Abstract
Congenital anomalies of the kidney and urinary tract (CAKUT) constitute 20% of all congenital malformations occurring in one in 500 live births. Worldwide, CAKUT are responsible for 40% to 50% of pediatric and 7% of adult end-stage renal disease. Pathogenic variants in genes causing CAKUT include monogenic diseases such as polycystic kidney disease and ciliopathies, as well as syndromes that include isolated kidney disease in conjunction with other abnormalities. Prenatal diagnosis most often occurs using ultrasonography; however, further genetic diagnosis may be made using a variety of testing strategies. Family history and pathologic examination can also provide information to improve the ability to make a prenatal diagnosis of CAKUT. Here, we provide a comprehensive overview of genetic considerations in the prenatal diagnosis of CAKUT disorders. Specifically, we discuss monogenic causes of CAKUT, associated ultrasound characteristics, and considerations for genetic diagnosis, antenatal care, and postnatal care.
1 |. INTRODUCTION
In recent years, comprehensive fetal anatomic survey in the second trimester has become standard of care. Among those receiving this evaluation, identification of fetal anomalies is the primary goal with congenital abnormalities of the kidney and urinary tract (CAKUT) accounting for up to 20% of all birth defects identified.1 A variety of CAKUT disorders, ranging from minor to major, structural and functional defects can be screened using ultrasound imaging. However, the sensitivity of ultrasound for detection of CAKUT is unknown given that many fetuses with prenatal CAKUT diagnosis have a normal phenotype postnatally. The diagnosis of CAKUT is an indication for the provider to review family history and provide recommendations for parental evaluation if indicated. Furthermore, it calls for the evaluation of other structural abnormalities of the fetus and provision of options for genetic counseling, prenatal diagnosis, pregnancy termination if desired, and informed care in the newborn period.
In this review, we provide an overview of inherited CAKUT and their associated ultrasonographic presentations. We will discuss: (a) embryologic processes of renal development; (b) common classifications of renal abnormalities; and (c) ultrasound findings and clinical considerations associated with a variety of inherited renal disorders. We focus on describing some single gene disorders commonly seen with CAKUT. Single gene disorders may be a primary source of CAKUT as evidenced by the following: (a) CAKUT appears with familial segregation, (b) monogenic mouse models exhibit CAKUT phenotypes, and (c) human multi-organ monogenic syndromes may include CAKUT phenotypes.2 In fact, 10% to 50% of children with CAKUT will report a family history of kidney anomalies or urinary tract disease.3Although there are hundreds of Mendelian disorders associated with prenatal CAKUT phenotypes, we will focus specifically on polycystic kidney disease (autosomal dominant and recessive), select ciliopathies such as Bardet-Biedel and Meckel-Gruber, and genetic associations with apparently isolated yet more common prenatal ultrasound findings such as renal agenesis, megacystis microcolon, urinary tract dilation, and multicystic dyplastic kidney (MCDK). This review provides a systemic approach to the prenatal diagnosis of CAKUT and highlights specific prenatal genetic considerations when CAKUT is identified.
2 |. EMBRYOLOGY
Kidney development is a multistage process initiated by the ureteric bud and the metanephric mesenchyme. At approximately 5 weeks gestation (Carnegie stages 14–15) (the most critical period for renal development), the ureteric bud arises from the nephric duct and undergoes a mesenchyme to epithelial transition and branching nephrogenesis. Eventually, this leads to nephron patterning and elongation. Perturbations in any part of this multistep process can lead to congenital anomalies of the urogenital tract or deficit in kidney function.4,5 Given early development of the kidneys and urinary tract, teratogens, including certain medications such as ACE inhibitors and warfarin among others (Table 1), should be avoided in the first trimester.
TABLE 1.
Drugs shown to influence renal development
| Drug | Effect of Maternal Treatment During Pregnancy on Fetal Kidney Development | Effect of Maternal Treatment While Breastfeeding on Neonatal Kidney Development |
|---|---|---|
| Aminoglycosides | Tubular alterations, low nephron count | Tubular damage, low nephron count |
| Cyclosporin A Prostaglandin synthetase inhibitors | Low nephron count, tubular alterations | Glomerular and tubular injury |
| ACE Inhibitors (ACEIs) Angiotensin Receptor Blocker (ARB) | Renal insufficiency | Atrophy of renal papilla, tubular alterations, low nephron count |
| Dexamethasone | Altered tubular transporters, low nephron count | No effect |
| Furosemide | Renal concentrating defect | No effect |
| Anti-epileptic drugs | Increased likelihood of congenital malformations (MCDK)* | No effect |
| Mycophenolate Mofetil | Renal agenesis, ectopia | No effect |
| Adriamycin | Bladder agenesis, hydronephrosis | No effect |
| Cyclophosphamide | Hydronephrosis | No effect |
Note. This table has been adapted from Schreuder, 2011.6
3 |. CLASSIFICATION AND DESCRIPTORS OF CAKUT
CAKUT are categorized on the basis of genetic versus nongenetic origins.7 Previous classification schemes, including the Potter classification system and the use of histopathological descriptors, have now fallen out-of-favor because CAKUT has a wide spectrum of phenotypes and because of confusion in differentiating pathological subclassifications from individual disorders (for example, differentiating between medullary cystic kidney disease, medullary cystic dysplasia, and MCDK disease is difficult because of subtle differences).
Histologic classification systems often categorize cystic pathology by a variety of descriptors, including the presence or absence of dysplasia, the loss of the cortico-medullary junction, and the size and location of cysts within the kidneys (the cortex, cortico-medullary junction, or medulla).
Dysplasia is a widely used descriptor in renal pathology. Renal dysplasia occurs as a result of failure of renal parenchyma to form normal nephrons and collecting ducts.8,9 Histologic characteristics of renal dysplasia include incomplete branching of collecting ducts surrounded by undifferentiated mesenchymal stroma.9 The difficulty with classifying renal disorders on the basis of presence or absence of dysplasia is the wide spectrum of sonographic appearance of dysplastic kidneys, which may range from small and hypoplastic to large and multicystic with varying degrees of echogenicity. Additionally, renal dysplasia may occur with or without cystic renal disease and vice versa, with substantial overlap between related gene disorders.9
Despite the limitations of using histologic subclassifications, these characteristics are still valuable to pathologists in describing the pathophysiology associated with these disorders. More recent changes to a classification structure based on genetic versus nongenetic origin is spurred by a better understanding of ciliopathies and how they contribute to cystic kidney disease. Inherited defects in the structure or function of primary cilia can lead to a variety of cystic phenotypes with multi-organ involvement.7 Conditions discussed here, such as Meckel-Gruber and Bardet-Biedl, commonly presenting with cystic kidneys and fall into the category of ciliopathies.10 Phakomatoses such as Tuberous Sclerosis and Von-Hippel Landau, can also, albeit less frequently, and very rarely present with cystic kidneys.11
4 |. CYSTIC KIDNEY DISEASE
4.1 |. Polycystic kidney disease
Polycystic kidney disease (PKD) is the most common heritable kidney disease.11 It is composed of the more frequently encountered autosomal dominant PKD (ADPKD) and the rare autosomal recessive polycystic kidney disease (ARPKD), which are described in detail below. Although PKD is the most common etiology of dysplastic kidneys, several ciliopathies can mimic the phenotype of PKD, suggesting there are multiple pathways that culminate in renal cyst development.12–14 Because of differences in inheritance, natural history, and clinical management, accurately distinguishing between PKD and other ciliopathies is necessary.10,11 In this section, we will discuss the genetic basis of PKD, clinical manifestations, and perinatal/neonatal aspects of management.
4.1.1 |. Autosomal dominant polycystic kidney disease
ADPKD is one of the most commonly inherited renal diseases, with an incidence of one in 500 to one in 1000 live births.15 As with many autosomal dominant disorders, significant heterogeneity exists in the clinical severity and manifestations of ADPKD, ranging from isolated renal disease to multi-organ disease involving cardiovascular health and the biliary tract.16,17 In adulthood, ADPKD accounts for 5% to 10% of all cases of end stage renal disease (ESRD).16,18 ESRD is defined as the glomerular filtration rate < 15% or the need to commence and continue dialysis therapy.7Most affected individuals present in the fifth to sixth decades of life, however, prenatal presentation can occur in approximately 2% to 5% of cases. The presentation is variable but literature suggests that the time of presentation is more in the third trimester.17,19 However, reports of prenatal presentation have been published earlier in gestation.7
Genetics of ADPKD
The primary genetic associations with ADPKD are germ-line mutations in the PKD1 and PKD2 genes, which encode for polycystin-1 and polycystin-2, respectively.17 Polycystin 1 and 2 are trans-membrane proteins, interacting through their C terminal tails forming a polycystin complex. Polycystin-2 is primarily involved in cellular calcium signaling.20 The exact structure and function of the polycystin complex and how pathogenic variants of these trans-membrane proteins leads to cyst formation are yet to be elucidated.12
Cyst formation occurs with variable severity and timing, likely related to the degree of protein truncation caused by a PKD1 or PKD2 pathogenic variant.17 Generally, PKD2 pathogenic variants are phenotypically milder than PKD1, with lower incidence of ESRD and arterial hypertension occurring later in life.21 Even in the setting of a known or likely pathogenic variant, clinical presentation, timing, and severity of disease is strikingly different from patient to patient.12,22 The association between genotype and phenotype is not well-understood, particularly in the prenatal period. Several factors may influence phenotypic presentation including PKD1 versus PKD2 variant, allelic changes, timing of gene inactivation, mosaicism, and family history.16
Ultrasound findings of ADPKD
Typical ultrasound findings include bilateral, enlarged kidneys (with or without hyperechogenicity), and may include increased or poor cortico-medullary differentiation. The presence of cysts is variable. The most common time of presentation of ADPKD is in the third trimester. However, family history or an affected parent or molecular diagnosis is the only reliable way to differentiate ADPKD from ARPKD because the phenotype and timing of presentation is variable in both conditions. The presence of hepatic abnormalities or anhydramnios/oligohydramnios is rarely seen prenatally with ADPKD. If anhydramnios/oligohydramnios is identified at the 18- to 20-week anatomy ultrasound, there is a high rate of mortality in the neonatal period because of pulmonary hypoplasia.19
Clinical considerations of ADPKD
The most common timing of disease is in the 5th to 6th decade of life, commonly with progressive renal insufficiency and presence of cystic kidneys on ultrasound.23 In such individuals, molecular diagnosis to identify PKD1 and PKD2 pathogenic variants is important.24 However, early manifestations during the prenatal, neonatal, and childhood periods have been reported, with variable development of renal cysts and parenchymal changes mimicking an ARPKD pattern.
If ADPKD is suspected, parental evaluation with renal ultrasound and genetic counseling is recommended. If discussion with parents elicits a family history of renal disease suggestive of ADPKD or there is already a molecular diagnosis in the family, molecular testing of a known pathogenic variant from the affected relative should be offered. If there is no known family history but large, bright, and/or cystic kidneys present prenatally, parents should be offered renal ultrasounds as identification of parental renal cysts will aid diagnosis in the fetus and prenatal counseling. In the absence of an obvious diagnosis, amniocentesis for chromosomal microarray (CMA) should be considered. If the CMA is normal, a targeted molecular panel for ADPKD versus trio whole exome sequencing (WES) (if available) can be considered.
Prenatally manifesting ADPKD has poorer prognosis than later onset disease. Mortality associated with isolated prenatal findings is unknown. However, in the setting of oligohydramnios, the 1-year mortality is estimated to be as high as 40%. If pulmonary hypoplasia is suspected, secondary to oligohydramnios, 1 year mortality may be as high as 80%.19 Neonatal considerations should include early establishment of care with pediatric nephrology and periodic assessment of renal volume and cyst development. Long-term management strategies should including screening and treatment of hypertension, assessment of proteinuria, and early diagnosis and treatment of genitourinary infections. Improved management of disease is directly correlated with lower likelihood of progression to ESRD.21
4.1.2 |. Autosomal recessive polycystic kidney disease (ARPKD)
Autosomal Recessive Polycystic Kidney Disease (ARPKD) is a severe form of cystic disease that involves the kidneys and biliary tract. The incidence of disease is 1 in 20,000 live births with variable timing of presentation and severity of phenotype.17 Diagnosis and care of the affected fetus requires a multidisciplinary team including perinatology, genetics, neonatology, and nephrology. Consistency of care is critical in providing adequate informed parental counseling of all options, including termination of pregnancy if indicated.25
Genetics of ARPKD
ARPKD is an autosomal recessive condition, often associated with pathogenic variants of the PHKD1 gene on chromosome 6p12, which encodes for the protein fibrocystin/polyductin complex (FPC). Significant evidence suggests alternative splicing may be implicated in protein truncation and subsequent disease manifestations as full length protein is required for adequate biologic function.25 Among those with significant clinical or histologic suggestion of ARPKD, detection of PHKD1 mutations reaches rates of 80–85%. However, variants in hepatocyte nuclear factor-1 beta (HNF1B) and other genes that lead to hepatorenal fibrocystic disease (HRFD) may mimic the phenotype of ARPKD and can also present prenatally.25 We present further discussion on HNF1B later in this review.
Like HNF1B, variants in the DAZ interacting protein 1-like (DZIP1L) gene leads to a ciliopathy that presents similarly to ARPKD and may also present prenatally, although rarely. DZIP1L encodes a cilliary protein that is required in regulating transformation zone integrity, with DZIP1L variants causing a similar phenotype to PHKD1 variants.17 However, variants in the DZIP1L tend to have a more moderate clinical course compared to ARPKD, rarely resulting in perinatal demise given the lack of amniotic fluid abnormalities and subsequent pulmonary complications.12
When ARPKD is suspected, it is critical to perform a detailed ultrasound to identify extra-renal abnormalities and consider other syndromic or infectious causes of CAKUT. Molecular genetic analysis using single gene testing is the only reliable method to provide a definitive diagnosis prenatally. Given the heterogeneous etiologies of large hyperechoic kidneys, this may be best done using a panel test or trio WES. Parents should be appropriately counseled regarding options of pregnancy continuation or termination based on individual preferences. Given the autosomal recessive inheritance pattern, it is important to identify the molecular etiology to allow the family to have prenatal diagnosis or pre-implantation genetic diagnosis in future pregnancies.
Ultrasound findings of ARPKD
Abnormal-appearance of fetal kidneys on a prenatal ultrasound are usually identified as enlarged and hyperechogenic kidneys with variability in timing of presentation. Some have reported a prenatal ARPKD phenotype in the early second trimester while others report diagnosis in the third trimester26 Characteristic findings include the presence of bilateral, large, hyperechogenic kidneys with poor cortico-medullary differentiation, retained reniform contour, and numerous microscopic cysts confined to distal tubules and collecting ducts (Figure 1).17,25 Macrocysts (> 10 mm) are unusual but have been reported in ARPKD and suggest multicystic dyplasia as a possible alternative diagnosis confirmed by molecular diagnosis in prior studies.7 ARPKD is difficult to differentiate from ADPKD unless a diagnosis in the family is known or inheritance pattern suggests a diagnosis because of phenotypic overlap and variability in timing of presentation.12 Cases of ARPKD diagnosed in the prenatal period are typically associated with severe disease and can lead to a Potter-like syndrome associated with oligohydramnios, massively enlarged kidneys, pulmonary hypoplasia, Potter-like facies, contracted limbs and club feet.17 It is important to note that hyperechogenic kidneys can also be a normal variant especially when normal amniotic fluid and normal anatomy are noted. Hyperechogenic kidneys can also be seen in other syndromes such as, but not limited to, ADPKD, congenital finnish nephrosis, Meckel Gruber syndrome, Trisomy 13, Beckwith Wiedemann syndrome, among others (Figure 2).
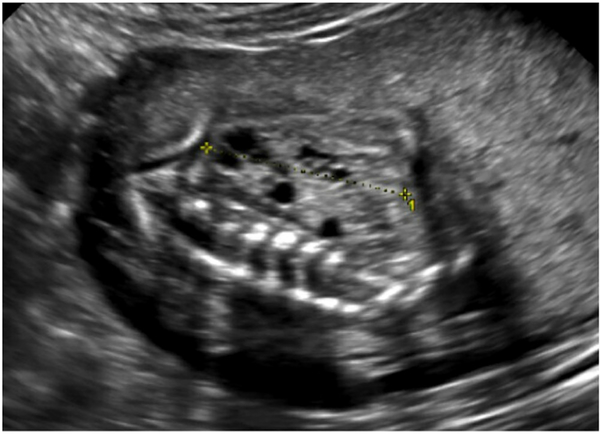
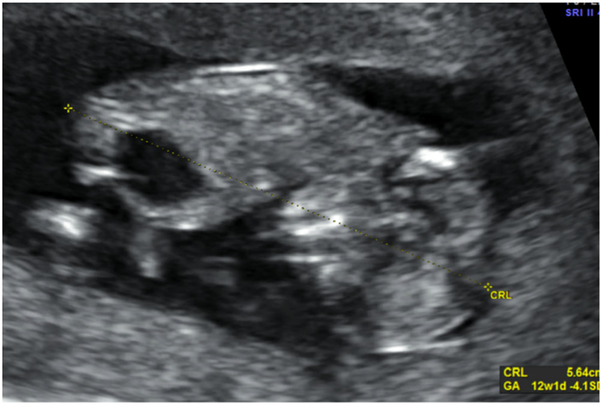
FIGURE 1.
Ultrasound findings associated with autosomal dominant polycystic kidney disease (ADPKD). One fetal kidney seen on antenatal ultrasound demonstrates enlarged, hyperechogenic appearance with the presence of cysts
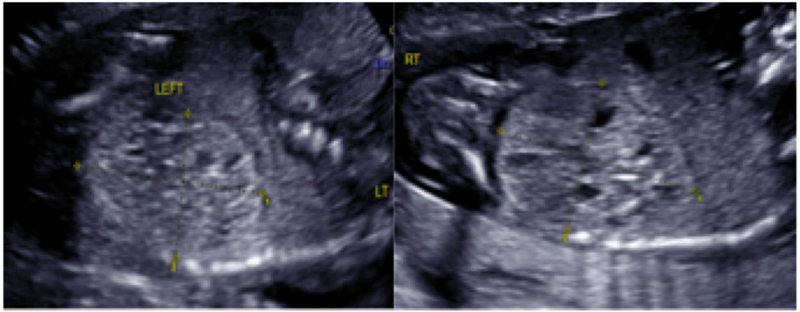
FIGURE 2.
Ultrasound findings associated with autosomal recessive polycystic kidney disease (ARPKD). Bilateral fetal kidneys seen in two separate images obtained via prenatal ultrasound. Kidneys appear enlarged with poor cortico-medullary differentiation and are hyperechoic in appearance due to the presence of numerous microscopic cysts
Clinical considerations of ARPKD
Significant risk of perinatal mortality exists when the fetus is diagnosed with ARPKD. Renal size greater than 4 standard deviations above normal with the presence of oligohydramnios or anhydramnios is associated with near 100% perinatal mortality due to pulmonary hypoplasia.25 Given the latter, repeat comprehensive ultrasound for assessment of kidney size, fluid, and fetal growth is recommended every 3–4 weeks. A multidisciplinary care team and access to a tertiary care center is often required for the specialized antenatal and perinatal care required by the fetus with ARPKD.25,19 The option of termination of pregnancy should be discussed and made available.
In continuing pregnancies, optimal delivery timing should be determined with multidisciplinary consensus involving maternal fetal medicine, neonatology, and pediatric nephrology; with careful consideration of additional risks of prematurity in the setting of possible pulmonary hypoplasia.25 In an analysis of prenatally diagnosed newborns with ARPKD followed prospectively in the ARegPKD study, 33.6% (107/318) had prenatally determined oligohydramnios or anhydramnios at variable points in gestation. Further, 23.4% (78/333) required assisted ventilation after delivery (mean gestational age of delivery 37.5 (SD 2.5). Most importantly however, the presence of amniotic fluid abnormalities at any point in pregnancy increased the risk of adverse pregnancy outcomes. Assisted ventilation and prenatal diagnosis of amniotic fluid anomalies were independently associated with increased risk of dialysis at 1 year (HR 4.47 (1.29–15.45) p = 0.018) (HR 6.99 (1.54 – 31.85) p = 0.012), respectively.27 Thus, the presence of amniotic fluid abnormalities in the fetus with an ultrasound phenotype consistent with ARPKD is associated with increased severity of disease and impacts prenatal course and outcomes.
When considering delivery, the preferred route is vaginal delivery. Some have voiced concerns regarding the possibility of abdominal dystocia due to renal enlargement26; however, this risk is theoretical and evidence is lacking to support recommending an alternative route of delivery. Careful discussion with the patient regarding preferences, future reproductive plans, and risks of cesarean delivery compared to trial of vaginal delivery should be undertaken. It is our practice to routinely offer a trial of vaginal delivery to these patients if the fetus is cephalic.
Early neonatal surveillance may include monitoring of kidney function, pulmonary status, and control of severe arterial hypertension. Patients with ARPKD are also likely to have liver involvement, including biliary duct ectasia and hepatic fibrosis.28 Severity of perinatal and early neonatal disease often determines subsequent clinical course, such as time to progression to ESRD. While approximately 40% of patients with ARPKD will require dialysis by age 15, those with prenatal findings may require more intensive monitoring and care given higher risk of dialysis dependence in infancy and mortality rates are high due to pulmonary hypoplasia caused by anhydramnios or oligohydramnios.29
4.2 |. Nephronophthisis and Nephronophthisis-related ciliopathies
Nephronophthisis (NPHP) is a broad diagnosis for autosomal recessive renal conditions characterized by the formation of multiple cysts within the cortico-medullary region, leading to inflammation, fibrosis, and ultimately ESRD. Histologically, NPHP is characterized by tubular cysts and atrophy with interstitial and polyglomerular fibrosis and tubular basement membrane disruption. Clinically, NPHP is subdivided by age of onset: infantile, juvenile, and adolescent/adult, with more severe forms presenting earlier. Since the initial description of the NPHP1 gene in 1997, more than 20 causative genes have been identified, all of which are involved in primary ciliary structure or function. While variants within several of these genes produce a similar phenotype, they have also been shown to cause a wide spectrum of disorders. However, despite the sharp increase in NPHP-associated genes identified within the last two decades, the underlying genetic etiology of NPHP remains unknown in two-thirds of cases.30
While the majority of NPHP conditions result in isolated renal disease, 10% to 15% of cases are associated with extra renal manifestations as part of clinically recognized syndromes. These polymalformative renal ciliopathy syndromes, sometimes referred to as NPHP-related ciliopathies, are more likely to result in infantile disease and pathologic prenatal findings (Table 2). Additional characteristics common to many ciliopathies include ocular and cerebellar malformations, hepatic fibrosis, and skeletal abnormalities (particularly polydactyly), although a variety of associated anomalies have been described and are dependent upon the underlying genetic cause. Well-described genetic syndromes that have been associated with NPHP are described below and include Meckel-Gruber syndrome and Bardet-Biedl syndrome, Joubert syndrome, and Jeune syndrome. Other, less common NPHP-related syndromes include Senior-Løken syndrome, which results in cystic kidney disease and retinitis pigmentosa30; Cranioectodermal dysplasia (Sebsenbrenner syndrome), characterized by craniofacial, skeletal and ectodermal abnormalities35; Oral-facial-digital syndrome36,7; and renal-hepatic-pancreatic dysplasia syndrome (Ivemark’s syndrome).7,37 With the exception of oral-facial-digital syndrome, which can be X-linked, these disorders are all of autosomal recessive inheritance.9,36,37
TABLE 2.
Genes commonly implicated with renal cystic disease
| Disorder | Gene(s) | Inheritance | Prenatal Presentation | Postnatal Presentation |
|---|---|---|---|---|
| Autosomal dominant polycystic kidney disease (ADPKD) | PKD1, PKD2 | Autosomal dominant | Bilateral cystic kidneys (rare) | Hypertension, progressive renal failure (adult onset) |
| Autosomal recessive polycystic kidney disease (ARPKD) | PHKD1 | Autosomal recessive | Bilateral cystic kidneys | Hypertension, biliary duct dilation (neonatal –childhood onset) |
| ARPKD-like phenotype | HNF1B, DZIP1L | Autosomal recessive, sporadic | Bilateral cystic kidneys | Hypertension, biliary duct dilation (neonatal findings) |
| Meckel-Gruber syndrome (MKS) | MKS1, TMEM216, TMEM67, RPGRIP1L, CEP290, CC2D2A | Autosomal recessive | Multicystic kidneys, occipital encephalocele, polydactyly, possible oligohydramnios | Pulmonary hypoplasia if oligohydramnios; hepatic fibrosis, high postnatal mortality |
| Bardet-Biedl syndrome | BBS1→ 12, MSK1, TMEM67, CEP290 | Autosomal recessive | Large, hyperechogenic kidneys, polydactyly, possible genital anomalies | Retinal abnormalities, obesity, infertility, short stature, anosmia, and renal dysplasia |
| Joubert syndrome | NHPH1, INPP5E, ARL13B, AHI1, CXORF5 (+ all listed MKS genes) | Autosomal recessive | “Molar tooth sign” (hypoplasia of cerebellar vermis)b | Hypotonia, ataxia, intellectual disability, renal dysplasia |
| Jeune syndrome (Jeune asphyxiating thoracic dystrophy) | IFT80, DYNC2H1, WDR35, WDR19 (IFT144) | Autosomal recessive | Small, bell shaped chest, short long bones, polydactylya | Renal dysplasia leading to renal failure, biliary cirrhosis |
| Senior-Løken syndrome | NPH1, NPH4, CEP290, WDR19 (IFT144) | Autosomal recessive | Normal prenatal ultrasound | Nephronopthisis;c Leber congenital amaurosis, rarely liver fibrosis or skeletal anomalies |
| Cranioectodermal dysplasia | WDR35, WDR19 (IFT144), IFT43, IFT122 | Autosomal recessive | Normal prenatal ultrasound | Nephronopthisis,c abnormal facies, brachydactyly, short long bones |
| Oral-facial-digital syndrome | OFD1 | X linked dominant | Polycystic kidneys, brachydactyly | Abnormal facies and oral cavity |
| Renal-hepatic-pancreatic dysplasia (Ivemark’s syndrome) | NPHP3 | Autosomal recessive | Bilateral renal cysts, bile duct dilation, pancreatic cyst (very rare and may vary)d | Neonatal death, If rare survival: chronic jaundice, ESRD, insulin dependent diabetes mellitus |
Note. This table has been adapted from Avni, 2012.7
Prenatal ultrasound imaging of kidneys is typically normal, however exceedingly rarely may include small renal cysts or increased echogenicity of kidneys based on case reports.31,32
Prenatal findings other than molar tooth sign are exceedingly rare and vary. Prior case reports have mentioned polydactyly, renal cysts, ventriculomegaly, polyhydramnios, and hypoplastic phallus.33
Nephronopthisis is defined as multicystic kidneys leading to progressive fibrosis, renal insufficiency, and end stage renal disease.7
Presence of findings are exceedingly rare and vary; if present, have been reported as early as 16 weeks.34
4.2.1 |. Meckel-Gruber syndrome
Meckel-Gruber syndrome (MKS) is an autosomal recessive disorder characterized by MCDK (Figure 3), polydactyly, and occipital encephalocele. Ultrasound findings may include presence of large, hyperechogenic kidneys in addition to other findings. It is uniformly associated with poor outcomes and has a very high rate of mortality for the affected fetus. Hepatic fibrosis is also commonly present. Estimates of incidence vary widely, ranging from 1:9000 live births in Finland, due to founder effect, to 1:140 000 live births in other parts of the world.38 Pathogenic variants in several genes have been shown to cause MKS, including MKS1, TMEM216, TMEM67, RPGRIP1L, CEP290, and CC2D2A.9,39 If prenatal findings are suggestive of MKS, genetic counseling and amniocentesis should be offered, with testing via CMA and targeted molecular panels or trio WES if available (Figure 4–6).
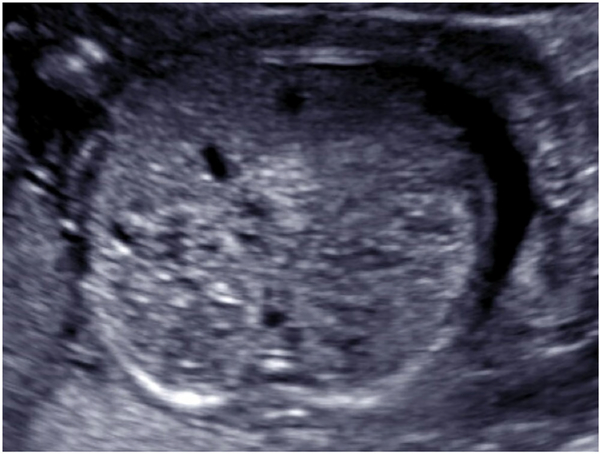
FIGURE 3.
Ultrasound images of a fetus diagnosed with Meckel-Gruber syndrome in the prenatal period. Ultrasound findings included enlarged, hyperechogenic kidneys with cystic foci
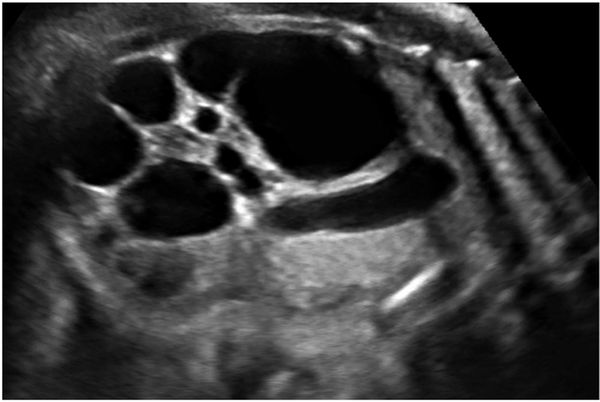
FIGURE 4.
Multicystic dysplastic kidney (MCDK) at 33 weeks. Characteristic appearance of MCDK at 33 weeks. Unilateral kidney demonstrated here; findings are usually bilateral
FIGURE 6.
Enlarged fetal bladder at 11 weeks gestation. Fetal bladder measurements are not available in current image. Diameter of 7 mm in the first trimester is suggestive of fetal microcystis
4.2.2 |. Bardet-Biedl syndrome
Bardet-Biedl syndrome (BBS) is a typically autosomal recessive disorder characterized by retinal degeneration, polydactyly or other extremity anomalies, obesity, intellectual impairment, hypogonadism, and renal malformations. Common ultrasound characteristics suggestive of Bardet Biedl include large hyperechogenic kidneys, sometimes with visible polydactyly and genital anomalies. It is rare, estimated to affect one of 175 000 live births.40 There still remains a wide phenotypic range in BBS, both in the severity of abnormalities and associated secondary features, which include short stature, speech and developmental delay, and endocrine abnormalities, such as diabetes and hypercholesterolemia.9,41 Prognosis depends upon the underlying variant and severity of anomalies, but many patients survive into adulthood. Over 20 genes have been reported in Bardet-Biedl syndrome, including BBS1–12, BBS15, and three genes also implicated in Meckel-Gruber syndrome, MKS1, TMEM67, and CEP290.9 Thus, CMA, targeted molecular testing or trio WES should be offered after genetic counseling when BBS is suspected prenatally.
5 |. MULTICYSTIC DYSPLASTIC KIDNEY
It is estimated that MCDK affects one in 2200 to one in 4300 live births.26 The exact etiology of MCDK is unknown, however, may be secondary to abnormal formation of ureteric bud, teratogens, or urinary tract obstruction.26 Several studies also link MCDK to the HNF1B spectrum of disease, or associate the finding with other ciliopathies, such as Meckel Gruber syndrome (see Table 1).10,1 Thus, referral to genetic counseling and the option of prenatal genetic diagnosis should be offered and discussed. Testing may include CMA, targeted molecular testing, or WES as available.
6 |. NONCYSTIC FETAL RENAL PATHOLOGY
6.1 |. Renal agenesis
Renal agenesis is defined as the absence of one (unilateral) or both kidneys (bilateral). Bilateral renal agenesis occurs in 0.1 to 0.3 of 1000 births and generally has a poor prognosis with little to no chance of survival because of the pulmonary hypoplasia that results because of anhydramnios at the critical stage of lung development (16–20 weeks gestation), although exceptions have been reported.42 Unilateral renal agenesis is seen in one of 1000 pregnancies and has a favorable prognosis when compared with bilateral renal agenesis. Although renal agenesis can be an isolated finding, it may also be part of a syndrome. Various inheritance patterns have been described in families with renal agenesis. If renal agenesis is detected in the fetus, an evaluation of the parents is warranted using renal ultrasound.
Bilateral renal agenesis is diagnosed by ultrasound findings of anhydramnios identified at the time of 18 to 20 week anatomical survey (the placenta produces amniotic fluid in the first trimester and the fetal kidneys start to produce fluid around 15–16 weeks), absent bladder due to lack of filling, absence of renal tissue, and absence of color doppler flow from renal arteries which arise from the aorta.1,43
Conversely, unilateral renal agenesis presents on ultrasound as absence of renal tissue in the renal fossa with the bladder visualized and normal amniotic fluid. The contralateral kidney may be useful to help identify unilateral agenesis because of compensatory hyperplasia of the normal kidney. An anteroposterior (AP) and transverse (TR) diameter ratio of 0.9 or greater has been shown to have high sensitivity, specificity, and accuracy of demonstrating compensatory renal hyperplasia.44
If renal agenesis (unilateral or bilateral) is identified, a detailed ultrasound to view all organ systems is recommended because the risk of genetic syndrome may be as high as 30%.45 Single gene disorders associated with unilateral or bilateral renal agenesis are listed in Table 3.1 Many of these have a variable or limited prenatal phenotype. When renal agenesis is identified prenatally, as with any fetal abnormality, diagnostic testing should be offered. Placental biopsy may be necessary if there is anhydramnios and amniocentesis is not possible. Parental renal ultrasounds can be offered and a careful family history should be obtained. Standard genetic testing (karyotype, CMA) should be performed on the fetal specimen and molecular testing via targeted CAKUT panels or WES, on a research or clinical basis if available, can be considered, especially if other organ systems are affected or there are multiple affected pregnancies with the same phenotype suggestive of a genetic etiology.
TABLE 3.
Renal agenesis (unilateral or bilateral) and related syndromes
| Syndrome (Gene or copy number variant) | Inheritance | Other Anomalies/Renal Agenesis or Other Renal Presentations |
|---|---|---|
| Kallman syndrome (KAL1) | X-linked | Anosmia; hypogonadotropic hypogonadism; renal agenesis |
| Lenz micro-opthalmia (BCOR) | X-linked | Micro-opthalmia; genital abnormalities; renal agenesis |
| Goltz-Gorlin syndrome (PORCN) | X-linked | Dermal hypoplasia; limb defects; cardiac abnormalities; renal agenesis |
| Fraser syndrome (FRAS1) | Autosomal recessive | Crypto-opthalmos; ambiguous genitalia; cutaneous syndactyly; malformed ears; dysplastic kidneys; unilateral or bilateral renal agenesis. |
| Smith-Lemli-Opitz syndrome (DHCR7) | Autosomal recessive | 2–3 toe syndactyly; post-axial polydactyly; growth restriction; cardiac and brain abnormalities; ambiguous genitalia; urinary tract dilation, cystic or hypoplastic kidneys, hypospadias, unilateral or bilateral renal agenesis. |
| Microcephaly, facial dysmorphism, renal agenesis, and ambiguous genitalia syndrome [MFRG syndrome] (CTU2) | Autosomal recessive | Cardiac abnormalities; lissencephaly; skeletal anomalies; polydactyly; founder mutation in Saudi population in a synonymous variant T247 T thought to impair splicing causing a frameshift that causes premature truncation46; renal agenesis. |
| Cat eye syndrome [Inv dup (22)(q11)] | Autosomal dominant | Coloboma of the iris and anal atresia, cardiac abnormalities; renal agenesis. |
| Antley-Bixler syndrome (FGFR2) | Autosomal dominant | Craniosynostosis, joint contractures, choanal atresia, ambiguous genitalia, vertebral anomalies, thin ribs; renal agenesis. |
| Branchio-oto-renal syndrome | Autosomal dominant | Ear anomalies such as ear pits, microtia, anotia, branchial cysts; renal agenesis. |
| Ectrodactly-ectodermal dysplasia-cleft syndrome (P63) | Autosomal dominant | Ectrodactyly; ectrodermal dysplasia; cleft palate; megaureter, ureterocele, renal aplasia, genital anomalies. |
| Townes-Brock syndrome (SALL1) | Autosomal dominant | Imperforate anus; external ear anomalies; deafness; thumb anomalies; renal agenesis. |
| Renal coloboma syndrome (PAX2) | Autosomal dominant | Fetal renal hypodysplasia47–49; renal agenesis. |
| Renal hypoplasia/aplasia (GREB1L) | Autosomal dominant | Bilateral renal agenesis, anhydramnios, unilateral renal agenesis, vesicoureteral reflux |
| Miller Dieker syndrome (LIS1) | Autosomal dominant | Lissencephaly, midface hypoplasia, low set ears, thick upper lip, omphalocele, rare renal agenesis50 |
| Fraser syndrome (FRAS13, FREM2, and GRIP1) | Autosomal recessive | Cryptopthalmos, syndactyly, umbilical hernia, cleft lip and palette, skeletal abnormalities, intellectual delays; renal dysplasia, renal agenesis.51 |
| Goldenhar syndrome (SKI) | Autosomal dominant | Craniosynostosis, hypertelorism, exophthalmos, micrognathia, Marfanoid habitus, developmental delay; rare renal agenesis.50 |
Note. Adapted from Dias et al, 2014.1
6.1.1 |. Treatments for renal agenesis
Once bilateral renal agenesis has been diagnosed, the family should be counseled about the poor prognosis. Case reports have been published regarding serial amnioinfusion showing that with such interventions, there is possibility of survival.42,52 However, given the lack of prospectively collected data and the unknown maternal/fetal risks of serial amnioinfusions, it is not recommended that this be offered outside of a clinical trial52 (at least two are ongoing and registered with clinicaltrials.gov; NCT03101891; NCT03723564). There is no needed treatment for unilateral renal agenesis because amniotic fluid generally is normal, and therefore, fetal lung maturation is not impaired.
Lower urinary tract obstruction (LUTO) or fetal megacystis
LUTO has an estimated incidence of one in 1500 pregnancies.53 It is variably defined and can be diagnosed as early as 11 to 14 weeks gestation.1 The most common definitions include a longitudinal bladder length of greater than 7 mm in the first trimester. In the second trimester and beyond, a sagittal dimension greater than the following measurement is considered diagnostic: gestational age in weeks +12 mm. Other criteria, such as bladder wall thickness, have also been reported, with measurement of the bladder wall greater than 3 mm associated with LUTO.53 Gross bladder appearance has also been used as diagnostic criteria, with the ultrasonographic presence of an abnormally enlarged bladder in the second or third trimester with or without emptying for over 45 minutes.
There are several etiologies underlying LUTO including posterior urethral valves, urethra atresia/stenosis, prune belly syndrome, megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS), and cloacal anomalies. LUTO has a high association with aneuploidy when diagnosed in the first trimester, especially trisomy 18, 13, and 21. Fetal karyotype abnormalities are identified in up to 25% of cases in which megacystis is seen with longitudinal bladder diameter of 7 to 15 mm.53 However, if the megacystis resolves spontaneously, 90% have normal karyotypes. If the longitudinal bladder diameter is greater than 15 mm, the risk of chromosomal defects is noted to be approximately 10%. In this same study, the chromosomally normal group still had progressive obstructive uropathy showing a poor prognosis with bladder diameters of greater than 15 mm.53
6.1.2 |. Posterior urethral valves
Posterior urethral valves affects 3.8 per 100 000 live male births and is the predominant cause of lower urinary tract obstruction in male fetuses. Prenatal ultrasound may show a distended fetal bladder as early as the first trimester (11–14 weeks). Common second trimester ultrasound findings include oligohydramnios, a distended urinary bladder, bilateral hydronephrosis, and obstructive renal dysplasia. In the setting of severe obstruction, massive bladder enlargement could occur due to urine accumulation leading to abdominal muscle atrophy, undescended testes, intestinal malrotation, or pulmonary hypoplasia. Severe oligohydramnios could also lead to a Potter-like syndrome. Endoscopic placement of a vesico-amniotic shunt may be required to decrease the risk of the aforementioned downstream consequences, however, may lead to the neonatal appearance of a wrinkled abdomen, or “Prune Belly syndrome.”54 Early management of lower urinary tract obstruction prevents downstream sequelae, most notably pulmonary hypoplasia. However, long-term complications of vesico-amniotic shunt placement includes bilateral obstructive renal dysplasia and consequent chronic renal failure among surviving infants.54 Fetal cystoscopy is an accurate method in the diagnosis of the etiology of lower urinary tract obstruction (LUTO) and serves as a guide to specific prenatal treatment. Accurate diagnosis of LUTO was made in 92% of cases in a recent series using fetal cystoscopy. However, current use of fetal cystoscopy for diagnostic and treatment modalities is limited to tertiary care centers that offer advanced fetal therapy and further analysis regarding immediate and long-term outcomes is required before routine utilization.55
Notably, few known genes to date are associated with posterior urethral valves. Prune Belly syndrome is associated with HNF1B in 3% of recognized cases, yet the majority of those diagnosed do not have a known genetic cause.54 Posterior urethral valves, pyelectasis, megaureters, are within the array of CAKUT abnormalities that can be associated with Trisomy 21.56 Very rarely, other chromosome abnormalities, such as trisomy of chromosome 11 or partial duplication of chromosome 6 have been associated with UTD, however, data is limited to case reports.57 Thus, the early detection of posterior urethral valves warrants genetic counseling referral, offering diagnostic testing, CMA, possible molecular testing or trio WES if available, and further workup as suspected by prenatal ultrasound findings.
6.1.3 |. Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS)
MMIHS accounts for approximately 1% of cases in which fetal megacystis is prenatally diagnosed. Exact genetic origins and inheritance patterns are unknown; however, an autosomal recessive pattern is suspected. Further, a tendency towards females is also noted with a suspected incidence of 2:1.58 Sonographic findings include a markedly enlarged fetal bladder, bilateral fetal hydronephrosis, and polyhydramnios. Bladder enlargement can progress to massive proportions, eventually enlarging the abdomen and displacing the diaphragm.59
Anomalies of the gastrointestinal tract, such as nonfunctional microcolon primarily contribute to the high morbidity of this rare condition.60 Suspicion of MMIHS should include comprehensive sonographic evaluation for other fetal anomalies, consultation with reproductive genetics, and discussion of pregnancy continuation versus termination with an obstetrician specialized in the care of such high-risk pregnancies. Initial perinatal mortality varies but is suspected to approach 50%. Survival is marked by lifelong morbidity secondary to numerous gastrointestinal and genito-urinary procedures and the potential need for lifelong parenteral nutrition.59
6.1.4 |. Urinary tract dilation
Urinary tract dilation (UTD) occurs in 1% to 2% of all pregnancies and is the most common CAKUT.61 Isolated dilation of a portion of the fetal urinary tract may be caused by a variety of structural abnormaliteis, such as ureteral duplication, ureteropelvic junction (UPJ) obstruction, and posterior urethral valves among others.2 While isolated mild UTD is usually a normal finding, it is important to note that UTD, especially in the presence of other anomalies, can be associated with both aneuploidy and single gene disorders. The finding of UTD is a marker for trisomy 21 with a likelihood ratio of 1.5 and counseling about this information is recommended.56 The clinical phenotypes of urinary tract dilation vary, ranging from inconsequential (most common) to severe obstructive disease (rare). Severe obstructive disease accounts for one third of all cases of pediatric ESRD.3
Prenatal diagnosis of UTD can occur as early as the first trimester, but most commonly occurs during a comprehensive anatomical ultrasound or second trimester scan. Findings that are suggestive of UTD include presence and extent of calyceal dilation, parenchymal abnormalities, bladder and ureteral abnormalities, and low amniotic fluid volume.61 When UTD is identified, the patient should be counseled and offered diagnostic testing or aneuploidy screening based on the patient’s preferences and ultrasound findings. Inclusion of pediatric nephrology and urology should be considered in order to offer further discussion of postnatal diagnosis and management.
6.2 |. Recent genetic advancements in renal pathology
As prenatal WES is being used more commonly62 in cases with fetal abnormalities and in nonviable pregnancies where microarray is normal, new genes have been identified to explain prenatal renal phenotypes.63 In this section, we will focus on discussion of recently identified genes that cause congenital abnormalities of the kidney and urinary tract.
6.2.1 |. GREB1L
Cohorts including fetuses with renal agenesis that had WES revealed deleterious de novo variants in GREB1L pointing to its potential role as a novel candidate gene critical to renal development.64,63 GREB1L encodes for growth regulation by estrogen in breast cancer 1 protein. Studies in mice show that GREB1L is highly expressed in the murine developing kidney. Functional studies in zebrafish were performed to confirm the role of GREB1L in kidney development.65
6.2.2 |. HNF1B
As described in our review of PKD, pathogenic variants in many different genes can mimic ARPKD/ADPKD findings of large, multicystic kidneys diagnosed on prenatal ultrasound. Recent studies have provided evidence that HNF1B may constitute the main cause of prenatally diagnosed bilateral multicystic kidneys. Inherited in an autosomal dominant fashion, HNF1B pathogenic variants commonly result in phenotypes with renal cystic pathology and diabetes. However, an estimated 30% to 50% of diagnosed HNF1B mutations are de novo.12
It is expected that as more prenatal sequencing is performed, additional genes critical to human kidney development will be identified. Given the frequency of prenatal renal abnormalities and relative ease of identifying structural abnormalities in the renal system, further gene discovery specific to renal pathology using prenatal cohorts are expected.
6.3 |. Other syndromes/sequences with prenatal renal abnormalities
6.3.1 |. Phakomatoses
Rarely, phakomatoses such as tuberous sclerosis complex (TSC) and Von Hippel-Lindau (VHL) may be associated with prenatally diagnosed renal abnormalities. Tuberous sclerosis is a neurocutaneous disorder that can present at any age and rarely prenatally. Associated with the TSC1 and TSC2 genes, TSC is most commonly associated with hypomelanotic macules on the skin, but can also lead to multi-organ involvement. Renal involvement may include the presence of renal cysts, angiomyolipomas, and rarely renal cell carcinoma. However, most children with TSC are born with normal kidneys and renal involvement appears later as they age. Prenatal presence of renal lesions is exceedingly rare with only half a dozen cases of renal cysts reported prenatally in the setting of TSC. There are no reported cases of prenatal angiomyolipoma.66,67 VHL is an autosomal dominant condition with incidence of one of 360 000. It is characterized by hemagnioblastomas of the neurologic system and renal cysts with an increased incidence of renal cell carcinoma. Prenatal presence of renal abnormalities has not been reported in the literature to our knowledge.68
Other conditions, such as Smith-Lemli-Opitz syndrome (SLOS) and Fraser syndrome can lead to pansystemic anomalies and intellectual disability, including the presence of renal cystic disease and clinically significant renal functional damage. SLOS is caused by a deficiency of cholesterol synthesis resulting from a deficiency of 7-dehydrocholesterol (7DHC) reductase encoded by the DHCR7 gene and is inherited in an autosomal recessive pattern. Renal anomalies can range from minor functional defects, simple cystic kidney disease, to renal agenesis. The presence of major anomalies may be noted on prenatal ultrasound, however, early detection of multiple malformations was noted in only 10% of postnatally diagnosed cases in one series.69 Similarly rare, Fraser syndrome is a multi-organ system malformation disorder, inherited in an autosomal recessive fashion with an incidence of 0.2 of 100 000 births. Implicated genes include FRAS13, FREM2, and GRIP1. Renal anomalies associated with this condition may include unilateral or bilateral renal agenesis, dysplastic kidneys, and oligohydramnios. Such findings were present in 77% of diagnosed cases in one series of 38 cases.51
Although such conditions are exceedingly rare, immediate family history of this condition should prompt referral to genetic counseling and a comprehensive anatomical ultrasound. If prenatal findings on ultrasound further suspicion of a multiple anomaly syndrome, referral to genetic counseling and maternal fetal medicine specialist is recommended. There, appropriate options regarding pregnancy continuation versus termination should be provided as dictated by fetal prognosis and local availability.
6.3.2 |. Malformation sequences
VATER syndrome (or VACTERL association) is a sequence of anomalies that includes vertebral anomalies, anorectal malformations, cardiac defects, trachea-esophageal fistula and/or esophageal atresia, radial dysplasia/renal anomalies, and limb defects. Genes associated with this complex syndrome include FGF8, FOXF1, HOXD13, LPP, TRAP1, ZIC3. The incidence of renal abnormalities associated with VACTERL ranges from 1:10 000 to 1:40 000. Renal anomalies may include a range of CAKUT, ranging from mild vesicoureteral reflux to renal agenesis. A particular renal phenotype of VACTERL is associated with the TRAP1 gene, in which mouse models demonstrate a higher likelihood of duplex kidney and unilateral renal agenesis.70
MURCS association syndrome stands for Mullerian duct aplasia, unilateral renal agenesis, cervico-thoracic somite fusion defects. Like VACTERL, MURCS is also a sequence syndrome. It is inherited in a sporadic or autosomal dominant fashion and may be associated with copy number changes in the WT1 or PAX2 genes. Typical renal findings include unilateral renal agenesis.
If a fetal malformation sequence disorder is suspected, the affected patient should be offered a comprehensive anatomical ultrasound, maternal fetal medicine, diagnostic testing, and genetic counseling referral. As with any fetal anomaly, discussion of options regarding pregnancy continuation versus termination is recommended.
7 |. APPROACH TO EVALUATION
When prenatal ultrasonographic findings are suspicious for CAKUT, we recommend an individualized approach based on sonographic findings (including appearance of fetal kidney and any extra-renal findings), and parental preferences regarding obtaining a definitive prenatal diagnosis. However, a standard framework for the approach to the care of pregnancies with suspected CAKUT disorders may be helpful to clinicians and patients (Figure 7). All patients with a suspected CAKUT should be offered genetic counseling and care by a multidisciplinary team. Reproductive genetic counselors can assist in providing optimal recommendations for genetic testing depending on clinical findings. This approach should include an initial work-up for chromosomal abnormalities, including a chromosomal microarray (CMA). If normal, proceeding with targeted molecular testing (such as a targeted gene panel) or with trio WES if available, is indicated. From the largest trio WES cohorts with unselected anomalies, the diagnostic yield in CAKUT was 0% (0/16) in the PAGE UK study and 16% (4/16) in the US series.71,72 Another paper on application of WES to CAKUT in the setting of normal CMA showed a detection rate of 2/22 (9.1%) for isolated CAKUT and 2/8 (25%) for CAKUT with other abnormalities. However, larger studies are needed to determine the utility of WES when applied to prenatal CAKUT.73 Serial ultrasonography for fetal surveillance is often utilized, while the approach to antenatal testing and timing of delivery requires individualization. As with any anomaly, the option of termination of pregnancy should be offered and discussion of legal limits specific to the geographic area is indicated. Some conditions such as bilateral renal agenesis and trisomy 13 have a lethal/poor prognosis whereas others, such as urinary tract dilation, usually have a favorable outcome. It is our practice to offer diagnostic testing to all women and provide information on the diagnosis so that the families can make decisions about termination of pregnancy or continuation consistent with their values and beliefs. In the case of severe abnormalities with a poor prognosis, we also offer the option of palliative care in continuing pregnancies. If a fetal or neonatal demise occurs, there is value in fetal/neonatal autopsy with careful attention to pathologic examination of the kidneys and urinary tract as well as utility in extracting DNA for possible genetic testing which can inform future pregnancies.
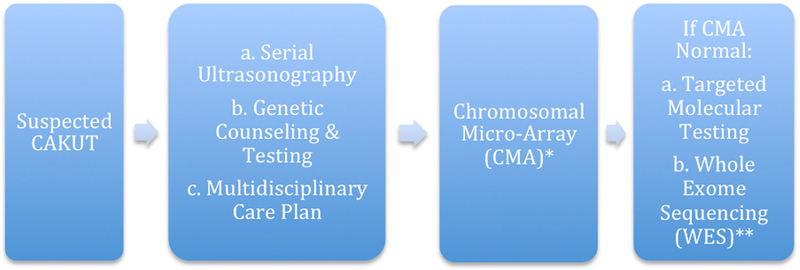
FIGURE 7.
Algorithm for evaluation of suspected congenital anomalies of the kidney and urinary tract (CAKUT). Further management decisions should be based on final diagnosis and expert opinion and practice. *Genetic testing should only be offered by providers with genetics expertise if indicated by the clinical scenario and with appropriate plans for follow-up with a multidisciplinary care team if indicated. **Whole exome sequencing (WES) may be considered in certain situations such as in pregnancies recurrent CAKUT phenotypes (ie, multiple pregnancies with renal agenesis or cystic kidneys)
8 |. CONCLUSIONS
As ultrasound capabilities and prenatal genetic diagnostic testing continue to improve, screening for and diagnosis of CAKUT is a critical part of providing comprehensive antenatal care. CAKUT anomalies present in a number of ways and can be diagnosed as early as 11 weeks gestation, ranging from subtle anomalies to syndromic manifestations affecting not only the genitourinary tract, but also other fetal structures and amniotic fluid. Monogenic disorders associated with CAKUT often require involving providers with genetics expertise to ensure that the genetic testing strategy is appropriate. Early and comprehensive multidisciplinary care may include maternal fetal medicine specialists, genetic counselors, pediatric nephrologists, and pediatric urology as indicated if a CAKUT anomaly is suspected. As such, early prenatal diagnosis is integral to coordination of care when low and high-risk CAKUT phenotypes are suspected.
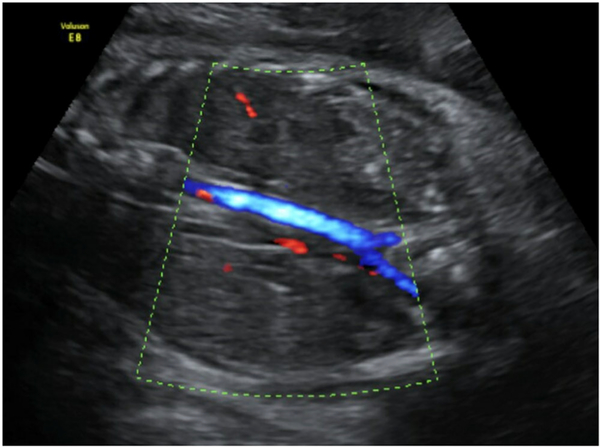
FIGURE 5.
Renal agenesis and absence of color Doppler flow. Ultrasound images obtained in the prenatal period demonstrate bilateral fetal renal agenesis as demonstrated by absent renal arteries, absent bladder, and anhydramnios
What is already known about this topic?
Prenatally, CAKUT abnormalities are often identified and can be isolated to the kidney and urinary tract or be seen in conjunction with other anomalies
Outcomes secondary to such abnormalities range from almost certain mortality (eg, bilateral renal agenesis) to having minimal impact on the affected fetus (eg, urinary tract dilation grade A1).
Prenatal diagnosis of CAKUT includes ultrasound, genetic counseling, and genetic testing and is central to the creation of a fetal/neonatal care plan to optimize outcomes.
What does this review add?
This review provides a summary of syndromic CAKUT disorders that may be identified prenatally and genetic considerations specific to prenatal CAKUT abnormalities.
Given the significant advances in prenatal diagnosis and application of genomics over the last decade, this review is presented at a necessary time when antenatal diagnosis and management of CAKUT are evolving.
We outline genetic considerations for a provider faced with a new diagnosis of CAKUT based on current evidence and expert opinion.
ACKNOWLEDGEMENTS
We would like to thank Nancy Chescheir, MD for providing us with some of the ultrasound images.
Funding information
Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant/Award Number: K23HD088742
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study.
REFERENCES
- 1.Dias T, Sairam S, Kumarasiri S. Ultrasound diagnosis of fetal renal abnormalities. Best Pract Res Clin Obstet Gynaecol. 2014;28(3):403–415. 10.1016/j.bpobgyn.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 2.Vivante A, Kohl S, Hwang D-Y, Dworschak GC, Hildebrandt F. Single-gene causes of congenital anomalies of the kidney and urinary tract (CAKUT) in humans. Pediatr Nephrol. 2014;29(4):695–704. 10.1016/j.joca.2015.05.020.Osteoarthritic [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uy N, Reidy K. Developmental genetics and congenital anomalies of the kidney and urinary tract. J Pediatr Genet. 2015;05(01):051–060. 10.1055/s-0035-1558423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Capone VP, Morello W, Taroni F, Montini G. Genetics of congenital anomalies of the kidney and urinary tract: the current state of play. Int J Mol Sci. 2017;18(4). 10.3390/ijms18040796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.dos Santos Junior ACS, de Miranda DM. Simões e Silva AC. Congenital anomalies of the kidney and urinary tract: an embryogenetic review. Birth Defects Res Part C—Embryo Today Rev. 2014;102(4):374–381. 10.1002/bdrc.21084 [DOI] [PubMed] [Google Scholar]
- 6.Schreuder MF, Bueters RR, Huigen MC, Russel FGM, Masereeuw R, Van Den Heuvel LP. Effect of drugs on renal development. Clin J Am Soc Nephrol. 2011;6(1):212–217. 10.2215/CJN.04740510 [DOI] [PubMed] [Google Scholar]
- 7.Avni FE, Garel C, Cassart M, D’Haene N, Hall M, Riccabona M. Imaging and classification of congenital cystic renal diseases. Am J Roentgenol. 2012;198(5):1004–1013. 10.2214/AJR.11.8083 [DOI] [PubMed] [Google Scholar]
- 8.Woolf AS, Price KL, Scambler PJ, Winyard PJD. Evolving concepts in human renal dysplasia. J Am Soc Nephrol. 2004;15(4):998–1007. [DOI] [PubMed] [Google Scholar]
- 9.Waters AM, Beales PL. Ciliopathies: an expanding disease spectrum. Pediatr Nephrol. 2011;26(7):1039–1056. 10.1007/s00467-010-1731-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kagan KO, Dufke A, Gembruch U. Renal cystic disease and associated ciliopathies. Curr Opin Obstet Gynecol. 2017;29(2):85–94. 10.1097/GC0.0000000000000348 [DOI] [PubMed] [Google Scholar]
- 11.Dillman JR, Trout AT, Smith EA, Towbin AJ. Hereditary renal cystic disorders: imaging of the kidneys and beyond. Radiographics. 2017;37(3):924–946. 10.1148/rg.2017160148 [DOI] [PubMed] [Google Scholar]
- 12.Bergmann C Genetics of autosomal recessive polycystic kidney disease and its differential diagnoses. Front Pediatr. 2018;5(February):1–13. 10.3389/fped.2017.00221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ong ACM, Devuyst O, Knebelmann B, Walz G. Autosomal dominant polycystic kidney disease: the changing face of clinical management. Lancet. 2015;385(9981):1993–2002. 10.1016/S0140-6736(15)60907-2 [DOI] [PubMed] [Google Scholar]
- 14.Rangan GK, Tchan MC, Tong A, Wong ATY, Nankivell BJ. Recent advances in autosomal-dominant polycystic kidney disease. Intern Med J. 2016;46(8):883–892. 10.1111/imj.13143 [DOI] [PubMed] [Google Scholar]
- 15.Srivastava A, Patel N. Autosomal dominant polycystic kidney disease. Am Fam Physician. 2014;90(5):303–307. 10.1358/dof.2006.031.07.995040 [DOI] [PubMed] [Google Scholar]
- 16.Chebib FT, Torres VE. Autosomal dominant polycystic kidney disease: core curriculum 2016. Am J Kidney Dis. 2016;67(5):792–810. 10.1186/s40945-017-0033-9.Using [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergmann C Recent advances in the molecular diagnosis of polycystic kidney disease. Expert Rev Mol Diagn. 2017;17(12):1037–1054. 10.1080/14737159.2017.1386099 [DOI] [PubMed] [Google Scholar]
- 18.Schrier RW, Brosnahan G, Cadnapaphornchai MA, et al. Predictors of autosomal dominant polycystic kidney disease progression. J Am Soc Nephrol. 2014;25(11):2399–2418. 10.1681/ASN.2013111184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erger F, Brüchle NO, Gembruch U, Zerres K. Prenatal ultrasound, genotype, and outcome in a large cohort of prenatally affected patients with autosomal-recessive polycystic kidney disease and other hereditary cystic kidney diseases. Arch Gynecol Obstet. 2017;295(4):897–906. 10.1007/s00404-017-4336-6 [DOI] [PubMed] [Google Scholar]
- 20.Wu M, Yu S. New insights into the molecular mechanisms targeting tubular channels/transporters in PKD development. Kidney Dis. 2016;2(3):128–135. 10.1159/000444839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rangan GK, Alexander SI, Campbell KL, et al. KHA-CARI guideline recommendations for the diagnosis and management of autosomal dominant polycystic kidney disease. Nephrol Ther. 2016;21(8):705–716. 10.1111/nep.12658 [DOI] [PubMed] [Google Scholar]
- 22.Rangan GK, Lopez-Vargas P, Nankivell BJ, et al. Autosomal dominant polycystic kidney disease: a path forward. Semin Nephrol. 2015;35(6):524–537. 10.1016/j.semnephrol.2015.10.002 [DOI] [PubMed] [Google Scholar]
- 23.Lover AA, Harvard KE, Lindawson AE, et al. Regional initiatives for malaria elimination: building and maintaining partnerships. 2017:1–10. [DOI] [PMC free article] [PubMed]
- 24.Tchan M, Savige J, Patel C, et al. KHA-CARI Autosomal dominant poly cystic kidney disease guideline: genetic testing for diagnosis. Semin Nephrol. 2015;35(6):545–549.e2. 10.1016/j.semnephrol.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 25.Woodford LMG, Bissler JJ, Braun MC, et al. Diagnosis and management of autosomal recessive polycystic kidney disease: report of an. J Pediatr. 2014;165(3):611–617. 10.1016/j.jpeds.2014.06.015.CONSENSUS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verghese P, Miyashita Y. Neonatal polycystic kidney disease. Clin Perinatol. 2014;41(3):543–560. 10.1016/j.clp.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 27.Burgmaier K, Kunzmann K, Ariceta G, et al. Risk factors for early dialysis dependency in autosomal recessive polycystic kidney disease. J Pediatr. 2018;199:22–28.e6. 10.1016/j.jpeds.2018.03.052 [DOI] [PubMed] [Google Scholar]
- 28.Mehta L, Jim B. Hereditary renal diseases. Semin Nephrol. 2017;37(4):354–361. 10.1016/j.semnephrol.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 29.Dell KM, Matheson M, Hartung EA, Warady BA, Furth SL. Kidney disease progression in autosomal recessive polycystic kidney disease. J Pediatr. 2016;171(e1):196–201. 10.1186/s40945-017-0033-9.Using [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolf MTF. Nephronophthisis and related syndromes. Curr Opin Pediatr. 2015;27(2):201–211. 10.1097/MOP.0000000000000194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tongsong T, Chanprapaph P, Thongpadungroj T. Prenatal sonographic findings associated with asphyxiating thoracic dystrophy (Jeune syndrome). J Ultrasound Med. 1999;18(8):573–576. 10.7863/jum.1999.18.8.573 [DOI] [PubMed] [Google Scholar]
- 32.Rahmani R, Sterling CL, Bedford HM. Prenatal diagnosis of Jeune-like syndromes with two-dimensional and three-dimensional sonography. J Clin Ultrasound. 2012;40(4):222–226. 10.1002/jcu.20902 [DOI] [PubMed] [Google Scholar]
- 33.Doherty D, Glass IA, Siebert JR, et al. Prenatal diagnosis in pregnancies at risk for Joubert syndrome by ultrasound and MRI. Prenat Diagn. 2005;25(6):442–447. 10.1002/pd.1145 [DOI] [PubMed] [Google Scholar]
- 34.Vijayaraghavan SB, Kamalam M, Raman ML. Prenatal sonographic appearance of congenital bile duct dilatation associated with renal-hepatic-pancreatic dysplasia. Ultrasound Obstet Gynecol. 2004;23(6):609–611. 10.1002/uog.1006 [DOI] [PubMed] [Google Scholar]
- 35.Walczak-Sztulpa J, Eggenschwiler J, Osborn D, et al. Cranioectodermal dysplasia, Sensenbrenner syndrome, is a ciliopathy caused by mutations in the IFT122 gene. Am J Hum Genet. 2010;86(6):949–956. 10.1016/j.ajhg.2010.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franco B, Thauvin-Robinet C. Update on oral-facial-digital syndromes (OFDS). Cilia. 2016;5(1):12 10.1186/s13630-016-0034-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vankalakunti M, Gupta K, Kakkar N, Das A. Renal-hepatic-pancreatic dysplasia syndrome (Ivemark’s syndrome). Diagn Pathol. 2007;2(1):24 10.1186/1746-1596-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salonen R, Norio R. The Meckel syndrome in Finland: epidemiologic and genetic aspects. Am J Med Genet. 1984;18(4):691–698. 10.1002/ajmg.1320180415 [DOI] [PubMed] [Google Scholar]
- 39.Logan CV, Abdel-Hamed Z, Johnson CA. Molecular genetics and pathogenic mechanisms for the severe ciliopathies: insights into neurodevelopment and pathogenesis of neural tube defects. Mol Neurobiol. 2011;43(1):12–26. 10.1007/s12035-010-8154-0 [DOI] [PubMed] [Google Scholar]
- 40.Suspitsin EN, Imyanitov EN. Bardet-Biedl syndrome. Mol Syndromol. 2016;7(2):62–71. 10.1159/000445491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet-Biedl syndrome: results of a population survey. J Med Genet. 1999;36(6):437–446. [PMC free article] [PubMed] [Google Scholar]
- 42.Bienstock JL, Birsner ML, Coleman F, Hueppchen NA. Successful in utero intervention for bilateral renal agenesis. Obstet Gynecol. 2014;124(2 Pt 2 Suppl 1):413–415. 10.1097/AOG.0000000000000339 [DOI] [PubMed] [Google Scholar]
- 43.DeVore GR. The value of color Doppler sonography in the diagnosis of renal agenesis. J Ultrasound Med. 1995;14(6):443–449. [DOI] [PubMed] [Google Scholar]
- 44.Cho JY, Moon MH, Lee YH, Kim KW, Kim SH. Measurement of com pensatory hyperplasia of the contralateral kidney: usefulness for differential diagnosis of fetal unilateral empty renal fossa. Ultrasound Obstet Gynecol. 2009;34(5):515–520. 10.1002/uog.7336 [DOI] [PubMed] [Google Scholar]
- 45.Deshpande C, Hennekam RCM. Genetic syndromes and prenatally detected renal anomalies. Semin Fetal Neonatal Med. 2008;13(3):171–180. 10.1016/j.siny.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 46.Shaheen R, Al-Salam Z, El-Hattab AW, Alkuraya FS. The syndrome dysmorphic facies, renal agenesis, ambiguous genitalia, microcephaly, polydactyly and lissencephaly (DREAM-PL): Report of two additional patients. Am J Med Genet A. 2016;170(12):3222–3226. 10.1002/ajmg.a.37877 [DOI] [PubMed] [Google Scholar]
- 47.Madariaga L, Moriniere V, Jeanpierre C, et al. Severe prenatal renal anomalies associated with mutations in HNF1B or PAX2 genes. Clin J Am Soc Nephrol. 2013;8(7):1179–1187. 10.2215/CJN.10221012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinovic-Bouriel J, Benachi A, Bonniere M, et al. PAX2 mutations in fetal renal hypodysplasia. Am J Med Genet A. 2010;152A(4):830–835. 10.1002/ajmg.a.33133 [DOI] [PubMed] [Google Scholar]
- 49.Hwang D-Y, Dworschak GC, Kohl S, et al. Mutations in 12 known dominant disease-causing genes clarify many congenital anomalies of the kidney and urinary tract. Kidney Int. 2014;85(6):1429–1433. 10.1038/ki.2013.508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adams DJ, Clark DA. Common genetic and epigenetic syndromes. Pediatr Clin North Am. 2015;62(2):411–426. 10.1016/j.pcl.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 51.Tessier A, Sarreau M, Pelluard F, et al. Fraser syndrome: features suggestive of prenatal diagnosis in a review of 38 cases. Prenat Diagn. 2016;36(13):1270–1275. 10.1002/pd.4971 [DOI] [PubMed] [Google Scholar]
- 52.Thomas AN, McCullough LB, Chervenak FA, Placencia FX. Evidence-based, ethically justified counseling for fetal bilateral renal agenesis. J Perinat Med. 2017;45(5):585–594. 10.1515/jpm-2016-0367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taghavi K, Sharpe C, Stringer MD. Fetal megacystis: a systematic review. J Pediatr Urol. 2017;13(1):7–15. 10.1016/j.jpurol.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 54.Rodriguez MM. Congenital anomalies of the kidney and the urinary tract (CAKUT). Fetal Pediatr Pathol. 2014;33(5–6):293–320. 10.3109/15513815.2014.959678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sananes N, Cruz-Martinez R, Favre R, et al. Two-year outcomes after diagnostic and therapeutic fetal cystoscopy for lower urinary tract obstruction. Prenat Diagn. 2016;36(4):297–303. 10.1002/pd.4771 [DOI] [PubMed] [Google Scholar]
- 56.Niamien-Attai C, Bacchetta J, Ranchin B, Sanlaville D, Cochat P. Renal abnormalities in Down syndrome: A review. Arch Pediatr. 2017;24(10):1013–1018. 10.1016/j.arcped.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 57.Chiaramonte C, Bommarito D, Zambaiti E, Antona V, Li Voti G. Genetic basis of posterior urethral valves inheritance. Urology. 2016;95:175–179. 10.1016/j.urology.2016.05.043 [DOI] [PubMed] [Google Scholar]
- 58.Mc Laughlin D, Puri P. Familial megacystis microcolon intestinal hypoperistalsis syndrome: a systematic review. Pediatr Surg Int. 2013;29(9):947–951. 10.1007/s00383-013-3357-x [DOI] [PubMed] [Google Scholar]
- 59.Tuzovic L, Anyane-Yeboa K, Mills A, Glassberg K, Miller R. Megacystis-microcolon-intestinal hypoperistalsis syndrome: case report and review of prenatal ultrasonographic findings. Fetal Diagn Ther. 2014;36(1):74–80. 10.1159/000357703 [DOI] [PubMed] [Google Scholar]
- 60.Gosemann JH, Puri P. Megacystis microcolon intestinal hypoperistalsis syndrome: systematic review of outcome. Pediatr Surg Int. 2011;27(10):1041–1046. 10.1007/s00383-011-2954-9 [DOI] [PubMed] [Google Scholar]
- 61.Nguyen HT, Benson CB, Bromley B, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014;10(6):992–998. 10.1016/j.jpurol.2014.10.002 [DOI] [PubMed] [Google Scholar]
- 62.Best S, Wou K, Vora N, Van der Veyver IB, Wapner R, Chitty LS. Promises, pitfalls and practicalities of prenatal whole exome sequencing. Prenat Diagn. 2018;38(1):10–19. 10.1002/pd.5102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rasmussen M, Sunde L, Nielsen ML, et al. Targeted gene sequencing and whole-exome sequencing in autopsied fetuses with prenatally diagnosed kidney anomalies. Clin Genet. 2018;93(4):860–869. 10.1111/cge.13185 [DOI] [PubMed] [Google Scholar]
- 64.Boissel S, Fallet-Bianco C, Chitayat D, et al. Genomic study of severe fetal anomalies and discovery of GREB1L mutations in renal agenesis. Genet Med. 2018;20(7):745–753. 10.1038/gim.2017.173 [DOI] [PubMed] [Google Scholar]
- 65.Sanna-Cherchi S, Khan K, Westland R, et al. Exome-wide association study identifies GREB1L mutations in congenital kidney malformations. Am J Hum Genet. 2017;101(6):1034 10.1016/j.ajhg.2017.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Leung AKC, Robson WLM. Tuberous sclerosis complex: a review. J Pediatr Health Care. 2007;21(2):108–114. 10.1016/j.pedhc.2006.05.004 [DOI] [PubMed] [Google Scholar]
- 67.Dragoumi P, O’Callaghan F, Zafeiriou DI. Diagnosis of tuberous sclerosis complex in the fetus. Eur J Paediatr Neurol. 2018;22(6):1027–1034. 10.1016/j.ejpn.2018.08.005 [DOI] [PubMed] [Google Scholar]
- 68.van Leeuwaarde RS, Ahmad S, Links TP, Giles RH. Von Hippel-Lindau syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al. , eds. Gene Reviews; Seattle (WA); 2018. [Google Scholar]
- 69.Nowaczyk MJM, Irons MB. Smith-Lemli-Opitz syndrome: phenotype, natural history, and epidemiology. Am J Med Genet Part C Semin Med Genet. 2012;160 C(4):250–262. 10.1002/ajmg.c.31343 [DOI] [PubMed] [Google Scholar]
- 70.Reutter H, Hilger AC, Hildebrandt F, Ludwig M. Underlying genetic factors of the VATER/VACTERL association with emphasis on the “Renal” phenotype. Pediatr Nephrol n.d.;16 AD; 3(11):2025–2033. 10.1002/jmri.25711.PET/MRI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lord J, McMullan DJ, Eberhardt RY, et al. Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. Lancet (London, England). 2019;393(10173):747–757. 10.1016/S0140-6736(18)31940-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petrovski S, Aggarwal V, Giordano JL, et al. Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. Lancet (London, England). 2019;393(10173):758–767. 10.1016/S0140-6736(18)32042-7 [DOI] [PubMed] [Google Scholar]
- 73.Lei T-Y, Fu F, Li R, et al. Whole-exome sequencing for prenatal diagnosis of fetuses with congenital anomalies of the kidney and urinary tract. Nephrol Dial Transplant. 2017;32(10):1665–1675. 10.1093/ndt/gfx031 [DOI] [PubMed] [Google Scholar]