Abstract
The rapid evolution of the health emergency linked to the spread of severe acute respiratory syndrome coronavirus 2 requires specifications for the rehabilitative management of patients with coronavirus disease 2019 (COVID-19). The symptomatic evolution of patients with COVID-19 is characterized by 2 phases: an acute phase in which respiratory symptoms prevail and a postacute phase in which patients can show symptoms related to prolonged immobilization, to previous and current respiratory dysfunctions, and to cognitive and emotional disorders. Thus, there is the need for specialized rehabilitative care for these patients. This communication reports the experience of the San Raffaele Hospital of Milan and recommends the setup of specialized clinical pathways for the rehabilitation of patients with COVID-19. In this hospital, between February 1 and March 2, 2020, about 50 patients were admitted every day with COVID-19 symptoms. In those days, about 400 acute care beds were created (intensive care/infectious diseases). In the following 30 days, from March 2 to mid-April, despite the presence of 60 daily arrivals to the emergency department, the organization of patient flow between different wards was modified, and several different units were created based on a more accurate integration of patients’ needs. According to this new organization, patients were admitted first to acute care COVID-19 units and then to COVID-19 rehabilitation units, post-COVID-19 rehabilitation units, and/or quarantine/observation units. After hospital discharge, telemedicine was used to follow-up with patients at home. Such clinical pathways should each involve dedicated multidisciplinary teams composed of pulmonologists, physiatrists, neurologists, cardiologists, physiotherapists, neuropsychologists, occupational therapists, speech therapists, and nutritionists.
Keywords: Coronavirus, Critical pathways, Neuropsychology, Physical therapy modalities, Rehabilitation, Telemedicine
List of abbreviations: COVID-19, coronavirus disease 2019; ED, emergency department; ICU, intensive care unit; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
The rapid exponential diffusion of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has dramatically shaken the functional organization of public and private health facilities in Italy. The San Raffaele Hospital of Milan (Lombardy, Italy) admitted more than 400 patients with coronavirus disease 2019 (COVID-19) in 1 month (typically, during the month of February, about 300 patients are admitted in the whole San Raffaele Hospital).
After this first phase, the clinical care of patients was reorganized to provide better treatment for patients in acute condition and to better meet the rehabilitation needs of patients post COVID-19 to optimize home discharge. This report describes the experience of the Rehabilitation and Functional Recovery Department of the San Raffaele Hospital (Milan, Italy) and aims to identify barriers to the functional recovery of patients with COVID-19 and to provide suggestions for the setup of a specialized clinical standard procedure flow for the rehabilitation of these patients.
First Phase
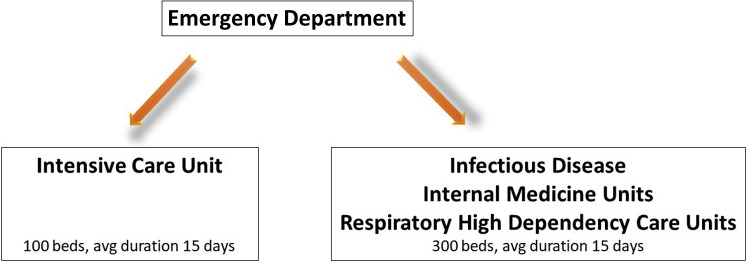
At the outbreak of the pandemic in the Lombardy region of Italy the clinical burden was divided between emergency departments (EDs), intensive care units (ICUs), respiratory high-dependency care units, and infectious diseases units according to the different stages of the disease (fig 1 ). The San Raffaele Hospital of Milan admitted more than 400 patients with COVID-19 in 1 month. Patients with COVID-19 can develop pneumonia characterized by bilateral interstitial infiltrates with severe hypoxic respiratory insufficiency following a serious alteration of the ventilation-perfusion ratio. Patients with acute hypoxemic may also experience persistent dyspnea despite the administration of high oxygen flows. In these cases, other devices such as invasive and noninvasive ventilation may be useful. This first phase led patients to a prolonged stay in intensive and nonintensive areas and prolonged immobilization, which complicated the postinfectious recovery.1
Fig 1.
Hospitalization of patients with COVID-19 in phase 1. Figure 1 summarizes the clinical movement flow undertaken by patients with COVID-19 during phase 1, before the organization of specialized COVID-19 rehabilitation standard procedure flow. Patients entered the hospital through the ED and were admitted to either the ICU or the infectious disease, internal medicine, or respiratory high dependency care departments, according to their clinical status. The hospitalization stays were, on average, 15 days; 400 beds were created in 1 month. Abbreviation: avg, average.
In February 2020 the San Raffaele Hospital admitted 100 patients to the ICU and 300 patients to the medicine and infectious diseases units. In this first phase, 10 physicians of the specialized rehabilitation units and 40 physiotherapists were reassigned to the acute wards for patients with COVID-19. Various wards were merged, and no specialized rehabilitation care was provided. Patients were hospitalized for about 2 weeks, after which they were usually home-discharged to meet the need for new patient admissions. Based on our experience, about 20%-25% of discharged patients were discharged for home confinement with SARS-CoV-2–positive swabs. Based on our experience, it usually takes 2-4 weeks from symptom onset to obtain negative swabs.
Thus, the mean duration of hospitalization in the San Raffaele Acute COVID-19 Unit in phase 1 was 15 days, after which patients were discharged home.
After 1 month, the following criticisms emerged: (1) hospitalization stays in the acute wards were too long and impeded the admission of new critically ill patients; (2) patients were discharged after the resolution of respiratory distress, sometimes even with positive swabs; (3) the deployment of health care workers was not optimized because specialized rehabilitation professionals were recruited to serve as internal medicine specialists; (4) about 25% of the health care workers caring for patients in acute condition presented with symptoms of SARS-CoV-2 infection, in part because of improper use of personal protective equipment (PPE) and lack of experience in infectious diseases, particularly for workers relocated to new infectious wards; and (5) this organization lacked a specialized multidisciplinary rehabilitation strategy to improve patients’ functional recovery, causing the discharge of patients still in need of respiratory, motor, or cognitive rehabilitation.
A specialized rehabilitation was thus greatly needed in the postacute phase. In phase 1, we observed that about 20% of patients with acute COVID-19 met the criteria for hospitalization in a rehabilitation department.
Second Phase
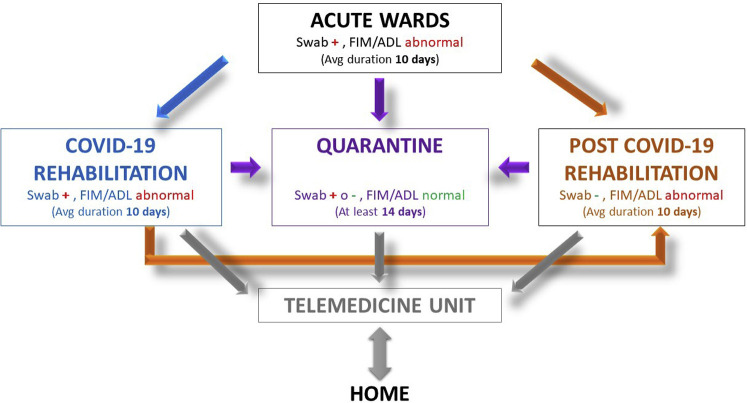
One month from the onset of admissions of patients with COVID-19, despite a continuous flow of 60 daily arrivals to the ED, the following wards were reorganized or created: acute COVID-19 units, rehabilitation COVID-19 units, post–COVID-19 units, quarantine/observation units, and a unit for telemedicine and telerehabilitation (fig 2 ). The new objectives of phase 2 were to discharge only patients with negative swabs and maximal functional autonomy and to limit infections among patients and health care workers inside the hospital.
Fig 2.
Rehabilitation paths for patients with COVID-19 and patients post COVID-19 in phase 2. Figure 2 summarizes the clinical flow of patients with COVID-19, from acute wards until home return. Each transition between the different units is discussed and decided by the multidisciplinary team. Following the acute phase (for an average of 10d) and according to the swabs results as well as functional abilities of patients, patients should be admitted to COVID-19 rehabilitation wards (for an average duration of 10d), quarantine (for at least 14d), or post-COVID-19 rehabilitation wards (for an average of 10d) to undergo rehabilitation. Following quarantine or post-COVID rehabilitation, patients can return home and continue rehabilitation according to their needs under the supervision of hospital specialists using the telemedicine unit. Moreover, even during quarantine, patients and caregivers can benefit from remote supervision using the telemedicine unit. Abbreviation: avg, average.
These different wards provided specialized rehabilitation to patients according to their clinical status. Respiratory, motor, and cognitive rehabilitation treatments were designed based on the literature according to patients’ symptoms and functional impairments. A multidisciplinary team of specialists dedicated to each unit evaluated and monitored patient conditions throughout the rehabilitation process. The teams were composed of pulmonologists, physiatrists, neurologists, cardiologists, physiotherapists, occupational therapists, speech therapists, and neuropsychologists. For each patient, personalized care must always be applied,2 especially for patients with severe and/or critical illness, advanced age, obesity, multiple underlying diseases, and organ complications. For each individual patient, a personalized rehabilitative project (addressing cardiorespiratory, neuromotor, and cognitive impairments) must be designed.
The following instrumental examinations were performed at the patient’s bedside: radiography, echocardiogram, lung ultrasonography, aorta ultrasonography, fibroscopy for patients with dysphagia, and electromyogram. Thus, the patient did not have to be moved to perform these examinations.
For patients hospitalized with COVID-19, the purpose of rehabilitation in both the acute and postcritical phases was to improve respiratory dynamics, counteract musculoskeletal deconditioning and immobilization, reduce the onset of complications, recover the cognitive and emotional status in patients with hypoxic damage, reduce disability, and improve the quality of life in anticipation of the patient’s discharge. During hospitalization, the electrolyte balance (frequent hypernatremia) and cardiac load (probrain natriuretic peptide, cardiac, lung, and aorta ultrasonography) must be monitored. Central nervous system involvement has also been reported, even in patients without hypoxemia, with dysgeusia, hyposmia, and altered mental state or neuropsychological manifestations. Symptoms related to neuromuscular pathology and cranial nerve involvement (ageusia and anophthalmia, isolated paralysis of the VII cranial nerve) were also observed.3
Like patients admitted to ICUs with acute respiratory failure due to chronic conditions (exacerbations of chronic obstructive pulmonary disease), early respiratory rehabilitation should be a priority in the COVID-19 units.4 , 5 Relevant physiotherapy aspects were the multidisciplinary management of noninvasive ventilation, the management of the patient's correct posture (and possible variation of posture), and, when the patient was in a stable clinical state, the recovery of mobility. In post-COVID-19 units, the recovery of patient mobility and autonomy was of critical importance.
The rehabilitative interventions in this phase were the following:
-
(1)
Management of posture/positional therapy: postural variation should be performed several times a day, with a dosage adapted to the patient's clinical conditions. Patients with severe acute respiratory distress syndrome can benefit from being placed in a prone position (even for more than 12h/d) during noninvasive ventilation.6 The pronation procedure should be interrupted in case of worsening of oxygenation. In a second phase, a gradual increase in raised positioning until the patient can maintain a seated and a standing position is recommended. The treatments aimed at recovering orthostatism and regaining gait ability and balance.
-
(2)
Multidisciplinary management of noninvasive ventilation: the physiotherapist can collaborate with medical and nursing staff in the management of noninvasive ventilation. The management of the ventilation device is of particular importance to improve patient comfort and compliance.
-
(3)
Passive and active mobilization of the patient: whenever possible, according to the clinical status of the subject, it is recommended to proceed to a passive or active mobilization of the patient, aimed at preventing secondary damage from being bedridden and the recovery and/or maintenance of muscle strength.
-
(4)
Identification of respiratory and motor criteria for the patient’s discharge from COVID-19 units.
Here is a list of general recommendations that have been implemented during phase 2 for the different units:
-
-
Avoid the shift of nurses, physicians, and rehabilitation therapists between COVID-19 and non-COVID-19 wards. Therefore, keep the staff of the different units separated.
-
-
Entry and exit accesses to and from the COVID-19 departments should be separated from the other units.
-
-
Movement of patients in the COVID-19 units should be carried out only through dedicated paths that should be sanitized and separated from the non-COVID units.
-
-
Body temperature measurement of all health care professionals should be taken at beginning and end of each shift (implementation of thermal cameras at the different hospital entry points).
-
-
Filtering facepiece 2 or filtering facepiece 3 masks should be used in COVID-19 units, and other PPE should be used in all COVID-19/non-COVID-19 departments.
Since the initiation of phase 2, the mean duration of hospitalization in the San Raffaele Acute COVID-19 unit was shortened to 10 days, after which patients were admitted to the COVID-19 rehabilitation units. Following the above recommendations, none of the health care professionals involved showed signs of SARS-CoV-2 infection during the first month, as shown by body temperature monitoring. In both phases, contamination was tested by swabs only in symptomatic workers.
COVID-19 Rehabilitation Unit (Positive Swab, FIM That Shows Areas of Dependence, Not Under Assisted Ventilation)
Criteria for admission were as follows: this unit admitted patients who, once discharged from the COVID-19 acute wards, still had a positive swab, FIM<100, no fever for at least 4 days, stable oxygen saturation with no need for respiratory assistance or with no more than 4 L/min, and need to continue the specialized, hospitalized rehabilitation process (appendix 1).
Rehabilitation: the rehabilitation of stable and paucisymptomatic patients after discharge from the acute COVID-19 units mainly aimed to restore the motor abilities of the subject and to promote the recovery of independence and psychological adaptation.
The rehabilitation intervention focused on the areas of impairment identified in the patient7 , 8:
-
•
Deconditioning: endurance training must be proposed with the frequency and intensity recommended by the international literature for subjects with respiratory and/or deconditioning symptoms. We preferred to use cycle ergometer or arm ergometer because of the limited space available for confined patients.
-
•
Strength deficit: resistance training using elastic resistance bands.
-
•
Balance dysfunction: static and dynamic balance training exercises.
-
•
Deficits in basic activities of daily living: intervention on the recovery and/or adaptation of these activities through the support of physiotherapists and occupational therapists.
-
•
Cognitive deficits: neuropsychological training, counseling sessions, and psychological support should be provided in case of cognitive deficits such as disorientation or confusion.
Shared equipment was carefully sanitized after use.
The following rating scales were used for functional assessments and monitoring of patients:
-
-
Mini-Mental State Examination9
-
-
Montreal Cognitive Assessment10
-
-
Malnutrition Universal Screening Tool11
-
-
FIM12
-
-
Short Physical Performance Battery13
-
-
Barthel Dyspnea Index14
- -
-
-
Borg rating of perceived exertion for dyspnea and fatigue17 (during reconditioning training and 6-minute walk test)
-
-
30-second sit-to-stand test18
-
-
6-minute walk test (performed only before discharge)19
The San Raffaele COVID-19 rehabilitation unit capacity was 30 beds. The mean time from admission to discharge was 10 days. By mid-April 2020, 50 patients had been discharged from this unit.
Post-COVID-19 Rehabilitation Unit (2 Consecutive Negative Swabs at 24h Intervals, FIM That Shows Areas of Dependence)
Patients admitted to the post-COVID-19 ward were patients with 2 consecutive negative swabs at 24-hour intervals and with areas of dependence at FIM evaluation. The post-COVID-19 ward was thus constituted as a traditional rehabilitative ward. The same rehabilitation procedures undergone in the COVID-19 unit were applied. The average duration of post-COVID-19 rehabilitation was 10 days.
Quarantine/Observation Unit (Positive or Negative Swab, Normal FIM/Activities of Daily Living)
It seems indispensable to establish a low intensity ward to admit clinically stable patients with minimal activities of daily living (ADL) reduction needing a prolonged surveillance period (duration of at least 2wk).
This allowed 3 different options at the end of the rehabilitation or postacute hospitalization: (1) home discharge with scheduled clinical check: all patients with negative swabs and ADL and FIM showing no areas of dependence (or with patient evaluation of dependence concordant with the objectives of each single rehabilitative plan) (see appendix 1); (2) home discharge with outpatient rehabilitation: for patients with negative swabs but with 1 area of dependence at the basic activities of daily living and FIM>110; (3) discharge and transfer to observation/quarantine: for patients with normal ADL and no areas of dependence at FIM evaluation but with positive swabs.
The duration of recovery in the quarantine ward was at least 14 days.
Telemedicine and Remote Rehabilitation Unit
The presence of a telemedicine and rehabilitation unit is recommended to promote protected discharge, to monitor patients in quarantine, and to ensure the continuity of care for patients with COVID-19 but also for patients that do not have COVID-19. It is also useful for sharing complex clinical cases with other hospitals or clinics in the area (hub-and-spoke system), thus avoiding unnecessary patient movements.
In the last years, the rehabilitation and functional recovery department of the San Raffaele Hospital has been increasingly using remote rehabilitation for memory and language deficits. Such remote care of patients can be expanded to help caregivers in the daily assistance of patients, for example with nutritional advice to avoid malnutrition after discharge.20
In respiratory rehabilitation, telemedicine is useful for remote monitoring of the prescribed exercises that can be performed online and offline and for monitoring the status of oxygen saturation and cardiovascular parameters.21
For cognitive and motor rehabilitation, telemedicine must be adapted to each clinical case. Motor telerehabilitation is especially recommended for patients who have few losses of ADL after discharge from the rehabilitation departments to maintain and increase the autonomy achieved during hospitalization.22 , 23 The main areas of intervention in telerehabilitation that must be adapted to the functional state of the subject are cognitive training, mobility, resistance training, and gait training.
Discussion
Acquisition of clinical data is in progress. We started to gather follow-up data at 1 month post discharge. Although these data have not been published yet, the establishment of a specialized multidisciplinary rehabilitation standard procedure flow for patients with COVID-19 and patients post COVID-19 was intended to discharge patients with negative swabs and improve patient functional status. The final goal is to discharge patients only after functional rehabilitation meets the objectives of each personal rehabilitative plan. All patients were discharged with negative swabs and FIM and ADL showing minimal areas of dependence. Moreover, so far, none of the dedicated health care workers have been contaminated after the establishment of the specialized rehabilitation standard procedure flow, potentially related to improved compliance with correct PPE use. Contamination of hospital staff is monitored through mandatory body temperature measurements at hospital entry and exit.
Overall, rehabilitation care needs to be integrated in the clinical care of patients with COVID-19.
In the case of the San Raffaele Hospital, the procedures and timing were formulated based on the experience gained in the field. The drastic and unexpected flow of patients in the first 30 days led to an emergency organization. The experience gained subsequently led us to recommend the establishment of different units that followed the course of the disease with a more rational use of rehabilitation health care professionals. This type of organization of the second phase, according to our experience, was the most suitable for managing such a situation in a large hospital that has a continuous daily flow of 50-60 patients with COVID-19 to the ED.
Future directions
Thanks to this organizational model of rehabilitation flow, patients with COVID-19 were discharged after the resolution of the respiratory infection (negative swabs) and with no or minimal areas of functional dependence. Future communications should be provided to report patients’ motor, cognitive, and cardiorespiratory functions at discharge and at several weeks post discharge for follow-up. For example, according to the San Raffaele experience, the patient mean age was about 70 years. About 80% of patients presented with abnormal scores at Mini-Mental State Examination or Montreal Cognitive Assessment at admission to the COVID-19 rehabilitation unit, and most patients recovered normal values at hospital discharge. Further reports are thus needed to fully assert such functional improvements. We are also currently improving our telemedicine system by simplifying the remote follow-up of patients with the development of an application that will be provided to patients in May. This application contains cognitive and motor rehabilitative exercises that can benefit patient recovery at low costs.
Patient clinically recovered from COVID-19: a patient who, after presenting with clinical manifestations (fever, rhinitis, cough, sore throat, possibly dyspnea, and, in severe cases, pneumonia with respiratory failure) associated with the virologically documented infection by SARS-CoV-2, becomes asymptomatic because of the resolution of the clinical symptomatology (apyrexia, improvement of respiratory symptoms until no need for ventilatory support, improved lung imaging). The clinically healed subject may still test positive for the SARS-CoV-2 test.
Recovered patient: a patient who recovers from the symptoms of COVID-19 infection with 2 consecutive negative SARS-CoV-2 testing swabs, carried out 24 hours apart.
Definition of FIM that shows areas of dependence: a score on the FIM scale that shows areas of dependence of the subject (score≤5), in particular in the motor functions, affecting the overall autonomy of the patient.24 The main use of the FIM consists of the analysis of average scores on patient populations for the control of efficacy and efficiency of hospitalization rehabilitation programs.
References
- 1.Griffiths R.D., Jones C. Recovery from intensive care. BMJ. 1999;319:427–429. doi: 10.1136/bmj.319.7207.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wouters E.F.M., Wouters B.B.R.E.F., Augustin I.M.L., et al. Personalised pulmonary rehabilitation in COPD. Eur Respir Rev. 2018;27:170125. doi: 10.1183/16000617.0125-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brugliera L., Spina A., Castellazzi P., et al. Rehabilitation of COVID-19 patients. J. Rehabil Med. 2020;52 doi: 10.2340/16501977-2678. [DOI] [PubMed] [Google Scholar]
- 4.Kallet R.H., Hemphill J.C., Dicker R.A., et al. The spontaneous breathing pattern and work of breathing of patients with acute respiratory distress syndrome and acute lung injury. Respir Care. 2007;52:989–995. [PubMed] [Google Scholar]
- 5.Guérin C., Reignier J., Richard J.-C., et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 6.Sartini C., Tresoldi M., Scarpellini P., et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020 doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lau H.M.-C., Ng G.Y.-F., Jones A.Y.-M., et al. A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome. Aust J Physiother. 2005;51:213–219. doi: 10.1016/S0004-9514(05)70002-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connolly B., Salisbury L., O’Neill B., et al. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev. 2015;6:CD008632. doi: 10.1002/14651858.CD008632.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Nasreddine Z.S., Phillips N.A., Bédirian V., et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 11.Elia M. BAPEN; Redditch: 2003. Screening for malnutrition: a multidisciplinary responsibility. Development and use of the Malnutrition Universal Screening Tool (‘MUST’) for adults. A Report by the Malnutrition Advisory Group of the British Association for Parenteral and Enteral Nutrition. [Google Scholar]
- 12.Pasqua F., Biscione G.L., Crigna G., et al. Use of functional independence measure in rehabilitation of inpatients with respiratory failure. Respir Med. 2009;103:471–476. doi: 10.1016/j.rmed.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Guralnik J.M., Simonsick E.M., Ferrucci L., et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 14.Vitacca M., Paneroni M., Baiardi P., et al. Development of a Barthel Index based on dyspnea for patients with respiratory diseases. Int J Chron Obstruct Pulmon Dis. 2016;11:1199–1206. doi: 10.2147/COPD.S104376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah S., Vanclay F., Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 16.Berg K.O., Maki B.E., Williams J.I., Holliday P.J., Wood-Dauphinee S.L. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73:1073–1080. [PubMed] [Google Scholar]
- 17.Borg G.A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 18.Gill S.D., de Morton N.A., McBurney H. An investigation of the validity of six measures of physical function in people awaiting joint replacement surgery of the hip or knee. Clin Rehabil. 2012;26:945–951. doi: 10.1177/0269215511434993. [DOI] [PubMed] [Google Scholar]
- 19.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 20.Brugliera L., Spina A., Castellazzi P., et al. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur J Clin Nutr. 2020;74:860–863. doi: 10.1038/s41430-020-0664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ambrosino N., Fracchia C. The role of tele-medicine in patients with respiratory diseases. Expert Rev Respir Med. 2017;11:893–900. doi: 10.1080/17476348.2017.1383898. [DOI] [PubMed] [Google Scholar]
- 22.Agostini M., Moja L., Banzi R., et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21:202–213. doi: 10.1177/1357633X15572201. [DOI] [PubMed] [Google Scholar]
- 23.Tenforde A.S., Hefner J.E., Kodish-Wachs J.E., Iaccarino M.A., Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9:S51–S58. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 24.Stineman M.G., Ross R.N., Fiedler R., Granger C.V., Maislin G. Functional independence staging: conceptual foundation, face validity, and empirical derivation. Arch Phys Med Rehabil. 2003;84:29–37. doi: 10.1053/apmr.2003.50061. [DOI] [PubMed] [Google Scholar]