Abstract
Background:
In sub-Saharan Africa, trauma is a leading cause of mortality in people less than 45 years. Injury mechanism and cause of death are difficult to characterize in the absence of pre-hospital care and a trauma surveillance database. Pre-hospital deaths (PHD) and in-hospital deaths (IHD) of trauma patient were compared to elucidate comprehensive injury characteristics associated with mortality.
Methods:
A retrospective, descriptive analysis of adults (≥13 years) presenting to Kamuzu Central Hospital in Lilongwe, Malawi, from February 2008 to May 2018 was performed. Utilizing an emergency department-based trauma surveillance database, univariate and bivariate analysis was performed to compare patient and injury characteristics of pre-hospital and in-hospital deaths. A Poisson multivariate regression was performed, predicting the relative risk of PHD.
Results:
Between February 2008 and May 2018, 131,020 adult trauma patients presented to KCH, with 2007 fatalities. Of those patients, 1130 (56.3%) and 877 (43.7%) were PHD and IHD, respectively. The majority were men, with a mean age of 33.4 years (SD 12.1) for PHD and 37.4 years (SD 15.5) for IHD, (p<0.001). Head injuries (n=545, 49.2% vs. n=435, 49.7%) due to assaults (n=255, 24.7% vs. n=178, 21.8%) and motor vehicle collisions (MVC) (n=188, 18.2% vs. n=173, 21.2%) were the leading cause of both groups (PHD vs. IHD). Transportation to the hospital was primarily police (n=663, 60.1%) for PHD and ambulance (n=401, 46.4%) for IHD. Patients who were transported to KCH by the police (RR 1.97, 95% 1.52 – 2.55, p<0.001) when compared to transport via minibus had an increased relative risk of PHD. Patients with a head or spine (RR 1.32, 95% CI 1.34 – 1.53, p<0.001), chest (RR 1.34, 95% CI 1.11 – 1.62, p=0.002), or abdomen and pelvis (RR 1.30, 95% CI 1.14 – 1.53, p=0.004) when compared to extremity injury had an increased relative risk of PHD.
Conclusions:
Head injury from assaults and MVC is the leading cause of PHD and IHD in Malawi. The majority of patients are transported via police if PHD. Of IHD patients, the majority are transported by ambulance, most often from outside hospitals. Both are consistent with the absence of a pre-hospital system in Malawi. Improving pre-hospital care, with a particular focus on head injury and strategies for vehicular injury prevention within a trauma system will reduce adult trauma mortality in Malawi.
Introduction
Trauma remains the leading cause of death and disability in people between 1 and 44 years-old.1 Injury-related morbidity and mortality is a neglected health concern in many low- and middle-income countries (LMIC) and accounts for approximately 90% of all global cases of trauma-related mortality.2 Significant contributors to the high rate of morbidity and mortality, particularly in LMIC, are interpersonal violence and road traffic injuries.3,4 Across much of sub-Saharan Africa, patients with emergency medical and traumatic conditions are often limited in their ability to access higher-level hospitals directly. Access is limited in part to patient transportation barriers, ineffective referral networks, and limited or nonexistent pre-hospital emergency medical services.5,6
Emergency medical services (EMS) are defined as the system that organizes all aspects of care provided to patients in the pre-hospital or out-of-hospital environment.7 Hence, EMS is a critical component of the health systems and is necessary to improve outcomes of injuries and other time-sensitive illnesses. The true scope of EMS in LMIC, delivery of pre-hospital care, and the proportion of need being met remains unknown.8 A recent analysis demonstrated less than one in three African countries has a pre-hospital EMS in place. This results in a limited capacity to respond, evaluate, treat, and safely transport critically ill patients.9
Most studies regarding the burden of trauma rely on hospital-based trauma registries, and hence, the focus of the evaluation of trauma systems has been oriented towards in-hospital care. This has led to significant underestimation of trauma-associated mortality as pre-hospital deaths are typically not captured. As a result, little is known about the epidemiology of those patients who die in the pre-hospital setting.
In Malawi, a small, landlocked country in southeast Africa, there is a lack of an organized trauma system, and pre-hospital trauma care is nonexistent. The mechanism by which patients reach a hospital is variable and unpredictable. Following motor vehicle collisions, the police will usually bring the victims to the closest hospitals. Depending on the level of care required, an ambulance may transfer patients to a higher-level hospital. this study, we aim to describe the variation in the epidemiology, injury characteristics, and risk factors between patients with pre-hospital versus in-hospital deaths presenting to our trauma center in Malawi to better elucidate areas for improvement in pre-hospital care.
Method
This study is a retrospective database analysis of prospectively collected Kamuzu Central Hospital (KCH) Trauma Surveillance Registry from February 2008 to May 2018, which includes all patients presenting to KCH with traumatic injuries. All adult patients, greater than or equal to 13 years, who were brought in dead, died in casualty, or died during their admission were included in the study. Patients were excluded if age or outcome variables were missing.
KCH is the tertiary center for the central region of Malawi. It is a 900-bed hospital with a catchment of 6 million persons. The hospital contains a 4-bed casualty department, 6-bed intensive care unit, and 5-bed high-density unit, as well as both female and male wards. Clinical officers, medical doctor interns and surgical residents staff the KCH casualty department, and trauma care is provided by general surgery, orthopedic consultant consultants, general surgery residents, and clinical officers. During the study period, there was only one neurosurgeon in the central region of Malawi and a total of two neurosurgeons in the entire country. CT scan capability only became available in 2014 at KCH. There is minimal critical care capacity following traumatic brain injury and invasive intracranial pressure monitoring is nonexistent.
Death was the primary outcome for the study and was categorized into pre-hospital death (PHD) and in-hospital death (IHD). PHD was defined as patients who presented to the casualty department deceased. IHD was defined as death occurring while the patient was in casualty or during hospital admission.
Univariate analysis was performed to evaluate the missing data and distribution of variables. Bivariate analysis was performed over PHD versus IHD. Central tendencies were described with means (standard deviations [SD]) and median (interquartile ranges [IQR]) for normally and non-normally distributed variables, respectively. χ2 for categorical variables, Student’s T-Test for normally distributed continuous variables, and Kruskal-Wallis for non-normally distributed continuous variables were used to compare central tendencies.
A Poisson multivariate regression was performed to determine the relative risk of a priori, were age, presenting as a PHD to KCH. Covariates included in the regression, a priori were age, primary injury location, time to presentation, and night presentation. Covariates were included after bivariate analysis if p<0.05, which included sex, mode of transport, transfer status, and injury mechanism. A backward elimination approach was utilized to reduce error in the model. Variables were removed based on p-value and confirmed to maintain precision and reduce bias by narrowing of the confidence intervals and less than a 10% change in coefficients, respectively. Sex, night presentation, and time to presentation were removed based on these criteria.
This analysis was performed with StataCorp v16.0, College Station, Texas. The Malawi National Health Science Research Committee and the University of North Carolina Institutional Review Board approved this study.
Results
Throughout the study, 131,020 patients were registered in the KCH Trauma Surveillance Registry, and 92,471 (70.6%) were greater than or equal 13 years of age. Overall, 2,007 (2.2%) patients died. Of the 12,929 admissions during the study, in-hospital mortality was 6.8% (n=877). PHD and IHD composed 56.3% (n=1130) and 43.7% (n=877), of trauma related deaths, respectively.
The majority of both cohorts were male. IHD patients were older (37.4 years, SD 15.5 versus 33.4 years, SD 12.1, p<0.001). Both PHD and IHD patients were primarily injured on the road (n=650, 59.4%; n=564, 66.8%). PHD were primarily transported to the hospital via police (n=663, 60.1%) and private vehicles (n=282, 25.6%) in contrast to IHD who were transported via ambulance (n=401, 46.4%) and private vehicle (n=244, 28.1%), p<0.001. Of the PHD and IHD, 7.5% (n=83) and 48.2% (n=421) were transferred from an outside hospital, respectively p<0.001. Of the IHD, 92.5% (n=371) of the ambulance pre-hospital transport was for inter-hospital transfer. The majority of PHD and IHD were injured by assault (n=255, 24.7%; n=178, 21.8%) or MVC (n=188, 18.2%; n=173, 21.2%), p<0.001, Figure 1. The primary injury location for both PHD and IHD is head injury, 70.8% (n=773) and 67.4% (n=590), respectively, Table 1.
Figure 1:
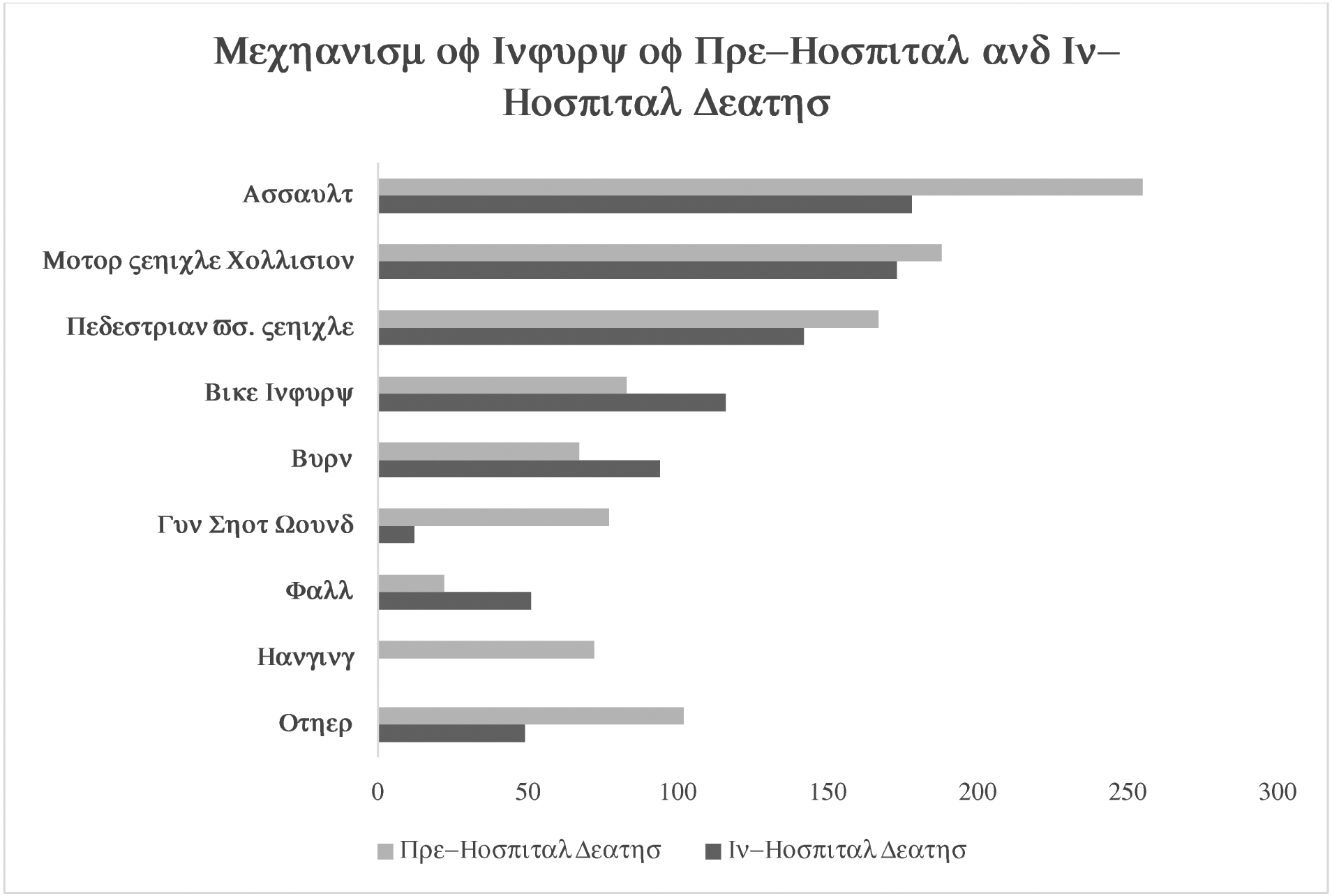
Mechanism of Injury for Pre-Hospital and In-Hospital Deaths
Table 1.
Bivariate analysis of characteristics of Pre-Hospital and In-Hospital Deaths
| Overall (n=2,007) | Pre-hospital Death (n=1,130, 56.3%) | In-hospital Death (n=877, 43.7%) | p-value | |
|---|---|---|---|---|
| Male Sex: n (%) | 1715 (85.6) | 985 (87.5) | 730 (83.2) | 0.007 |
| Age: mean (Sd) | 35.2 (13.8) | 33.5 (12.1) | 37.4 (15.5) | <0.001 |
| Injury Setting: n (%) | <0.001 | |||
| Road | 1214 (62.6) | 650 (59.4) | 564 (66.8) | |
| Home | 402 (20.7) | 229 (20.9) | 173 (20.5) | |
| Public Space | 131 (6.8) | 96 (8.8) | 35 (4.1) | |
| Work | 64 (3.3) | 28 (2.6) | 36 (4.3) | |
| Other | 128 (6.6) | 91 (8.3) | 37 (4.4) | |
| Transport: n (%) | <0.001 | |||
| Police | 793 (40.3) | 663 (60.1) | 130 (15.0) | |
| Private Vehicle | 526 (26.7) | 282 (25.6) | 244 (28.1) | |
| Ambulance‡ | 483 (24.5) | 82 (7.4) | 401 (46.4) | |
| Minibus | 97 (4.9) | 35 (3.2) | 62 (7.2) | |
| Other | 69 (3.5) | 41 (3.7) | 28 (3.2) | |
| Transferred: n (%) | 504 (25.5) | 83 (7.5) | 421 (48.2) | <0.001 |
| Injury Intent: n (%) | <0.001 | |||
| Unintentional | 1413 (71.6) | 737 (66.8) | 676 (77.7) | |
| Assault | 499 (25.3) | 310 (28.1) | 189 (21.7) | |
| Self-Inflicted | 62 (3.1) | 57 (5.2) | 5 (0.6) | |
| Injury Mechanism: n (%) | <0.001 | |||
| Assault | 433 (23.4) | 255 (24.7) | 178 (21.8) | |
| Motor Vehicle Collision | 361 (19.5) | 188 (18.2) | 173 (21.2) | |
| Pedestrian vs. Vehicle | 309 (16.7) | 167 (16.2) | 142 (17.4) | |
| Bike Injury | 199 (10.8) | 83 (8.0) | 116 (14.2) | |
| Burn | 161 (8.7) | 67 (6.5) | 94 (6.3) | |
| Gun Shot Wound | 89 (4.8) | 77 (7.5) | 12 (1.5) | |
| Fall | 73 (4.0) | 22 (2.1) | 51 (6.3) | |
| Hanging | 72 (3.9) | 72 (7.0) | 0 (0.0) | |
| Other | 151 (8.2) | 102 (9.9) | 49 (6.0) | |
| Primary Injury Location: n (%) | ||||
| Head/Spine | 1363 (69.3) | 773 (70.8) | 590 (67.4) | 0.1 |
| Chest | 102 (5.2) | 64 (5.9) | 38 (4.3) | 0.1 |
| Abdomen/Pelvis | 173 (8.8) | 89 (8.2) | 84 (9.6) | 0.3 |
| Extremities | 268 (13.6) | 107 (9.8) | 161 (18.4) | <0.001 |
| Other | 62 (3.2) | 59 (5.4) | 3 (0.3) | <0.001 |
| Injury Type: n (%) | <0.001 | |||
| Head Injury | 980 (49.4) | 545 (49.2) | 435 (49.7) | |
| Fracture | 227 (11.4) | 85 (7.7) | 142 (16.2) | |
| Laceration | 144 (7.3) | 80 (7.2) | 64 (7.3) | |
| Burn | 131 (6.6) | 39 (3.5) | 92 (10.5) | |
| Injury to Internal Organ | 82 (4.1) | 40 (3.6) | 42 (4.8) | |
| Gun Shot Wound | 80 (4.0) | 70 (6.3) | 10 (1.1) | |
| Contusion | 79 (4.0) | 56 (5.1) | 3 (2.6) | |
| Penetrating Wound | 75 (3.8) | 47 (4.2) | 28 (3.2) | |
| Other | 186 (9.4) | 146 (13.2) | 40 (4.6) | |
| Arrival Glasgow Coma Score: median (IQR) | 3 (3 – 15) | 3 (3 – 3) | 15 (7 – 15) | <0.001 |
|
Time from Injury to Arrival (days): median (IQR) |
0 (0 – 0) | 0 (0 – 0) | 0 (0 – 1) | <0.001 |
| Arrival Time of Day: n (%) | 1.0 | |||
| Day (6 AM – 6 PM) | 1028 (450 (51.7) | 450 (51.7) | 578 (51.8) | |
| Night (6 PM – 6 AM) | 960 (48.3) | 421 (48.3) | 539 (48.2 |
Majority of IHD were transferred from outside hospitals by ambulance
On multivariate Poisson regression, patients who were transported to KCH by the police (RR 2.61, 95% CI 1.89 – 3.59, p<0.001) when compared to transport via ambulance had an increased relative risk of PHD. Patients with a head or spine (RR 1.32, 95% CI 1.14 – 1.53, p<0.001), chest (RR 1.34, 95% CI 1.11 – 1.62, p=0.002), and abdomen or pelvis (RR 1.30, 95% CI 1.08 – 1.55, p=0.004) injury when compared to extremity injury had an increased relative risk of PHD. Finally, being injured by hanging (RR 1.43, 95% CI 1.31 – 1.56, p<0.001), motor vehicle collision (RR 1.33, 95% CI 1.18 – 1.50, p.<0.001), and gunshot wound (RR 1.31, 95% CI 1.17 – 1.47, p<0.001) had an increased relative risk of PHD when compared to assault, Table 2.
Table 2:
Poisson Regression Predicting Risk of Pre-Hospital Death
| Relative Risk | 95% Confidence Interval | p-value | |
|---|---|---|---|
| Age | 1.00 | 0.99 – 1.00 | 0.009 |
| Injury Location | |||
| Head/Spine | 1.32 | 1.14 – 1.53 | <0.001 |
| Chest | 1.34 | 1.11 – 1.62 | 0.002 |
| Abdomen/Pelvis | 1.30 | 1.08 – 1.55 | 0.004 |
| Extremity | Ref | - | - |
| Other | 1.78 | 1.48 – 2.13 | <0.001 |
| Transport | |||
| Minibus | 1.33 | 0.90 – 1.96 | 0.2 |
| Private Vehicle | 1.72 | 1.24 – 2.38 | 0.001 |
| Ambulance | Ref | - | - |
| Police | 2.61 | 1.89 – 3.59 | <0.001 |
| Other | 1.94 | 1.34 – 2.80 | <0.001 |
| Transferred | 0.48 | 0.35 – 0.65 | <0.001 |
| Injury Mechanism | |||
| Assault | Ref | - | - |
| Motor Vehicle Collision | 1.33 | 1.18 – 1.50 | <0.001 |
| Pedestrian vs. Vehicle | 1.13 | 1.00 – 1.27 | 0.05 |
| Bike Injury | 1.06 | 0.89 – 1.25 | 0.5 |
| Burn | 1.02 | 0.87 – 1.19 | 0.8 |
| Gunshot Wound | 1.31 | 1.17 – 1.47 | <0.001 |
| Fall | 0.94 | 0.70 – 1.25 | 0.7 |
| Hanging | 1.43 | 1.31 – 1.56 | <0.001 |
| Other | 1.17 | 1.02 – 1.34 | 0.03 |
Discussion
Violence and injuries are significant global public health concerns characterized by marked regional variation in incidence.10 In this comparative analysis of a trauma cohort in the pre-hospital versus in-hospital setting, we show head injury was the primary injury location and cause of mortality in all patients. Furthermore, upon assessing risk factors for PHD versus IHD, we show head injury, gunshot wounds, hangings, and being transferred to the hospital by the police, increase the relative risk of pre-hospital deaths.
This study is the first comparative analysis of pre-hospital deaths in Malawi following trauma. Pre-hospital deaths accounted for more deaths than in-hospital deaths in our cohort at 56.3%, which is consistent with other studies in the region. A study assessing fatal injuries by Gathecha et al. and Saidi et al. showed 51.4 and 57.5% of all trauma-related deaths in Nairobi occurred in the pre-hospital setting, respectively. However, reports from the Transkei region in South Africa found pre-hospital death following trauma in 74% of patients.11 In Ghana, 81% of all trauma deaths were in the pre-hospital setting.12 Interestingly, in the United States, Baker et al. in the 1980s showed 53% and 47% of trauma deaths occurred at the scene and in-hospital, respectively13,14 The attribution for the timing of death, particularly in the pre-hospital setting, maybe due to injury severity. However, other factors, such as the absence of functional pre-hospital care systems, play a significant role in death attribution.15,16 In Malawi, like similar countries in the region, pre-hospital care and EMS development remain underdeveloped, and access to professional pre-hospital care is almost nonexistent.17
Head injury is the predominant injury location and cause of death in both our PHD and IHD cohort at 70.8 and 67.4%, respectively. Several studies have investigated the causes of death in trauma patients. Baker et al. found that brain injury accounted for 50% of deaths.12 Shackford et al. also found that head injury was the most common cause of death. When combined with spinal cord injury, neurologic injuries were responsible for 49% of deaths.18 Similarly, in a study conducted in South Africa, specifically looking at PHD and IHD following trauma, head injury accounted for 50% of deaths.11
The in-hospital mortality of 6.8% following trauma in our cohort is comparable to most reported trauma mortality in sub-Saharan Africa. Reports from Kenya and South Africa show similar in-hospital mortality rates of 4.4 and 5.9%, respectively.19,20 Of note, in the United States, in-hospital trauma mortality is 4.39%.21 However, in a study from Nigeria by Ekeke et al., the reported the average yearly IHD rate was 16.6 %.22
The most prevalent mechanism of injury in both the PHD and IHD cohorts was assault, followed by motor vehicle injury. This is consistent with another study in western Kenya, which found assault was the leading cause of injury fatality.23 There is a high prevalence of fatal interpersonal violence in sub-Saharan Africa. The high rate of assault in Africa is due to several factors, including political instability leading to failure of governance, economic vulnerability, and post-colonial inter-ethnic and interracial injustices, including apartheid.24 The current homicide estimates in Africa is the second highest in the world at 10.9 per 100,000 after the Americas.25 Other African countries such as Rwanda and Ethiopia have reported that assault is the second leading cause of injury after motor vehicle injuries, unlike the pattern in Malawi.26,27
Results of a recent Africa-wide EMS survey show EMS serves less than 9% of Africans, and this may indeed be a gross underestimate.5 Attenuating pre-hospital deaths can only be achieved by the establishment of functional pre-hospital care systems and the training of emergency medical service providers. This may, in turn, also change in-hospital mortality following trauma. In a recent systematic review of barriers to the provision of out of hospital emergency care in developing countries, culture, infrastructure, communication/coordination, transport, equipment, and human resources were cited as the commonest barriers.28 Though many may cite the lack of ambulances as a major barrier, an ambulance without a trained EMS provider is just another mode of transport to a health care facility for definitive care without the ability for pre-hospital clinical intervention. More importantly, many countries in sub-Saharan Africa do not have the financial wherewithal within a meager health care budget to invest in pre-hospital care.
Some researchers have piloted innovative programs instead of the creation of a formalized EMS system. Upon noticing the majority of injured persons are transported to the hospital by some type of commercial vehicles, such as a taxi or bus, Mock et al. trained Ghanaian commercial drivers using a 6-hour first aid course.29 They showed a sustained improvement in the delivery of components of first aid. This is the type of innovation required, in addition to a commitment by the local ministry of health, to build a pre-hospital system benefitting trauma and non-trauma patients alike.
This study has several limitations. This is a single-center study in the capital city of Malawi, and this may limit generalizability. The PHD cohort may be an underestimate as we may not have captured all pre-hospital deaths that were transferred straight to the mortuary, leading to presentation bias. We believe this is minimal as all deceased patients presenting to our center require death declaration in the emergency room before transfer to the mortuary. Lastly, we did not account for the cause of death in some patient that had significant injuries in more than one body region.
Conclusions
In Malawi, there is a preponderance of pre-hospital trauma fatalities, mostly in men and primarily resulting from interpersonal violence and motor vehicle collisions. Head injury is the primary injury location resulting in death. The creation of both formal initiatives such as implementation of an ambulance transport system with EMS provider training and informal programs like training police officers, and commercial transport drivers are imperative to attenuate both PHD and IHD for trauma and non-trauma patients alike.
Acknowledgements
This study was funded by the NIH Fogarty International Center (Laura Purcell, Grant #D43TW009340). We wish to thank all of our collaborators and partners at Kamuzu Central Hospital.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.WHO, Global Health Challenges: https://www.who.int/whr/2003/chapter1/en/index3.html#box_1_3 accessed January 4th 2020
- 2.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health, 90 (4) (2000), pp. 523–526, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013 Inj Prev, 22 (1) (2016), pp. 3–18, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Injuries and violence: the facts 2014 WHO, Geneva: (2014) http://apps.who.int/iris/bitstream/10665/149798/1/9789241508018_eng.pdf [Google Scholar]
- 5.Mould-Millman NK., Dixon JM, Sefa N, Yancey A, Hollong BG, Hagahmed M, et al. The state of emergency medical services (EMS) systems in Africa Prehospital Disaster Med (2017), pp. 1–11, [DOI] [PubMed] [Google Scholar]
- 6.Mould-Millman NK, Rominski SD, Bogus J, Ginde AA, Zakariah AN, Boatemaah CA, et al. Barriers to accessing emergency medical services in Accra, Ghana: development of a survey instrument and initial application in Ghana. Global Health: Sci Practice, 3 (4) (2015), pp. 577–590, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mistovich JJ, Hafen BQ, Karren KJ. Pre-hospital emergency care. USA: 8th ed: Brady Prentice Hall Health; 2007 [Google Scholar]
- 8.Calvello EJ, Broccoli M, Risko N, Theodosis C, Totten VY, Radeos MS, et al. Emergency care and health systems: consensus-based recommendations and future research priorities. Acad Emerg Med. 2013;20:1278–1288. [DOI] [PubMed] [Google Scholar]
- 9.Mould-Millman NK, Dixon JM, Sefa N, Yancey A, Hollong BG, Hagahmed M, et al. The State of Emergency Medical Services (EMS) Systems in Africa. Prehospital and Disaster Medicine. 2017;32(03):273–283 [DOI] [PubMed] [Google Scholar]
- 10.Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev. 2016;22(1):3–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meel BL. Pre-hospital and hospital traumatic deaths in the former homeland of Transkei, South Africa.J Clin Forensic Med. 2004. February;11(1):6–11. [DOI] [PubMed] [Google Scholar]
- 12.Mock CN, Jurkovich GJ, nii-Amon-Kotei D, Arreola-Risa C, Maier RV. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998; 44: 804–814. [DOI] [PubMed] [Google Scholar]
- 13.Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD. Epidemiology of trauma deaths. Am J Surg. 1980;140(1):144–150. [DOI] [PubMed] [Google Scholar]
- 14.Trunkey DD. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, timely surgery, and further research. Sci Am. 1983;249(2):28–35. [PubMed] [Google Scholar]
- 15.Kuzma K, Lim HG, Kepha B, Nalitolela NE, Reynolds TA. The Tanzanian trauma patients’ pre-hospital experience: a qualitative interview-based study. BMJ Open. [DOI] [PMC free article] [PubMed]
- 16.Mock C, Quansah R, Kobusingye O, Goosen J. Trauma care in Africa: the way forward. Afr J Trauma. 2014;3:3–10. [Google Scholar]
- 17.Suryanto, Plummer V, Boyle M. EMS Systems in Lower-Middle Income Countries: A Literature Review. Prehosp Disaster Med. 2017. February;32(1):64–70. [DOI] [PubMed] [Google Scholar]
- 18.Shackford SR, Mackersie RC, Holbrook TL, Davis JW, Hollingsworth-Fridlund P, Hoyt DB, Wolf PL. The epidemiology of traumatic death. A population-based analysis. Arch Surg. 1993;128(5):571–575. [DOI] [PubMed] [Google Scholar]
- 19.Botchey IM Jr, Hung YW, Bachani AM, Saidi H, Paruk F, Hyder AA. Understanding patterns of injury in Kenya: Analysis of a trauma registry data from a National Referral Hospital. Surgery. 2017. December;162(6S):S54–S62. [DOI] [PubMed] [Google Scholar]
- 20.Spence RT, Scott JW, Haider A, Navsaria PH, Nicol AJ. Comparative assessment of in-hospital trauma mortality at a South African trauma center and matched patients treated in the United States.Surgery. 2017. September;162(3):620–627. [DOI] [PubMed] [Google Scholar]
- 21.NTDB Annual Report 2016© American College of Surgeons 2016. https://www.facs.org/-/media/files/quality-programs/trauma/ntdb/ntdb-annual-report-2016.ashx Accessed January 7th 2020.
- 22.Ekeke ON, Okonta KE.Trauma: a major cause of death among surgical inpatients of a Nigerian tertiary hospital. Pan Afr Med J. 2017. September 5;28:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odhiambo FO, Beynon CM, Ogwang S, Hamel MJ, Howland O, van Eijk AM, et al. Trauma-related mortality among adults in rural western Kenya: characterizing deaths using data from a health and demographic surveillance system. Plos one. 2013;8:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glaser Clive (2008) Violent Crime in South Africa: Historical Perspectives, South African Historical Journal, 60:3, 334–352, DOI: 10.1080/02582470802417433 [DOI] [Google Scholar]
- 25.World Health Organisation. Global status report on violence Prevention 2014. http://www.who.int/violence_injury_prevention/violence/status_report/2014/en/. Accessed January 10,2020
- 26.Kim WC, Byiringiro JC, Ntakiyiruta G, Kyamanywa P, Irakiza JJ, Mvukiyehe JP,et al. Vital statistics: estimating injury mortality in Kigali, Rwanda. World J Surg. 2016;40(1):6–13. [DOI] [PubMed] [Google Scholar]
- 27.Tsegaye F, Abdella K, Ahmed E, Tadesse T, Bartolomeos K. Pattern of fatal injuries in Addis Ababa, Ethiopia: a 1-year audit. East Cent Afr J Surg. 2010;2:10–7. [Google Scholar]
- 28.Kironji AG, Hodkinson P, de Ramirez SS, Anest T, Wallis L, Razzak J, Jenson A, Hansoti B. Identifying barriers for out of hospital emergency care in low and low-middle income countries: a systematic review. BMC Health Serv Res. 2018. April 19;18(1):291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mock CN, Tiska M, Adu-Ampofo M, Boakye G. Improvements in pre-hospital trauma care in an African country with no formal emergency medical services. J Trauma. 2002. July;53(1):90–7. [DOI] [PubMed] [Google Scholar]


