Abstract
Background: Infectious gastroenteritis is a risk factor for the development of post-infectious Irritable Bowel Syndrome (PI-IBS). Recent clinical studies reported a higher prevalence of the intestinal parasite Blastocystis in IBS patients. Using a rat model, we investigated the possible association between Blastocystis infection, colonic hypersensitivity (CHS), behavioral disturbances and gut microbiota changes. Methods: Rats were orally infected with Blastocystis subtype 4 (ST4) cysts, isolated from human stool samples. Colonic sensitivity was assessed by colorectal distension and animal behavior with an automatic behavior recognition system (PhenoTyper), the Elevated Plus Maze test and the Forced Swimming tests. Feces were collected at different time points after infection to study microbiota composition by 16 S rRNA amplicon sequencing and for short-chain fatty acid (SFCA) analysis. Results: Blastocystis-infected animals had non-inflammatory CHS with increased serine protease activity. Infection was also associated with anxiety- and depressive-like behaviors. Analysis of fecal microbiota composition showed an increase in bacterial richness associated with altered microbiota composition. These changes included an increase in the relative abundance of Oscillospira and a decrease in Clostridium, which seem to be associated with lower levels of SCFAs in the feces from infected rats. Conclusions: Our findings suggest that experimental infection of rats with Blastocystis mimics IBS symptoms with the establishment of CHS related to microbiota and metabolic shifts.
Subject terms: Microbiology, Gastroenterology
Introduction
Chronic visceral pain related to colonic hypersensitivity (CHS) is generally described as a poorly localized, diffuse and stabbing sensation that can be associated with many gastrointestinal disorders such as Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS)1. IBS generates a significant health care burden, is one of the most common disorders encountered in gastrointestinal practice and greatly affects the quality of life. The Rome IV criteria define IBS as a functional chronic disorder characterized by abdominal pain, changes in bowel habits and no macroscopic organic lesions2. Patients are classified into four subgroups: IBS-C for patients with predominant constipation, IBS-D when diarrhea is predominant, IBS-M for patients with alternating constipation and diarrhea and IBS-U when no clear classification can be established3. The pathophysiology of IBS is complex and poorly understood, and its etiology is suspected to be multifactorial. IBS patients exhibit several biological perturbations such as disturbances in gut epithelial barrier integrity leading to increased intestinal permeability, immune activation and modifications of intestinal microbiota composition and function2,4. Psychological co-morbidities also occur in more than half of cases, such as anxiety, depression and hypochondria5.
Infectious gastroenteritis is a key risk factor for the development of IBS, referred to as post-infectious IBS (PI-IBS)6. PI-IBS often has characteristics of IBS-D, and can occur in 4% to 31% of patients following infectious acute gastroenteritis6. Several studies have supported a role in PI-IBS for pathogen-mediated modifications in the resident intestinal microbiota, epithelial barrier integrity and immune activation7–9. The role of certain pathogenic bacteria such as Shigella spp., Escherichia coli, Salmonella and Campylobacter jejuni or protozoa such as Giardia intestinalis is now well established10. Interestingly, a recent meta-analysis showed that the risk of IBS was higher after a protozoa-related or parasitic enteritis than with a bacterial infection11.
Blastocystis spp. are the most frequent enteric protozoa found in the intestinal tract of humans and various animals12. These parasites have been classified into 17 subtypes (ST) according to the small subunit ribosomal RNA-encoding gene. Subtypes ST1 to ST9 and ST12 have been recovered in human stool samples with ST3 being the most frequent followed by ST1, ST2 and ST413–15. Interestingly, ST4 was reported to be the most frequent ST in some studies performed in Europe16–19. Blastocystis spp. prevalence in humans ranges from 0.5% to 100% according to country and hygiene conditions and sanitary practices13,20. However, the involvement of Blastocystis spp. in human diseases is highly debated. Interest of the scientific and medical communities in Blastocystis spp. infection has increased in the last few years since epidemiological studies reported a higher prevalence of the parasite in IBS patients21–24. Changes in the microbiota of Blastocystis-infected subjects are often reported but results can also be heterogeneous19,22,25,26. Some clinical studies reported an increase in microbiota diversity, suggesting a potential benefit for Blastocystis-associated microbiota19,25,26. In contrast, one other study described a decrease in protective bacteria22. A more recent study reported a decrease in short-chain fatty acid (SCFA) levels in fecal samples from Blastocystis-infected patients26 SCFAs, including acetate, propionate and butyrate, enhance epithelial barrier function and immune tolerance, promoting gut homeostasis27.
In the present study we aimed to characterize whether chronic Blastocystis infection can lead to IBS-like symptoms. We first characterized non-inflammatory CHS associated with anxiety- and depressive-like behaviors in infected rats. We then demonstrated that Blastocystis infection was associated with microbiota and metabolic shifts that can induce intestinal epithelial barrier dysfunction.
Results
Blastocystis infection induces non-inflammatory colonic hypersensitivity with an increase in serine protease activity
Four-week-old Wistar rats were infected with 105 ST4 cysts purified from a healthy human carrier (Supplementary Fig. 1). Infection monitoring by xenic culture of the feces showed the presence of parasites from day 1 until euthanasia on day 31 post-infection, as described previously28.
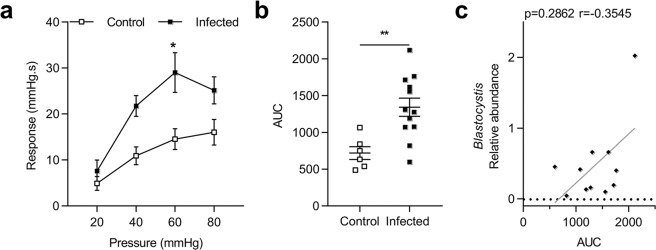
Colorectal distension (CRD) showed that colonic sensitivity was significantly increased at 60 mmHg (p = 0.01) in Blastocystis infected rats at D31 (Fig. 1a). AUC from 20 to 80 mmHg were almost 2-times higher in infected rats than in control rats (Fig. 1b).Interestingly, colonic hypersensitivity was not correlated with a relative abundance of Blastocystis obtained by 16 S sequencing (Fig. 1c).
Figure 1.
Evaluation of colonic hypersensitivity after infection with Blastocystis ST4. (a) Representative colonic response to colorectal distension (CRD) in infected (n = 12) and control (n = 6) rats at D31. (b) Area under the curve (AUC) of colonic response calculated by the trapeze method between 20 mmHg and 80 mmHg. (c) Correlation between relative abundance of Blastocystis and AUC of colonic response. Statistical analysis: a, Two-way ANOVA test followed by a Sidak post-hoc test; b, t-test; c, Spearman-test; *p < 0.05 **p < 0.01; three independent experiments were performed.
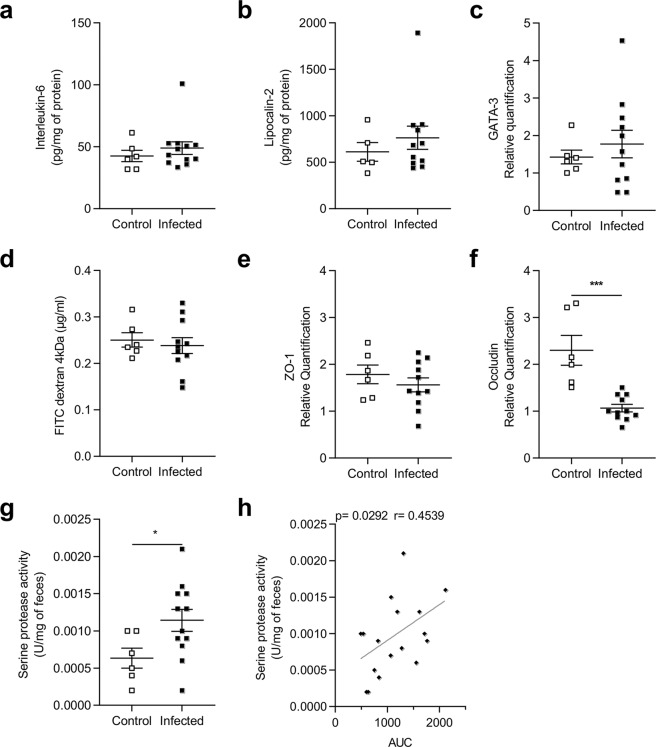
We then assessed anatomical parameters and inflammatory mediator production at D31 post-infection. Surprisingly, chronic infection had no effect on body weight (Supplementary Fig. 2a), colon weight (Supplementary Fig. 2b) or length (Supplementary Fig. 2c), and was not associated with any histological changes such as cell infiltration, edema or crypt disruption (Supplementary Fig. 2d). Colonic levels of IL-6 and lipocalin-2 proteins were unchanged in infected animals (Fig. 2a,b). In addition, GATA-3 (transcription factor promoting T-helper 2 differentiation) mRNA expression was not higher in infected rats (Fig. 2c).
Figure 2.
Quantification of inflammatory mediators after infection with Blastocystis.(a,b) Quantification of Interleukin-6 (IL-6) (a) and Lipocalin-2 (b) in colonic tissues of control (n = 5) and infected rats (n = 11) at D31. Values were expressed as pg/mg protein. (c) Colonic expression of GATA-3 in control (n = 6) and infected rats (n = 11) at D31. (d) FITC-Dextran 4 kDa concentration in serum of control (n = 6) and infected (n = 11) rats at D21. Colonic expression of ZO-1 (e) and occludin (f) in control (n = 6) and infected rats (n = 11) at D31. (g) Serine protease activity (U/mg feces) in supernatants from feces of control (n = 6) and infected rats (n = 12) at D31. (h) Correlation between serine protease activity and AUC of colonic response. Statistical analysis: Values were expressed as relative expression compared to GAPDH expression. Statistical analysis: a and b, Mann-Whitney test: c, d, e, f, g and h t-test; Spearman-test; *p < 0.05 **p < 0.01; ***p < 0.001; three independent experiments were performed.
The potential impact of infection on intestinal barrier integrity was then explored by a functional test using FITC-Dextran 4 kDa on D21 and mRNA quantification of two tight junction components on D31. Intestinal permeability in vivo and mRNA levels of ZO-1 were unchanged in the infected animals (Fig. 2d,e) we observed a strong decrease in occludin expression (Fig. 2f). Because intestinal permeability was performed at D21 and a decrease in occludin expression observed at D31, we assessed epithelial barrier function ex vivo with Ussing chambers. As previously observed, intestinal permeability was not altered in infected rats (Supplementary Fig. 3).
Serine protease activity, which is suspected to participate in CHS, was measured in fecal samples at D31. A significant increase in serine protease activity was observed in the supernatant of infected rat feces (Fig. 2g). Interestingly, colonic hypersensitivity was significantly correlated with the increase in serine protease activity (p = 0.03) (Fig. 2h).
Blastocystis infection induces behavioral changes
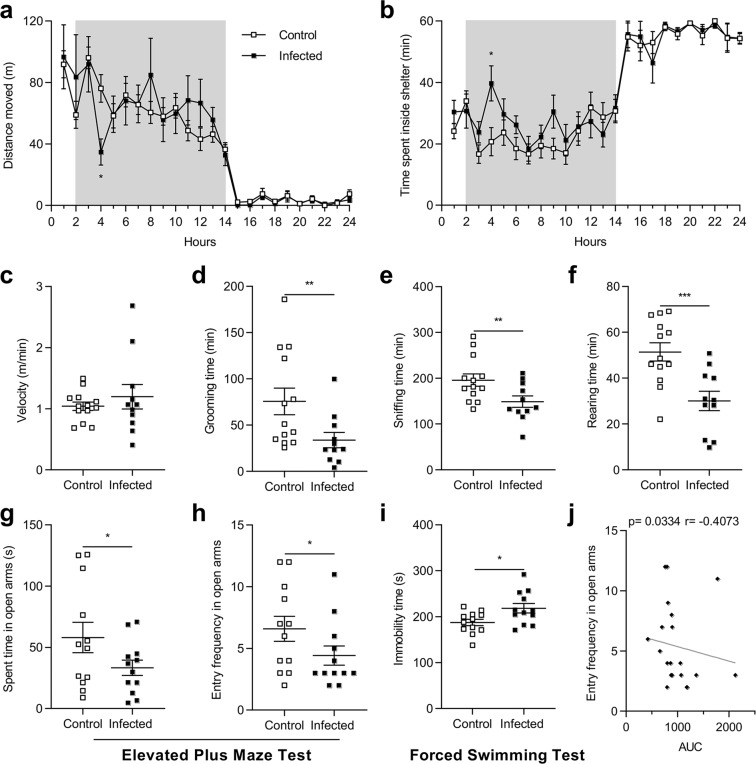
We analyzed the impact of Blastocystis infection on animal behavior at D27 with PhenoTyper. Infected rats did not present any differences in distances traveled (Fig. 3a), time spent in the hidden zone (Fig. 3b), velocity (Fig. 3c), and in drinking and eating behaviors (Supplementary Fig. 4a,b). However, the total duration of grooming (p = 0.004), rearing (p = 0.0006) and sniffing (p = 0.01) was significantly shorter during the dark period (Fig. 3d,e,f) suggestive of anxiety- and depression-like behavior. These behavioral alterations were confirmed at D29 with a series of more classical tests including the Elevated Plus Maze (EPM) test and the Forced Swimming Test (FST). The EPM test showed that infected rats entered the open arms less frequently and spent much less time there (Fig. 3g,h). In addition, immobility time during the FST was longer in infected rats (Fig. 3i), indicative of depressive-like behavior. Interestingly, the AUC value of intracolonic pressure in response to CRD was negatively correlated with the frequency of entry in the open arms (Fig. 3j).
Figure 3.
Behavior assessments of rats after infection with Blastocystis in a representative experiment. Control and infected rats were placed in PhenoTyper home cages at D27 for 24 h video recording. The total distance moved (a) and time spent inside the shelter (b) were determined during a 12 h:12 h light-dark cycle. Mean velocity (c), grooming (d), rearing (e) and sniffing (f) times were only measured during the 12-hour dark period. Time spent (g) and entry frequency (h) of control and infected rats into the open arms of the Elevated Plus Maze (EPM) at D29. (i) Immobility time during the Forced Swimming Test of control and infected rats at D29. (j) Correlation between the areas under the curve (AUC) of colonic sensitivity and the frequency of entries into the open arms of the EPM. Each plot represents one rat. Statistical analyses: a and b, Two-way ANOVA test followed by a Sidak post-hoc test; c, e, f, g and i, t-test; d and h, Mann-Whitney; j, Spearman-test; *p < 0.05, **p < 0.01, ***p < 0.001; two independent experiments with 12 rats per group were performed.
Blastocystis infection is associated with fecal microbiota modifications in rats
To evaluate the influence of Blastocystis infection on intestinal microbiota, the fecal microbiota composition of both infected and control rats was characterized by Illumina sequencing (SRA accession PRJNA607663). At D0 (i.e. before infection), no difference in fecal microbiota composition was observed between groups (Supplementary Fig. 5). At D31, bacterial richness was significantly greater in chronically-infected rats (p = 0.02) (Fig. 4a,b). In addition, the PCoA of beta-diversity clearly demonstrated significant differences (Adonis, p = 0.001) in the evolution of microbial composition between infected and control rats (Fig. 4c). This was accompanied by an increase in the relative abundance of Proteobacteria and Tenericutes in infected animals (Fig. 4d). The decrease in the Firmicutes/Bacteroidetes ratio (Fig. 4e, p = 0.0623) was correlated with colonic hypersensitivity (p = 0.04) (Fig. 4f). At the genus level, we observed a decrease in the relative abundance of Clostridium, Pseudomonas and Rhodoplanes in infected rats, whereas the relative abundance of Anaerovorax, Oscillospira and Parabacteroides was greater (Fig. 4f). Interestingly, colonic hypersensitivity was significantly correlated with the decrease in the relative abundance of Oscillospira (p = 0.0129) (Fig. 4g) and the increase in that of Clostridium (p = 0.0151) (Fig. 4h).
Figure 4.
Fecal microbiota variations associated with Blastocystis infection in rats in a representative experiment. (a) Alpha diversity was determined by observed Operational Taxonomic Unit (OTU) measurement according to sequences per sample in feces of control (n = 6) and infected (n = 12) rats at D31. (b) Area under the curve (AUC) of the observed OTUs for control and infected rats. (c) Principal coordinates analysis (PCoA) of the unweighted UniFrac distance of control (red plots) and infected (blue plots) rats at D31. Significance (p = 0.001) and the strength of explained variation (R² = 0.0962) were assessed with Adonis. (d) LEfSE (LDA Effect Size) was used to investigate bacterial taxa that drive differences between control and infected rats. Red, taxa higher in controls; Green, taxa higher in infected rats. (e) Ratio Firmicutes/Bacteroides in control (n = 6) and infected (n = 12) rats at D31. (f) Correlation between AUC of colonic sensitivity and Firmicutes/Bacteroides ratio. (g-h) Correlation between AUC of colonic sensitivity and relative abundance of Oscillospira (g) and Clostridium (h). Statistical analyses: a Two-way ANOVA test followed by a Sidak post-hoc test; b, t-test; e, Mann-Whitney; f, g and h, Spearman-test; *p < 0.05.
Shifts in microbiota community composition were associated with metabolite changes in infected rats. We quantified the ratio of SCFAs between the end and beginning of the experiment (D31/D0). We observed a decrease in the D31/D0 ratio for both acetate and propionate (Fig. 5a,b). The decrease in the butyrate ratio was not significant, however, (p = 0.06) (Fig. 5c) in the feces of infected rats.
Figure 5.
Impact of microbiota modifications on fecal Short-Chain Fatty Acid (SCFA) levels in a representative experiment. D31/D0 ratio of acetate (a), propionate (b) and butyrate (c) in feces from control and infected rats. The SCFAs were quantified by gas liquid chromatography in feces of control (n = 6) and infected rats (n = 12) at D31. Statistical analysis: a-c, t-test *p < 0.05.
Discussion
The role of Blastocystis spp. as a human pathogen remains unclear since, although some studies have associated it with acute or chronic digestive disorders29,30, it can be found in both symptomatic and asymptomatic patients. In symptomatic patients, blastocystosis is associated with non-specific symptoms, such as chronic diarrhea, abdominal pain and bloating, sometimes mimicking IBS symptoms31,32. Interestingly, an increasing number of studies have suggested an association between Blastocystis spp. and IBS21–23. In numerous studies, Blastocystis spp. was more frequently detected in IBS patients than in control groups21–24. Experimental and genomic data support this association and suggest interactions between the intestinal microbiota and Blastocystis spp., which could be involved in the gut dysbiosis associated with IBS33. Our results also suggest that Blastocystis spp. chronic infection may lead to IBS-like symptoms. We characterized non-inflammatory CHS associated with anxiety- and depressive-like behaviors in infected rats. We then demonstrated that Blastocystis infection was associated with both microbiota and metabolic shifts that can lead to CHS.
The origins of CHS associated with IBS remain elusive. However, CHS occurs in up to 80–90% of IBS patients34. Thus, the epidemiological link between Blastocystis spp. and IBS needs to be clarified. Using a recent model of chronic infection with Blastocystis ST4 in rats, our study establishes for the first time the relationship between Blastocystis spp. infection and CHS. As previously described by Leder et al., we didn’t correlate the relative abundance with the CHS in infected rats35.
During acute gastroenteritis the immune system is highly activated, leading to inflammatory response. After gastroenteritis resolves, inflammation should subside but some studies have described infiltration of immune cells and high cytokine levels in PI-IBS patients, which suggests that the establishment of low grade inflammation following gastroenteritis could be a causal factor of CHS10. Some in vitro studies have also shown immunomodulatory effects of Blastocystis spp. on mammalian cell cultures. The production of pro-inflammatory cytokines, including IL-8, granulocyte-macrophage colony-stimulating factor (GM-CSF), IL-1β, IL-6, and Tumor Necrosis Factor-α (TNF-α) in response to acute Blastocystis exposure have been described in vitro in epithelial cell lines and murine macrophages36,37. In our experimental conditions, we did not observe any clearance of the parasite until 31 days after infection, as observed in PI-IBS, suggesting that the Blastocystis infection model is an infectious model of IBS. However, we observed no inflammation or tissue perturbations on D31 (histological analysis, IL-6 and lipocalin-2 levels and GATA-3 mRNA). The disease activity index (DAI) including body weight loss, stool consistency and blood in stool was monitored every week until 31 days post-infection and any modifications were characterized especially in stool consistency. On D21, IL-6 and TNF-α levels in the serum were too low to be quantified in either group.
In absence of inflammation, altered epithelial barrier function is probably one of the most important mechanisms involved in IBS2. An increase in intestinal permeability would allow the diffusion of luminal antigens and/or proteases to the submucosal compartments38. This intestinal permeability is related to an altered expression of tight junction (TJ) proteins, including a decrease in the expression of occludin and ZO-138. Biopsy analysis from Blastocystis-infected patients showed disturbances of barrier function integrity and permeability39. These modifications are probably the result of multiple factors, but congruent data have been reported in some in vitro experiments showing the ability of Blastocystis factors to interfere with ZO-1 and occludin, leading to TJ dysfunctions40. In our model, infected animals had lower occludin mRNA expression in the colon and intestinal permeability was not altered. However, study reports that the barrier function of the intestinal epithelium was normal in occludin knockout mice41. In our study, the absence of inflammation and barrier impairment could have been due to the use of Blastocystis ST4, which is considered to be of murine origin and probably the best suited to rats. Moreover, the isolate used in our study was purified from stools of an asymptomatic human carrier. Interestingly, Hussein et al. reported that the degrees of severity of pathological changes and intestinal permeability in rats were correlated with the intensity of symptoms in patients from whom isolates were collected and with STs of Blastocystis, suggesting the existence of other, more virulent strains/subtypes42.
Hydrolases and proteases have been identified as candidate virulence factors of Blastocystis spp. and the panel which are secreted could explain the difference in terms of virulence33,43,44. Interestingly, several studies showed an increase in serine protease activity in IBS patients45–47. Likewise, higher serine protease activity was observed in a PI-IBS mouse model48. Taken together, the data above suggest an important role for serine proteases in IBS. Diffusion to the submucosa of serine proteases, which was increased in our infected rats, could be responsible for activation of the neuronal protease activated receptor (PAR) and nociceptive signal45. However, the origin of the serine proteases was unclear. Although Blastocystis can produce serine proteases, serine protease activity originates mainly in the host49 and the contribution of the gut microbiota to their production is not inconsiderable43,50. Further experiments are required to identify this origin and assess how the increase in intra-luminal serine proteases could have contributed to CHS in our model.
Psychological disturbances, especially anxiety and depression, are the most frequent comorbidities associated with visceral pain51. In our study, global behavior was analyzed with the PhenoTyper, a video tracking system which allows continuous and long-term monitoring of animals’ home cage behavior. Some behaviors in rats have been reported to be associated with specific psychological or physiological changes. A decrease in grooming is positively associated with depressive-like behavior, and a decrease in sniffing, related to curiosity or exploration, is positively associated with anxiety-like behavior52,53. Rearing, which is also considered as a behavior related to exploration, can be an effective indicator of pain54. These three behavior profiles were modified in our study and confirmed by EPM and FST reference tests. Our results show that Blastocystis-infected rats presented both anxiety- and depressive-like behaviors, probably related to visceral pain. Indeed, we observed a correlation between an increase in time spent in the open arms (EPM test) and CHS severity, which reinforces the role of visceral pain in the behavioral changes seen in our models.
Finally, because gut microbiota is a key player in the pathophysiology of IBS4, we characterized the microbiota modifications in Blastocystis-infected rats. In the absence of low grade inflammation, colonic hypersensitivity can be explained by alterations in intestinal microbiota composition that result in metabolite changes. Some recent studies described either a healthy Blastocystis-associated microbiota characterized by increased bacterial richness and certain beneficial bacteria such as Akkermansia, or dysbiosis accompanied by a decrease in SCFA-producing bacteria19,22,25,26. A recent study showed that Blastocystis ST7 isolate causes changes in the microbiota composition of infected mice, with a decrease in beneficial bacteria55, which is consistent with previous results of ours22. The association between Blastocystis and microbiota composition still needs to be clarified, as does the causal link between microbial community changes and Blastocystis. Our results showed that Blastocystis ST4 infection in rats is associated with bacterial community shifts, confirming for the first time the effect of this parasite on microbiota composition. The changes were characterized by an increase in bacterial richness and a decrease in the Firmicutes/Bacteroidetes ratio, which was correlated with CHS. The increase in bacterial richness in human intestinal microbiota associated with Blastocystis infection has been reported in different clinical studies, and is usually associated with a healthy microbiota26. The Firmicutes/Bacteroidetes ratio is a rough indicator of bacterial population shifts, and both a higher and lower ratio of Firmicutes/Bacteroidetes have been described in IBS patients4. Deeper analysis showed that the relative abundances of bacterial genera were modified in infected animals including an increase in the relative abundance of Oscillospira and a decrease in that of Clostridium, both being correlated with CHS. Our results are, therefore, in agreement with previous reports describing a decrease in Clostridium genus in IBS patients, and the association of that genus with visceral pain56,57. The Clostridiaceae family, including the Clostridium genus, also belongs to SCFA-producing bacteria58. SCFAs, including acetate, propionate and butyrate, play an important role in the maintenance of a healthy epithelial barrier, and a decrease in their number has been reported in IBS patients27,59. In our study, the feces composition of infected rats was characterized by a decrease in the overall content of SFCAs. Interestingly, a recent study observed a reduction in acetate, propionate and butyrate production in Blastocystis-colonized humans, in combination with an over-representation of Oscillospira26. A recent meta-analysis showed that the fecal level of propionate and butyrate was significantly lower in IBS-C60, which is consistent with the absence of epithelial barrier alterations in our study. However, SCFAs might influence neuropsychiatric disorders and psychological functioning as depression61. Thus, the decrease of these metabolites may participate to the behavioral disturbance observed in our model.
To conclude, we demonstrate for the first time that establishment of Blastocystis within gut microbiota is responsible for bacterial community perturbations associated with metabolic shifts leading to CHS. Interestingly, some of the modifications observed in the infected rats have also been reported in humans25,26. The mechanisms of Blastocystis-induced CHS are not fully understood but the perturbations observed were sufficient to affect animal behavior. Our results showed that blastocystosis symptoms in rats mimic human IBS, which raises the question of eradication of this protist in Blastocystis-positive IBS patients. The Blastocystis rat model seems to be a good model to decipher non-inflammatory CHS.
Materials and Methods
Animals
Three-week-old specific pathogen-free (Charles River Lab, Saint Germain Nuelles, France) Wistar male rats were housed two or three per cage in animal biosafety level 2 (21–22 °C, 12 h:12 h light-dark cycle) with access to food and water ad libitum. All experiments were performed according to the ethical guidelines set out in the Guide for the Care and Use of Laboratory Animals and with approval of the “Comité d’Ethique pour l’Expérimentation Animale Auvergne” (C2E2A), the local ethics committee (Reference number: EU0116–3003), and followed the guidelines of the Committee for Research and Ethical issues of the International Association for the Study of Pain62.
Experimental infections
An asymptomatic human carrier of Blastocystis ST4 was enrolled after a statement attesting to informed consent for study participation by the medical laboratory of Parasitology of the Clermont-Ferrand teaching hospital. All experiments were performed in accordance with the relevant guidelines and regulations, and approved by the research ethics committees, “Comité de Protection des Personnes Sud-Est 6”, France, agreement ref: 2014/CE29). Three days prior experiments, rats were pre-screened to ensure that they were healthy and free of Blastocystis or any other intestinal parasites. Four-week-old Wistar male rats were then orally inoculated with sterile PBS as control (n = 12) or with 105 Blastocystis ST4 cysts purified from human stools (n = 12) as previously reported28. The success of infection was confirmed by fecal cultures in Jone’s medium at 37 °C, as previously described28. Body weight of animals was monitored and feces were sampled every week until euthanasia and stored at −80 °C. Rats were euthanized at the end of the experiment (D31), and colon tissues were collected and split to be stored at −80 °C for molecular assays or in 4% paraformaldehyde for histological analyses.
Colorectal distension (CRD) test
This test assesses visceral sensitivity by measuring the response of the colon when submitted to distension. The CRD protocol was adapted for rats from Larauche et al.63. At D31, after 30 min in a restrainer, rats were anesthetized (3% Isoflurane) to introduce the CRD devices into the colon-rectum before being connected to an amplifier (Millar Instruments, Houston, TX, USA). The CRD protocol consisted of a set of distensions at constant pressures from 20 to 80 mm Hg, performed in duplicate as follows: 20 mm Hg steps of 20 sec duration with 4.5 min inter-stimuli intervals. P-spectrum was extracted from raw data with “smoothsec” at a time constant of 1.5 sec, followed by “absolute valor” and finally another “smoothsec” at a time constant of 1.5 sec to exclude the slower and tonic changes. Colonic response to CRD (mmHg.s) was quantified by measuring the area under the curve (AUC) during 20 sec of distension using the Integral relative to Minimum in Labchart.
Behavior recognition system PhenoTyper
The PhenoTyper (Noldus Information Technology, Wageningen, The Netherlands) is an automated infrared (IR) video-tracking system developed to measure the behavior of laboratory animals. The device is composed of eight Plexiglas cages (45 cm × 45 cm), each containing an opaque plastic square shelter accessible by two entrances and delimited areas for feeding and drinking. The cages are surrounded by a top unit provided with an infrared (IR) sensitive camera for video recording and IR led units. Briefly, at D27 rats were transferred into PhenoTyper cages (1 per cage) and animal activities were recorded with Mediarecorder (Noldus Information Technology, Wageningen, The Netherlands) for 24 h, including a light-dark cycle (12 h:12 h). Rats had ad libitum access to food, water and shelter. Raw data were analyzed with Ethovision XT software (Version 12, Noldus Information Technology, Wageningen, The Netherlands) and various specific behaviors were compared between infected and control rats.
Elevated-Plus-Maze (EPM) test
At D29, EPM was performed as previously described64. Animals were recorded for 5 min by Mediarecorder software. Analysis was performed by Ethovision XT software (version 12).
Forced Swimming Test (FST)
At D29, each rat was placed in a glass cylinder (30 cm diameter x 50 cm height) containing water at 22 ± 1 °C. The immobility time of rats was recorded for 6 min. Each rat was judged to be immobile when it stopped swimming and floated, making only those movements necessary to keep its head above water65.
In vivo intestinal permeability assay
At D21 intestinal permeability was determined by FITC-dextran in fasted animals as previously described66. Briefly, rats were administered 60 mg/100 g body weight of FITC-dextran (4 kDa, Sigma-Aldrich, FD-4) by gavage and samples were obtained from the retro-orbital venous plexus 5 h after administration. Serum FITC levels were determined by fluorometry at 488 nm using a microplate reader (Tecan, Lyon, France). Concentrations were calculated from a standard curve.
Assessment of epithelial barrier function
Two segments of distal colon of each animal were mounted in modified Ussing chambers (Biomecatronics, Ruitz, France) after removal of the seromuscular layer, leaving an exposed area of 0.0314 cm2. The luminal and basolateral compartments were filled with Krebs‐Ringer bicarbonate buffer (NaCl 120 mM, KCl: 5.9 mM, MgCl2: 1.2 mM, NaH2PO4: 1.2 mM, CaCl2: 2.5 mM, NaHCO3: 14 mM) supplemented with 10 mmol/L glucose. Solutions were kept at 37 °C and gassed with carbogen. Transmucosal potential difference was continuously monitored using calomel electrodes filled with saturated KCl and connected to the chambers with 3 M KCl-agar salt-bridges. The transepithelial electrical resistance (TEER) was calculated according to Ohm’s law from the voltage deflections induced by bipolar current pulses of 10 µA with a duration of about 2 sec. The TEER values were registered for each tissue just after mounting, at 40 minutes after mounting and then at 30‐minute intervals up to 160 minutes. The average TEER between 100 and 160 minutes was calculated over the two pieces of tissue per animal. These time points were selected because a stable TEER plateau was reached in most of the tissues at these times.
Tissue preparation for histological analysis
Flushed colons were opened longitudinally, cut into 4 cm and rolled. The samples were fixed in 4% paraformaldehyde (24 h, 4 °C), incubated in 30% sucrose (48 h, 4 °C) and embedded in OCT medium (ThermoFisher Scientific, Waltham, MA, USA; Cat. No. 23-730-571). Ten micrometer cross-sections were mounted on SuperFrost Plus slides (ThermoFisher Scientific, Waltham, MA, USA; Cat. No. 10149870), stained with hematoxylin phloxin safran and examined blindly by an anatomopathologist according to the following criteria: cellular infiltration and mucosal alteration (vasculitis, muscular thickening, and crypt abscesses) were graded from 0 to 3 (absent, mild, moderate and severe). Submucosal edema was scored from 0 to 2 (absent, moderate, and severe).
Enzyme-linked immunosorbent assay (ELISA)
Total proteins of rat proximal colon were extracted with lysis buffer (50 mM HEPES, 150 mM NaCl, 10 mM EDTA, 10 mM tetrasodium pyrophosphate, 2 mM vanadate, 100 mM NaF, 0.5 mM PMSF, 100 UI/mL iniprol/aprotinin, 20 µM leupeptin, 1% triton), and protein concentrations were determined with a BC Assay Protein quantification kit (Interchim, Montluçon, France; Cat. No. UP40840A). Colonic interleukin-6 (IL-6) and lipocalin-2 were quantified with the enzyme linked immunosorbent assay kit (R&D Systems, Minneapolis, MN, USA; Cat. No. Rat IL-6 DuoSet, DY506 and Rat Lipocalin-2/NGAL DuoSet DY3508) according to the manufacturer’s instructions. Concentrations were calculated from standard curve and normalized to the total protein concentration.
Reverse transcription and quantitative polymerase chain reaction (RT-qPCR)
Total RNAs of proximal colon were extracted with Trizol (ThermoFisher Scientific, Waltham, MS, USA; Cat. No. 15596026). DNAse-treated RNAs were reverse transcribed with high capacity cDNA RT kit (ThermoFisher Scientific, Waltham, MS, USA; Cat. No. 4368814) for reverse transcription-quantitative PCR (RT-qPCR). Specific cDNA were amplified for occludin (occF 5′-AGTACATGGCTGCTGCTGATG-3′; occR 5′-CCCACCATCCTCTTGATGTGT-3′), zonula occludens-1 (ZO-1) (ZO-1F 5′-AGCGAAGCCACCTGAAGATA-3′; ZO-1R 5′-GATGGCCAGCAGGAATATGT-3′), GATA-3 (GATA-3F 5′-AAGAGTGCCTCAAGTATCAG-3′; GATA-3R 5′- GCGGATAGGTGGTAATGG-3′) and GAPDH (GAPDHF 5′-AGACAGCCGCATCTTCTTGT-3′; GAPDHR 5′-TGATGGCAACAATGTCCACT-3′). qPCR assays were performed with SsoAdvanced Universal SYBR Green Supermix (Biorad, Hercules, CA, USA; Cat. No. 1725271) and carried out on CFX96 Touch Real-Time PCR Detection System (Biorad, Hercules, CA, USA). Relative quantifications of occludin, ZO-1 and GATA-3 genes were expressed as fold-change, using the 2−∆∆Ct method with GAPDH as reference gene.
Fecal microbiota analysis
DNA was extracted from rat feces collected at D0 and D31 with the NucleoSpin Soil kit protocol (Macherey-Nagel SARL, Hoerdt, France; Cat. No. 740780.250). Illumina high throughput sequencing was performed by MRDNA lab (Shallowater, TX, USA) on a MiSeq following the manufacturer’s guidelines. Briefly, the V4 region of the bacterial 16 S rRNA gene was amplified by 515 F (5′-GTGCCAGCMGCCGCGGTAA-3′) and 806 R (5′-GGACTACHVGGGTWTCTAAT-3′) primers and HotStarTaq Plus Master Mix Kit (Qiagen, Germantown, MD, USA; Cat. No. 203646) under the following conditions: denaturation 94 °C/3 min, followed by 28 cycles of 94 °C/30 sec, 53 °C/40 sec, and 72 °C/1 min, with a final elongation step 72 °C/5 min. Pooled PCR products were purified with calibrated Ampure XP beads. Illumina sequencing was performed and DNA libraries built by according to the Illumina TruSeq DNA library preparation protocol.
We performed microbiota analysis on Quantitative Insights Into Microbial Ecology (QIIME, version 1.8.0) software package67. In summary, sequences were demultiplexed to remove barcodes and primer sequences. Chimeric sequences were removed with USEARCH6168. Sequences were clustered with USEARCH61 at a 97% homology threshold69. Taxonomic analysis was performed with the Greengenes reference database (version 13-8).
Alpha diversity measures the richness of single microbial taxa within a sample. Observed operational taxonomic unit (OTU) measurements were determined with QIIME using an OTU table rarefied at various depths. AUC were calculated for each rarefaction curve. Beta diversity measures the variation in microbiota composition between individual samples. Unweighted UniFrac distances between samples were computed to measure beta diversity with the rarefied OTUs count table. Principal coordinates analysis (PCoA) was used to further assess and visualize beta diversity. Groups were compared for distinct clustering with Adonis. LEfSe (LDA Effect Size) was used to investigate bacterial members that drive differences between groups70.
Short chain fatty acid (SCFA) analysis
Acetate, propionate and butyrate were quantified from rat feces collected at D0 and D31. Briefly, about 200 mg of fecal samples were diluted in 200 µl of distilled water. After centrifugation, proteins were precipitated overnight with phosphotungstic acid (Sigma-Aldrich, Saint-Louis, MO, USA, Cat. No. P4006) and centrifuged to obtain a clear supernatant.
One microliter of the clear supernatant was used to analyze SCFA composition by gas liquid chromatography (Agilent technologies 6850 Network GC system, Santa Clara, SA, USA) with a splitless injector, a flame-ionization detector and a capillary column (30 m; 0.25 mm; 0.25 µm) impregnated with nitroterephthalic acid modified polyethylene glycol (Agilent technologies, Santa Clara, SA, USA; Cat. No. AT-122-3232E). Carrier gas (Helium) flow rate was 0.7 ml/min and inlet, column and detector temperatures were 175, 100 and 240 °C, respectively. Volatile free acid mix was used as the internal standard (Supelco. Saint-Quentin-Fallavier, France; Cat. No. CRM46975).
Data were collected and peaks integrated with OpenLAB software (Agilent technologies, Santa Clara, SA, USA). Values were expressed in M/g of feces and the ratio was calculated between D31 and D0.
Serine protease activity assay
About 200 mg of feces were diluted in 1 ml of distilled water, homogenized and centrifuged at 1000 g for 5 min. One hundred microliters of fecal supernatants were added to 100 µl of buffer (50 mM Tris-HCl pH 8, 1 mM CaCl2) containing 100 µM specific serine protease substrate (suc-phe-ala-ala-phe-pNA) (Bachem, Switzerland; Cat. No. 4013859) and incubated at 37 °C for 6 h. Substrate cleavage was measured at 400 nm with NUNC 96-well plates (ThermoFisher Scientific, Waltham, MS, USA) and normalized to the total feces weight.
Statistical analysis
Statistical analysis was performed with Prism 7 software (GraphPad, La Jolla, CA, USA). Data were expressed as mean ± standard error of mean (SEM). Colonic sensitivity to gradual CRD, body weight, distance moved, time spent in the hidden zone and microbiota analysis (taxonomy) were analyzed by two-way ANOVA followed by Sidak post hoc test for multiple comparisons. Rate comparisons were performed by Fisher’s exact test. Most comparisons were performed by the Student test. For non-Gaussian data, comparisons were performed by the non-parametric Mann Whitney U test (Unpaired data). A p-value ≤ 0.05 was considered statistically significant.
Supplementary information
Acknowledgements
This work was supported by co-financing from the Region Auvergne-Rhône-Alpes and FEDER in 2015 (“Thématiques émergentes”). Manon Defaye and Elodie Baudu received grants from the Auvergne-Rhône-Alpes Region. This work was supported by the « Ministère de la Recherche et de la Technologie », Inserm and University Clermont Auvergne [UMR1107, UMR1071]; INRA [USC-2018]; CNRS [UMR6023]. We thank Bruno Pereira for his help with statistical analysis (Unité de Biostatistiques, Direction de la Recherche Clinique (DRCI), CHU de Clermont-Ferrand, France) and the “Centre Imagerie Cellulaire Santé” (CICS) for the colon sections.
Author contributions
(M.D.1,2, D.A.1, F.D.1, F.A.C.2,a,b, P.P.1,3,a,b) study concept and design; (M.D.1,2, C.N.1,3,a,b, E.B.2,4, A.L.2, M.Maëva2, M.Mathieu2, M.M.2, I.W.1, V.B.4, J.B.2) acquisition of data; (M.D.1,2, C.N.1,3,a,b, B.C6,7,8,9, C.G.5, F.D.1, F.A.C.2,a,b, P.P.1,3,a,b) analysis and interpretation of data; (M.D.1,2, C.N.1,3,a,b, M.Mathieu.2, I.W.1, N.B.4 M.B.4, D.A.1, F.D.1, F.A.C.2,a,b, P.P.1,3,a,b) drafting of the manuscript; (N.B.4 M.B.4, D.A.1, F.D.1, F.A.C.2,a,b, P.P.1,3,a,b) obtaining funding; (A.G.1, N.B.4 M.B.4, D.A.1, F.D.1, F.A.C.2,a,b, P.P.1,3,a,b) study supervision.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Frédéric Antonio Carvalho and Philippe Poirier.
Contributor Information
Frédéric Antonio Carvalho, Email: frederic.carvalho@uca.fr.
Philippe Poirier, Email: ppoirier@chu-clermontferrand.fr.
Supplementary information
is available for this paper at 10.1038/s41598-020-66156-w.
References
- 1.Johnson AC, Greenwood-Van Meerveld B. The Pharmacology of Visceral Pain. in. Advances in pharmacology (San Diego, Calif.) 2016;75:273–301. doi: 10.1016/bs.apha.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Enck P, et al. Irritable bowel syndrome. Nat. Rev. Dis. Prim. 2016;2:16014. doi: 10.1038/nrdp.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drossman DA. Functional gastrointestinal disorders: what’s new for Rome IV? Lancet Gastroenterol. Hepatol. 2016;1:6–8. doi: 10.1016/S2468-1253(16)30022-X. [DOI] [PubMed] [Google Scholar]
- 4.Rodiño-Janeiro BK, Vicario M, Alonso-Cotoner C, Pascua-García R, Santos J. A Review of Microbiota and Irritable Bowel Syndrome: Future in Therapies. Adv. Ther. 2018;35:289–310. doi: 10.1007/s12325-018-0673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fond G, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2014;264:651–60. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 6.Lee YY, Annamalai C, Rao SSC. Post-Infectious Irritable Bowel Syndrome. Curr. Gastroenterol. Rep. 2017;19:56. doi: 10.1007/s11894-017-0595-4. [DOI] [PubMed] [Google Scholar]
- 7.Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat. Rev. Gastroenterol. Hepatol. 2010;7:163–73. doi: 10.1038/nrgastro.2010.4. [DOI] [PubMed] [Google Scholar]
- 8.Bercík P, et al. Visceral hyperalgesia and intestinal dysmotility in a mouse model of postinfective gut dysfunction. Gastroenterology. 2004;127:179–87. doi: 10.1053/j.gastro.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Beatty JK, Bhargava A, Buret AG. Post-infectious irritable bowel syndrome: mechanistic insights into chronic disturbances following enteric infection. World J. Gastroenterol. 2014;20:3976–85. doi: 10.3748/wjg.v20.i14.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Downs IA, Aroniadis OC, Kelly L, Brandt LJ. Postinfection Irritable Bowel Syndrome. J. Clin. Gastroenterol. 2017;51:869–877. doi: 10.1097/MCG.0000000000000924. [DOI] [PubMed] [Google Scholar]
- 11.Klem F, et al. Prevalence, Risk Factors, and Outcomes of Irritable Bowel Syndrome After Infectious Enteritis: A Systematic Review and Meta-analysis. Gastroenterology. 2017;152:1042–1054.e1. doi: 10.1053/j.gastro.2016.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan KSW. New Insights on Classification, Identification, and Clinical Relevance of Blastocystis spp. Clin. Microbiol. Rev. 2008;21:639–665. doi: 10.1128/CMR.00022-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alfellani MA, et al. Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop. 2013;126:11–18. doi: 10.1016/j.actatropica.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Rene BA, Stensvold CR, Badsberg JH, Nielsen HV. Subtype analysis of Blastocystis isolates from Blastocystis cyst excreting patients. Am. J. Trop. Med. Hyg. 2009;80:588–92. [PubMed] [Google Scholar]
- 15.Ramírez JD, et al. Geographic distribution of human Blastocystis subtypes in South America. Infect. Genet. Evol. 2016;41:32–35. doi: 10.1016/j.meegid.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Poirier P, et al. Development and Evaluation of a Real-Time PCR Assay for Detection and Quantification of Blastocystis Parasites in Human Stool Samples: Prospective Study of Patients with Hematological Malignancies. J. Clin. Microbiol. 2011;49:975–983. doi: 10.1128/JCM.01392-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Domínguez-Márquez MV, Guna R, Muñoz C, Gómez-Muñoz MT, Borrás R. High prevalence of subtype 4 among isolates of Blastocystis hominis from symptomatic patients of a health district of Valencia (Spain) Parasitol. Res. 2009;105:949–955. doi: 10.1007/s00436-009-1485-y. [DOI] [PubMed] [Google Scholar]
- 18.Olsen KEP, Christiansen DB, Nielsen HV, Stensvold CR. Blastocystis sp. Subtype 4 is Common in Danish Blastocystis-Positive Patients Presenting with Acute Diarrhea. Am. J. Trop. Med. Hyg. 2011;84:883–885. doi: 10.4269/ajtmh.2011.11-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tito Raul Y, Chaffron Samuel, Caenepeel Clara, Lima-Mendez Gipsi, Wang Jun, Vieira-Silva Sara, Falony Gwen, Hildebrand Falk, Darzi Youssef, Rymenans Leen, Verspecht Chloë, Bork Peer, Vermeire Severine, Joossens Marie, Raes Jeroen. Population-level analysis of Blastocystis subtype prevalence and variation in the human gut microbiota. Gut. 2018;68(7):1180–1189. doi: 10.1136/gutjnl-2018-316106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El Safadi D, et al. Children of Senegal River Basin show the highest prevalence of Blastocystissp. ever observed worldwide. BMC Infect. Dis. 2014;14:164. doi: 10.1186/1471-2334-14-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ragavan, N. D., Kumar, S., Chye, T. T., Mahadeva, S. & Shiaw-Hooi, H. Blastocystis sp. in Irritable Bowel Syndrome (IBS) - Detection in Stool Aspirates during Colonoscopy. Plos one10, e0121173 (2015). [DOI] [PMC free article] [PubMed]
- 22.Nourrisson Céline, Scanzi Julien, Pereira Bruno, NkoudMongo Christina, Wawrzyniak Ivan, Cian Amandine, Viscogliosi Eric, Livrelli Valérie, Delbac Frédéric, Dapoigny Michel, Poirier Philippe. Blastocystis Is Associated with Decrease of Fecal Microbiota Protective Bacteria: Comparative Analysis between Patients with Irritable Bowel Syndrome and Control Subjects. PLoS ONE. 2014;9(11):e111868. doi: 10.1371/journal.pone.0111868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rostami A, et al. Erratum to: the role of Blastocystis sp. and Dientamoeba fragilis in irritable bowel syndrome: a systematic review and meta-analysis. Parasitol. Res. 2017;116:2611–2612. doi: 10.1007/s00436-017-5556-1. [DOI] [PubMed] [Google Scholar]
- 24.Kesuma Y, Firmansyah A, Bardosono S, Sari IP, Kurniawan A. Blastocystis ST-1 is associated with Irritable Bowel Syndrome-diarrhoea (IBS-D) in Indonesian adolescences. Parasite Epidemiol. Control. 2019;6:e00112. doi: 10.1016/j.parepi.2019.e00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Audebert C, et al. Colonization with the enteric protozoa Blastocystis is associated with increased diversity of human gut bacterial microbiota. Sci. Rep. 2016;6:25255. doi: 10.1038/srep25255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nieves-Ramírez, M. E. et al. Asymptomatic Intestinal Colonization with Protist Blastocystis Is Strongly Associated with Distinct Microbiome Ecological Patterns. mSystems3 (2018). [DOI] [PMC free article] [PubMed]
- 27.Rooks MG, Garrett WS. Gut microbiota, metabolites and host immunity. Nat. Rev. Immunol. 2016;16:341–352. doi: 10.1038/nri.2016.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Defaye Manon, Nourrisson Céline, Baudu Elodie, Warwzyniak Ivan, Bonnin Virginie, Bonnet Mathilde, Barnich Nicolas, Ardid Denis, Delbac Frédéric, Carvalho Frédéric Antonio, Poirier Philippe. Efficient and reproducible experimental infections of rats with Blastocystis spp. PLOS ONE. 2018;13(11):e0207669. doi: 10.1371/journal.pone.0207669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cekin AH, et al. Blastocystosis in patients with gastrointestinal symptoms: a case–control study. BMC Gastroenterol. 2012;12:122. doi: 10.1186/1471-230X-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stark D, van Hal S, Marriott D, Ellis J, Harkness J. Irritable bowel syndrome: a review on the role of intestinal protozoa and the importance of their detection and diagnosis. Int. J. Parasitol. 2007;37:11–20. doi: 10.1016/j.ijpara.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 31.Toro Monjaraz EM, et al. Blastocystis Hominis and Chronic Abdominal Pain in Children: Is there an Association between Them? J. Trop. Pediatr. 2018;64:279–283. doi: 10.1093/tropej/fmx060. [DOI] [PubMed] [Google Scholar]
- 32.Salvador F, et al. Epidemiological and clinical profile of adult patients with Blastocystis sp. infection in Barcelona, Spain. Parasit. Vectors. 2016;9:548. doi: 10.1186/s13071-016-1827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poirier P, Wawrzyniak I, Vivarès CP, Delbac F, El Alaoui H. New insights into Blastocystis spp.: A potential link with irritable bowel syndrome. PLoS Pathog. 2012;8:1–4. doi: 10.1371/journal.ppat.1002545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farzaei MH, Bahramsoltani R, Abdollahi M, Rahimi R. The Role of Visceral Hypersensitivity in Irritable Bowel Syndrome: Pharmacological Targets and Novel Treatments. J. Neurogastroenterol. Motil. 2016;22:558–574. doi: 10.5056/jnm16001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leder K, Hellard ME, Sinclair MI, Fairley CK, Wolfe R. No correlation between clinical symptoms and Blastocystis hominis in immunocompetent individuals. J. Gastroenterol. Hepatol. 2005;20:1390–1394. doi: 10.1111/j.1440-1746.2005.03868.x. [DOI] [PubMed] [Google Scholar]
- 36.Puthia MK, Lu J, Tan KSW. Blastocystis ratti contains cysteine proteases that mediate interleukin-8 response from human intestinal epithelial cells in an NF-kappaB-dependent manner. Eukaryot. Cell. 2008;7:435–43. doi: 10.1128/EC.00371-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lim MX, et al. Differential regulation of proinflammatory cytokine expression by mitogen-activated protein kinases in macrophages in response to intestinal parasite infection. Infect. Immun. 2014;82:4789–801. doi: 10.1128/IAI.02279-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Camilleri M, et al. Intestinal barrier function in health and gastrointestinal disease. Neurogastroenterol. Motil. 2012;24:503–512. doi: 10.1111/j.1365-2982.2012.01921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dagci, H. et al. Epidemiological and diagnostic features of blastocystis infection in symptomatic patients in izmir province, Turkey. Iran. J. Parasitol. 9, 519–29 [PMC free article] [PubMed]
- 40.Nourrisson C, et al. On Blastocystis secreted cysteine proteases: a legumain-activated cathepsin B increases paracellular permeability of intestinal Caco-2 cell monolayers. Parasitology. 2016;143:1713–1722. doi: 10.1017/S0031182016001396. [DOI] [PubMed] [Google Scholar]
- 41.Saitou M, et al. Complex phenotype of mice lacking occludin, a component of tight junction strands. Mol. Biol. Cell. 2000;11:4131–42. doi: 10.1091/mbc.11.12.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hussein EM, Hussein AM, Eida MM, Atwa MM. Pathophysiological variability of different genotypes of human Blastocystis hominis Egyptian isolates in experimentally infected rats. Parasitol. Res. 2008;102:853–860. doi: 10.1007/s00436-007-0833-z. [DOI] [PubMed] [Google Scholar]
- 43.Denoeud F, et al. Genome sequence of the stramenopile Blastocystis, a human anaerobic parasite. Genome Biol. 2011;12:R29. doi: 10.1186/gb-2011-12-3-r29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gentekaki Eleni, Curtis Bruce A., Stairs Courtney W., Klimeš Vladimír, Eliáš Marek, Salas-Leiva Dayana E., Herman Emily K., Eme Laura, Arias Maria C., Henrissat Bernard, Hilliou Frédérique, Klute Mary J., Suga Hiroshi, Malik Shehre-Banoo, Pightling Arthur W., Kolisko Martin, Rachubinski Richard A., Schlacht Alexander, Soanes Darren M., Tsaousis Anastasios D., Archibald John M., Ball Steven G., Dacks Joel B., Clark C. Graham, van der Giezen Mark, Roger Andrew J. Extreme genome diversity in the hyper-prevalent parasitic eukaryote Blastocystis. PLOS Biology. 2017;15(9):e2003769. doi: 10.1371/journal.pbio.2003769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cenac N, et al. Role for protease activity in visceral pain in irritable bowel syndrome. J. Clin. Invest. 2007;117:636–647. doi: 10.1172/JCI29255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Róka R, et al. A pilot study of fecal serine-protease activity: a pathophysiologic factor in diarrhea-predominant irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 2007;5:550–5. doi: 10.1016/j.cgh.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 47.Gecse K, et al. Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity. Gut. 2008;57:591–599. doi: 10.1136/gut.2007.140210. [DOI] [PubMed] [Google Scholar]
- 48.Ibeakanma C, et al. Brain–Gut Interactions Increase Peripheral Nociceptive Signaling in Mice With Postinfectious Irritable Bowel Syndrome. Gastroenterology. 2011;141:2098–2108.e5. doi: 10.1053/j.gastro.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Tooth D, et al. Characterisation of faecal protease activity in irritable bowel syndrome with diarrhoea: origin and effect of gut transit. Gut. 2014;63:753–60. doi: 10.1136/gutjnl-2012-304042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steck N, Mueller K, Schemann M, Haller D. Bacterial proteases in IBD and IBS. Gut. 2012;61:1610–1618. doi: 10.1136/gutjnl-2011-300775. [DOI] [PubMed] [Google Scholar]
- 51.Shah E, Rezaie A, Riddle M, Pimentel M. Psychological disorders in gastrointestinal disease: epiphenomenon, cause or consequence? Ann. Gastroenterol. 2014;27:224–230. [PMC free article] [PubMed] [Google Scholar]
- 52.Rosa PB, et al. Folic acid prevents depressive-like behavior induced by chronic corticosterone treatment in mice. Pharmacol. Biochem. Behav. 2014;127:1–6. doi: 10.1016/j.pbb.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 53.Crumeyrolle-Arias M, et al. Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats. Psychoneuroendocrinology. 2014;42:207–17. doi: 10.1016/j.psyneuen.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 54.Cho H, et al. Voluntary movements as a possible non-reflexive pain assay. Mol. Pain. 2013;9:25. doi: 10.1186/1744-8069-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yason JA, Liang YR, Png CW, Zhang Y, Tan KSW. Interactions between a pathogenic Blastocystis subtype and gut microbiota: in vitro and in vivo studies. Microbiome. 2019;7:30. doi: 10.1186/s40168-019-0644-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.X.-Y. Z, et al. Visceral hypersensitive rats share common dysbiosis features with irritable bowel syndrome patients. World J. Gastroenterol. 2016;22:5211–5227. doi: 10.3748/wjg.v22.i22.5211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao K, Yu L, Wang X, He Y, Lu B. Clostridium butyricum regulates visceral hypersensitivity of irritable bowel syndrome by inhibiting colonic mucous low grade inflammation through its action on NLRP6. Acta Biochim. Biophys. Sin. (Shanghai). 2018;50:216–223. doi: 10.1093/abbs/gmx138. [DOI] [PubMed] [Google Scholar]
- 58.Hugenholtz Floor, Davids Mark, Schwarz Jessica, Müller Michael, Tomé Daniel, Schaap Peter, Hooiveld Guido J. E. J., Smidt Hauke, Kleerebezem Michiel. Metatranscriptome analysis of the microbial fermentation of dietary milk proteins in the murine gut. PLOS ONE. 2018;13(4):e0194066. doi: 10.1371/journal.pone.0194066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pozuelo M, et al. Reduction of butyrate- and methane-producing microorganisms in patients with Irritable Bowel Syndrome. Sci. Rep. 2015;5:12693. doi: 10.1038/srep12693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sun Q, Jia Q, Song L, Duan L. Alterations in fecal short-chain fatty acids in patients with irritable bowel syndrome: A systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e14513. doi: 10.1097/MD.0000000000014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dalile B, Van Oudenhove L, Vervliet B, Verbeke K. The role of short-chain fatty acids in microbiota–gut–brain communication. Nature Reviews Gastroenterology and Hepatology. 2019;16:461–478. doi: 10.1038/s41575-019-0157-3. [DOI] [PubMed] [Google Scholar]
- 62.Zimmermann M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain. 1983;16:109–10. doi: 10.1016/0304-3959(83)90201-4. [DOI] [PubMed] [Google Scholar]
- 63.Larauche M, Gourcerol G, Million M, Adelson DW, Taché Y. Repeated psychological stress-induced alterations of visceral sensitivity and colonic motor functions in mice: influence of surgery and postoperative single housing on visceromotor responses. Stress. 2010;13:343–54. doi: 10.3109/10253891003664166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aissouni Y, et al. Acid-Sensing Ion Channel 1a in the amygdala is involved in pain and anxiety-related behaviours associated with arthritis. Sci. Rep. 2017;7:43617. doi: 10.1038/srep43617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Slattery DA, Cryan JF. Using the rat forced swim test to assess antidepressant-like activity in rodents. Nat. Protoc. 2012;7:1009–1014. doi: 10.1038/nprot.2012.044. [DOI] [PubMed] [Google Scholar]
- 66.Tulstrup Monica Vera-Lise, Christensen Ellen Gerd, Carvalho Vera, Linninge Caroline, Ahrné Siv, Højberg Ole, Licht Tine Rask, Bahl Martin Iain. Antibiotic Treatment Affects Intestinal Permeability and Gut Microbial Composition in Wistar Rats Dependent on Antibiotic Class. PLOS ONE. 2015;10(12):e0144854. doi: 10.1371/journal.pone.0144854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Caporaso JG, et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Edgar RC, Flyvbjerg H. Error filtering, pair assembly and error correction for next-generation sequencing reads. Bioinformatics. 2015;31:3476–3482. doi: 10.1093/bioinformatics/btv401. [DOI] [PubMed] [Google Scholar]
- 69.Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26:2460–2461. doi: 10.1093/bioinformatics/btq461. [DOI] [PubMed] [Google Scholar]
- 70.Segata Nicola, Izard Jacques, Waldron Levi, Gevers Dirk, Miropolsky Larisa, Garrett Wendy S, Huttenhower Curtis. Metagenomic biomarker discovery and explanation. Genome Biology. 2011;12(6):R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.