18 hours later. Here, we report alterations in gene expression that may contribute to the pathophysiology of schizophrenia, including significant alterations in interneuron development and ribosome function.
Introduction
Schizophrenia is a debilitating psychiatric disorder that affects just under 1% of the population[1]. It is characterized by positive symptoms, such as delusions and hallucinations; negative symptoms, such as blunted affect and social avoidance; and cognitive symptoms, including disruptions in working memory and cognitive inflexibility. As early as the 1980’s, it was proposed that schizophrenia was a neurodevelopmental disorder[2,3]. Evidence for this theory comes from the observation that prenatal complications such as maternal infection[4–8] and famine[9–13] significantly increase the risk of developing psychosis; and postmortem studies reveal neuroanatomical alterations indicative of abnormal neuronal development (i.e. heterotopias[14,15]). Further, many of the genes implicated in schizophrenia have been associated with neurodevelopmental processes[16,17] and the etiology of schizophrenia overlaps with the etiology of other neurodevelopmental disorders, like autism[18].
Recent work has demonstrated a key role for the hippocampus in the pathology of schizophrenia. In humans, anatomical and physiological changes are consistently observed in the hippocampus. Specifically, using imaging approaches, an increase in hippocampal activity at rest has been observed in schizophrenia patients[19–22]. This increase in hippocampal activity has been correlated with the severity of positive symptoms[23], suggesting that aberrant hippocampal activity may be a key site of pathology in schizophrenia. Indeed, we have previously used rodent models to demonstrate that aberrant dopamine system function and behavioral correlates of positive, negative and cognitive symptoms of schizophrenia are directly attributable to a pathological increase in hippocampal activity[24,25].
This increase in hippocampal activity is thought to be caused by a loss of inhibitory interneuron function. In schizophrenia patients, reductions in specific interneuron subtypes have been observed in the hippocampus[26,27], and work in our lab (and others) has demonstrated that disrupting interneuron function can induce schizophrenia-like deficits in behavior[28,29]. Further, restoring interneuron function in a rodent model of schizophrenia was able to alleviate schizophrenia-like deficits[30,31]. However, these disruptions in hippocampal and interneuron function have all been observed in schizophrenia patients after the first episode of psychosis or in the prodromal period. Due to the developmental nature of the disorder, it is important to identify the neurobiological changes that occur during gestation. Therefore, we began these studies with the a priori hypothesis that schizophrenia-like deficits are caused by disruptions in interneuron development and migration. This hypothesis could be tested by qPCR to measure the expression of a limited number of genes involved in interneuron development and migration. However, recent technological advances have made RNA Sequencing more feasible. Therefore, in the current experiments, we use RNA Sequencing to identify changes across the entire transcriptome to determine if development disruptions affect interneuron development as well as other neural pathways.
While there are limitations to the use of individual rodent models to parallel human schizophrenia, the examination of similarities across a number of diverse models can provide critical information about alterations that may contribute to schizophrenia. Therefore, in the current experiments, we utilize three validated developmental disruption models of schizophrenia, induced by the administration of methylazoxymethanol acetate (MAM) [32], Polyinosinic:polycytidylic acid (Poly I:C) [33], or protein malnutrition[34], to examine potential overlapping alterations in the hippocampal transcriptome during embryonic development.
Materials and methods
All experiments were performed in accordance with the guidelines outlined in the USPH Guide for the Care and Use of Laboratory Animals and were approved by the Institutional Animal Care and Use Committee of the University of Texas Health Science Center at San Antonio.
Rodent models
Timed pregnant female Sprague-Dawley rats were obtained from Envigo on gestational day 11. Either polyinosine:cytosine (Poly I:C, 7.5 mg/kg, i.p), methylazoxymethanol acetate (MAM: 22mg/kg, i.p.) or saline were administered on gestational day 17. For maternal protein malnutrition, pregnant rats had access to a low protein diet ad libitum (Envigo: TD.90016) containing 6.1% protein, 75.6% carbohydrate and 5.5% fat (3.8Kcal/g) from GD11-GD18. Control rats were fed an isocaloric diet of 20.3% protein, 61.6% carbohydrate and 5.5% fat (3.8Kcal/g: Envigo: TD.91352) from GD11-GD18. Pregnant rats were sacrificed on GD18 (18 hours following drug administration), three pups per mom were removed and the developing neocortex and hippocampus (Fig 1) were dissected on ice and frozen. Experiments included pups from multiple (two) litters for a total of 6 pups per group.
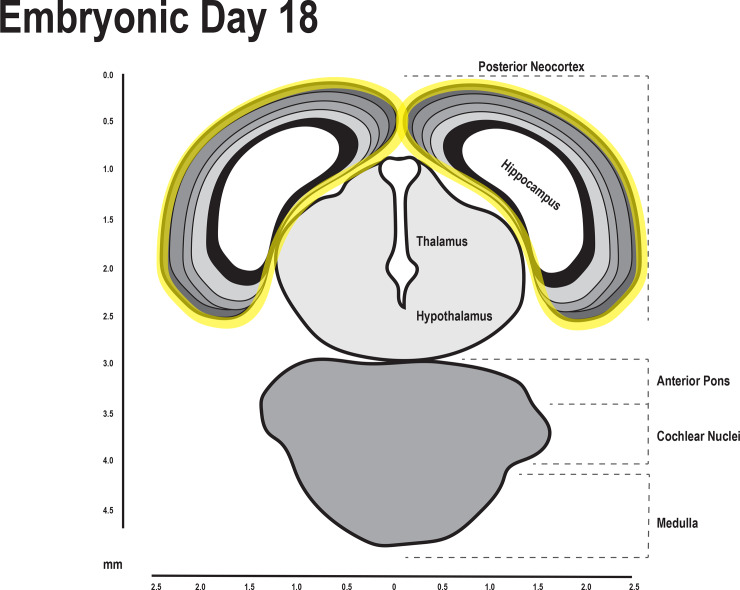
Fig 1. The hippocampus and neocortex was dissected for RNA sequencing.
Diagram of the fetal brain on embryonic day 18. The hippocampal and neocortical regions that were dissected are outlined in yellow[35].
RNA sequencing
RNA was extracted using the Qiagen AllPrep kit. Briefly, 17-75mg of tissue were homogenized in 600–2,400ul RLT buffer, and then processed through the AllPrep kit following manufacturer’s instructions. RNA samples were then DNase treated using the TurboDNA-free kit (Thermo Fisher Scientific) and cleaned with the Zymo RNA Clean and Concentrator kit. 250ng of RNA underwent cDNA library preparation using the Illumina TruSeq Stranded mRNA kit, followed by cluster generation and sequencing (2x100bp paired end read) on the Illumina HiSeq 2500.
In Partek Flow, input paired fastq files were trimmed by quality at both ends using phred 30 and minimum read length of 25 as cutoffs (Trim Bases tool). Quality reads were aligned to the RefSeq rn6 genome (Rattus norvegicus) with the STAR v2.4.1d aligner using default parameters for a mammalian genome. Aligned reads were quantified (Quantify to Annotation Model Partek E/M tool) against RefSeq rn6 Transcripts 80 (2017-02-06) and resulting counts were normalized by sample to TPM (Total per million) with an offset of 0.0001 (Normalize Counts tool). Normalized reads were used for GSA (Gene Specific Analysis tool) of differential expression at gene and transcript levels. For differential expression analysis, genes were included if the lowest average coverage (normalized read count) by treatment group was greater than 1.0 and if they were within the estimation reliability cutoff defined by the Partek software. In total, 5,212 genes were included for differential expression analysis.
Quantitative polymerase chain reaction
300 ng RNA was converted to cDNA using the Applied Biosystems High Capacity Reverse Transcription Kit. Real-time quantification of diluted cDNA was performed in triplicate reactions containing sample (10 ng), Applied Biosystems TaqMan Universal PCR Master Mix (20X), and TaqMan Gene Expression Assay (20X) on a BioRad CFX384 Real Time System. Cycling Conditions consisted of one cycle at 50°C for 2 min, one cycle at 95°C for 10 min, followed by 50 cycles of denaturation (95°C for 15 sec) and elongation (60°C for 1 min). The relative gene expression was calculated using the 2-ΔΔCT method. The following TaqMan Gene Expression Assays were used: Dlx1 (Rn01513884), Dlx5 (Rn00564070), Lhx6 (Rn1438474), Nkx2.1 (Rn01512482), and GAPDH (Rn01775763).
Analysis
The RNA Sequencing data were analyzed using Advaita Bioinformatics iPathwayGuide (http://www.advaitabio.com/ipathwayguide) to define significantly affected pathways, biological processes, molecular interactions, etc. Differences between each treatment group (Poly I:C, MAM and low protein) and control were analyzed individually (S1 Table), followed by a meta-analysis of these data in order to examine potential overlapping or consistent effects of these discrete prenatal manipulations. The qPCR data was analyzed using One-way ANOVAs followed by the Holm-Sidak post-hoc test.
Results
All RNA Sequencing data is freely available online at the GEO (Gene Expression Omnibus) public functional genomics data repository (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE149828).
MAM
In this experiment, 599 differentially expressed genes were identified out of a total of 5211 genes with measured expression (S1 Table). These were obtained using a threshold of 0.05 for statistical significance (p-value). These data were analyzed in the context of pathways obtained from the Kyoto Encyclopedia of Genes and Genomes (KEGG) database (Release 81.0+/01-20, Jan 17)[36,37], gene ontologies from the Gene Ontology Consortium database (2016-Sep26) [38], predicted miRNAs from the miRBase (Release 21) and MICROCOSM (Microsm version:v5) databases[39–44], and diseases from the KEGG database (Release 81.0+/01-20, Jan 17)[36,37]. In summary, 28 pathways were found to be significantly impacted (S1 Table). In addition, 503 Gene Ontology (GO) terms, 15 miRNAs (predicted based on targets), and 3 diseases were found to be significantly enriched based on uncorrected p-values (S1 Table).
Poly I:C
In this experiment, 532 differentially expressed genes were identified out of a total of 5211 genes with measured expression (S1 Table). These were obtained using a threshold of 0.05 for statistical significance (p-value) and a log fold change of expression with absolute value of at least 0.6. We identified 22 pathways, 527 Gene Ontology (GO) terms, 52 miRNAs, and 5 diseases that were significantly enriched based on uncorrected p-values (S1 Table).
Protein malnutrition
In this experiment, 440 differentially expressed genes were identified out of a total of 5211 genes with measured expression (S1 Table). These were obtained using a threshold of 0.05 for statistical significance (p-value) and a log fold change of expression with absolute value of at least 0.6. We identified 21 pathways, 476 Gene Ontology (GO) terms, 29 miRNAs, and 7 diseases that were significantly enriched based on uncorrected p-values (S1 Table).
Meta-analysis
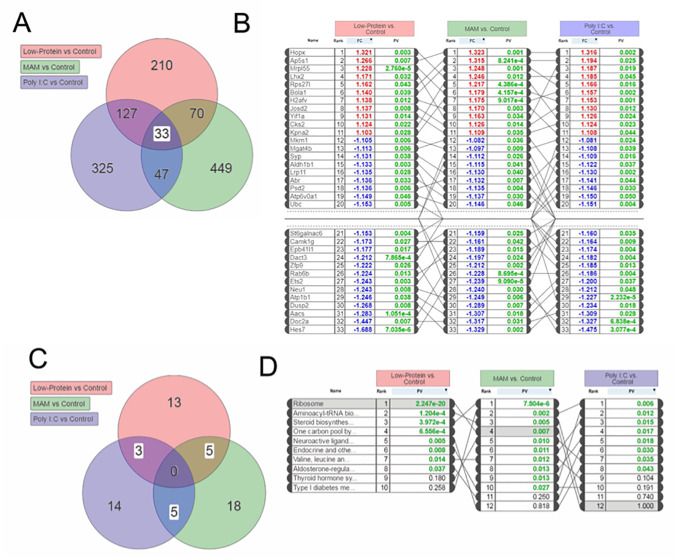
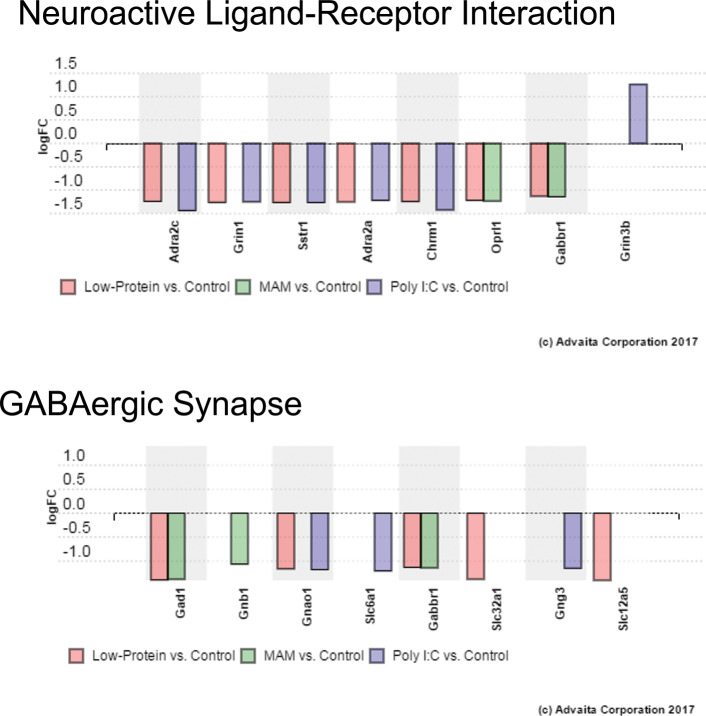
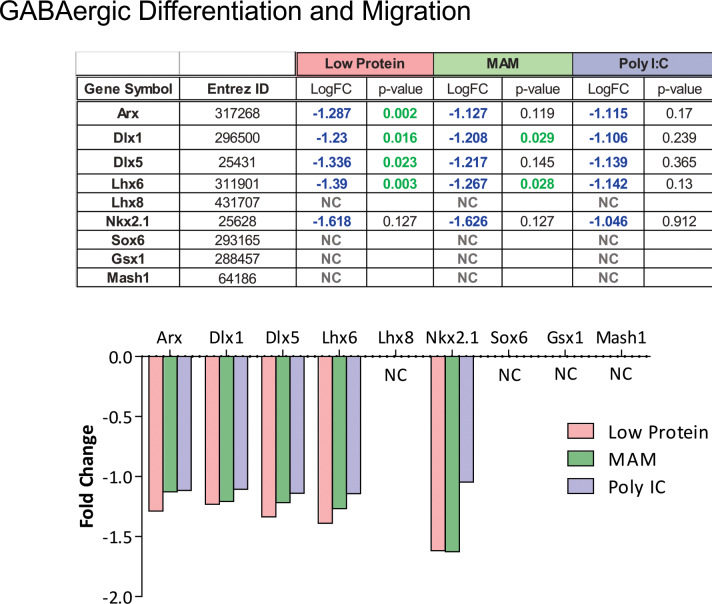
To examine potential overlapping alterations in the transcriptome that could underlie the common neurophysiological and behavioral alterations observed in these rodent models, we performed a meta-analysis of these data using iPathway Guide. Of the differentially expressed genes described above, ~20% were consistently altered in 2 or more experimental conditions and 33 total genes were consistently altered across all three experimental groups (Fig 2). Similarly, 13 of the 58 pathways identified were also consistently altered in multiple (2 or more) experimental conditions (Fig 2). Of specific relevance to schizophrenia, were GO terms ‘Neuroactive Ligand-Receptor Interactions’ (ranked 5th) and ‘GABAergic Synapses’ (Ranked 15th) (Fig 3). We also had an a priori hypothesis that these conditions would produce alterations in genes known to regulate GABAergic neuron differentiation and migration. Indeed, we observed decreased expression of genes related to specific subsets of GABAergic development, specifically those associated with medial ganglionic eminence (MGE: but not caudal GE) derived interneurons (Fig 4). These results were confirmed using qPCR (Fig 5). Finally, some of the most robust alterations were observed in genes associated with ribosomal function (ranked 1st—Fig 6).
Fig 2. Transcriptional analysis identified consistent and overlapping changes in gene expression across three developmental models of schizophrenia.
(A) Venn Diagram showing the number of genes that were differentially expressed in each schizophrenia model compared to control animals. Of these, 33 genes were differentially expressed in all three models. (B) The differentially expressed genes that were affected by all three prenatal manipulations, were ranked. (C) Venn Diagram depicting the pathways differentially altered by all three conditions. (D) Those pathways that showed overlap between at least 2 treatment groups are ranked.
Fig 3. Pathway analysis identified expression changes in genes associated with Neuroactive Ligand-Receptor Interactions and GABAergic Synapses.
The unbiased pathway analyses identified pathways with relevance to schizophrenia, including GO terms ‘Neuroactive Ligand-Receptor Interactions’ (ranked 5th) and ‘GABAergic Synapses’ (Ranked 15th) (A) Graph showing the differentially expressed genes in the Neuroactive Ligand-Receptor Interaction pathway. (B) Graph showing the differentially expressed genes in the GABAergic Synapse pathway.
Fig 4. Alterations in genes associated with GABAergic development.
In addition to the independent pathway analyses, we had an a priori hypothesis that genes involved in interneuron development and migration would be altered in these groups. Specifically, those genes associated with MGE-derived interneurons were downregulated (Arx, Dlx1, Dlx5, Lhx6, & Nkx2.1) whereas markers of CGE-derived interneurons (Sox6, Gsx1, & Mash1) were not significantly affected.
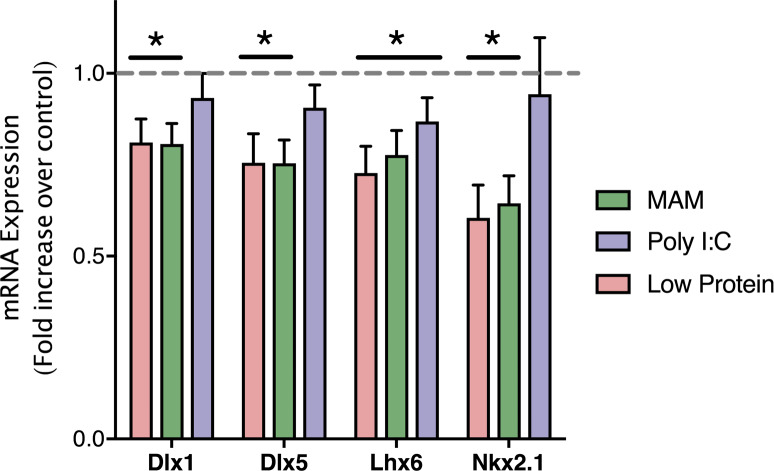
Fig 5. qPCR confirmation of genes associated with GABAergic development.
qPCR confirmed that the expression of genes associated with the development and migration of GABAergic interneurons (Dlx1, Dlx5, Lhx6, and Nkx2.1) were decreased by developmental disruption models of schizophrenia. * is p<0.05 compared to saline-treated controls. n = 5–6 per group.
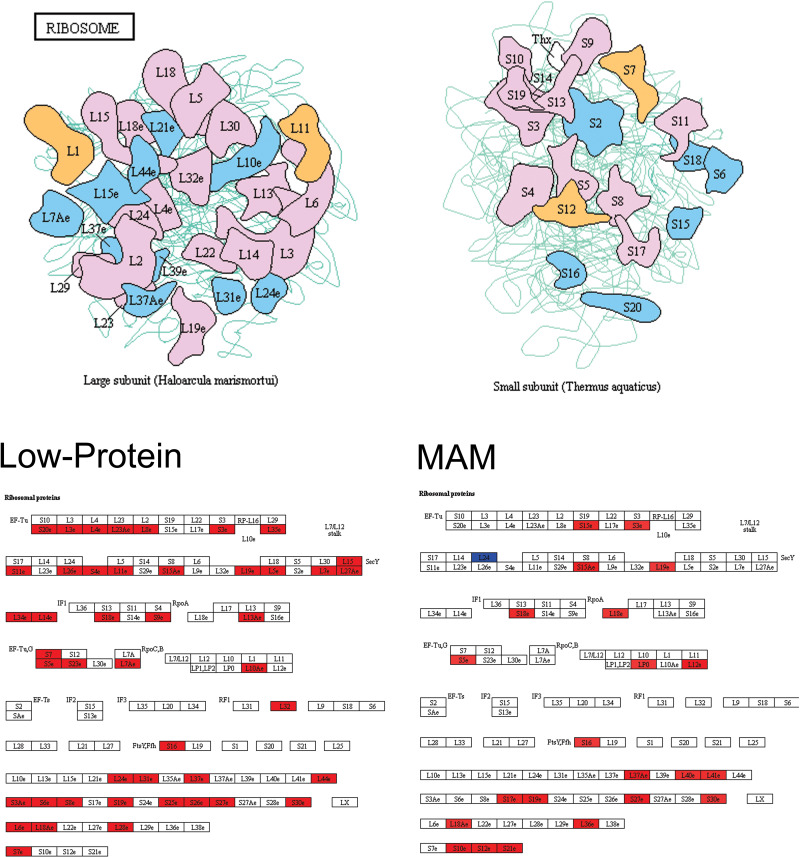
Fig 6. Pathway analysis identified expression changes in ribosomal proteins.
The most significant pathway identified was that of Ribosomal function. (Top) Cartoon depicting proteins in the large (left) and small (right) subunits of the ribosome. (Bottom) Both Low-Protein and MAM caused changes in the expression of genes associated with ribosomal proteins. For each treatment group, an increased expression of genes encoding ribosomal proteins are highlighted in red while decreased expression is shown in blue.
Quantitative polymerase chain reaction
To confirm the Meta-Analysis finding that developmental disruption decreases expression of genes related to GABAergic neuron differentiation and migration, we performed qPCR. One way ANOVAs confirmed that developmental disruption significantly alters the expression of Dlx 1 (F22 = 10.34, p<0.05), Dlx 5 (F22 = 15.65, p<0.05), Lhx6 (F22 = 16.78, p<0.05) and Nkx2.1 (F22 = 14.54, p<0.05). The Holm-Sidak post-hoc analysis found that Dlx 1, Dlx 5 and Nkx2.1 expression were all significantly decreased in the Low Protein and MAM treatment groups, as compared to saline-treated controls (p<0.05). Lhx6 expression was decreased by all three developmental disruptions (p<0.05).
Discussion
In the current experiments, we used an unbiased transcriptional analysis of the developing hippocampus and found consistent and overlapping alterations in gene expression across three distinct developmental models of schizophrenia. Because the hippocampus is hyperactive at baseline in schizophrenia patients, we chose to examine baseline transcription in the three developmental models. In the MAM model, a DNA methylating agent, methylazoxymethanol acetate (MAM), is administered to pregnant female rats on gestational day 17. This model has been shown to produce anatomical (e.g. reduced cortical thickness and hippocampal area[45]), physiological (e.g. hippocampal hyperactivity[24,30,31] and increased dopamine cell population activity[24]), and behavioral changes (e.g. stimulant-induced hyperlocomotion[24,45], prepulse inhibition deficits[45,46], latent inhibition deficits[31,47], decreased social interaction[31,46], working memory impairments[46,48], and cognitive inflexibility[31,47]) that model schizophrenia (for review, see [32]). Viral infection during pregnancy has been associated with an increased risk of schizophrenia in humans[5,49–51] and administration of the viral mimetic, polyriboinosinic-polyribocytidilic acid (Poly I:C), on gestational day 17 has also been shown to produce anatomical (e.g. enlarged ventricles and reduced hippocampal volume[52,53]), physiological (e.g. increased dopamine cell population activity[54] and increased striatal dopamine release[53]), and behavioral (e.g. stimulant-induced hyperlocomotion[53,55], prepulse inhibition deficits[55], latent inhibition deficits[53], decreased social interaction time[56,57], working memory impairments[57,58], and cognitive inflexibility[56]) deficits that resemble schizophrenia (for review, see [33,59]). Epidemiological evidence also suggests that dietary deficiencies during pregnancy is a major risk factor for schizophrenia[9,13,60–62]. Although this rodent model has been less extensively validated than MAM or Poly I:C, evidence suggests that prenatal protein malnutrition can produce anatomical (e.g. decreased prefrontal cortical volume[63]) and behavioral changes (e.g. prepulse inhibition deficits[64], decreased social interaction[65], cognitive inflexibility[66]) that model schizophrenia.
Our meta-analysis identified 33 genes that were altered consistently across the three rodent models. However, of these 33 genes, some have already been implicated in the pathology of schizophrenia. For example, the LHX2 gene encodes the Lim homeobox protein 2, a cortical selector gene that is expressed in cortical precursor cells[67]. LHX2 regulates processes such as axon guidance[68] and is required for normal hippocampal development[67]. LHX2 is down-regulated in the hippocampus of schizophrenia patients[69], while our data suggest that it is upregulated in the same region during gestation, a discrepancy that is likely explained by the developmental time point at which the gene was measured. Regardless, implication of this gene in both animal models and human patients reinforces the developmental nature of schizophrenia, and the role of the hippocampus in the pathology of this disorder[32].
In addition, we found that the Syp gene was down-regulated in all three rodent models of schizophrenia. Synaptophysin, an integral synaptic vesicle membrane protein, is encoded by the Syp gene. This result is in line with multiple human studies that have found decreased synaptophysin expression in the hippocampus and prefrontal cortex of schizophrenia patients[70–72]. Further, one study found that schizophrenia patients were more likely than controls to have rare single nucleotide polymorphisms in the Syp gene[73]. Schizophrenia patients have decreased hippocampal volumes[74], without a concomitant decrease in neuronal cell loss[75,76], leading some to hypothesize that the volume decrease is a result of reduced synaptic levels[77]. Results derived from our neurodevelopmental model of schizophrenia that show a decrease in Syp gene expression, along with similar findings in human studies, are in line with this hypothesis, as synaptophysin is a major synaptic vesicle protein and one of the most widely used markers of synaptic density.
In addition to a loss of synapses, schizophrenia has also been associated with alterations in neurotransmission. The pathway analysis performed in the current experiments identified consistent alterations (across at least 2 conditions) in genes associated with ‘Neuroactive Ligand-Receptor Interactions’ (Ranked 5th). Some of the genes in this pathway have already been associated with schizophrenia in humans. For example, we found that both Low-Protein and Poly I:C decreased expression of Adra2c and Adra2a, genes that encode two forms of the G-protein coupled alpha-adrenergic receptor. In humans, positive symptoms are exacerbated by noradrengergic agonists and reduced by antagonists[78]. Further, targeting the alpha 2 noradrenergic receptor has been shown to improve cognitive and negative symptoms in schizophrenia[79]. In addition, schizophrenia has also been linked to glutamatergic dysfunction. For example, antagonists of the ionotropic NMDA glutamate receptor, such as phencyclidine and ketamine, produce psychosis in humans[80]. We also found that both Poly I:C and Low-Protein treatments decreased expression of Grin1, the gene that encodes one form of the NMDA receptor. Gene association studies have identified Grin1 as a candidate gene for schizophrenia and there is a strong association between the G1001C polymorphism on the Grin1 gene promoter and schizophrenia[81]. Our results support the hypothesis that schizophrenia symptoms are associated with disruptions in neurotransmission, even during early stages of neurodevelopment.
GABA is the primary inhibitory neurotransmitter in the brain and pathway analysis identified specific changes in gene expression associated with GABAergic synapses. This is not surprising as deficits in GABAergic function have also been consistently observed in schizophrenia patients. For example, GABA is synthesized by the enzymes glutamic acid decarboxylase 1 and 2 (GAD1 and GAD2) and decreases in GAD expression have been observed across multiple brain regions, including the hippocampus and cortex[82]. This is in line with our finding that both Low-Protein and MAM treatments decreased Gad1 expression. Further, schizophrenia has been associated with altered expression of multiple GABAergic receptors. For example, a decrease in the metabotropic GABAB receptor has been observed in the hippocampus of schizophrenia patients[83]. In the current experiments, we found that both Low Protein and MAM produce a decrease in expression of Gabbr1, the gene for subunit 1 of the GABAB receptor. In addition, other aspects of GABAergic function are affected by schizophrenia, including transport and maintenance[84]. We also identified additional genes that were decreased by at least one of the schizophrenia models examined, including slc6a1 and slc32a1, two genes that encode GABAergic transporters, and slc12a5, the gene for the potassium-chloride cotransporter 2, which regulates intracellular chloride levels and thus GABAergic inhibition. It should be noted that in the current experiments, the dissections were not limited to the hippocampus but also included regions of the neocortex. However, the interneuron dysfunction in schizophrenia patients has been observed both in hippocampal [26,27] and cortical[85–88] regions.
We have previously demonstrated that aberrant interneuron function can induce a schizophrenia-like phenotype[28], and that transplantation of specific interneuron subtypes, derived from the MGE, can reverse neurophysiological and behavioral deficits associated with schizophrenia, in the MAM rat[30,31]. For this reason, we had an a priori hypothesis that developmental disruptions may alter interneuron development and migration. During development, GABAergic interneurons are born in the subpallial forebrain in progenitor regions called ganglionic eminences before migrating tangentially into hippocampal and cortical regions[89]. In these progenitor regions, the cellular fate of interneuron precursors is determined by activation of a series of morphogen-regulated transcription factors. Some of the first of these transcription factors to be activated are the Dlx homeobox genes, including Dlx1/2 and Dlx5/6. Dlx1 and Dlx2 are activated in all interneurons downstream of early patterning genes and play an important role in the generation, specification, and migration of interneurons (for review see [90]). In humans, reduced Dlx1 mRNA has been observed in the OFC[91] and thalamus[92] of schizophrenia patients. Downstream, Dlx 5/6 are direct targets of Dlx1/2, and have been shown to play a role in interneuron maturation. In the current experiments, we also found that all three prenatal manipulations decreased Dlx1 and Dlx5 gene expression, suggesting that these transcription factors may be one mechanism by which prenatal disruptions can lead to alterations in interneuron development. Specificity for the MGE developing interneurons (including PV and SST) come from the early expression of NK2 homeobox 1 (NKX2.1). Indeed, unlike the Dlx homeobox transcription factors, Nkx2.1 is absent from the LGE and CGE [93], suggesting a specific role in MGE neurogenesis. Nkx2.1 is expressed in PV and SST progenitors of the MGE and activates the downstream transcription factor, Lhx6, which is required for interneuron migration and post-migratory maturation[89]. Interestingly, all three prenatal manipulations that we examined produced a decrease in Lhx6 expression. This finding is in line with results from human studies that identified deficits in Lhx6 function in schizophrenia patients[94,95]. Further, many of the genetic cascades downstream of Lhx6 have also been implicated in schizophrenia. For example, alterations in the expression of the chemokine receptors (CXCR4 & CXCR7) have been reported [96] and an association between neuregulin signaling (via the Erb4 receptor) has been extensively studied [97–101]. Interestingly, we did not see changes in markers of pyramidal cells (CAMKII, TBR1, MAP2), astrocytes (GFAP, Slc1A3, S100B, ALDH1L1), microglia (TMEM119, CX3CR1), or oligodendrocytes (PDGFRA, OLIG2, MBP). Taken together, we posit that the decrease in Dlx1, Dlx5, and Lhx6 expression that we observed in our schizophrenia models may lead to the cell-specific deficits in interneuron development that are thought to play a key role in the pathophysiology of schizophrenia.
Finally, the highest ranked pathway observed was in ribosomal function. Specifically, we found increases in the expression of multiple genes that encode ribosomal proteins in both the Low-Protein and MAM models. Protein abnormalities have previously been observed in schizophrenia patients[102] but total protein levels can be affected by changes in a variety of factors, including transcription, mRNA stability, gene regulation by microRNAs, protein stability, and ubiquitination. However, in line with our results, others have used neural progenitor cells derived from human induced pluripotent stem cells to demonstrate that schizophrenia patients have an increase in total protein levels that was the result of an increase in translational machinery[102]. In addition, one post-mortem study demonstrated genetic changes in ribosome and translational activity in the brain of schizophrenia patients[103]. Together with our results, this suggests that the protein abnormalities associated with schizophrenia may be a direct result of increased ribosomal machinery and translation.
It should be noted, that some genes that are known to be affected in schizophrenia were not affected by all three animal models that we examined. Further, there were zero pathways that were affected by all three models. In our initial analysis, we found that 127 genes were commonly affected by protein malnutrition and Poly I:C while MAM and protein malnutrition only shared 70 common genes and MAM and Poly I:C only shared 47 common genes. Of these genes, COMTD1 has been shown to be differentially methylated in schizophrenia patients[104], which would lead to altered transcription of this gene. In the current study, we found that COMTD1 expression was significantly down-regulated by prenatal protein malnutrition and Poly I:C, but not by MAM. Conversely, the Srr gene, was only downregulated by MAM treatment. Interestingly, reduced Srr immunoreactivity has been observed in the prefrontal cortex of schizophrenia patients [105] and Srr mutant mice show schizophrenia-like behavioral deficits[106]. Although prenatal MAM, Poly I:C and protein malnutrition have all been shown to produce schizophrenia-like deficits, epidemiological evidence has only found Poly I:C and protein malnutrition to be associated with an increased risk for schizophrenia. Further, these two rodent models seem to produce less robust behavioral changes compared to the MAM model. Therefore, it is possible that MAM treatment produces schizophrenia-like deficits via a mechanism that is different than Poly I:C or protein malnutrition.
The results of the current studies are limited by the fact that only the hippocampus and neocortex were examined and that both sexes were combined. In future studies, a more nuanced approach will be used to examine transcriptomic changes across brain regions and between sexes. In conclusion, our unbiased transcriptional analysis of the developing hippocampus identified consistent and overlapping alterations in gene expression, especially related to neurotransmission, GABAergic interneuron development, and ribosomal function. Our results suggest that schizophrenia is associated with changes in gene expression that occur during gestation, and identify potential targets for future therapeutics.
Supporting information
(XLSX)
Data Availability
All RNA Sequencing data are freely available online at the GEO (Gene Expression Omnibus) under accession number is GSE149828 or at https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE149828.
Funding Statement
This work was supported by the Owens Foundation (DJL), R01 MH090067 (DJL) from the National Institute for Mental Health, by TL1TR002647 (JJD) from the National Center for Advancing Translational Science, and by K99MH121355 (JJD) from the National Institute of Mental Health. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Owens Foundation: NA NIMH: https://www.nimh.nih.gov/index.shtml NCATS: https://ncats.nih.gov/.
References
- 1.Moreno-Kustner B, Martin C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PloS one. 2018;13(4):e0195687 10.1371/journal.pone.0195687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feinberg I. Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence? Journal of psychiatric research. 1982;17(4):319–34. 10.1016/0022-3956(82)90038-3 [DOI] [PubMed] [Google Scholar]
- 3.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Archives of general psychiatry. 1987;44(7):660–9. 10.1001/archpsyc.1987.01800190080012 [DOI] [PubMed] [Google Scholar]
- 4.Brown AS. Prenatal infection as a risk factor for schizophrenia. Schizophrenia Bulletin. 2006;32(2):200–2. 10.1093/schbul/sbj052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown AS, Begg MD, Gravenstein S, Schaefer CA, Wyatt RJ, Bresnahan M, et al. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Archives of General Psychiatry. 2004;61(8):774–80. 10.1001/archpsyc.61.8.774 [DOI] [PubMed] [Google Scholar]
- 6.Brown AS, Derkits EJ. Prenatal infection and schizophrenia: A review of epidemiologic and translational studies. American Journal of Psychiatry. 2010;167(3):261–80. 10.1176/appi.ajp.2009.09030361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buka SL, Tsuang MT, Torrey EF, Klebanoff MA, Bernstein D, Yolken RH. Maternal infections and subsequent psychosis among offspring. Archives of general psychiatry. 2001;58(11):1032–7. 10.1001/archpsyc.58.11.1032 [DOI] [PubMed] [Google Scholar]
- 8.Shi L, Fatemi SH, Sidwell RW, Patterson PH. Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. Journal of Neuroscience. 2003;23(1):297–302. 10.1523/JNEUROSCI.23-01-00297.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown AS. The environment and susceptibility to schizophrenia. Progress in Neurobiology. 2011;93(1):23–58. 10.1016/j.pneurobio.2010.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown AS, Susser ES. Prenatal nutritional deficiency and risk of adult schizophrenia. Schizophrenia Bulletin. 2008;34(6):1054–63. 10.1093/schbul/sbn096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.St Clair D, Xu M, Wang P, Yu Y, Fang Y, Zhang F, et al. Rates of adult schizophrenia following prenatal exposure to the Chinese famine of 1959–1961. Journal of the American Medical Association. 2005;294(5):557–62. 10.1001/jama.294.5.557 [DOI] [PubMed] [Google Scholar]
- 12.Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, et al. Schizophrenia after prenatal famine further evidence. Archives of General Psychiatry. 1996;53(1):25–31. 10.1001/archpsyc.1996.01830010027005 [DOI] [PubMed] [Google Scholar]
- 13.Susser ES, Lin SP. Schizophrenia after prenatal exposure to the Dutch hunger winter of 1944–1945. Archives of General Psychiatry. 1992;49(12):983–8. 10.1001/archpsyc.1992.01820120071010 [DOI] [PubMed] [Google Scholar]
- 14.Chevassus-au-Louis N, Represa A. The right neuron at the wrong place: Biology of heterotopic neurons in cortical neuronal migration disorders, with special reference to associated pathologies. Cellular and Molecular Life Sciences. 1999;55(10):1206–15. 10.1007/s000180050367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nopouulos PC, Flaum M, Andreasen NC, Swayze VW. Gray matter heterotopias in schizophrenia. Psychiatry Research: Neuroimaging. 1995;61(1):11–4. 10.1016/0925-4927(95)02573-g [DOI] [PubMed] [Google Scholar]
- 16.Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM, et al. Rare Structural Variants Disrupt Multiple Genes in Neurodevelopmental Pathways in Schizophrenia. Science. 2008;320(5875):539–43. 10.1126/science.1155174 [DOI] [PubMed] [Google Scholar]
- 17.Niwa M, Kamiya A, Murai R, Kubo K, Gruber AJ, Tomita K, et al. Knockdown of DISC1 by in utero gene transfer disturbs postnatal dopaminergic maturation in the frontal cortex and leads to adult behavioral deficits. Neuron. 2010;65(4):480–9. 10.1016/j.neuron.2010.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guilmatre A, Dubourg C, Mosca AL, Legallic S, Goldenberg A, Drouin-Garraud V, et al. Recurrent rearrangements in synaptic and neurodevelopmental genes and shared biologic pathways in schizophrenia, autism, and mental retardation. Archives of general psychiatry. 2009;66(9):947–56. 10.1001/archgenpsychiatry.2009.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heckers S, Rauch SL, Goff D, Savage CR, Schacter DL, Fischman AJ, et al. Impaired recruitment of the hippocampus during conscious recollection in schizophrenia. Nature neuroscience. 1998;1(4):318–23. 10.1038/1137 [DOI] [PubMed] [Google Scholar]
- 20.Schobel SA, Kelly MA, Corcoran CM, Van Heertum K, Seckinger R, Goetz R, et al. Anterior hippocampal and orbitofrontal cortical structural brain abnormalities in association with cognitive deficits in schizophrenia. Schizophrenia research. 2009;114(1‚Äì3):110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malaspina D, Storer S, Furman V, Esser P, Printz D, Berman A, et al. SPECT study of visual fixation in schizophrenia and comparison subjects. Biol Psychiatry. 1999;46(1):89–93. 10.1016/s0006-3223(98)00306-0 [DOI] [PubMed] [Google Scholar]
- 22.Medoff DR, Holcomb HH, Lahti AC, Tamminga CA. Probing the human hippocampus using rCBF: Contrasts in schizophrenia. Hippocampus. 2001;11(5):543–50. 10.1002/hipo.1070 [DOI] [PubMed] [Google Scholar]
- 23.Schobel SA, Lewandowski NM, Corcoran CM, et al. DIfferential targeting of the ca1 subfield of the hippocampal formation by schizophrenia and related psychotic disorders. Arch Gen Psychiatry. 2009;66(9):938–46. 10.1001/archgenpsychiatry.2009.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lodge DJ, Grace AA. Aberrant Hippocampal Activity Underlies the Dopamine Dysregulation in an Animal Model of Schizophrenia. The Journal of Neuroscience. 2007;27(42):11424–30. 10.1523/JNEUROSCI.2847-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aguilar DD, Chen L, Lodge DJ. Increasing Endocannabinoid Levels in the Ventral Pallidum Restore Aberrant Dopamine Neuron Activity in the Subchronic PCP Rodent Model of Schizophrenia2015 2015-01-01 00:00:00. [DOI] [PMC free article] [PubMed]
- 26.Zhang ZJ, Reynolds GP. A selective decrease in the relative density of parvalbumin-immunoreactive neurons in the hippocampus in schizophrenia. Schizophrenia research. 2002;55(1–2):1–10. 10.1016/s0920-9964(01)00188-8 [DOI] [PubMed] [Google Scholar]
- 27.Konradi C, Yang CK, Zimmerman EI, Lohmann KM, Gresch P, Pantazopoulos H, et al. Hippocampal interneurons are abnormal in schizophrenia. Schizophrenia research. 2011;131(1–3):165–73. 10.1016/j.schres.2011.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boley AM, Perez SM, Lodge DJ. A fundamental role for hippocampal parvalbumin in the dopamine hyperfunction associated with schizophrenia. Schizophrenia research. 2014;157(1–3):238–43. 10.1016/j.schres.2014.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perez SM, Boley A, Lodge DJ. Region specific knockdown of Parvalbumin or Somatostatin produces neuronal and behavioral deficits consistent with those observed in schizophrenia. Transl Psychiatry. 2019;9(1):264 10.1038/s41398-019-0603-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perez SM, Lodge DJ. Hippocampal interneuron transplants reverse aberrant dopamine system function and behavior in a rodent model of schizophrenia. Molecular psychiatry. 2013;18(11):1193–8. 10.1038/mp.2013.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Donegan JJ, Tyson JA, Branch SY, Beckstead MJ, Anderson SA, Lodge DJ. Stem cell-derived interneuron transplants as a treatment for schizophrenia: preclinical validation in a rodent model. Molecular psychiatry. 2017;22(10):1492–501. 10.1038/mp.2016.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lodge DJ, Grace AA. Gestational methylazoxymethanol acetate administration: a developmental disruption model of schizophrenia. Behavioural brain research. 2009;204(2):306–12. 10.1016/j.bbr.2009.01.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meyer U, Feldon J. To poly(I:C) or not to poly(I:C): advancing preclinical schizophrenia research through the use of prenatal immune activation models. Neuropharmacology. 2012;62(3):1308–21. 10.1016/j.neuropharm.2011.01.009 [DOI] [PubMed] [Google Scholar]
- 34.Butler PD, Susser ES, H P, Brown AS, Kaufman CA, Gorman JM. Prenatal Nutritional Deprivation as a Risk Factor in Schizophrenia: Preclinical Evidence. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2003;11:227. [DOI] [PubMed] [Google Scholar]
- 35.Joseph Altman SAB. Atlas of Prenatal Rat Brain Development. 1st Edition ed: CRC Press; 1994. [Google Scholar]
- 36.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic acids research. 2000;28(1):27–30. 10.1093/nar/28.1.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kanehisa M, Goto S, Kawashima S, Nakaya A. The KEGG databases at GenomeNet. Nucleic acids research. 2002;30(1):42–6. 10.1093/nar/30.1.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nature genetics. 2000;25(1):25–9. 10.1038/75556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agarwal V, Bell GW, Nam JW, Bartel DP. Predicting effective microRNA target sites in mammalian mRNAs. eLife. 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nam JW, Rissland OS, Koppstein D, Abreu-Goodger C, Jan CH, Agarwal V, et al. Global analyses of the effect of different cellular contexts on microRNA targeting. Molecular cell. 2014;53(6):1031–43. 10.1016/j.molcel.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffiths-Jones S, Saini HK, van Dongen S, Enright AJ. miRBase: tools for microRNA genomics. Nucleic acids research. 2008;36(Database issue):D154–8. 10.1093/nar/gkm952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kozomara A, Griffiths-Jones S. miRBase: annotating high confidence microRNAs using deep sequencing data. Nucleic acids research. 2014;42(Database issue):D68–73. 10.1093/nar/gkt1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Friedman RC, Farh KK, Burge CB, Bartel DP. Most mammalian mRNAs are conserved targets of microRNAs. Genome research. 2009;19(1):92–105. 10.1101/gr.082701.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grimson A, Farh KK, Johnston WK, Garrett-Engele P, Lim LP, Bartel DP. MicroRNA targeting specificity in mammals: determinants beyond seed pairing. Molecular cell. 2007;27(1):91–105. 10.1016/j.molcel.2007.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moore H, Jentsch JD, Ghajarnia M, Geyer MA, Grace AA. A neurobehavioral systems analysis of adult rats exposed to methylazoxymethanol acetate on E17: implications for the neuropathology of schizophrenia. Biological psychiatry. 2006;60(3):253–64. 10.1016/j.biopsych.2006.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Pen G, Gourevitch R, Hazane F, Hoareau C, Jay TM, Krebs MO. Peri-pubertal maturation after developmental disturbance: a model for psychosis onset in the rat. Neuroscience. 2006;143(2):395–405. 10.1016/j.neuroscience.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 47.Flagstad P, Glenthoj BY, Didriksen M. Cognitive deficits caused by late gestational disruption of neurogenesis in rats: a preclinical model of schizophrenia. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2005;30(2):250–60. [DOI] [PubMed] [Google Scholar]
- 48.Gourevitch R, Rocher C, Le Pen G, Krebs MO, Jay TM. Working memory deficits in adult rats after prenatal disruption of neurogenesis. Behav Pharmacol. 2004;15(4):287–92. 10.1097/01.fbp.0000135703.48799.71 [DOI] [PubMed] [Google Scholar]
- 49.Brown AS. Prenatal infection as a risk factor for schizophrenia. Schizophr Bull. 2006;32(2):200–2. 10.1093/schbul/sbj052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. The American journal of psychiatry. 2010;167(3):261–80. 10.1176/appi.ajp.2009.09030361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buka SL, Tsuang MT, Torrey EF, Klebanoff MA, Bernstein D, Yolken RH. Maternal infections and subsequent psychosis among offspring. Archives of general psychiatry. 2001;58(11):1032–7. 10.1001/archpsyc.58.11.1032 [DOI] [PubMed] [Google Scholar]
- 52.Piontkewitz Y, Assaf Y, Weiner I. Clozapine administration in adolescence prevents postpubertal emergence of brain structural pathology in an animal model of schizophrenia. Biological psychiatry. 2009;66(11):1038–46. 10.1016/j.biopsych.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 53.Zuckerman L, Rehavi M, Nachman R, Weiner I. Immune activation during pregnancy in rats leads to a postpubertal emergence of disrupted latent inhibition, dopaminergic hyperfunction, and altered limbic morphology in the offspring: a novel neurodevelopmental model of schizophrenia. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2003;28(10):1778–89. [DOI] [PubMed] [Google Scholar]
- 54.Perez SM, Lodge DJ. Convergent Inputs from the Hippocampus and Thalamus to the Nucleus Accumbens Regulate Dopamine Neuron Activity. The Journal of Neuroscience. 2018;38(50):10607–18. 10.1523/JNEUROSCI.2629-16.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Giovanoli S, Engler H, Engler A, Richetto J, Feldon J, Riva MA, et al. Preventive effects of minocycline in a neurodevelopmental two-hit model with relevance to schizophrenia. Transl Psychiatry. 2016;6:e772 10.1038/tp.2016.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Donegan JJ, Boley AM, Lodge DJ. Embryonic stem cell transplants as a therapeutic strategy in a rodent model of autism. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2018;43(8):1789–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Osborne AL, Solowij N, Babic I, Huang XF, Weston-Green K. Improved Social Interaction, Recognition and Working Memory with Cannabidiol Treatment in a Prenatal Infection (poly I:C) Rat Model. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2017;42(7):1447–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murray BG, Davies DA, Molder JJ, Howland JG. Maternal immune activation during pregnancy in rats impairs working memory capacity of the offspring. Neurobiol Learn Mem. 2017;141:150–6. 10.1016/j.nlm.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 59.Reisinger S, Khan D, Kong E, Berger A, Pollak A, Pollak DD. The poly(I:C)-induced maternal immune activation model in preclinical neuropsychiatric drug discovery. Pharmacol Ther. 2015;149:213–26. 10.1016/j.pharmthera.2015.01.001 [DOI] [PubMed] [Google Scholar]
- 60.Brown AS, Susser ES. Prenatal nutritional deficiency and risk of adult schizophrenia. Schizophr Bull. 2008;34(6):1054–63. 10.1093/schbul/sbn096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.St Clair D, Xu M, Wang P, Yu Y, Fang Y, Zhang F, et al. Rates of adult schizophrenia following prenatal exposure to the Chinese famine of 1959–1961. Jama. 2005;294(5):557–62. 10.1001/jama.294.5.557 [DOI] [PubMed] [Google Scholar]
- 62.Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, et al. Schizophrenia after prenatal famine. Further evidence. Archives of general psychiatry. 1996;53(1):25–31. 10.1001/archpsyc.1996.01830010027005 [DOI] [PubMed] [Google Scholar]
- 63.Cruz-Rizzolo RJ, Limieri LL, de Paiva IR, Ribeiro JOB, Pimenta TF, Pinato L, et al. Protein malnutrition during gestation and early life decreases neuronal size in the medial prefrontal cortex of post-pubertal rats. IBRO Rep. 2017;3:65–71. 10.1016/j.ibror.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Palmer AA, Printz DJ, Butler PD, Dulawa SC, Printz MP. Prenatal protein deprivation in rats induces changes in prepulse inhibition and NMDA receptor binding. Brain Res. 2004;996(2):193–201. 10.1016/j.brainres.2003.09.077 [DOI] [PubMed] [Google Scholar]
- 65.Almeida SS, Tonkiss J, Galler JR. Prenatal protein malnutrition affects the social interactions of juvenile rats. Physiol Behav. 1996;60(1):197–201. 10.1016/0031-9384(95)02236-8 [DOI] [PubMed] [Google Scholar]
- 66.Tonkiss J, Galler JR. Prenatal protein malnutrition and working memory performance in adult rats. Behavioural brain research. 1990;40(2):95–107. 10.1016/0166-4328(90)90002-v [DOI] [PubMed] [Google Scholar]
- 67.Mangale VS, Hirokawa KE, Satyaki PR, Gokulchandran N, Chikbire S, Subramanian L, et al. Lhx2 selector activity specifies cortical identity and suppresses hippocampal organizer fate. Science. 2008;319(5861):304–9. 10.1126/science.1151695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sanuki R, Onishi A, Koike C, Muramatsu R, Watanabe S, Muranishi Y, et al. miR-124a is required for hippocampal axogenesis and retinal cone survival through Lhx2 suppression. Nature neuroscience. 2011;14(9):1125–34. 10.1038/nn.2897 [DOI] [PubMed] [Google Scholar]
- 69.Benes FM, Lim B, Matzilevich D, Walsh JP, Subburaju S, Minns M. Regulation of the GABA cell phenotype in hippocampus of schizophrenics and bipolars. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(24):10164–9. 10.1073/pnas.0703806104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vawter MP, Howard AL, Hyde TM, Kleinman JE, Freed WJ. Alterations of hippocampal secreted N-CAM in bipolar disorder and synaptophysin in schizophrenia. Molecular psychiatry. 1999;4(5):467–75. 10.1038/sj.mp.4000547 [DOI] [PubMed] [Google Scholar]
- 71.Glantz LA, Lewis DA. Reduction of synaptophysin immunoreactivity in the prefrontal cortex of subjects with schizophrenia. Regional and diagnostic specificity. Archives of general psychiatry. 1997;54(10):943–52. 10.1001/archpsyc.1997.01830220065010 [DOI] [PubMed] [Google Scholar]
- 72.Osimo EF, Beck K, Reis Marques T, Howes OD. Synaptic loss in schizophrenia: a meta-analysis and systematic review of synaptic protein and mRNA measures. Molecular psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shen YC, Tsai HM, Ruan JW, Liao YC, Chen SF, Chen CH. Genetic and functional analyses of the gene encoding synaptophysin in schizophrenia. Schizophrenia research. 2012;137(1–3):14–9. 10.1016/j.schres.2012.01.028 [DOI] [PubMed] [Google Scholar]
- 74.Nelson MD, Saykin AJ, Flashman LA, Riordan HJ. Hippocampal volume reduction in schizophrenia as assessed by magnetic resonance imaging: a meta-analytic study. Archives of general psychiatry. 1998;55(5):433–40. [DOI] [PubMed] [Google Scholar]
- 75.Arnold SE. Cellular and molecular neuropathology of the parahippocampal region in schizophrenia. Annals of the New York Academy of Sciences. 2000;911:275–92. 10.1111/j.1749-6632.2000.tb06732.x [DOI] [PubMed] [Google Scholar]
- 76.Harrison PJ. The neuropathology of schizophrenia. A critical review of the data and their interpretation. Brain: a journal of neurology. 1999;122 (Pt 4):593–624. [DOI] [PubMed] [Google Scholar]
- 77.Mirnics K, Middleton FA, Lewis DA, Levitt P. Analysis of complex brain disorders with gene expression microarrays: schizophrenia as a disease of the synapse. Trends in Neurosciences. 2001;24(8):479–86. 10.1016/s0166-2236(00)01862-2 [DOI] [PubMed] [Google Scholar]
- 78.Maletic V, Eramo A, Gwin K, Offord SJ, Duffy RA. The Role of Norepinephrine and Its alpha-Adrenergic Receptors in the Pathophysiology and Treatment of Major Depressive Disorder and Schizophrenia: A Systematic Review. Frontiers in psychiatry. 2017;8:42 10.3389/fpsyt.2017.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Arnsten AF. Adrenergic targets for the treatment of cognitive deficits in schizophrenia. Psychopharmacology. 2004;174(1):25–31. 10.1007/s00213-003-1724-3 [DOI] [PubMed] [Google Scholar]
- 80.Moghaddam B, Javitt D. From Revolution to Evolution: The Glutamate Hypothesis of Schizophrenia and its Implication for Treatment. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2011;37:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Galehdari H, Pooryasin A, Foroughmand A, Daneshmand S, Saadat M. Association between the G1001C polymorphism in the GRIN1 gene promoter and schizophrenia in the Iranian population. Journal of molecular neuroscience: MN. 2009;38(2):178–81. 10.1007/s12031-008-9148-5 [DOI] [PubMed] [Google Scholar]
- 82.Heckers S, Stone D, Walsh J, Shick J, Koul P, Benes FM. Differential hippocampal expression of glutamic acid decarboxylase 65 and 67 messenger RNA in bipolar disorder and schizophrenia. Archives of general psychiatry. 2002;59(6):521–9. 10.1001/archpsyc.59.6.521 [DOI] [PubMed] [Google Scholar]
- 83.Mizukami K, Sasaki M, Ishikawa M, Iwakiri M, Hidaka S, Shiraishi H, et al. Immunohistochemical localization of gamma-aminobutyric acid(B) receptor in the hippocampus of subjects with schizophrenia. Neuroscience letters. 2000;283(2):101–4. 10.1016/s0304-3940(00)00939-3 [DOI] [PubMed] [Google Scholar]
- 84.Wassef A, Baker J, Kochan LD. GABA and schizophrenia: a review of basic science and clinical studies. Journal of clinical psychopharmacology. 2003;23(6):601–40. 10.1097/01.jcp.0000095349.32154.a5 [DOI] [PubMed] [Google Scholar]
- 85.Akbarian S, Kim JJ, Potkin SG, Hagman JO, Tafazzoli A, Bunney WE Jr., et al. Gene expression for glutamic acid decarboxylase is reduced without loss of neurons in prefrontal cortex of schizophrenics. Archives of general psychiatry. 1995;52(4):258–66. 10.1001/archpsyc.1995.03950160008002 [DOI] [PubMed] [Google Scholar]
- 86.Guidotti A, Auta J, Davis JM, Di-Giorgi-Gerevini V, Dwivedi Y, Grayson DR, et al. Decrease in reelin and glutamic acid decarboxylase67 (GAD67) expression in schizophrenia and bipolar disorder: a postmortem brain study. Archives of general psychiatry. 2000;57(11):1061–9. 10.1001/archpsyc.57.11.1061 [DOI] [PubMed] [Google Scholar]
- 87.Hashimoto T, Volk DW, Eggan SM, Mirnics K, Pierri JN, Sun Z, et al. Gene expression deficits in a subclass of GABA neurons in the prefrontal cortex of subjects with schizophrenia. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2003;23(15):6315–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Volk DW, Austin MC, Pierri JN, Sampson AR, Lewis DA. Decreased glutamic acid decarboxylase67 messenger RNA expression in a subset of prefrontal cortical gamma-aminobutyric acid neurons in subjects with schizophrenia. Archives of general psychiatry. 2000;57(3):237–45. 10.1001/archpsyc.57.3.237 [DOI] [PubMed] [Google Scholar]
- 89.Tyson JA, Anderson SA. GABAergic interneuron transplants to study development and treat disease. Trends Neurosci. 2014;37(3):169–77. 10.1016/j.tins.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rossignol E. Genetics and Function of Neocortical GABAergic Interneurons in Neurodevelopmental Disorders. Neural Plasticity. 2011;2011:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Joshi D, Fung SJ, Rothwell A, Weickert CS. Higher gamma-aminobutyric acid neuron density in the white matter of orbital frontal cortex in schizophrenia. Biological psychiatry. 2012;72(9):725–33. 10.1016/j.biopsych.2012.06.021 [DOI] [PubMed] [Google Scholar]
- 92.Kromkamp M, Uylings HB, Smidt MP, Hellemons AJ, Burbach JP, Kahn RS. Decreased thalamic expression of the homeobox gene DLX1 in psychosis. Archives of general psychiatry. 2003;60(9):869–74. 10.1001/archpsyc.60.9.869 [DOI] [PubMed] [Google Scholar]
- 93.Sussel L, Marin O, Kimura S, Rubenstein JL. Loss of Nkx2.1 homeobox gene function results in a ventral to dorsal molecular respecification within the basal telencephalon: evidence for a transformation of the pallidum into the striatum. Development. 1999;126(15):3359–70. [DOI] [PubMed] [Google Scholar]
- 94.Volk DW, Edelson JR, Lewis DA. Cortical inhibitory neuron disturbances in schizophrenia: role of the ontogenetic transcription factor Lhx6. Schizophr Bull. 2014;40(5):1053–61. 10.1093/schbul/sbu068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Volk DW, Matsubara T, Li S, Sengupta EJ, Georgiev D, Minabe Y, et al. Deficits in transcriptional regulators of cortical parvalbumin neurons in schizophrenia. The American journal of psychiatry. 2012;169(10):1082–91. 10.1176/appi.ajp.2012.12030305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Volk DW, Chitrapu A, Edelson JR, Lewis DA. Chemokine receptors and cortical interneuron dysfunction in schizophrenia. Schizophrenia research. 2015(0). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Corfas G, Roy K, Buxbaum JD. Neuregulin 1-erbB signaling and the molecular/cellular basis of schizophrenia. Nature neuroscience. 2004;7(6):575–80. 10.1038/nn1258 [DOI] [PubMed] [Google Scholar]
- 98.Harrison PJ, Law AJ. Neuregulin 1 and Schizophrenia: Genetics, Gene Expression, and Neurobiology. Biological Psychiatry. 2006;60(2):132–40. 10.1016/j.biopsych.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 99.Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: On the matter of their convergence. Molecular Psychiatry. 2005;10(1):40–68. 10.1038/sj.mp.4001558 [DOI] [PubMed] [Google Scholar]
- 100.Mei L, Xiong WC. Neuregulin 1 in neural development, synaptic plasticity and schizophrenia. Nature Reviews Neuroscience. 2008;9(6):437–52. 10.1038/nrn2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Stefansson H, Sigurdsson E, Steinthorsdottir V, Bjornsdottir S, Sigmundsson T, Ghosh S, et al. Neuregulin 1 and Susceptibility to Schizophrenia. American Journal of Human Genetics. 2002;71(4):877–92. 10.1086/342734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Topol A, English JA, Flaherty E, Rajarajan P, Hartley BJ, Gupta S, et al. Increased abundance of translation machinery in stem cell–derived neural progenitor cells from four schizophrenia patients. Translational Psychiatry. 2015;5:e662 10.1038/tp.2015.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wu JQ, Wang X, Beveridge NJ, Tooney PA, Scott RJ, Carr VJ, et al. Transcriptome sequencing revealed significant alteration of cortical promoter usage and splicing in schizophrenia. PloS one. 2012;7(4):e36351 10.1371/journal.pone.0036351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nishioka M, Bundo M, Koike S, Takizawa R, Kakiuchi C, Araki T, et al. Comprehensive DNA methylation analysis of peripheral blood cells derived from patients with first-episode schizophrenia. J Hum Genet. 2013;58(2):91–7. 10.1038/jhg.2012.140 [DOI] [PubMed] [Google Scholar]
- 105.Bendikov I, Nadri C, Amar S, Panizzutti R, De Miranda J, Wolosker H, et al. A CSF and postmortem brain study of D-serine metabolic parameters in schizophrenia. Schizophrenia research. 2007;90(1–3):41–51. 10.1016/j.schres.2006.10.010 [DOI] [PubMed] [Google Scholar]
- 106.Labrie V, Fukumura R, Rastogi A, Fick LJ, Wang W, Boutros PC, et al. Serine racemase is associated with schizophrenia susceptibility in humans and in a mouse model. Hum Mol Genet. 2009;18(17):3227–43. 10.1093/hmg/ddp261 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All RNA Sequencing data are freely available online at the GEO (Gene Expression Omnibus) under accession number is GSE149828 or at https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE149828.