Abstract
OBJECTIVES:
We aim to compare short-term oncological and functional outcomes of salvage focal cryotherapy (SFC) to salvage total cryotherapy (STC) for radiation persistent/recurrent prostate cancer.
METHODS:
We queried the COLD registry for men who underwent SFC and STC of the prostate for radiation persistent/recurrent disease. Propensity score weighting was used to match age at time of treatment, pre-salvage therapy PSA, Gleason sum, and pre-salvage cryotherapy androgen deprivation therapy status. Primary outcome was progression-free survival (PFS).
RESULTS:
A total of 385 men with biopsy-proven persistent/recurrent prostate cancer after primary radiotherapy were included in the study. Median follow-up, age, PSA and Gleason sum pre-salvage cryotherapy was 24.4 months (1st/3rd quartile: 9.8/60.3), 70 years (1st/3rd quartile: 66/74), 4 ng/dl (1st/3rd quartile: 2.7/5.6) and 7 (1st/3rd quartile: 6/8), respectively. After propensity score weighting, patients who were treated with STC did not have a significant difference test in PFS compared to patients treated with SFC on weighted log-rank test (79.8% vs. 76.98%, p= 0.11). SFC was associated with a lower probability of post-treatment transient urinary retention (5.6% vs 22.4%. p<0.001). There were no significant differences in rectal fistula (1.4% vs 3.8, p=0.30), new onset urinary incontinence within 12 months (9.3% vs 15.1%, p=0.19) or new-onset erectile dysfunction within 12 months (52.6% vs 59.6, p=0.47) in the SFC vs STC group, respectively.
CONCLUSIONS:
STC has similar 2-year oncological outcome compared to SFC in the radiation-persistent/recurrent disease population, but patients who underwent SFC have a lower urinary retention rate compared to STC.
Keywords: Salvage Cryotherapy, Localized Prostate Cancer, Focal Therapy, Radiation
Micro Abstract:
Focal therapy has been gaining a lot of interest in recent years. However, there is very limited evidence on salvage focal therapy for radiotherapy persistent/recurrent prostate cancer. We show that salvage focal cryotherapy has similar short-term oncological outcomes but better functional outcomes compared to salvage whole gland therapy for radiotherapy persistent/recurrent prostate cancer. Salvage focal cryotherapy may be a promising salvage treatment option for select men with limited intraparenchymal, localized and non-metastatic radiotherapy persistent/recurrent prostate cancer.
Introduction
Localized prostate cancer (PCa) treated with external beam radiation therapy or brachytherapy results in biochemical recurrence in more than 50% of cases within 10 years.[1–3] The rate of biochemical recurrence differs based on the initial risk group, with studies reporting that patients with higher Gleason score, higher prostate-specific antigen (PSA) and higher clinical stage having greater risk of biochemical relapse.[1]
The treatment of radiation-persistent disease remains a challenge and should be tailored to the individual patient. Once the recurrence is deemed to be confined to the prostate based on imaging studies, these patients may be suitable candidates for localized therapy. These therapies include salvage prostatectomy with lymph node dissection, cryotherapy, high-intensity focused ultrasound or brachytherapy. Each of these therapies comes with its own risk of adverse events.
In recent years, two small case series have reported that salvage focal cryotherapy (SFC) result in better erectile function, urinary continence and less urinary retention outcomes compared to salvage total cryoablation (STC).[4, 5] The aim of our study is to compare the short-term oncological efficacy and functional outcomes for SFC versus STC following salvage cryotherapy for radiation persistent/recurrent disease in a large cryotherapy registry.
Methods
Cohort
We performed a retrospective review of a prospectively maintained database - the Cryo On-Line Database (COLD) Registry to identify men who were treated with SFT and STC of the prostate between 1992 and 2017 for clinically localized, histologically identified adenocarcinoma of the prostate following radiation therapy. Inclusion criteria for the analysis were men who underwent biopsy per physician’s judgement and were found to have a positive biopsy or men who met the Phoenix criteria (Nadir + 2 ng/mL). Exclusion criteria were men who had a post-radiation PSA above 10 at the time of salvage treatment and men above the age of 80 years at the time of salvage treatment. We selected these exclusion criteria as these men are not candidates for salvage therapy and excluding these men would remove the risk of misclassification in the registry. SFC and STC was performed at the discretion of the treating physician.
Aim
Primary outcome was progression-free survival (PFS). Secondary outcomes included post-treatment urinary incontinence, new onset erectile dysfunction, rectal fistulae, and urinary retention.
Clinical and Demographic Data
Variables of interest were age (in years, continuous), race (white, black, other), pre-salvage data including PSA (ng/ml, continuous), Gleason score prior to salvage therapy (Gleason sum), pre-salvage cryotherapy androgen deprivation therapy (yes/no), total prostate volume (TPV) at time of salvage treatment (cm3, continuous), post-salvage cryotherapy data including nadir PSA (ng/ml), time to reach PSA nadir (months) and follow-up (months). Biochemical recurrence was defined by the Phoenix criteria as PSA nadir +2 ng/ml. Urinary incontinence is defined by any degree of urine leakage in patients who did not have any urine leakage prior to salvage cryoablation as measured at 12 months follow up. New onset erectile dysfunction was defined as an inability to achieve an erection by patients who were able to achieve erections prior to salvage cryoablation at 12 months follow up with or without pharmacologic therapy.
The COLD Registry is a prospective online database for academic and community urologists to aggregate real-world cryotherapy outcomes. The registry consists of 37 sites and is supervised by board members comprising of practicing urologists. An independent audit of the clinical data is conducted yearly to ensure the accuracy of the data. The registry data is sponsored by HealthTronics (Austin, TX), and data collection was performed by an independent research company (Watermark Research Partners, Indianapolis, IN). All participating sites had approval from their institutional review board if required before submitting their data to the registry with a global institutional review board since 2006. As a registry, there is no prescribed protocol to mandate such as which patients undergo post-cryoablation biopsy, or what treatment template to use, and this was left to the individual physician’s judgement.
Statistical Analysis
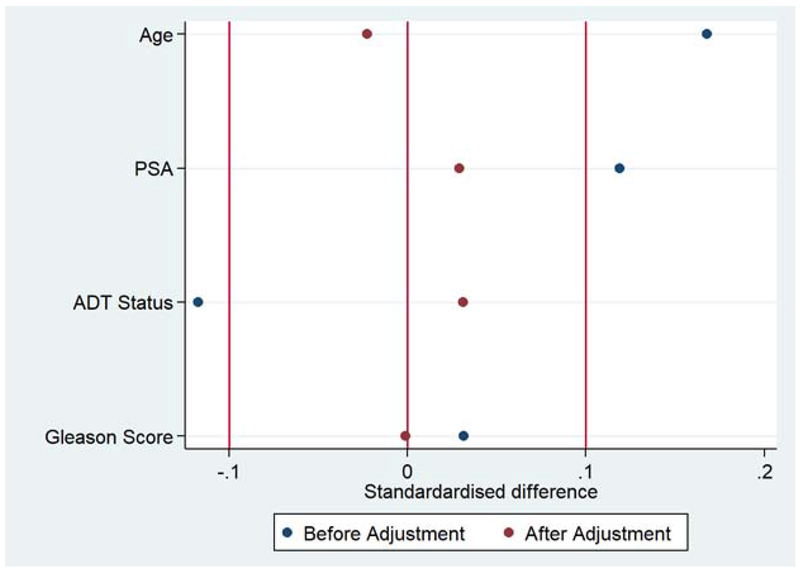
Data are presented as medians, 1st and 3rd quartile, and counts or frequencies with percentages or proportions. Categorical variables were assessed by nonparametric methods using the chi-square test. Given the distribution of the covariates across the salvage focal and salvage whole gland group differed and the cox-proportionate hazards assumption was not met, we performed a propensity score weighting to match patients treated with salvage focal cryoablation to patients treated with salvage total cryotherapy rather than a multi-variate cox proportionate regression model. Matching variables included age at time of salvage treatment, pre-salvage treatment PSA, Gleason sum and pre-salvage cryotherapy androgen deprivation therapy (ADT) status. We chose not to include type of radiation and year of salvage therapy into the propensity model to avoid over fitting the model. However, we created a second propensity model which included these variables as a sensitivity analysis. Standardized difference was used to report the differences between salvage focal therapy and salvage total cryoablation given it is a better method to calculate effect size compared with the p-value.[6] A standardized difference of under 10% (−0.1 to 0.1) is considered statistically indifference between both groups.[7] Survival analysis was depicted using a weighted Kaplan-Meier plot. Statistical significance was defined as p < 0.05. Data was analyzed using STATAv14.0 (StataCorp LP, College Station, TX, USA).
Results
Baseline Characteristics
A total of 385 men with biopsy-proven persistent/recurrence disease after primary radiotherapy were included in the study. 72 men (18.7%) underwent SFC whereas 313 men (81.3%) underwent STC. The median follow-up after salvage cryotherapy was 24.4 months (1st/3rd quartile: 9.8/60.3 months). The median age at time of salvage cryotherapy was 70 years (1st/3rd quartile: 66/74). The majority of patients were white - 308 (80%), followed by black-52 (13.5%) and others - 23 (6%).
Regarding pre-salvage information, 289 (75%) of patients underwent external beam radiation therapy, 62 (16%) underwent brachytherapy and 35 (9%) underwent a combination of both treatments. The median PSA prior to salvage cryoablation was 4 ng/ml (1st/3rd Quartile: 2.7/5.6 ng/ml) and the median Gleason score was 7 (1st/3rd quartile 6/8). Pre-salvage cryotherapy ADT was initiated in 98 (31%) patients. Baseline patient characteristics for variables before and after propensity score weighting are presented in Table 1. Figure 1 illustrates the standardized difference before and after propensity score weighting.
Table 1:
Baseline patient characteristics for unmatched and matched patient cohorts.
| Variable | Unweighted patient cohort | Weighted patient cohort | ||||
|---|---|---|---|---|---|---|
| Salvage focal cryotherapy, n=72, (%) | Salvage whole gland cryotherapy, n=313, (%) | p-value | Salvage focal cryotherapy (%) | Salvage whole gland cryotherapy (%) | p-value | |
| Age, years | ||||||
| <60 | 8 (11.1) | 27 (8.6) | 0.03 | 15.3 | 8.2 | 0.37 |
| 61-70 | 23 (31.9) | 140 (44.7) | 32.0 | 44.1 | ||
| 71-80 | 41 (56.9) | 146 (46.7) | 52.6 | 47.6 | ||
| PSA, ng/mL | ||||||
| ≤1 | 2 (2.8) | 6 (1.9) | <0.01 | 2.9 | 2.0 | 0.45 |
| 1-1.99 | 12 (16.7) | 37 (11.8) | 16.2 | 11.8 | ||
| 2-4.99 | 32 (44.4) | 168 (53.7) | 43.2 | 53.9 | ||
| 5-9.99 | 26 (36.1) | 102 (32.6) | 37.7 | 32.2 | ||
| Unknown | 0 (0) | 14 (3.72) | ||||
| Gleason Score | ||||||
| ≤6 (%) | 31 (45.6) | 107 (34.2) | 0.46 | 36.9 | 35.4 | 0.73 |
| 7 (%) | 26 (38.2) | 108 (34.5) | 38.0 | 34.6 | ||
| ≥ 8 (%) | 5 (7.4) | 84 (26.8) | 16.6 | 25.9 | ||
| Unknown (%) | 6 (8.8) | 14 (4.5) | 8.5 | 4.1 | ||
| ADT | ||||||
| Yes (%) | 19 (26.4) | 98 (31.3) | 0.85 | 29.0 | 30.4 | 0.18 |
| No (%) | 52 (72.2) | 209 (66.8) | 69.2 | 67.8 | ||
| Unknown (%) | 1 (1.4) | 6 (1.9) | 1.8 | 1.8 | ||
PSA: Prostate Specific Antigen; ADT: Androgen Deprivation Therapy
Figure 1:
Standardized difference in means for age, PSA, pre-salvage therapy ADT status and Gleason score for salvage focal cryotherapy and salvage total cryotherapy groups. PSA: Prostate Specific Antigen; ADT: Androgen Deprivation Therapy.
Oncologic Outcomes
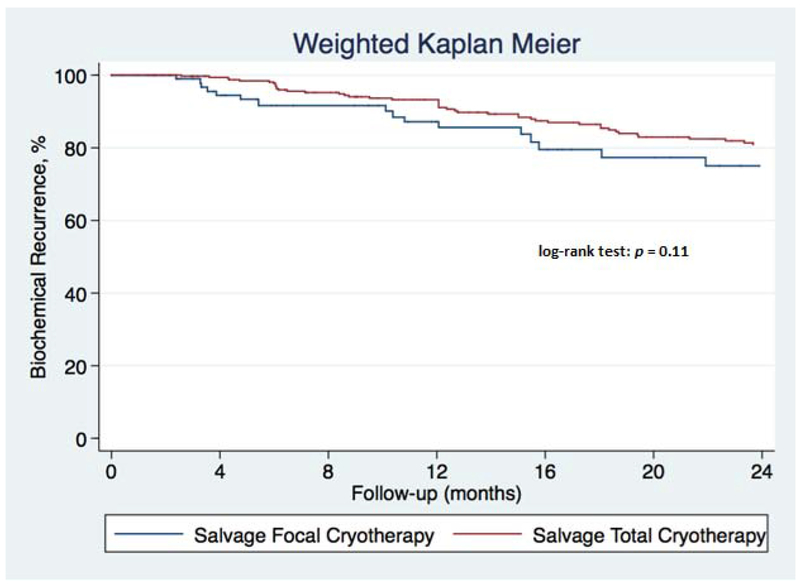
Biochemical recurrence after salvage cryotherapy was identified in 16 patients (22.2%) of the 72 patients in the SFC group and 65 of 302 patients (21.5%) in the STC group, p=0.9. Only 74 (19.2%) patients underwent for-cause prostate biopsy following salvage cryotherapy. There was no significant difference in the rate of positive biopsies in the SFC group vs STC group (33.3% vs. 24.3%), p=0.30. After propensity score weighting, patients who were treated with SFC did not have a significant difference in PFS compared to patients treated with STC on weighted log-rank test (76.98% vs 79.8%, p= 0.11) (Figure 2).
Figure 2:
Kaplan-Meier plot of salvage focal cryotherapy and salvage total cryotherapy with biochemical recurrence.
Functional Outcomes
SFC was associated with a lower probability of post-treatment, transient urinary retention (5.6% vs. 22.4%, p<0.001). There were no significant differences in rectal fistula (1.4% vs 3.8%, p=0.30), new onset urinary incontinence within 12 months (9.3% vs 15.1%, p=0.19) or new-onset erectile dysfunction within 12 months (52.6% vs 59.6%, p=0.47) in the SFC vs STC group, respectively.
Sensitivity Analysis
Sensitivity analysis was performed matching for pre-salvage treatment PSA, Gleason sum, type of radiation therapy and year of salvage cryoablation, and this did not alter the outcomes.
Discussion
The current National Comprehensive Cancer Network (NCCN) guidelines recommends observation, radical prostatectomy with pelvic lymph node dissection, cryotherapy, HIFU or brachytherapy for biopsy-proven local recurrence of PCa in the absence of distant metastases following primary radiation therapy.[8] The guideline does not address salvage focal therapy after primary radiation therapy given there is limited data on subject. In this study, we aim to determine the difference in oncological and functional outcome for patients undergoing salvage focal cryotherapy and salvage whole gland cryotherapy.
We believe this finding is important as focal therapy for prostate cancer has been gaining traction in the past decade. The basis of focal therapy is shaped around the hypothesis of the index lesion, defined as the biologically dominant lesion that drives disease progression in prostate cancer.[9] However, given that interpretation of the Gleason score after definitive RT and ADT is challenging, the index lesion hypothesis is even more provocative in the salvage setting and it is not yet known if the same concepts apply in this setting.[10] Also, patients who have undergone radiation therapy might harbor more aggressive disease as most of these tumors have radiation-resistant phenotypes.[11] In our study, we found that SFC has similar short-term oncological outcome and a lower rate of urinary retention compared to STC of the prostate.
Given the lack of consensus on the definition of biochemical recurrence after salvage cryotherapy of the prostate, we used the Phoenix criteria as applied to post-RT recurrence. [12–14] To the best of our knowledge, there have only been 3 smaller series reporting outcomes after SFC and all 3 studies used the Phoenix criteria to define biochemical recurrence. Only one study by Eisenberg et al reported a 2-year biochemical recurrence rate of 79% for SFC while the other 2 studies reported 5-year disease-free survival of 47% and 54% respectively.[4, 5, 12] Our study reports 77% progression-free survival at 2 years in the SFC group. Previously, Li et al also used the COLD registry to identify patients who underwent salvage focal cryoablation with curative intent.[15] However, our paper defer from what was previously published given we chose to exclude patients with no follow up and patients who would not meet criteria for salvage therapy. We excluded men who had post-radiation PSA above 10 at time of salvage treatment and men above the age of 80 years at the time of salvage treatment.
The three most common adverse events for salvage therapy for prostate cancer are erectile dysfunction, urinary incontinence and rectal fistulas. Similar to salvage surgery, STC of the prostate may be associated with these morbidities. However, contrary to STC, SFC has a lower adverse events rate.[4, 5, 12] One series showed that the new onset ED rate was 71% in the SFC group compared to 85% in the STC group.[4] In our study, we did not identify a similar finding. Our ED rate was lower in both groups but there was no statistical difference between patients who were treated with SFC vs STC (52.6% vs 59.6%).
Previous studies have also shown that the urinary incontinence rate following SFC is 0-5.3% and 0-13% following STC.[4, 5] In our study, the incontinence rate following SFC and STC was 9.3 and 15.1% respectively. We believe this is because the COLD registry uses an extremely strict ‘no pad’ definition of continence, given there is no standard metric to quantify urinary incontinence. Even with such a definition, we found that both focal and total salvage cryoablation of the prostate had a lower urinary incontinence rate when compared to salvage prostatectomy, which is between 21 and 90% in open series and 67-78% in minimally-invasive series.[16] Also, the severity of incontinence based of the number of pads required per day in salvage prostatectomy series is higher than salvage cryotherapy.[16]
In terms of urinary retention rate, our study showed that SFC was associated with a lower probability of post-treatment, transient urinary retention compared to STC. Our study also concurs with other smaller series whereby the rate of recto-urethral fistula after SFC is between 1 to 3.4% and 0 to 5.5% following STC.
Our study has several limitations and must be interpreted within context. First, selection bias is present due to the study’s retrospective nature. SFC and STC was performed at the discretion of the treating physician. Also, there was only 72 patients in the SFC group compared to 313 men in the STC group. To address this, we performed a propensity score matching, but matching does not account for unmeasured factors that may bias one surgical technique over the other. Second, recurrence was defined based on the Phoenix criteria, which is likely underestimating the true incidence of recurrence. A better end-point for this study would be to obtain post-treatment biopsies on all patients. In our study, only 19% of patients underwent a post-treatment for-cause biopsy at the discretion of the treating physician. Although relatively low, this is consistent with a recent systematic review of oncological and functional outcomes of primary prostate focal cryotherapy for localized PCa, showing that only 17% of men had a post-treatment biopsy, highlighting the difficulties in implementing a mandatory follow-up biopsy.[17] Third, 31% of patients received pre-salvage cryotherapy ADT. We are unable to determine the rationale for this. Patients qualified for salvage cryotherapy at the discretion of the treating physicians. Fourth, we did not use any standardized quality-of-life instruments to define functional outcomes. This is because the COLD registry was formed at a time that pre-dated the adoption and widespread utilization of such validated tools. Fifth, multi-parametric MRI of the prostate is now routinely obtained prior to focal therapy, especially in the primary setting.[18] The COLD registry did not capture the use of imaging, hence we are not able to determine the factors that contributed to the clinician deciding on SFC vs STC. There was also no means to determine whether the positive biopsy prior to SFC/STC was in the same location as the original biopsy prior to radiation therapy. Likewise, we are not able to determine whether the positive biopsy after salvage cryotherapy occurred in or out of the treatment field. Finally, the follow-up was only a median of 24.2 months, and this may be insufficient to determine true biochemical recurrence after salvage therapy but is usually of sufficient length to comment on early oncological control and on functional outcomes. For men who have limited and defined intraprostatic cancers in the absence of extra-prostatic disease, the concept of a targeted salvage ablative therapy is intriguing and may be beneficial in the well-selected patient.
Despite these limitations, we present the largest study to date comparing the oncological and functional outcomes of men undergoing SFC or STC post-primary radiation therapy. The COLD registry represents a community of clinician’s experience with cryosurgery and thus is a more accurate snapshot of what is occurring across the United States, in contrast to a single high-volume institution. We have shown for the first time that there is no significant difference in short-term oncological outcomes between SFC and STC post-primary radiation therapy after propensity weighting. Given the narrow confidence intervals, this indicates that increasing the sample size is unlikely to change the results since there is minimal variance between the groups. However, there is a clear separation between the Kaplan-Meier curves (Figure 2), even though the log-rank test showed no statistical difference between both groups at 2 years. Hence, the overall survival may ultimately be shorter in the patients treated with SFC compared to STC but this study was not designed to evaluate for that.
Conclusion
Men treated with SFC have no statistical difference in 2-year PFS and post-treatment biopsy compared to men treated with STC following biopsy-proved radiation resistant disease. Men undergoing SFC are also associated with a lower risk of urinary retention compared to men treated with STC for radiation-persistent PCa. SFC may be a promising salvage treatment option for select men with limited intraparenchymal, localized and non-metastatic radio-persistent
Clinical Practice Points:
Salvage focal cryotherapy has similar short-term oncological outcome, erectile dysfunction rate, urinary incontinence rate and rectal fistula rate compared to salvage whole gland cryotherapy.
Salvage focal cryotherapy has a lower rate of urinary retention compared to salvage whole gland cryotherapy.
Acknowledgments
Disclosures
TJP has a training consultant agreement with Endocare.
WPT is supported by the Ruth L. Kirschstein NRSA Institutional Research Training Grant (T32-CA093245).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Shipley WU, Thames HD, Sandler HM, et al. Radiation therapy for clinically localized prostate cancer: A multi-institutional pooled analysis. JAMA. 1999;281:1598–604. [DOI] [PubMed] [Google Scholar]
- [2].Neppl-Huber C, the ESWG, Zappa M, the ESWG, Coebergh JW, the ESWG, et al. Changes in incidence, survival and mortality of prostate cancer in Europe and the United States in the PSA era: additional diagnoses and avoided deaths. Annals of Oncology. 2012;23:1325–34. [DOI] [PubMed] [Google Scholar]
- [3].Zietman AL, Shipley WU, Willett CG. Residual disease after radical surgery or radiation therapy for prostate cancer. Clinical significance and therapeutic implications. Cancer. 1993;71:959–69. [DOI] [PubMed] [Google Scholar]
- [4].de Castro Abreu AL, Bahn D, Leslie S, Shoji S, Silverman P, Desai MM, et al. Salvage focal and salvage total cryoablation for locally recurrent prostate cancer after primary radiation therapy. BJU international. 2013;112:298–307. [DOI] [PubMed] [Google Scholar]
- [5].Eisenberg ML, Shinohara K. Partial salvage cryoablation of the prostate for recurrent prostate cancer after radiotherapy failure. Urology. 2008;72:1315–8. [DOI] [PubMed] [Google Scholar]
- [6].Sullivan GM, Feinn R. Using Effect Size-or Why the P Value Is Not Enough. Journal of graduate medical education. 2012;4:279–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Austin PC. Using the Standardized Difference to Compare the Prevalence of a Binary Variable Between Two Groups in Observational Research. Communications in Statistics - Simulation and Computation. 2009;38:1228–34. [Google Scholar]
- [8].National Comprehensive Cancer Netowrk. Prostate Cancer (Version 4.2018). . [Google Scholar]
- [9].Ahmed HU, Dickinson L, Charman S, Weir S, McCartan N, Hindley RG, et al. Focal Ablation Targeted to the Index Lesion in Multifocal Localised Prostate Cancer: a Prospective Development Study. European urology. 2015;68:927–36. [DOI] [PubMed] [Google Scholar]
- [10].Epstein JI, Allsbrook WC Jr., Amin MB, Egevad LL. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. The American journal of surgical pathology. 2005;29:1228–42. [DOI] [PubMed] [Google Scholar]
- [11].Sandler HM, Dunn RL, McLaughlin PW, Hayman JA, Sullivan MA, Taylor JM. Overall survival after prostate-specific-antigen-detected recurrence following conformal radiation therapy. International journal of radiation oncology, biology, physics. 2000;48:629–33. [DOI] [PubMed] [Google Scholar]
- [12].Wenske S, Quarrier S, Katz AE. Salvage Cryosurgery of the Prostate for Failure After Primary Radiotherapy or Cryosurgery: Long-term Clinical, Functional, and Oncologic Outcomes in a Large Cohort at a Tertiary Referral Centre. European urology. 2013;64:1–7. [DOI] [PubMed] [Google Scholar]
- [13].Ahmed HU, Cathcart P, McCartan N, Kirkham A, Allen C, Freeman A, et al. Focal salvage therapy for localized prostate cancer recurrence after external beam radiotherapy: a pilot study. Cancer. 2012;118:4148–55. [DOI] [PubMed] [Google Scholar]
- [14].Roach M, Hanks G, Thames H, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: Recommendations of the RTOG-ASTRO Phoenix Consensus Conference. International Journal of Radiation Oncology*Biology*Physics. 2006;65:965–74. [DOI] [PubMed] [Google Scholar]
- [15].Li YH, Elshafei A, Agarwal G, Ruckle H, Powsang J, Jones JS. Salvage focal prostate cryoablation for locally recurrent prostate cancer after radiotherapy: initial results from the cryo on-line data registry. The Prostate. 2015;75:1–7. [DOI] [PubMed] [Google Scholar]
- [16].Chade DC, Eastham J, Graefen M, Hu JC, Karnes RJ, Klotz L, et al. Cancer control and functional outcomes of salvage radical prostatectomy for radiation-recurrent prostate cancer: a systematic review of the literature. Eur Urol. 2012;61:961–71. [DOI] [PubMed] [Google Scholar]
- [17].Tay KJ, Polascik TJ. Focal Cryotherapy for Localized Prostate Cancer. Archivos espanoles de urologia. 2016;69:317–26. [PubMed] [Google Scholar]
- [18].Scheltema MJ, Tay KJ, Postema AW, de Bruin DM, Feller J, Futterer JJ, et al. Utilization of multiparametric prostate magnetic resonance imaging in clinical practice and focal therapy: report from a Delphi consensus project. World journal of urology. 2017;35:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]