Abstract
Cannabis-inspired medical products are garnering increasing attention from the scientific community, general public, and health policy makers. A plethora of scientific literature demonstrates intricate engagement of the endocannabinoid system with human immunology, psychology, developmental processes, neuronal plasticity, signal transduction, and metabolic regulation. Despite the therapeutic potential, the adverse psychoactive effects and historical stigma, cannabinoids have limited widespread clinical application. Therefore, it is plausible to weigh carefully the beneficial effects of cannabinoids against the potential adverse impacts for every individual. This is where the concept of “personalized medicine” as a promising approach for disease prediction and prevention may take into the account. The goal of this review is to provide an outline of the endocannabinoid system, including endocannabinoid metabolizing pathways, and will progress to a more in-depth discussion of the therapeutic interventions by endocannabinoids in various neurological disorders.
Keywords: Endocannabinoid system, Anandamide, 2-Arachidonyl glycerol, Cannabinoid receptor, Neurological disorder, Traumatic brain injury, Alzheimer’s disease, Parkinson’s disease, Amyloid lateral sclerosis, Cancer, Pain, Epilepsy, Multiple sclerosis, Huntington’s disease, Schizophrenia, Stroke, Anxiety, Depression, Multi-professional expertise, Therapeutic strategies, Health policy, Disease management, Predictive preventive personalized medicine (PPPM)
Introduction
Cannabis sativa is an herbaceous plant widely recognized for its psychotropic activity and recreational abuse. Undoubtedly, the most recognized cannabis-derived molecule is delta-9-tetrahydrocannabinol (Δ9-THC), which acts on the endocannabinoid system (ECS) and mediates the psychotropic effects of marijuana. Regardless of this activity, marijuana is being used for recreational purpose for centuries. In addition, anecdotal reports of medicinal value coupled with enormous interest from the public in natural medical products have sparked a keen interest in understanding the potential clinical utility of cannabis and targeted modulation of ECS. Indeed, oral formulations of cannabinoids (i.e., nabilone, dronabinol) having Δ9-THC may be useful for the treatment of nausea and vomiting in cancer patients undergoing chemotherapy [1, 2]. Despite potential prophylactic and/or therapeutic functions, the historical stigma of cannabinoids limited the performance of randomized controlled clinical trials to demonstrate the utility of cannabis in alleviating human diseases.
Incidences of neurological disorders increase manifold globally with the rise in life expectancy. According to a systematic analysis, neurological disorders were leading in disability-adjusted life years (DALYs) with 276 million incidences and was second most cause of death at 9 million in 2016, whereas stroke (42.2%), migraine (16.3%), and Alzheimer’s disease (AD) and other dementia (10.4) were highest contributors for DALYs [3, 4]. The DALYs and death counts due to neurological diseases increased by 15% and 39% respectively in between 1990 and 2016 [3]. According to WHO report, global DALYs and death for all combined neurological disorders could reach up to 6.77% and 12.22% respectively [5], and therefore, a close attention and action are needed from medical and scientific world to emphasize on therapeutic intervention of these diseases.
While dysregulation of the ECS is associated with detrimental outcomes in neurological injuries, targeted modulation of ECS remains an understudied approach to improve outcomes [6–16]. Of note, preclinical studies by our group and others found that selective activation of the non-psychoactive cannabinoid receptor 2 (CB2R) reduced neuropathology after a variety of neuropsychiatric and neurodegenerative diseases, including cerebral ischemia [11, 17, 18], traumatic brain injury (TBI) [15, 19], neuropathic pain [20], stroke [11], neurodegenerative disease [21–23], depression [24], anxiety [25], schizophrenia-like behaviors [26], and drug addiction [27–29]. The goal of this review is to describe the functions of the ECS with respect to neurological function, including potential utility in neurological impairments. With this understanding, the medical community can use an evidence-based approach to inform public policy regarding the consumption of cannabis products as therapeutics to improve brain health.
ECS: understanding components and their functions in health
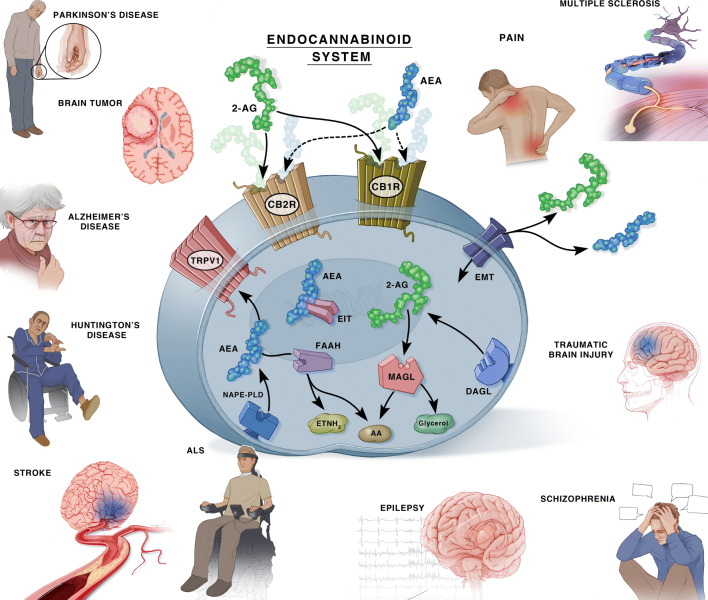
ECS is an endogenous regulatory system comprised of ligands (endocannabinoids), cannabinoid receptors (CBRs), and endocannabinoid synthesizing/degrading enzymes (Fig. 1). In the following sections, we discuss the different roles and physiological functions of ECS and how dysfunction within the ECS may result in neuropathology.
Fig. 1.
The endocannabinoid system in normal cellular homeostasis and its dysregulation in different neuropathologies. Schematic diagram shows ECS and its different components in normal cellular physiology. The dysregulated ECS as result of injury or pathologies to brain, becomes inefficient to maintain cellular homeostasis, and exaggerates the progression of different neurological disorders
Endogenous cannabinoids: ligands, metabolism, and receptors
Endocannabinoids and their synthesis
Endocannabinoids are arachidonate-based lipids (eicosanoids), such as anandamide (N-arachidonoylethanolamide, AEA) and 2-arachidonoylglycerol (2-AG), which are endogenous ligands to the cannabinoid receptors (CB1R and CB2R) [30, 31]. Both ligands AEA and 2-AG act as neurotransmitters affecting behavior in a manner different to that of THC [32], which is an exogenously derived cannabinoid and often has multiple side effects [33]. Both endogenous ligands are originated from arachidonic acid, as needed, to meet the physiological requirements of the body on a situational basis [34]. AEA synthesis involves multiple paths involving different phospholipases. AEA synthesis generally begins with N-arachidonoyl phosphatidyl ethanol (NAPE) as its starting material. NAPE is hydrolyzed primarily by NAPE-phospholipase D (NAPE-PLD) into products which subsequently form AEA [35–37]. 2-AG synthesis generally involves sequential hydrolysis of an arachidonoyl-containing phosphatidylinositol 4,5-bisphosphate (PIP2) by a phospholipase C-beta (PLC-β) [38, 39] to form diacylglycerol, which is then hydrolyzed by diacylglycerol lipase (DAGL) to form 2-AG [40]. While both endocannabinoids, AEA and 2-AG, bind to CBRs, they exhibit different responses, efficacy, and specificities. In general AEA, which has a moderate affinity to both CBRs, is activated in response to CNS stress and act as a response to pain in peripheral nervous system (PNS) [33, 41–43]. In contrast, 2-AG which is formed as an intermediate in several lipid metabolism pathway, is more abundant than AEA and thus, has high efficacy at both CBRs [33, 42–47].
Endocannabinoid metabolism
The enzyme fatty acid amino hydrolase (FAAH) degrades all fatty acid amides, including AEA [48]. In addition, cyclooxygenase-2 (COX-2) enzymatically degrades AEA to generate prostamides [49–51]. 2-AG, the most abundant endocannabinoid within the CNS, is primarily metabolized by three hydrolytic enzymes: monoacylglycerol lipase (MAGL) and alpha/beta domain hydrolases 6 and 12 (ABHD6 and 12) [51, 52]. Beyond this, 2-AG may additionally be degraded by COX-2 and FAAH enzymes [53]. Degradation by COX-2 occurs in neural tissue and results in the production of prostaglandin E2 (PGE2), an excitatory oxidative metabolite also found to be involved with synaptic transmission and plasticity [32]. 2-AG can also serve as an intermediate for lipid synthesis by acting as a source of arachidonic acid during prostaglandin synthesis [54].
Cannabinoid receptors
There are two primary cannabinoid receptors—CB1R and CB2R—which bind with different endogenous or exogenous cannabinoids to mediate the downstream effects. Both receptors share 44% homology in amino acid sequence [55] and act as Gi/o-linked G protein-coupled receptors (GPCRs). Both receptors can inhibit adenylyl cyclase and can activate mitogen-activated protein kinase (MAPK) [56, 57]. However, CB1Rs may also inhibit N or P/Q-type calcium channels and may activate inwardly correcting potassium channels [58, 59]. Although both these receptors possess similar binding pattern for cannabinoids [55], they acquire different functional roles (Table 1). CB1R is psychoactive whereas CB2R is thought to lose this effect.
Table 1.
Comparison between cannabinoid receptors CB1R and CB2R. CB1R and CB2R are two main cannabinoid receptors that share similar ligand binding pattern and has 44% homology in amino acid sequence in whole protein and 68% homology in transmembrane domain [55, 57]. However, both receptors act as Gi/o-linked GPCRs [56, 57, 479, 480] and are functionally quite different as highlighted in the given table
| Properties | Cannabinoid receptor 1 (CB1R) | Cannabinoid receptor 2 (CB2R) |
|---|---|---|
| History |
a. First discovered from rat brain P2 membrane and synaptosomes in 1988 [55, 481] b. Cloned for the first time from rat cerebral cortex cDNA library [55, 56] |
a. First discovered and cloned from human promyelocytic leukemia cell HL60 cDNA [55, 57] b. Located at chromosome 1p36 [55] |
| Localization |
a. Mainly in the CNS, abundant in basal ganglia, cerebellum, cortex, and hippocampus [55, 483, 484] b. Also, present in the pituitary, thyroid, gonads, upper airways, adrenal, liver, and uterus [483, 484] |
a. Mainly on immune cells and keratinocytes [483, 484] b. CB2R coexists with CB1R in the retina, heart, pancreas, stomach, bone, digestive tract, and CNS (microglia and astrocytes) in certain conditions [55, 483–487] c. Predominantly on glia cells and postsynaptic neurons [483–486] |
| Ligands |
a. Shows a strict requirement for pentyl or longer alkyl tails in ligands [483, 484] b. AEA has high affinity for CB1R [Ki = 89 nM] with EC50 = 31 nM [338, 488–491] c. 2-AG is full agonist to CB1R, with lower affinity [Ki = 472 nM] than AEA and with EC50 = 519 nM [338, 492–496] d. Binds with THC [Ki = 41 nM] [338] |
a. CB2R recognizes classical cannabinoids with shorter alkyl chains—dimethylpropyl or dimethylethyl [497, 498] b. AEA has comparatively lower affinity for CB2R than CB1R [Ki = 371 nM; EC50 = 27 nM] [338, 488–492, 494, 496, 499] c. 2-AG acts as a full agonist to CB2R [Ki=1400 nM] and has EC50=618 nM) [42, 338, 492, 494, 496, 500, 501] d. Binds with THC [Ki = 36 nM] [338] and with mildly psychoactive component cannabinol (CBN) [483, 484] |
| Functions |
a. Has psychoactive property [483, 484] b. Stimulates dopaminergic reward pathway [502] c. Motivates to eat, smoke or intake of drugs [502] d. Required for synaptic transmission [483, 484] e. CB1R signaling includes [58, 499, 503]: • Inhibition of forskolin-stimulated adenylyl cyclase • Inhibition of N-, P-, and Q-type calcium channels • Activation of inwardly rectifying potassium channels f. Plays an essential role in: • Fine-tuned motor control [504–506] • Central and peripheral regulation of food intake [504–506] |
a. Has immunological property [483, 484] • Regulates leukocytes adhesion and rolling on endothelium [70, 507–510] • Activation of CB2R improves microvascular circulation and protects BBB [70, 507–509, 511] • Regulates T cell differentiation [512, 513] • Inhibits melanoma cell transendothelial migration [514] b. CB2R may contribute to neuronal plasticity in mouse hippocampal CA3 and CA2 pyramidal neurons [64] c. CB2R signaling includes: • Phosphoinositide 3-kinase pathways [515] • Activation of de novo ceramide production or cyclooxygenase-2 (COX-2) induction [516] |
CB1Rs are found predominantly in the CNS on presynaptic axon terminals and stomata [60]. In particular, CB1Rs are expressed heavily in cortical association areas and the direct nigrostriatal pathway but less in the primary somatosensory cortex. Subcortically, CB1Rs are localized in the amygdala [61, 62], basal ganglia [63], hippocampus [64, 65], and cerebellum [66]. CB2R has lower expression in CNS, but is more involved with peripheral immune cells [67], including lymphocytes, followed by natural killer (NK) cells, monocytes, neutrophils, and T helper cells [68]. Consistent with higher expression on immune cells, CB2R is predominant found on microglia within the CNS, with lesser expression noted in CNS vascular elements [69, 70]. High expression of CB2R mRNA was also observed in ventral tegmental area (VTA), specially on dopaminergic neurons [71], with reports showing most neuronal CB2R localization post-synaptically on the cell body [64, 71]. In contrast to the constitutive expression of CB1R, CB2Rs are strongly induced following trauma or pathology [15, 63], making this a potentially interesting target for disease/injury mitigation. This inducible activity has also be correlated with neuropathic pain [20], stroke [11], traumatic brain injury [19], neurodegenerative disease [21–23], depression [24], anxiety [25], schizophrenia-like behaviors [26], and drug addiction [27–29].
Besides classical CBRs, non-cannabinoid receptors also may be involved with the ECS. For instance, transient receptor potential (TRP) channels may also be influenced by cannabinoids in the context of peripheral pain and temperature sensation [72]. Of the TRP receptors, TRPV1 has garnished the most attraction given its inducibility and affiliation with immune cells. Peroxisome proliferator-activated receptors (PPAR-α and PPAR-γ) also may be influenced by cannabinoid action to regulate gene transcription/regulation [73].
Physiological functions
ECS is a complex system that is intricately involved with human immunology, psychology, developmental process, neural plasticity, signal transduction, and metabolic regulation. With interplay into so many physiological components, understanding ECS and its implication in CNS homeostasis is critical to explore the therapeutic potential in various neurological diseases.
Neural transmission and synaptic regulation
Metabotropic suppression of inhibition/excitation (MSI/MSE) is also known as “synaptically evoked suppression of inhibition or excitation” or “endocannabinoid-mediated short-term depression” [32]. MSI/MSE is activated by the postsynaptic activation of Gq/11-linked GPCR which then activates PLC-beta to create diacylglycerol (DAG). This DAG gets deacetylated by diacylglycerol lipase (DAGL) to synthesize 2-AG which then diffuses presynaptically to CB1Rs and suppresses synaptic transmission [74]. This suppression is mediated by various GPCRs linked to Gq/11 including metabotropic glutamate receptor 1 (mGluR1) and 5 (mGluR5), M1 and M3 muscarinic receptor, orexin-A receptor, cholecystokinin A receptor, and alpha1-adrenergic receptor [75].
Endocannabinoid-mediated long-term depression (eLTD) is the final mode of retrograde suppression and exhibits a long-lasting inhibition through multiple mechanisms primarily through endocannabinoid-induced homo-/heterosynaptic transmission. Homosynaptic eLTD is much more prominent at the glutamatergic synapse of ventral and dorsal striatum [76, 77]. In contrast, heterosynaptic eLTD affects adjacent synapses to the one being stimulated. Both types of eLTD work in various capacities throughout CNS including hippocampal inhibitory synapses via adenylyl cyclase inhibition as well as cortical circuit maturation [78–80]. There is research indicating that by removing inhibition of eLTD, inhibitory synapses could increase dendritic excitability, thus potentiating excitatory transmission over a narrow spatial domain [81]. Finally, an autonomous self-inhibition exists as 2-AG can directly suppress neuronal excitability especially during intense neuron stimulation, which activates somatic CB1Rs and somatic potassium conductance via an inward rectifying K channel [82–84].
The two cannabinoid receptors converge on some functions but are divergent in others due to a variety of ligand diversification. CB1R is localized on presynaptic neurons, modulates neurotransmission, and plays a role in neuronal excitability by suppressing exogenous or endogenous cannabinoid binding [60]. Its activation decreases presynaptic GABA release, eliminates GABAergic inhibitory control of postsynaptic neurons, and excites postsynaptic neurons through disinhibition [85, 86]. CB2R, on the other hand, is described as a “modulatory volume transmitter” which can gradually control the strength of nociception. In the CNS, CB2Rs have lower expression levels than CB1Rs which can explain their inability to respond to cannabinoids under physiologic conditions [69, 70]. CB2Rs, however, are expressed abundantly in neuronal post-synaptic somatodendritic region, suggesting an opposing effect from CB1Rs [66, 87]. Activation of these receptors reduces VTA-DA neuron firing and excitability which may aid in neuroprotection by hyperpolarizing membrane potential and inhibits postsynaptic neuronal function [32]. Thus, the ECS plays vital role in both short-term and long-term synaptic plasticity [88–93].
Immune regulation
The release of endocannabinoids within the injured CNS enhances endogenous neuroprotection via undefined mechanisms [70, 94–96]. We reported upregulated CB2R expression on myeloid cells with unaltered cerebral CB1R mRNA expression within days of experimental TBI [15]. Functionally, we and others showed that selective activation of CB2R reduced inflammation, attenuated edema, limited disruption of the BBB, improved cerebral perfusion, and enhanced behavioral outcomes post-TBI [15, 70]. Moreover, CB2R activation is associated with anti-inflammatory effects in preclinical models for atherosclerosis [97], multiple sclerosis [98], Alzheimer’s disease [99], and arthritis [100]. Interestingly, early treatment with CB2R agonist AM1241 suppressed microglial activation in stroke rats, while the same agonist did not show any significant effect when administered in delayed manner [11].
Administration of the selective CB2R agonist, JWH133, shifted macrophages from a pro-inflammatory (M1) state into an anti-inflammatory (M2) state after acute liver failure, via a mechanism postulated to involve negative regulation of TLR4 [101]. Inhibition of TLR4 mitigates hypoperfusion-induced cognitive dysfunction and protects the BBB and white matter by reducing autophagy and inflammation [102–106]. Interestingly, pharmacological inhibition of MAGL, a principal 2-AG metabolizing enzyme, reduced macrophage infiltration during liver fibrosis [107]. Further, expression of macrophage MAGL inhibits tumor progression by promoting CD8+ T cell-mediated inflammation, while MAGL deficiency promoted CB2R/TLR4-dependent macrophage activation and suppression of inflammation [108]. CNS accumulation of infiltrating macrophages and TH cells were associated with parenchymal inflammation and neurodegeneration after experimental TBI or in resected brain tissue from TBI patients [109, 110]. Whereas the TH1/TH2 ratio remained unchanged in pediatric TBI patients [111], TH17 cells were increased after comorbid post-traumatic stress disorder with mild TBI in rats [112–114], suggesting a role for TH polarization in chronic neurological injury. CB2R agonist, GP1a, significantly reduced macrophage infiltration in the acute period after insult and protected CBF by polarizing macrophages into M2 (anti-inflammatory) phenotypes [15]. Further, CB2R agonists, β-caryophyllene, and COR167 were able to inhibit demyelination through modulating T cells [115, 116]. Although CB2R is highly recognized as anti-inflammatory receptor on immune cells, the role of other components in immune regulation cannot be ignored, and therefore, studies specifically focused on different components of ECS should be encouraged.
ECS and neurological diseases
The association of the ECS in different physiological processes, such as synaptic plasticity and neuronal transmission, advances the probability of its role in neurological recovery [11–16, 117]. Indeed, promising results have demonstrated that modulation of the ECS attenuates key features of neurological injury, including neurodegeneration, excitotoxicity, and immunomodulation [118]. Along these lines, activation of CB1R decreased neuronal excitotoxicity, whereas CB2R activation limited post-ischemic [17] and post-traumatic inflammation [15]. Thus, cannabis has the potential to influence injury progression involved in neurodegeneration and neurological recovery. In the following subsections, we discuss the evidence supporting a potential role for cannabinoids in a variety neurological disorders.
Traumatic brain injury: modulation of ECS improves recovery post TBI
Traumatic brain injury (TBI) is described as occurring in a series of two separate events [118]. The first insult consists of a purely mechanical trauma, resulting in cell death and axonal injury through vascular damage and edematous pressure. The secondary injury follows the mechanical damage and activates apoptotic pathways within surrounding neural tissues through the release of glutamate-mediated excitotoxicity and Ca2+ influx [119, 120]. Such secondary damage also involves cerebrovascular derangements and immunologic activation. This twofold positive cycle consisting of both mechanical and self-regulated cellular components complicates the clinical management of TBI [121].
Reduced CB1R expression negatively correlated with edema formation and behavioral impairments while increased, post-traumatic expression of CB2R was associated with higher neurological deficits after experimental TBI in rodents [19]. In line with these data, an increased ratio of CB2R density was observed in a porcine pediatric fluid percussion injury model of TBI [122]. Functionally, mice exposed to CB2R agonists, or CB1R antagonists, or inhibitors of cannabinoid degradation demonstrated a reduction in neurodegeneration [123]. In addition, CB2R agonists reduced lymphocyte rolling and adhesion, which can ameliorate lesion size and improve motor function [124]. Interestingly, repeated stress-induced loss of CB2R deprived improvement post TBI in females, while high basal level of CBR expressions in young naive females protected against TBI [125], suggesting a possible role for the ECS in modifying TBI outcomes.
Endocannabinoids 2-AG and AEA seem to play a major role in the neuromodulation after TBI. A transient increase in 2-AG at the injured site was observed and was thought to serve as a protective factor, while inhibition of this protective effect by SR-141716A, a CB1R antagonist, showed increasingly detrimental outcomes post TBI [126]. Further, exogenous 2-AG administration reduced edema, inhibited transactivation of the nuclear factor NF-kB, protected BBB, and reduced pro-inflammatory cytokine mRNA (Il-1β, TNFα, and IL-6) [127–129]. However, deletion of CB1R eliminated these effects, suggesting that CB1R receptors mediated the protective effects of exogenous 2-AG [128]. While direct effects of AEA or 2-AG on traumatic brain are not entirely explored, inhibition of specific metabolizing enzymes (e.g., FAAH, MAGL, and ABHD6) have shown promise in modulating cellular and molecular hallmarks of TBI pathology, such as cell death, excitotoxicity, inflammation, cerebrovascular breakdown, and cell death [12, 130–135], and improved functional outcomes [118]. JZL184, an inhibition of MAGL, a primary metabolizing enzyme for 2-AG, showed improved neurological recovery and reduced astrocytosis, synaptic hyperexcitability, and glutamate dyshomeostasis up to 2 weeks after mild TBI in rats [130]. The protein aggregates such as amyloid-β plaques [136], p-tau [137], and TDP-43 [138], found to be accumulated in traumatic brain within hour after axonal damage [136], were reduced by treating with MAGL inhibitors [12]. Further, inhibition of MAGL after repetitive mild closed TBI reduced inflammation, Aβ plaque formation, and tau phosphorylation, while improving synaptic transmission, recovering spatial memory, and preventing chronic traumatic encephalopathy (CTE) [12, 135]. Thus, inhibition of MAGL protected against TBI-induced microglial activation [12, 133], whereas inhibition of ABHD6 promoted microglia/macrophage shift from a pro-inflammatory M1 to an anti-inflammatory M2 phenotype possibly via upregulation of CBRs and inhibition of iNOS and COX-2 [131]. In addition, inhibition of FAAH restored the level of AEA [132], prevented microglial activation and BBB disintegration [133], activated CB2R receptors [139], and minimized COX-2 and iNOS activities [134]. Inhibition of FAAH further increased synaptophysin [134], a synaptic vesicle protein whose elimination impairs object recognition and spatial learning in mice [140], and prevented amyloid precursor protein and phosphorylation of tau protein [132]. While the mechanism of protection of BBB by ECS is not known completely, AEA decreased BBB permeability via TRPV1 in ischemic stroke [141]. Given that activation of TRPV1 receptors disrupts BBB integrity [142], it is possible that AEA, as a partial agonist at TRPV1 channels [143], maybe be acting as a functional antagonist against a high efficacy endogenous ligand.
Interestingly, cannabinoids are also shown to improve effect of exogenous drugs against traumatic injury. For example, modulation of CB2R by SMM-189 or raloxifene, a FDA-approved estrogen receptor-targeting drug reduced blast-induced visual impairment and retinal pathology post TBI [144, 145]. Similarly, leptin, a hormone that regulates energy balance, showed its neuroprotective effect against TBI via modulation of CB2R which was attenuated in presence of CB2R antagonist AM630 [146]. In addition, protective effect of minocycline after TBI was abolished by treatment with CB1R or CB2R antagonists (AM251 or AM630, respectively) [147]. Estradiol decreased the number of TBI-induced immunoreactive astrocytes, which was inhibited by CB1R/CB2R antagonists, while also increasing cerebral cortex mRNA levels of CB2Rs [148]. Thus, it can be claimed that eCB receptors in response to TBI may exert effect via endocrine as well as paracrine signaling mechanisms.
Use of marijuana either alone or with other drugs is common among TBI (single or multiple impact) patients that may affect the existing mental health and may lead to higher mortality [149, 150]. An observational study in Colorado revealed three common reasons of cannabis use—recreational (72%), to reduce stress/anxiety (62%), and to improve sleep (55%) among TBI victims [151]. One of the very interesting results published by Nguyen et al. investigated the relation between THC consumption and mortality after TBI [152]. Out of 446 patients included in study, 82 patients (18.4%) were found THC(+) and showed decreased mortality (2.4%; 2 deaths) in comparison to 42 deaths (11.5%) in THC(−) screened group [152].
A recent study with 307 acute concussion patients with average age 33.7 years did not observe significant impact on recovery by continuous use of cannabis, cigarette, and alcohol within 4 weeks of injury. However, use of cannabis was found to be associated with lower severity than the other two [153]. Most of the time patients are indulged in cannabis use post-injury, unaware of its proven benefits or multiple effects [151, 154]. Moreover, cannabis abuse may cause neurological stress and enhance risk of psychosis in adolescent patients and may outweigh its potential therapeutic benefits [155]. However, there is paucity of extensive data on efficacy and efficiency of natural cannabinoids in TBI, and therefore, more extensive studies on cannabis use in TBI and a strict guideline for use of cannabis and patient management must be incorporated clinically to avoid unwanted effects of cannabis abuse.
Stroke: cannabinoids reduce infarct volume
Stroke is one of the debilitating pathologies and has 13–35% of first month case-fatality rate [156]. The percentage of young population receiving stroke is alarmingly increasing and involves many factors such as genetic predisposition, alcohol consumption, sedentary lifestyle, and hypertension. Polivka et al. identified two less explored factors—primary vascular dysregulation and Flammer syndrome (FS)-associated symptoms in the disposition of young age stroke [156]. Therefore, innovative screening programs, targeted risk-mitigating measures, and exploration of new treatment options emerge as new therapeutic strategies for treatment of stroke.
Ischemic stroke has been reported to alter ECS in both clinical and preclinical conditions, indicating an important role of this system in normal blood circulation [17]. A recent meta-analysis by England and colleagues revealed that all subclasses of cannabinoids, cannabis-derived, synthetic and specific CB1R, and CB2R agonists significantly reduced infarct volume in transient/permanent ischemia and improve both early and late functional outcomes in experimental stroke [157]. Further, a selective and potent CB1R/CB2R agonist TAK-937 reduced infarct volume and improved functional outcomes in middle cerebral artery occluded (MCAO) rats, while minimizing infarct volume and S100β release in CSF following middle cerebral artery occlusion in non-human primates [158]. Similarly, administration of CB1R agonist HU-210 significantly reduced motor disability and infarct volume via hypothermia in a dose-dependent manner and was useful 4 h after stroke onset [159]. CB2R agonist JWH133 promoted neuroblast migration into lesioned tissue to encourage neurogenesis [160]. Interestingly, early treatment with CB2R agonist AM1241 suppressed microglial activation in stroke rats, while delayed treatment did not show any significant effect [11]. Further, exogenous AEA and 2-AG in combination reduced infarct size in focal ischemic rats, but could not facilitate effects alone [161]. AEA has been reported to protect BBB permeability in ischemic stroke, possibly through TRPV1 [141]. Given that activation of TRPV1 receptors disrupts BBB integrity [142], it is possible that AEA, being partial agonist to TRPV1 channels [143], may be acting as a functional antagonist in presence of stroke-induced endogenous agonist.
Phytocannabinoid CBD reduced the ischemia-induced gliosis, neuronal loss, and excitotoxicity to protect behavioral functions in neonatal MCAO rats [162]. Moreover, CBD reduced brain edema and BBB permeability associated with ischemic condition [163] and was also effective in diabetes-related atherosclerosis [164]. In mouse and piglet models of stroke, CBD improved cerebral blood flow [165, 166]. CBD protected cerebral hemodynamic and produced beneficial cardiac effects in stressful conditions, but not in normal condition [167, 168]. CBD showed trends to infarct reduction with administration of less than 6 h after stroke onset [157] and showed functional improvements even at the later time point [169]. Multiple targets have been reported to mediate the neuroprotective effects of CBD such as a combination of a potent antioxidant, immunosuppression, and anti-inflammatory actions [170]. However, CBD has negligible activity on CBRs, but may interfere with the ECS via non-cannabinoid receptors such as 5-hydroxytryptamine 1A receptors, adenosine receptors, TRPV1, and nuclear receptors of the peroxisome proliferator-activated receptor family [170]. Another component of cannabis, THC also showed trends to infarct reduction with administration of less than 4 h [157]. However, THC inhibits voltage-dependent calcium channels via CB1R and, thus, reduces excessive glutamate release, hypothermia, and loss of CBF [171, 172]. Further, THC, when acting on the CB2R on immune cells, was found to decrease the severity of stroke. Low oral doses of THC modulated myeloid and lymphoid cells to improve ischemia in atherosclerosis model [173].
Although numerous studies have evaluated cannabinoids and ECS in experimental stroke, reports are somewhat conflicting and thus start a debate on role of cannabinoids in stroke. A meta-study on 98 stroke patients having mean age 32.7 ± 12 years were identified as chronic cannabis users and thus indicated a correlation between cannabis consumption and incidence of stroke [174]. Additionally, pre-ischemic administration of 2-AG enlarged infarct volume and reduced CBF via platelet aggregation [175–177]. A possible explanation of this event occurred through an increase in downstream product arachidonic acid stimulated by increase in 2-AG [176, 177], as inhibition of COXs prevented platelet aggregation in the presence of 2-AG [175]. Further, platelet-dependent disease progression were not mediated via CB1R or CB2R, but through MAGL [176, 177]. On contrary, a recent systematic review reported neuroprotective effects of cannabis from a variety of methodologies to use of cannabinoids [157]. Since cannabinoids have shown excellent tolerability and beneficial effects in ischemic stroke, they may be capable candidates for therapeutic intervention in future. However, a cautious approach and model are needed as there is scarcity of clinical trials related to cannabinoids and stroke. The model of centralized stroke care as successfully run by the Czech Republic [178] may be a preferable model to adopt in this case. This model system meets the criteria for predictive, preventive, and personalized medicine (PPPM) and will ensure ideal prevention, diagnosis, and treatment of possible complications and prediction of outcomes with cannabinoid therapy [178].
Huntington’s disease: phytocannabinoids attenuate the symptoms of HD
Huntington disease (HD) is an autosomal dominant disorder, characterized by debilitating changes of mood, cognition, and movement control. It stems from an expansion of the CAG trinucleotide repeat found in chromosome 4, which leads to a decrease in GABA and acetylcholine-producing neurons of the basal ganglia [179]. Subsequent atrophy of the caudate nucleus and increase in dopamine production results in the characteristic findings described above. As there currently exists no cure for this disease, current investigations are attempting to more fully understand the disease process and invent potential therapeutic targets.
Recent studies have found that both CB1R and CB2R play vital roles in the progression of this disease [180–188]. Interestingly, the loss of CB1R from the GABAergic neurons is found to be an early sign of HD as well as a significant degeneration of receptors in globus pallidus externa. In contrast, CB2Rs are actually upregulated in postmortem HD basal ganglia [189]. Endocannabinoid levels of AEA and 2-AG were decreased in the striatum of patients with HD and correlate with disease burden, measured via trinucleotide repeats [190]. A study by Sapp et al. reported loss of CB1R early in the disease with an increase in CB2R that might be a protective mechanism in order to reduce pro-inflammatory cascade. However, this protective mechanism is not substantial enough to prevent progression of neuronal death [191]. Previously, Sativex, which is a combination of botanical extracts enriched with THC and CBD, attenuated oxidative stress and inflammation, and protected striatal neurons in a model of striatal injury indicative of HD [192]. Cannabigerol (CBG), a non-psychoactive phytocannabinoid, improved motor deficits and protected striatal neurons in both 3-nitropropionate (3-NP) intoxicated and R6/2 transgenic mice which replicate many features of HD [193]. Particularly, expressions of HD-associated genes, such as Huntington-associated protein 1, Sin3a, Rcor1, symplekin, and GABA-A, were normalized by CBG treatment, while CBG improved the gene expressions of BDNF, IGF-1, and PPARY in R6/2 mice [193]. Another CBG derivative, VCE-003.2, enhanced neuronal progenitor cell survival, improved motor deficits, and inhibited inflammation probably through PPARY in a mouse model of HD [194]. In addition, a recent study with cannabinoids in HD patients showed improvement in motor symptoms, mainly dystonia with less irritability, apathy, and hypersalivation in some cases [195]. Overall, the emerging scenario of cannabinoid-based therapies in HD and other neurodegenerative disorders suggests their pharmacological efficacy in attenuating disease progression and related symptoms and warrants for more experimental and clinical efforts.
Amyotrophic lateral sclerosis: cannabinoids delay the progression of disease
Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease) is a fatal motor neuron disease, disabling common activities, e.g., chew, speak, and walk. ALS causes the loss of voluntary muscle movement and thus causes gradual weakening, twitching, and wasting away. Other clinical symptoms are weakness, spasticity, cachexia, dysarthria, drooling, and pain secondary to immobility [54, 196–198]. ALS can be categorized into two types—sporadic (90%) and familiar (10%). Genetically, ALS is associated with mutations in the superoxide dismutase-1 gene (SOD-1), TAR-DNA binding protein-43 (TDP-43), fused in sarcoma (FUS) [199], and in non-coding hexanucleotide repeat sequence (GGGGCC) in the chromosome 9 open reading frame 72 (C9orf72) genes [54, 200].
ALS most of the time is difficult to diagnose as it presents similar symptoms to those of Parkinson’s disease, multiple sclerosis, and Huntington’s disease. Timely treatments of ALS may slow the progression of disease and reduce complications and discomfort. The US FDA has approved four medications for ALS—Rilutek (riluzole tablet), Tiglutik (riluzole oral suspension), Nuedexta (a combo of dextromethorphan and quinidine), and Radicava (edaravone). Riluzole, a glutamate antagonist, was able to block voltage-gated sodium channels to inhibit the presynaptic release of glutamate and can only prolong survival by 3–5 months [197, 198, 201]. Its tablet form (Rilutik) was approved in 1995, while much later in September 2018, a liquid form of riluzole (Tiglutik) was approved to avoid difficulty of swallowing tablets in ALS patients. Rilutek has also been approved for treatment for ALS in Canada, Australia, and across Europe. Radicava, the first intravenous treatment specifically for ALS was approved by the FDA in May 2017. Nuedexta was approved to treat pseudobulbar affect (inappropriate laughing or crying) in 2011. The quinidine in Nuedexta inhibits the metabolism of principal compound dextromethorphan in liver and thus increases its availability in circulation [54, 197, 198, 201]. However, with established treatment options, patients get partial benefits, and therefore, medical and research communities are trying to find more efficacious treatment options.
Recent in vivo studies suggest beneficial effect of cannabinoids in ALS. In transgenic hSOD(G93A) mice, which develop symptoms similar to human ALS, Δ9-THC administration either before or after symptoms emerged, improved motor impairment and increased survival [202]. It was argued that THC exerted anti-ALS effect by its anti-glutaminergic and antioxidant properties as THC attenuated oxidative stress in ALS hSOD(G93A) mouse spinal cord primary cultures exposed to the oxidant tert-butyl hydroperoxide (TBH) as assessed by lactate dehydrogenase (LDH) and SOD-1 release. However, this antioxidant effect of THC was independent of CB1R, as CB1R-antagonist SR141716A did not inhibit the antioxidant effect of THC [202]. But, anti-excitotoxic effect of THC was CB1R dependent as protective effect of THC against kainic acid-induced excitotoxicity in ALS hSOD(G93A) mouse spinal cord primary neuronal cultures was blocked with antagonist SR141716A [202]. Moreover, cannabinol (CBN), a non-psychotropic cannabinoid which has residual affinity to CB1R, was able to delay disease onset in ALS hSOD(G93A) mice. Further, commercially available Sativex® (2.7 mg ofΔ9-THC and 2.5 mg of CBD) treatment delayed ALS progression in the early stages of disease in ALS hSOD(G93A) transgenic mice [203]. However, the molecular mechanisms remain undefined [204].
CB1R/CB2R agonist WIN 55,212-2 delayed the disease progression, while deletion of FAAH abolished disease symptoms in 90 days old ALS hSOD(G93A) mice after onset of motor impairment and tremor, but had no effect on survival [205]. On the contrary, CB1R deletion did not affect onset of disease, but increased survival by 13% and extended lifespan by 15 days in ALS hSOD(G93A) mice [205]. CB2R and NAPE-PLD both were also found to be upregulated in the spinal cords of ALS hSOD(G93A) mice paralleling disease progression [203, 206, 207], and CB2R agonist AM-1241 increased survival by 56% and delayed motor deficits in ALS hSOD(G93A) mice after disease onset [207]. Therefore, it may be presumed that the beneficial effects of cannabinoids may be mediated by non-CB1R, such as CB2Rs, and were ascribed to regulation of microglial/macrophage activation, glutamate excitotoxicity, and oxidative stress [205–208].
Cannabinoids were also investigated clinically in ALS. In a single observational study with cannabinoids, only the 10% of ALS patients showed moderate improvement in appetite, pain, depression and salivation [209, 210]. In addition, Cannabis has been reported to subjectively improve spasticity [209]. A randomized, double-blind, and single-center study with 30 participants (Clinicaltrial.gov NCT03690791) on the safety, tolerability and efficacy of cannabis-based medicine extract (Centrist CBD Oil) in slowing the disease progression in ALS or motor neuron disease patients is currently under phase 3 trial. Participants are given 25 mg of CBD delayed-release (DR) capsules containing < 2 mg of THC or placebo. Difference in mean ALS Functional Rating Scale-Revised (ALSFRS-R) total score between groups at end of treatment (Total score: min 0–max 48) will be analyzed as primary outcome measure. Higher score represents better outcome [211]. However, paucity of clinical studies related to efficiency of cannabinoids in ALS remains a major challenge for future research.
Parkinson’s disease: cannabinoids protect dopaminergic system
Parkinson’s disease (PD) is the second most prevalent neurodegenerative disease, characterized by the loss of dopaminergic neurons from substantia nigra pars compacta of basal ganglia. The etiology of PD is not fully defined, but may be caused by gene mutations, protein inclusions, oxidative stress, and sustained inflammation [212]. The symptoms of PD are multi-factorial and classically defined by the triad of cogwheel: muscle rigidity, resting tremor, and bradykinesia in addition to behavioral and psychiatric manifestations, including sleep disturbances, cognitive deficits, anxiety, depression, and psychotic symptoms, occurring in the early stages of disease progression [213–217]. Currently, levodopa (L-DOPA) is the most widely used drug for treatment of PD, but prolonged L-DOPA administration may increase dyskinesia [212]. Thus, safe and efficacious therapies are needed to combat the negative symptoms associated with PD.
Components of the ECS are abundantly expressed in the basal ganglia and interact with glutamatergic, γ-aminobutyric acid-ergic (GABAergic), and dopaminergic neurotransmitter systems, suggesting therapeutic potential in PD [185, 218–228]. Endocannabinoid receptors are particularly vital in PD because both CB1R and D1/D2-like receptors are colocalized in striatal neurons [229]. In PD patients, a fourfold increased expression of CB2R was observed when compared to control samples [230], although gene expression profiling revealed a decrease in CB2R gene expression in the cerebellum and hippocampus of PD patients, as compared with healthy control patients [231]. Similarly, CB2R expression was decreased in putamen, while CB1R remained unchanged [230]. Sierra et al. found both CB1R and CB2R mRNA was localized within pallidothalamic-projecting neurons in both uninjured and MPTP-treated non-human primates, with reduced expression levels noted in dyskinetic subjects [232]; however, other reports showed elevated CB2R expression in striatal microglial cells in experimental models [22, 233] and in astrocytes within the substantia nigra of PD patients [230], suggesting the potential for model-, species-, and/or cell type-specific regulation of CBRs in PD.
Increased AEA levels within the cerebrospinal fluid of PD patients were normalized by L-DOPA treatment [219, 223, 234, 235], suggesting a compensatory protective role for AEA in PD. In line with these findings, increased striatal levels of AEA were observed in 6-hydroxydopamine (6-OHDA)-infused rodents (a preclinical model of PD), correlating with reduced activity of AMT and FAAH, although it is important to note that neither 2-AG levels nor AEA binding to CBRs were altered [228]. Functionally, chronic FAAH inhibition reduced AEA metabolism and prevented both MPTP-induced dopaminergic cell loss and motor impairment [236, 237]. Further studies showed that the increased levels of AEA, secondary to FAAH inhibition, increased dopamine levels in the nucleus accumbens shell and attenuated dyskinesia via CB1R activation in lesioned rats [238, 239]. In a similar manner, chronic inhibition of MAGL increased 2-AG levels, prevented motor impairments, and preserved the nigrostriatal pathway in MPTP-infused mice [240]. Together, these findings point to a possible beneficial role for targeted modulation of the ECS in the context of PD.
A number of preclinical and clinical PD studies demonstrated that CB1R modulates motor symptoms and components of cognitive processing [185, 213, 219, 227, 228, 241–244]. A [18F]MK-9470 PET study in PD patients found significant regional alterations in CB1R that are unrelated to levodopa-induced dyskinesia severity [245]. Low CB1R in mid-superior frontal gyrus and in midcingulate cortex was observed to be associated with poor mind, poor executive functioning, and poor episodic memory, while PD patients with severe visuospatial dysfunction had reduced CB1R in the precuneus, midcingulate, supplementary motor cortex, inferior orbitofrontal gyrus, and thalamus [213]. MPTP-lesioned marmosets displayed increased CB1R in the striatum, an effect normalized by L-DOPA treatment [246]. Pharmacological inhibition of CB1R promoted antiparkinsonian effects in rats with severe, but not lesser, nigral lesions [242], while low-dose rimonabant (0.1 mg/kg), a CB1R antagonist, attenuated dopaminergic neuronal cell death, blocked neuroinflammation, and partially reduced hypokinesia in 6-OHDA lesioned animals, independent of striatal dopaminergic, GABAergic, and glutamatergic neurotransmission [244, 247]. Moreover, the synthetic, non-selective CBR agonists, HU-210 and WIN55,212-2, protected nigrostriatal neurons in MPTP-lesioned rodents via a proposed antioxidant mechanism secondary to CB2R, but not CB1R, activation [248, 249]. Of note, HU-210 maximally reduced 6-OHDA-induced cell death in mouse cerebellar granule neurons when cocultured with glial cells, suggesting astrocytes may mediate the protective effect of cannabinoid in PD [246]. Together, these results indicate that nigrostriatal lesions are associated with changes in the ECS within the basal ganglia [250]. Although the mechanisms whereby CB1R modulating drugs affect PD progression remain only partially resolved, it is interesting to note that SR141716 almost fully protected SH-SY5Y neurons against MPP+ toxicity (an in vitro model of PD), even in the presence of the CB1R selective agonist, ACEA [251].
A number of research studies have investigated the role of natural cannabinoids in the treatment of PD symptoms. THC protected MPP+-treated neuronal cells in vitro and attenuated the loss of dopaminergic neurons in a 6-OHDA-induced neurodegeneration model [246, 252]. Interestingly, the beneficial effects of THC were mimicked by ACEA-induced CB1R activation, but not by the CB2R agonist, HU-308 [253]. Garcia and colleagues showed Δ9-tetrahydrocannabivarin (Δ9-THCV), a phytocannabinoid with antioxidant properties [254] decreased 6-OHDA-evoked motor deficit and diminished the dopaminergic neuron loss in the SNpc in hemiparkinsonian rodents [255]. Similarly, the phytocannabinoid β-caryophyllene attenuated gliosis, oxidative stress, and loss of nigrostriatal dopaminergic neurons in a rotenone-induced PD [256], while VCE-003.2, an aminoquinone derivative of the non-psychotropic phytocannabinoid cannabigerol (CBG), attenuated inflammatory neuronal injury, and improved behavioral outcomes after preclinical PD [257, 258]. CBD, the most widely utilized phytocannabinoid, protected neuronal cells against MPP+ toxicity, restored axonal and synaptic proteins, and attenuated microglial activation [259–261]. Administration of CBD (5 mg/kg) for 5 weeks did not reduce dopaminergic neuronal loss or improve motor deficits in MPTP-infused mice, although daily administration of a lower dose (3 mg/kg), initiated at the time of 6-OHDA injection, preserved striatal dopamine and tyrosine hydroxylase in rats, whereas delayed CBD treatment was ineffective [236, 246]. In line with reports showing a correlation between the antinociceptive effect of exercise and increased CB1R/CB2R expression within the anterior cingulate cortex and periaqueductal gray matter and in a rat model of PD [262], CBD-produced an antinociceptive effect in preclinical PD model while an inverse agonist of CB1R and CB2R prevented this effect [263]. Although the mechanisms underlying the beneficial effects remain undefined, CBD may decrease FAAH activity to facilitate AEA-mediated effects [264].
An open-label pilot study showed that CBD in combination with standard of care minimized psychotic symptoms without affecting cognitive or motor alterations in PD patients [265]. In another randomized double-blind clinical trial with 21 PD patients, CBD (75 and 300 mg daily) improved most quality of life outcomes for 6 weeks with CBD treatment, although motor function was not affected [266]. Similarly, a pilot study with 4 PD patients with REM sleep behavior disorder reported a reduction in incidences of agitation, beating, kicking, and nightmares after treatment with 99.9% purified CBD (75 or 300 mg orally per day) [267]. An open-label observational study in 22 PD patients showed significant improvements in resting tremor, rigidity, and bradykinesia and the non-motor aspects sleep and pain after smoking cannabis (500 mg, unspecified composition) [268]. Further, in a Web-based self-reported assessment (n = 595), 454 identified PD patients, who have consumed cannabis daily and for longer than 12 months, reported lower disability and fatigue, while 47.8% patients reported decline in intake of prescribed medicines since beginning of cannabis consumption [269]. These exciting early-stage clinical results showing a potential benefit of cannabinoids after PD will be further explored in the upcoming phase II, randomized, placebo-controlled, and double-blind enriched enrollment withdrawal study (The NMS-Nab Study) [270]. In this study, 4-week outcomes will be assessed in 38 PD patients following administration of a synthetic cannabinoid, nabilone [270]. Given the safety and early-stage efficacy, continued exploration of cannabis-inspired medicines, including studies aimed to identify and standardize the optimal substance(s), route of administration, doses, time point of analysis, and endpoints, is warranted in PD patients.
Multiple sclerosis: cannabis formulation modulates spasticity
Multiple sclerosis (MS) is an autoimmune chronic inflammatory disease that promotes the loss of myelin and damage axons in the central nervous system (CNS). The etiology of MS is poorly understood. However, it is known that inflammation present in MS promotes myelin loss and neuro-axonal degeneration. These events are responsible for impairing the signal conduction through the neurons resulting in disability [271–273]. The symptoms of MS can include, but are not restricted to, spasticity, ataxia, fatigue, pain, difficulty in speaking, constipation, loss of bladder control, depression, or anxiety [271, 274–276]. Interestingly, MS patients show well-described signs and symptoms which are also associated with Flammer syndrome (FS). These symptoms may work as a directive markers for therapeutic benefits and functional outcomes [277, 278]. MS patients most often show nine FS signs and symptoms, such as cold hands/feet, reduced thirst, dizziness, drug side effects, headaches from tension or medication overuse, weight loss, feeling cold, long sleep-onset time, and skin blotches [277, 279]. Scientific studies suggest a potential role of the ECS in controlling either the symptoms or the evolution of MS [280, 281]. The cannabinoids seem to have the potential to slow down the disease progression by exerting a neuroprotective effect [282]. However, patients with MS can present an impaired ECS with reduced levels of anandamide (AEA), palmitoylethanolamide (PEA), 2-AG, and oleoyl ethanolamide (OEA) in the CSF [283].
The fact that both natural and synthetic cannabinoids can act on the human by exerting immunosuppressive role and acting through the components of the ECS make them great allies in the search for an effective treatment for MS. Indeed, patients with MS reported relief after smoking cannabis or using cannabinoids [284–286]. The Δ9-THC was the first cannabinoid to be studied as a means of relieving spasticity, tremor, and pain in MS [284, 287]. This cannabinoid shows effective results in experimental autoimmune encephalomyelitis (EAE) models of MS [288] and in humans [287]. However, the use of Δ9-THC could be limited by its psychotropic effects which may induce acute psychosis, and impact executive function [289–291]. On the other hand, CBD was seen as a potential safe alternative for alleviating neuroinflammation and neurodegeneration in MS, also with lower toxicity and better psychological outcome (i.e., anxiolytic) in patients compared to Δ9-THC [290, 291]. However, CBD has no significant effect on spasticity, which seems more related to CB1R [281, 288, 292, 293].
Current pharmacological studies on MS have largely focused on a combination of Δ9-THC and CBD extracted from cannabis like Sativex® (nabiximols), a cannabinoid preparation with 1:1 ratio of Δ9-THC and CBD. While Δ9-THC promotes modulation of spasticity and has an anti-inflammatory property, CBD seems to reduce the psychoactive effects of Δ9-THC [294]. According to Zamil Al-Ghezi et al., Sativex® can change the expression of miRNA, downregulating some and upregulating others, inducing cell cycle arrest and apoptosis in activated T cells. This process would be responsible for promoting a neuroprotective and anti-inflammatory role as well as a switch of cytokines from pro-inflammatory to anti-inflammatory [295]. Also, the post-marketing studies revealed no evidence of addiction, but mild-to-moderate dizziness as the most common adverse effect [296]. In addition to Sativex, there are two more licensed cannabinoid preparations to be used in MS treatment in some countries, Marinol® and Cesamet®. The Marinol® has an active ingredient, dronabinol, a synthetic form of Δ9-THC [297]. This synthetic cannabinoid reduced the intensity of central and radiating pain after taking dose of 10 mg/day for 15 weeks [298]. In addition to the pain relief, patients that used dronabinol also reported improvement on sleep but no treatment effect on spasticity was reported [299, 300]. Similar to Marinol®, Cesamet® is a brand name for a synthetic Δ9-THC cannabinoid, called nabilone. Like dronabinol, nabilone has shown significant improvement in pain relief, but no change in spasticity [301]. Besides the side effects reported by patients during the use of cannabinoids in MS treatment, the use of phyto- or synthetic cannabinoids seems to be very helpful in neuroprotection and improvement of life quality [299, 300]. However, long-term benefits and risks of MS therapy is still not completely understood.
The treatment approach for MS has taken a shift from relapse prevention to a more personalized establishment with the choice of the suitable drugs and their sequential application over the time-course of the disease, considering patient preference, clinical findings, and related symptoms such as fatigue, depression, and cognitive impairment. Thus, future trials specially with cannabinoids must assign higher relevance to patient outcomes and should implement predictive markers for individual response to new treatment strategies. Thus in this way, benefit to individual patients may be maximized, and adverse events and risk to study participants may be mitigated in clinical trials [302].
Alzheimer’s disease: cannabinoids improve cognition
Changes within the ECS are strongly linked with the progression of Alzheimer’s disease (AD) [187, 303–312]. Analysis of postmortem AD patient brains revealed increased expression of CB2R, primarily in CNS resident immune cells surrounding β-amyloid plaque deposition, within the hippocampus and entorhinal cortex [313, 314]; however, positron emission tomography (PET) scans using [11C]NE40, a radioligand with low selectivity for CB2R over CB1R, suggested lower CB2R availability in AD patients, with no relationship to amyloid beta (Aβ) plaques [315]. CB2R expression paralleled the development of chronic neuroinflammation during the advanced stages of AD, whereas an initial rise in hippocampal and cortical CB1R expression was followed by reduced expression in the later stages of AD [316–318]. Similarly, PET studies demonstrated lower binding ratios of CB1R, with a more pronounced effect in males, in the parieto-temporal cortex and hippocampus of APP/PS1–21 mice, as compared with age-matched wild-type mice [319]. While no significant correlation was observed between CB1R expression and β-amyloid deposition in AD patients, as compared to age-matched controls [320], amyloid precursor protein (APP), which given rise to β-amyloid, interacts with and inhibits the biological activity of CB1R during presymptomatic stage in transgenic mice predisposed to develop AD [321]. Together, these data support a potential relationship between the expression of CBRs and AD progression.
The endocannabinoids, AEA and 2-AG, are released in response to Aβ-amyloid deposition, although transgenic mice predisposed to develop AD exhibit reduced AEA levels [322]. Although an explanation for these seemingly disparate results is lacking, endogenous levels of AEA are regulated by fatty acid amide hydrolase (FAAH), an enzyme expressed by astrocytes that degrades AEA into arachidonic acid. Indeed, arachidonic acid accumulates around pathogenic plaques, leading to pro-inflammatory responses to perpetuate the pathophysiology of AD [305]. A decrease in FAAH activity was observed in the frontal cortex of AD patients. Similarly, reduced FAAH activity was observed in cerebrocortical synaptosomes from aged rat brain, while elevated activity was noted in cerebrocortical membranes [323]. Of interest, CB2R selective agonist-JWH-133 slightly increased AEA hydrolysis in human controls, but suppressed AEA metabolism in cerebrocortical synaptosomes and membranes isolated from adult or aged rat. In comparison, WIN55,212-2, a mixed CB1/CB2-R agonist, increased AEA hydrolysis in AD patients, but decreased activity in human controls and in aged rat brain preparations [323]. Though FAAH activity is similarly regulated in aged rats synaptic endings and human AD brains, activity may be differentially modulated by CB1/CB2-R agonists [323]. In contrast, inhibition of the 2-AG metabolizing enzyme, monoacylglycerol (MAGL), reduces inflammatory activation and attenuates neuropathology, independently from CB2R, in AD-prone mice [304, 324].
The release of endocannabinoids activates neuronal CB1R, which is abundantly expressed within the hippocampus, basal ganglia and cerebellum—brain regions critical for memory function and cognition, to inhibit glutamate release, reduce intracellular Ca2+ concentrations, and enhance neurotrophin expression and neurogenesis [303, 314]. Endocannabinoids also interact with CB2R expressed on immune cells, including CNS resident macrophages/microglia, to attenuate the production of pro-inflammatory molecules implicated in the progression of AD [303, 314, 325]. Activation of CB2R reduced AD-like pathology, attenuated inflammation, and improved cognition [313, 326], while the non-psychoactive phytocannabinoid, CBD, reduced amyloid-β production, inhibited gliosis, suppressed oxidative stress and inflammation, decreased tau hyperphosphorylation, and chronically reduced both social and cognitive deficits in experimental AD models [260, 308, 327–329]. In contrast, CB2R−/− mice displayed AD-like tau hyperphosphorylation and hippocampus-dependent memory impairment while CB2R activation by JWH133 reduced tau phosphorylation in HEK293 cells [330]. Similarly, transgenic mice predisposed to develop AD that also lack CB2Rs (APP/PS1*CB2−/−) exhibited elevated cortical Aβ deposition and increased the levels of soluble Aβ40, as compared to AD mice with CB2R; however, mortality, tau hyperphosphorylation associated with Aβ plaques, and the beneficial effects of cannabis-based medicines were unaffected in mice lacking CB2R [331]. An independent study reported reduced neuronal loss, decreased plaque levels, increased expression of Aβ-degrading enzymes, less inflammation, and improved behavioral outcomes in APP/PS1*CB2−/− mice [332]. Thus, CB2R may provide endogenous protective mechanism that elicits detrimental outcomes if continuously engaged.
THC, a psychoactive component of cannabis, reversibly disrupts short-term memory and dose-dependently impairs attention and cognition [333–338]; however, when chronically administered at low doses, THC improves neurological function in aged animals and promotes hippocampal neurogenesis while reducing neurodegeneration in animal models of AD [99, 339–343]. A recent open-label pilot study showed THC oil (7.5 mg twice daily) was well tolerated and reduced AD-associated delusions, agitation/aggression, irritability, apathy, and sleep disturbances in 11 AD patients [344]. A separate randomized, double-blinded, and placebo-controlled study with non-psychoactive doses of THC (1.5 mg thrice daily for 3 weeks) did not reduce dementia-related neuropsychiatric symptoms in mild to severely demented patients [345]. While anecdotal evidence and early-stage clinical trials suggest a possible benefit of cannabinoids on AD-associated symptoms and pathology in humans, small sample sizes, short trial duration, and lack of placebo control limit the interpretation of these results. Thus, high-quality clinical studies that assess both safety and efficacy are needed to more definitively determine the translational value of cannabinoids in AD [345–348]. Toward this end, the results from a randomized placebo-controlled study (Clinicaltrial.gov NCT02351882) of daily nabilone (2 mg) administered for 6 weeks was recently completed in 40 AD patients is expected within the next year [349, 350]. A second 3-week, placebo-controlled pilot study (Clinicatrial.gov NCT02792257) investigating the effect of 5–10 mg dronabinol (Marinol®) in 160 AD patients is ongoing and will be completed in late 2020. These important clinical trials will provide critical insight regarding the future of cannabinoids in AD.
Schizophrenia: cannabinoids show anti-psychotic effect
The pathogenesis of schizophrenia, which is defined as hallucinations, delusions, and altered speech for greater than 6 months, is linked with alterations in the ECS [351–359]. Genetic studies showed CB1R [353, 360–364] and CB2R [365] polymorphisms are associated with schizophrenia. In addition, people with low CB2R function exhibited an increased risk for schizophrenia [365]. A particular mechanism of how schizophrenia functions is through increased CB1R density [366–373] and increased anandamide levels in CSF [366, 374, 375], and plasma [358, 376] in schizophrenic patients. Further, CB1R agonists led to schizophrenia-like behaviors [377–381], while CB1R antagonists proved to have antipsychotic properties [382, 383] in animal models. The antipsychotic effects of AEA have been also reported [377]. Additional evidence has reinforced the antipsychotic properties of CBD in both clinical and preclinical models of schizophrenia [377, 384–388]. It should be noted that recreational marijuana usage in adolescents is clinically linked to the development of schizophrenia. Possible reasons for this could be explored further. Personalized medicine in specific settings of psychological disorders is being established as a model of individualized care [389]. An integration of molecular science with cannabinoid therapy in clinical settings will certainly lead to novel therapies and certainly promises to a better predictive, preventive, and personalized medicine (PPPM) in psychiatry. With substantial progress in the methodology, omics analyses and data integration, the future for PPPM in psychiatry is encouraging.
Epilepsy: cannabinoids limit the epileptic seizures
Intensive and continual neuronal activity as well as a healthy balance of excitatory and inhibitory neurotransmission is essential to proper brain function. However, when this balance is disrupted, epileptic seizure occurs. Epileptic seizures and their excessive neuronal activity lead to excitotoxicity causing damage to the CNS.
Throughout multiple animal models and clinical studies, cannabinoids have been shown to exert both anti- and pro-convulsive activities with little current evidence for a mechanism [390]. Although not confirmed by large clinical human studies, CB1R agonists are beneficial in epilepsy. Most studies showing improvement in seizure control were associated with low THC/high CBD products rather than endocannabinoids, but also do not disclose sufficient data about subject randomization, group comparisons, anti-epileptic drug doses, and study design [391]. Although treatment options may be far from conclusive, there is strong evidence that cannabinoid receptors, more specifically CB1R, has a role in the intrinsic protection of neural tissue via suppression of pathologic neuronal excitability. There are literature discrepancies with the exact role of the CB1Rs, however, in some studies, it is suggested that downregulation of CB1Rs, particularly on glutamatergic axon terminals, diminish the neuroprotective properties of the endocannabinoid system leading to excessive neuronal excitability and damage in epileptic patients [392]. Other reported seizure-associated increases in CB1R possibly to protect against hyperexcitability or seizure propagation [393].
Other reports suggested the anti-epileptic effect of inhibitors of endocannabinoid metabolism. For example, inhibition of MAGL by JZL184 reduced seizure in kindling model of temporal lobe epilepsy possibly through CB1R-dependent mechanism [394]. Similarly, MAGL inhibition by potent and selective inhibitor CPD-4645 alleviated the inflammation and neuronal loss in status epilepticus and its effect was similar to effect observed in CB1R-deficient mice [395]. In addition, inhibition of FAAH through URB597 exhibited anti-epileptic effect via increase in AEA and possibly through stimulation of CB1R. The restoration of AEA by inhibiting FAAH or AEA transport led to inactivation of TRPV1 channel and reduced Ca2+ entry into the hippocampal cells and thus showed anti-epileptic effect [396]. URB597 further prevented seizure-induced alterations in both STP and LTP and was devoid of any deleterious effects as CB1R agonist, WIN55,212-2, showed in naïve animal [397]. These evidences advocate that boosting the eCB tone rather than CB1 activation might represent a potential strategy for the development of anti-epileptic drugs for treatment of both seizures and comorbid memory impairments associated with epilepsy. However, with a lack of widespread preclinical and clinical studies, it is apparent that the endocannabinoid system’s involvement in epilepsy is an area of need for future research.
Pain: cannabis extract relieves disease-associated pain
Pain is a complicated and multifaceted concept in medicine, which makes it especially difficult to understand and target therapeutically. Pain is thought to be a combination of a subjective experience in psychophysics, an objective sensory neurophysiology, as well as an emotional reaction to distressing stimuli [398]. Just as there are various modalities of pain modulation, the endocannabinoid system has shown a particular link to a variety of pain pathways [399–403].
It has been found that CB2R agonists are analgesic in chronic pain models [404] and help with peripheral inflammation [405]. One possible mechanism by which this is possible is that CB2R agonists allow beta-endorphin release from keratinocytes [406]. Furthermore, PEA, an analgesic in inflammatory pain, is targeted by the endocannabinoid system allowing for a functional improvement in pain modulation [407]. Cannabinoids allow pain modulation through spinal, supraspinal, and peripheral mechanisms [408–410].
In addition to somatic pain, neuropathic pain also demonstrates interplay with CB2Rs. Neuropathic pain can be due to traumatic injury as well as metabolic changes and chemotherapy. CB2R agonists were found to suppress neuropathic nociception using a nerve ligation model of L5 and L6 spinal nerves in rats [406]. Chemotherapy-induced neuropathic pain was also shown to be significantly suppressed via CB2Rs, even in the absence of peripheral nerve degeneration [411]. Finally, two CB2R-selective agonists, L768242 (GW405833) and AM1241, have shown to suppress capsaicin-evoked release of calcitonin gene-related peptide in murine models, suggesting a neuronal mechanism of analgesia [412].
Among the increasing incidences of opioid abuse, natural cannabinoids have emerged as strong candidate for pain management [413]. Clinical studies with oral cannabis extract (OCE) on MS patients were found effective in spasticity and related pain [414, 415]. Nabiximols mouth spray (Sativex®), which is a mixture of CBD and THC, is currently approved for treating MS-associated spasticity and neuropathic pain in the UK, Canada, and several European countries [416–418]. However, it was suggested that cannabis extract, when having low THC content (< 4%), was safe and produced greater therapeutic benefits [415, 419]. Therefore, a complete understanding of action of cannabis and its components is desired as they are able to alter the brain normal functioning even consumed in small quantities [420].
Brain tumor: cannabinoids reduce tumor growth and promote chemotherapy response
Brain tumor is one of the deadliest type of cancer with incidence of 10.85% per 100,000 people annually worldwide [421]. There are over several clinical subtypes of brain cancers based on the originating cells, but glioblastoma multiforme (GBM) has the most aggressive and constitutes 60% of all brain tumors of adults [422]. The lethality of glioblastoma can be gauged from the fact that more than two third of patients with glioblastoma die within 2 years [423]. The brain cancer affects all ages and is diagnosed in all anatomical regions of CNS. Most common pathologies, especially in children, include astrocytoma, medulloblastoma, germ-cell tumors, brainstem-gliomas, and epyndemomas [424]. Therefore, developing new natural and synthetic anti-glioma drugs has become main focus for FDA and global research [425].
The therapeutic use of cannabinoids in neurological disorders like multiple sclerosis and epilepsy has generated interest in its efficacy for treating diseases such as brain tumor, since the elucidation of psychotropic constituent of Cannabis sativa opened way to identification of sites of action of THC, CB1R, and CB2R and subsequently endogenous agonists to these receptors [426–428]. Although, the anti-neoplastic activity of THC and its analogs was first reported in the early 1970 [429], recent studies reflect the possibility that ECB system could be targeted to retard or block cancer growth [426]. The endocannabinoids AEA and 2-AG are ubiquitous among both vertebrate and invertebrate tissues and have modulatory role in cell proliferation, differentiation, and apoptosis, suggesting their roles in control of cell survival, transformation, and death [426, 430]. Further, the endocannabinoid signaling pathway that involves CB1R and CB2R is implicated in brain development and function physiologically. CB2R stimulation via sustained synthesis of ceramide and activation of ERK triggers nuclear events that lead to programmed glioma cells death [426]. Non-psychoactive CBD administration to the human glioma cell lines resulted in dramatic drop of glioma cell viability in a concentration-dependent manner evident within 24 h after administration. The reduction of viability was correlated to induction of apoptosis which was not reverted by cannabinoid antagonists. The CBD administered to nude mice at 0.5 mg/mouse inhibited the growth of subcutaneously implanted human glioma cells significantly, suggesting possible application of CBD as anti-neoplastic agent [431]. Also, administration of CBD in glioma stem cells displayed an increase in ROS and thus inhibition of cell survival and a significant increase in survival of glioma stem cells (GSC)-bearing mice [432].
The endocannabinoid system functions as tumor suppressive through variety of cytostatic, apoptotic, anti-angiogenic, and anti-metastatic mechanism [433]. The generation of malignant cells involve imbalance of endogenous ligands and receptors of cannabinoid system. THC has shown to downregulate the expression of E2F1 and cyclin A which leads to G1 arrest in GBM cells [434]. THC has also shown to induce apoptosis by releasing cathepsins leading to organelle permeabilization and apoptosis [435]. One of the first studies that showed the therapeutic benefits of cannabinoids in brain tumor demonstrated its efficacy by reduction in size of tumors in rats [436]. Additionally, oral administration of Sativex-mimic extract (THC/CBD in 1:1 ratio) in conjunction with temozolomide exhibited strong antitumor effect in subcutaneous and intracranial glioma cell-derived tumor xenograft [437].
The expression of CB2R have been shown to be upregulated in glioblastoma patients [438]. The grade of tumor varies from G1 (well-differentiated, least aggressive, low grade) to G4 (undifferentiated, most aggressive, high grade). The expression of CB2R was found to be twofold higher in tumor of high grade compared to low grade [439]. A highly selective CB2R-agonist COR167 restricted the growth of glioblastoma and anaplastic astrocytoma via reduction of TGF-β1 and TGF-β2 [440]. CB2R expression analysis can assist in the efforts to identify biomarkers that can identify patients that can respond to therapies. Tumor angiogenesis is an important component for growth and expansion of malignant cells as it provides new blood vessels for supply of oxygen and nutrition. Cannabinoids have shown to disrupt tumor angiogenesis by suppressing pro-angiogenic factors like VEGF and Ang2 and inhibition of endothelial cell migration and proliferation [441].
The clinical management of brain tumors is difficult as these tumors have low response rates to chemotherapeutic agents. A growing number of data from in vivo and in vitro studies with cannabinoids elucidated the beneficial role of cannabinoids as tumor-suppressing agent. The cannabinoids increase the chemo-sensitivity of GBM cells by acting as agonist for cationic receptor TRPV2 [442]. The transient loss of TRPV2 expression using siRNA showed downregulation of Fas and procaspase-8 and increased proliferation in human glioma cell lines [443]. Synthetic THC-mimics (dronabinol and nabilone), CBD, and a refined cannabis extract, nabiximols (THC/CBD = 1.08:1.00) have demonstrated calming effects against cancer-associated nausea, vomiting, pain, anxiety, anorexia, weight loss, or sleep disturbance [444]. Recently, a prominent increase in use of cannabinoids in conjunction with immunotherapy have been observed [445, 446]. In an observational study in patients treated with nivolumab, cannabis use during immunotherapy treatment decreased response rate [445]. In another case study, daily dose of CBD (400 mg/ day) alongside tumor resection followed by radio-chemotherapy increased the survival of patients with a mean survival time of 22.3 months [446].
In an interesting phase 1 interventional study with three patients with epilepsy with associated tumors enrolled in The University of Alabama at Birmingham CBD Program (Clinicaltrial.gov: NCT02700412 and NCT02695537), CBD (Epidiolex; Greenwich Biosciences) reduced tumor-associated seizure frequency and severity [447]. The phase II clinical trial of THC and CBD underway for its benefit in glioblastoma patients (ClinicalTrials.gov: NCT03529448). The preliminary results have showed better 1-year survival (83%) of treatment group compared to placebo control (53%) [448]. Cannabinoids executed their therapeutic effects by reducing tumor growth, by reducing angiogenesis, and by promoting tumor cell death. Moreover, cannabinoids inhibited the stem cell-like properties and invasiveness of GBM tumors [449]. Taken together, the importance of pharmacological effectiveness and the molecular mechanisms of the cannabinoid system in tumor pathophysiology cannot be ignored. In last two decades, there has been rapid development in field of personalized medicine due to development of technologies like next-generation sequencing (NGS) which can assist in rapid screening of clinically responsive patients [450]. Along with recent advances in multi-omics genomics, transcriptomics and proteomics screening of cancer patients which can be responsive to patient stratification and accurate, quick, and personalized treatments [451], the endocannabinoid system could be a potential pharmacologically target for novel anti-cancer drugs.
Therapeutic strategies and translational approaches
The ECS has emerged as a new therapeutic target in a variety of neurological and neuroinflammatory disorders [452]. The cannabinoids possess broad-spectrum activity at multiple cellular and molecular mechanisms that involve not only the ECS itself but also the immune system [309]. Cannabinoids can prevent excitotoxicity, oxidative stress, and neuroinflammation and can augment neuronal metabolism through either specific cannabinoid receptor-mediated signaling pathways or via direct interactions with transcription factors.
Current treatments involve the use of CB1R/CB2R activators or agonists. The current clinical CB1R/CB2R activators available are Cesamet (nabilone), Marinol (dronabinol; Δ9-tetrahydrocannabinol [Δ9-THC]), and Sativex (Δ9-THC with cannabidiol) [63]. The only selective agonist clinically approved by the FDA is a CB1R-selective agonist Resunab™; however, this drug is only designated for a fast-track development program in a phase II human clinical trial for scleroderma and is not openly clinically available [63]. Most of the agonists are synthetic exocannabinoids, typically derived some way from THC. A study showed lower post-TBI mortality in the THC(+) patients (2.4%) as compared with the THC(−) group and thus suggested an association of positive THC screen with decreased mortality in adult patients sustaining TBI [152]. THC, in itself has gained much media attention with few understanding its actual role in treatment or physiological effect. Similar to the endocannabinoid AEA, THC is a low effector agonist [42, 43, 453, 454]. THC or THC synthetics are also not equivalent to natural endocannabinoids. THC has multiple effects at once in a very imprecise and irregularly responsive manner compared to natural endocannabinoids that function with “right place, right time” manner that is precise in effect location and tightly controlled. Furthermore, endocannabinoids do not have the psychoactive effects of exocannabinoids or synthetics targeting CB1Rs and CB2Rs. Adding to the complications of THC use, the exocannabinoid was shown at times of low endocannabinoid receptor density or limiting postreceptor effectors to antagonize CB1Rs usually controlled by 2-AG showing potential adverse receptor response and imprecision in receptor targeting [455–458]. These adverse effects become a primary challenge to overcome in the future of endocannabinoid system involved treatments. The lack of specificity could also become dangerous as synthetic highly efficacious street cannabinoid agonists such as Spice can cause much greater psychoactive side effects [459]. However, some studies have shown promising results in limiting withdrawal symptom effects. High doses of a CB1R antagonist rimonabant attenuated “high” with no withdrawal effects in humans taking a supervised moderate dose of THC [460]. However, in rodent models, long-term high doses of THC elicited withdrawal symptoms, thus showing that the mechanism is much more complicated than just THC “highjacking” CB1Rs for physiological effect [461]. Current research has sought to target CB2Rs more heavily than CB1Rs due to their lower risk of adverse psychoactive effects. However, many complications regarding the use and study of CBR2s make the future challenging. There are currently a lack of highly selective CB2R antibodies [462] to study as well as no availability of CB2R floxed or Cre mouse to use. Under some conditions, CB1Rs and CB2Rs actually create a heteromer making it difficult to isolate each receptor’s function from one another in testing [463]. Furthering the isolation challenges, there has been trouble inducing only CB2Rs without CB1R effect as well as trouble selecting only for CNS CB2Rs without affecting PNS CB2Rs where they are most prevalent [32].
Phytocannabinoids: a viable treatment option?
The potential medicinal properties of marijuana have been the subject of intense scientific debate for decades. The approvals of nabiximols and purified CBD extract for the treatment of spasticity and pediatric epilepsy have drawn global medical attention to cannabinoids [464]. Thirty-two states and Washington, DC in the USA allow the use of marijuana to treat certain medical conditions. However, medical marijuana laws differ widely from state to state [465]. Cannabinoids may differ in composition and biological effects, depending on marijuana preparations. Medical cannabinoids, particularly non-psychotropic CBD, have demonstrated considerable promise in ameliorating chronic pain and various diseases ranging from neurological and movement disorders to cancer [466–468].
Clinical studies on patients with MS revealed efficacy of oral cannabis extract (OCE) in spasticity and related pain [414, 415]. In addition, nabiximols, a cannabis extract preparation, reduced bladder void in urinary infection [414]. Further, the studies reinforced the benefits of cannabis in neuropathic pain and suggested an improved safety profile as an extract without undesirable neurological effects when containing low THC concentrations (< 4%) produced therapeutic benefits without undesirable neurological effects [415, 419]. Nabiximols mouth spray (Sativex®) contains CBD and THC that are currently available in the UK, Canada, and several European countries for treating the spasticity and neuropathic pain in MS patients [416–418]. The US Food and Drug Administration (FDA) approved a CBD-based liquid medication called Epidiolex® for the treatment of two forms of severe childhood epilepsy [417, 418], as well as THC-based pills, dronabinol (Marinol®) and nabilone (Cesamet®), for the treatment of nausea in cancer patients undergoing chemotherapy and to stimulate appetite in AIDS patients with marked weight and muscle loss [417, 418]. In fact, with the rising concern over opioid epidemic, cannabis and cannabinoids are emerging as strong alternatives for pain relief [413]. However, a complete understanding of action of cannabis should be desired as THC-mediated relief in chronic radicular neuropathic pain is associated with altered brain connectivity among anterior cingulate and dorsolateral prefrontal cortex with somatosensory cortex [420].
The risks and benefits of cannabinoid should be weighed carefully as marijuana, like all drugs, has potential risks. For example, cannabinoid not only increased appetite in cancer patients but also declined the quality of life, which may be due to the side effects of cannabinoid [469]. Further, oral cannabinoids have shown many adverse effects, e.g., dysphoria, dizziness, depression, or hypotension compared with conventional antiemetic therapy [1]. In addition, efficacy of cannabinoids is still unknown in neurologic conditions, e.g., dyskinesia in patients with Parkinson’s disease, non-chorea-related symptoms of Huntington’s disease, Tourette syndrome, cervical dystonia, and epilepsy [1, 414]. Common side effects include dizziness, dry mouth, nausea, disorientation, euphoria, confusion, sedation, and cardiac arrhythmia in people who are already at risk. Regular smoking of marijuana can be addictive and is associated with breathing problems and lung infections [470].
Insufficient literature and varied composition of cannabis products lead to inconclusive evidence of cannabinoid use and their efficacy in many diseases. Further, the prevalence of a wide range of adverse events associated with medical marijuana (ranging from dry mouth to patient death) is a potential question that need to be addressed [415, 471]. As the scientific and medical world advance in the field of medical uses of marijuana, evidences suggest that marijuana may be an effective treatment for chronic pain, neuropathic (nerve) pain, and muscle spasms due to multiple sclerosis or paraplegia. Now as marijuana’s use as a treatment for certain medical indications has taken focus, patients and physicians both have to learn about its potential risks and benefits [472].
Conclusions and future PPPM strategies: innovative approach by predictive diagnostics, targeted prevention, and personalization of medical services
One of the most significant features of medicinal cannabis is its ability to be considered as personalized medicine by allowing individuals to control over their own treatment (e.g., dose, time, and type of cannabis). This aspect of medicinal cannabis is more meaningful in CNS-related diseases. All neurodegenerative diseases need great medical support from early diagnosis and prognostic evaluation to personalized therapeutic regimes and a better prediction of treatment outcomes. Brain imaging along with advanced data acquisition and analysis has become a major important tool to identify disease and proper treatment benefits clinically [473]. However, lack of specific biomarkers to identify persons at risk for neurodegenerative disorders is an avenue for major improvement in the field. The first step would be to invent new preclinical models for neurodegenerative diseases that depict initiation and progression of diseases more accurately. Then identifying key molecular pathways relevant for pathophysiology of neurodegenerative diseases maybe considered a novel and viable perspective for both predictive as well as individualized medicine and targeted therapeutic modality. In light of systemic alteration, because it may seem that the impact of mechanistic approach would be diminished, at least in the short-term, therefore, the multi-omics at DNA and protein (both expression and activity) levels would be highly recommended and useful. An established biomarker panel is considered as a powerful tool for personalized medicine as for an individualized patient profiling and improved multi-level diagnostics, in a predictive, preventive, and prognostic fashion. A major requisite to achieve this is an increased interaction between basic scientists and clinicians with respect to preventive, predictive, and personalized medicines (PPPM) in neurodegenerative diseases [473].
The ECS has been shown to influence a range of CNS diseases as detailed in this review and numerous other systemic pathologies as well. The current literature is only just starting to scratch the surface on how the ECS can be targeted and modulated for therapeutic benefit. The future seeks to further understand CB2Rs due to their highly inducible feature making them a great therapeutic target [32]. The use of selective CB2R agonists shows promising targets to manipulate drug-seeking behavior, reward, dependence, and addiction pathways [28, 29, 474]. A primary target for future research would be to develop more selective CB2R agonists with less CB1R adverse activation. Another strategy would be to develop tissue specific activator/inhibitor of CBRs to limit peripheral side effects [475]. Additional options to be further explored are combination treatment plans in which FAAH modulators are used with agonists to control effect of metabolism and synthesis of natural endocannabinoids while implementing effects of synthetic agonists [32, 33].
Cannabis or cannabis-based compounds are becoming common in treating medical conditions. Since there is a definite lack of conclusive data on efficiency and side effects of cannabinoids in clinical conditions, treatment with cannabis or its products must be proceeded cautiously. Health care professionals serve as the most frequent source of information regarding cannabis risks and benefits. As more and more states have adopted medical cannabis laws, medical professionals must be trained for cannabis effect and health outcomes and must provide awareness about cannabis to concerned patients. Planned and standardized training could ensure that health care professionals are prepared to identify medically appropriate symptoms and conditions for use of cannabis [476].
The endocannabinoids show great promise for future therapeutics; however, a rational approach is necessary to develop specific agonist/antagonist régimes and to avoid unwanted health outcomes. In order to inform policymakers, practitioners and users more clearly, future studies should be performed by following uniform guidelines and reporting of patient outcomes [477]. In addition, better understanding of mechanisms responsible for the pathophysiology of neurodegenerative diseases and involvement of cannabinoid system would establish more certain platform for PPPM effectively [478]. Hence, further studies are needed to identify functional links between neurodegenerative diseases and endocannabinoid system and to translate them according to PPPM-guidelines [478] to provide higher standards of health care to affected patient.
Acknowledgments
The authors thank Colby Zahn for the illustration provided in this review.
Funding information
Financial support for this study was provided by grants from the National Institutes of Neurological Diseases and Stroke (NS065172, NS097825 to KMD and NS110378 to BB/KMD), National Institutes of Child Health and Development (HD094606 to KV), and American Heart Association (GRNT33700286 to KMD).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vamsi Reddy and Dayton Grogan contributed equally to this work.
References
- 1.Badowski ME. A review of oral cannabinoids and medical marijuana for the treatment of chemotherapy-induced nausea and vomiting: a focus on pharmacokinetic variability and pharmacodynamics. Cancer Chemother Pharmacol. 2017;80(3):441–449. doi: 10.1007/s00280-017-3387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rock EM, Parker LA. Cannabinoids as potential treatment for chemotherapy-induced nausea and vomiting. Front Pharmacol. 2016;7:221. doi: 10.3389/fphar.2016.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–480. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feigin VL, Vos T. Global burden of neurological disorders: from global burden of disease estimates to actions. Neuroepidemiology. 2019;52(1–2):1–2. doi: 10.1159/000495197. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Global burden of neurological disorders: estimates and projections. In: Neurological disorders: public health challenges. Geneva, Switzerland: WHO Press. https://www.who.int/mental_health/neurology/chapter_2_neuro_disorders_public_h_challenges.pdf?ua=1. Accessed Jan 22 2020.
- 6.Abey NO. Cannabis sativa (marijuana) alters blood chemistry and the cytoarchitecture of some organs in Sprague Dawley rat models. Food Chem Toxicol. 2018;116(Pt B):292–7. 10.1016/j.fct.2018.04.023. [DOI] [PubMed]
- 7.Atakan Z. Cannabis, a complex plant: different compounds and different effects on individuals. Ther Adv Psychopharmacol. 2012;2(6):241–254. doi: 10.1177/2045125312457586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal H, Awad HH, Ghali JK. Role of cannabis in cardiovascular disorders. J Thoracic Dis. 2017;9(7):2079–2092. doi: 10.21037/jtd.2017.06.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goyal H, Singla U, Gupta U, May E. Role of cannabis in digestive disorders. Eur J Gastroenterol Hepatol. 2017;29(2):135–143. doi: 10.1097/MEG.0000000000000779. [DOI] [PubMed] [Google Scholar]
- 10.Zimmermann K, Walz C, Derckx RT, Kendrick KM, Weber B, Dore B, et al. Emotion regulation deficits in regular marijuana users. Hum Brain Mapp. 2017;38(8):4270–4279. doi: 10.1002/hbm.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu SJ, Reiner D, Shen H, Wu KJ, Liu QR, Wang Y. Time-dependent protection of CB2 receptor agonist in stroke. PLoS One. 2015;10(7):e0132487. doi: 10.1371/journal.pone.0132487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang J, Teng Z, Song Y, Hu M, Chen C. Inhibition of monoacylglycerol lipase prevents chronic traumatic encephalopathy-like neuropathology in a mouse model of repetitive mild closed head injury. J Cereb Blood Flow Metab. 2015;35(3):443–453. doi: 10.1038/jcbfm.2014.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang M, Martin BR, Adler MW, Razdan RK, Ganea D, Tuma RF. Modulation of the balance between cannabinoid CB(1) and CB(2) receptor activation during cerebral ischemic/reperfusion injury. Neuroscience. 2008;152(3):753–760. doi: 10.1016/j.neuroscience.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ilyasov AA, Milligan CE, Pharr EP, Howlett AC. The endocannabinoid system and oligodendrocytes in health and disease. Front Neurosci. 2018;12(733). 10.3389/fnins.2018.00733. [DOI] [PMC free article] [PubMed]
- 15.Braun M, Khan ZT, Khan MB, Kumar M, Ward A, Achyut BR, et al. Selective activation of cannabinoid receptor-2 reduces neuroinflammation after traumatic brain injury via alternative macrophage polarization. Brain Behav Immun. 2017. 10.1016/j.bbi.2017.10.021. [DOI] [PMC free article] [PubMed]
- 16.Zhou J, Noori H, Burkovskiy I, Lafreniere JD, Kelly MEM, Lehmann C. Modulation of the endocannabinoid system following central nervous system injury. Int J Mol Sci. 2019;20(2). 10.3390/ijms20020388. [DOI] [PMC free article] [PubMed]
- 17.Cecilia JH. Role of cannabinoids and endocannabinoids in cerebral ischemia. Curr Pharm Des. 2008;14(23):2347–2361. doi: 10.2174/138161208785740054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zarruk JG, Fernandez-Lopez D, Garcia-Yebenes I, Garcia-Gutierrez MS, Vivancos J, Nombela F, et al. Cannabinoid type 2 receptor activation downregulates stroke-induced classic and alternative brain macrophage/microglial activation concomitant to neuroprotection. Stroke. 2012;43(1):211–219. doi: 10.1161/STROKEAHA.111.631044. [DOI] [PubMed] [Google Scholar]
- 19.Lopez-Rodriguez AB, Acaz-Fonseca E, Viveros MP, Garcia-Segura LM. Changes in cannabinoid receptors, aquaporin 4 and vimentin expression after traumatic brain injury in adolescent male mice. Association with edema and neurological deficit. PLoS One. 2015;10(6):e0128782. doi: 10.1371/journal.pone.0128782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Svizenska IH, Brazda V, Klusakova I, Dubovy P. Bilateral changes of cannabinoid receptor type 2 protein and mRNA in the dorsal root ganglia of a rat neuropathic pain model. J Histochem Cytochem. 2013;61(7):529–547. doi: 10.1369/0022155413491269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Concannon RM, Okine BN, Finn DP, Dowd E. Upregulation of the cannabinoid CB2 receptor in environmental and viral inflammation-driven rat models of Parkinson’s disease. Exp Neurol. 2016;283(Pt A):204–212. doi: 10.1016/j.expneurol.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 22.Concannon RM, Okine BN, Finn DP, Dowd E. Differential upregulation of the cannabinoid CB(2) receptor in neurotoxic and inflammation-driven rat models of Parkinson’s disease. Exp Neurol. 2015;269:133–141. doi: 10.1016/j.expneurol.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Aso E, Ferrer I. CB2 cannabinoid receptor as potential target against Alzheimer’s disease. Front Neurosci. 2016;10:243. doi: 10.3389/fnins.2016.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Gutierrez MS, Perez-Ortiz JM, Gutierrez-Adan A, Manzanares J. Depression-resistant endophenotype in mice overexpressing cannabinoid CB(2) receptors. Br J Pharmacol. 2010;160(7):1773–1784. doi: 10.1111/j.1476-5381.2010.00819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia-Gutierrez MS, Manzanares J. Overexpression of CB2 cannabinoid receptors decreased vulnerability to anxiety and impaired anxiolytic action of alprazolam in mice. J Psychopharmacol. 2011;25(1):111–120. doi: 10.1177/0269881110379507. [DOI] [PubMed] [Google Scholar]
- 26.Ortega-Alvaro A, Aracil-Fernandez A, Garcia-Gutierrez MS, Navarrete F, Manzanares J. Deletion of CB2 cannabinoid receptor induces schizophrenia-related behaviors in mice. Neuropsychopharmacology. 2011;36(7):1489–1504. doi: 10.1038/npp.2011.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agudelo M, Yndart A, Morrison M, Figueroa G, Munoz K, Samikkannu T, et al. Differential expression and functional role of cannabinoid genes in alcohol users. Drug Alcohol Depend. 2013;133(2):789–793. doi: 10.1016/j.drugalcdep.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ortega-Alvaro A, Ternianov A, Aracil-Fernandez A, Navarrete F, Garcia-Gutierrez MS, Manzanares J. Role of cannabinoid CB2 receptor in the reinforcing actions of ethanol. Addict Biol. 2015;20(1):43–55. doi: 10.1111/adb.12076. [DOI] [PubMed] [Google Scholar]
- 29.Navarrete F, Rodriguez-Arias M, Martin-Garcia E, Navarro D, Garcia-Gutierrez MS, Aguilar MA, et al. Role of CB2 cannabinoid receptors in the rewarding, reinforcing, and physical effects of nicotine. Neuropsychopharmacology. 2013;38(12):2515–2524. doi: 10.1038/npp.2013.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buch SJ. Cannabinoid receptor 2 activation: a means to prevent monocyte-endothelium engagement. Am J Pathol. 2013;183(5):1375–1377. doi: 10.1016/j.ajpath.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Ashton CH, Moore PB. Endocannabinoid system dysfunction in mood and related disorders. Acta Psychiatr Scand. 2011;124(4):250–261. doi: 10.1111/j.1600-0447.2011.01687.x. [DOI] [PubMed] [Google Scholar]
- 32.Lu HC, Mackie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79(7):516–525. doi: 10.1016/j.biopsych.2015.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mackie K. Cannabinoid receptors as therapeutic targets. Annu Rev Pharmacol Toxicol. 2006;46:101–122. doi: 10.1146/annurev.pharmtox.46.120604.141254. [DOI] [PubMed] [Google Scholar]
- 34.Pacher P, Batkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58(3):389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu J, Wang L, Harvey-White J, Osei-Hyiaman D, Razdan R, Gong Q, et al. A biosynthetic pathway for anandamide. Proc Natl Acad Sci U S A. 2006;103(36):13345–13350. doi: 10.1073/pnas.0601832103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simon GM, Cravatt BF. Characterization of mice lacking candidate N-acyl ethanolamine biosynthetic enzymes provides evidence for multiple pathways that contribute to endocannabinoid production in vivo. Mol BioSyst. 2010;6(8):1411–1418. doi: 10.1039/c000237b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsuboi K, Ikematsu N, Uyama T, Deutsch DG, Tokumura A, Ueda N. Biosynthetic pathways of bioactive N-acylethanolamines in brain. CNS Neurol Disord Drug Targets. 2013;12(1):7–16. doi: 10.2174/1871527311312010005. [DOI] [PubMed] [Google Scholar]
- 38.Shonesy BC, Winder DG, Patel S, Colbran RJ. The initiation of synaptic 2-AG mobilization requires both an increased supply of diacylglycerol precursor and increased postsynaptic calcium. Neuropharmacology. 2015;91:57–62. doi: 10.1016/j.neuropharm.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jung KM, Astarita G, Zhu C, Wallace M, Mackie K, Piomelli D. A key role for diacylglycerol lipase-alpha in metabotropic glutamate receptor-dependent endocannabinoid mobilization. Mol Pharmacol. 2007;72(3):612–621. doi: 10.1124/mol.107.037796. [DOI] [PubMed] [Google Scholar]
- 40.Murataeva N, Straiker A, Mackie K. Parsing the players: 2-arachidonoylglycerol synthesis and degradation in the CNS. Br J Pharmacol. 2014;171(6):1379–1391. doi: 10.1111/bph.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luk T, Jin W, Zvonok A, Lu D, Lin XZ, Chavkin C, et al. Identification of a potent and highly efficacious, yet slowly desensitizing CB1 cannabinoid receptor agonist. Br J Pharmacol. 2004;142(3):495–500. doi: 10.1038/sj.bjp.0705792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gonsiorek W, Lunn C, Fan X, Narula S, Lundell D, Hipkin RW. Endocannabinoid 2-arachidonyl glycerol is a full agonist through human type 2 cannabinoid receptor: antagonism by anandamide. Mol Pharmacol. 2000;57(5):1045–1050. [PubMed] [Google Scholar]
- 43.Breivogel CS, Childers SR. Cannabinoid agonist signal transduction in rat brain: comparison of cannabinoid agonists in receptor binding, G-protein activation, and adenylyl cyclase inhibition. J Pharmacol Exp Ther. 2000;295(1):328–336. [PubMed] [Google Scholar]
- 44.Neu A, Foldy C, Soltesz I. Postsynaptic origin of CB1-dependent tonic inhibition of GABA release at cholecystokinin-positive basket cell to pyramidal cell synapses in the CA1 region of the rat hippocampus. J Physiol. 2007;578(Pt 1):233–247. doi: 10.1113/jphysiol.2006.115691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hentges ST, Low MJ, Williams JT. Differential regulation of synaptic inputs by constitutively released endocannabinoids and exogenous cannabinoids. J Neurosci. 2005;25(42):9746–9751. doi: 10.1523/JNEUROSCI.2769-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hashimotodani Y, Ohno-Shosaku T, Tsubokawa H, Ogata H, Emoto K, Maejima T, et al. Phospholipase Cbeta serves as a coincidence detector through its Ca2+ dependency for triggering retrograde endocannabinoid signal. Neuron. 2005;45(2):257–268. doi: 10.1016/j.neuron.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Bender VA, Bender KJ, Brasier DJ, Feldman DE. Two coincidence detectors for spike timing-dependent plasticity in somatosensory cortex. J Neurosci. 2006;26(16):4166–4177. doi: 10.1523/JNEUROSCI.0176-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cravatt BF, Giang DK, Mayfield SP, Boger DL, Lerner RA, Gilula NB. Molecular characterization of an enzyme that degrades neuromodulatory fatty-acid amides. Nature. 1996;384(6604):83–87. doi: 10.1038/384083a0. [DOI] [PubMed] [Google Scholar]
- 49.Woodward DF, Liang Y, Krauss AH. Prostamides (prostaglandin-ethanolamides) and their pharmacology. Br J Pharmacol. 2008;153(3):410–419. doi: 10.1038/sj.bjp.0707434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hermanson DJ, Hartley ND, Gamble-George J, Brown N, Shonesy BC, Kingsley PJ, et al. Substrate-selective COX-2 inhibition decreases anxiety via endocannabinoid activation. Nat Neurosci. 2013;16(9):1291–1298. doi: 10.1038/nn.3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hermanson DJ, Gamble-George JC, Marnett LJ, Patel S. Substrate-selective COX-2 inhibition as a novel strategy for therapeutic endocannabinoid augmentation. Trends Pharmacol Sci. 2014;35(7):358–367. doi: 10.1016/j.tips.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blankman JL, Simon GM, Cravatt BF. A comprehensive profile of brain enzymes that hydrolyze the endocannabinoid 2-arachidonoylglycerol. Chem Biol. 2007;14(12):1347–1356. doi: 10.1016/j.chembiol.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim J, Alger BE. Inhibition of cyclooxygenase-2 potentiates retrograde endocannabinoid effects in hippocampus. Nat Neurosci. 2004;7(7):697–698. doi: 10.1038/nn1262. [DOI] [PubMed] [Google Scholar]
- 54.Nomura DK, Morrison BE, Blankman JL, Long JZ, Kinsey SG, Marcondes MC, et al. Endocannabinoid hydrolysis generates brain prostaglandins that promote neuroinflammation. Science. 2011;334(6057):809–813. doi: 10.1126/science.1209200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Howlett AC, Abood ME. CB1 and CB2 receptor pharmacology. Adv Pharmacol (San Diego, Calif) 2017;80:169–206. doi: 10.1016/bs.apha.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346(6284):561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- 57.Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365(6441):61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 58.Mackie K, Lai Y, Westenbroek R, Mitchell R. Cannabinoids activate an inwardly rectifying potassium conductance and inhibit Q-type calcium currents in AtT20 cells transfected with rat brain cannabinoid receptor. J Neurosci. 1995;15(10):6552–6561. doi: 10.1523/JNEUROSCI.15-10-06552.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Twitchell W, Brown S, Mackie K. Cannabinoids inhibit N- and P/Q-type calcium channels in cultured rat hippocampal neurons. J Neurophysiol. 1997;78(1):43–50. doi: 10.1152/jn.1997.78.1.43. [DOI] [PubMed] [Google Scholar]
- 60.Onaivi ES, Ishiguro H, Gu S, Liu QR. CNS effects of CB2 cannabinoid receptors: beyond neuro-immuno-cannabinoid activity. J Psychopharmacol. 2012;26(1):92–103. doi: 10.1177/0269881111400652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Navarrete F, Perez-Ortiz JM, Manzanares J. Cannabinoid CB(2) receptor-mediated regulation of impulsive-like behaviour in DBA/2 mice. Br J Pharmacol. 2012;165(1):260–273. doi: 10.1111/j.1476-5381.2011.01542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Garcia-Gutierrez MS, Garcia-Bueno B, Zoppi S, Leza JC, Manzanares J. Chronic blockade of cannabinoid CB2 receptors induces anxiolytic-like actions associated with alterations in GABA(A) receptors. Br J Pharmacol. 2012;165(4):951–964. doi: 10.1111/j.1476-5381.2011.01625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen DJ, Gao M, Gao FF, Su QX, Wu J. Brain cannabinoid receptor 2: expression, function and modulation. Acta Pharmacol Sin. 2017;38(3):312–316. doi: 10.1038/aps.2016.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stempel AV, Stumpf A, Zhang HY, Ozdogan T, Pannasch U, Theis AK, et al. Cannabinoid type 2 receptors mediate a cell type-specific plasticity in the hippocampus. Neuron. 2016;90(4):795–809. doi: 10.1016/j.neuron.2016.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li Y, Kim J. Neuronal expression of CB2 cannabinoid receptor mRNAs in the mouse hippocampus. Neuroscience. 2015;311:253–267. doi: 10.1016/j.neuroscience.2015.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Viscomi MT, Oddi S, Latini L, Pasquariello N, Florenzano F, Bernardi G, et al. Selective CB2 receptor agonism protects central neurons from remote axotomy-induced apoptosis through the PI3K/Akt pathway. J Neurosci. 2009;29(14):4564–4570. doi: 10.1523/JNEUROSCI.0786-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bradshaw HB, Walker JM. The expanding field of cannabimimetic and related lipid mediators. Br J Pharmacol. 2005;144(4):459–465. doi: 10.1038/sj.bjp.0706093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bouaboula M, Rinaldi M, Carayon P, Carillon C, Delpech B, Shire D, et al. Cannabinoid-receptor expression in human leukocytes. Eur J Biochem. 1993;214(1):173–180. doi: 10.1111/j.1432-1033.1993.tb17910.x. [DOI] [PubMed] [Google Scholar]
- 69.Walter L, Franklin A, Witting A, Wade C, Xie Y, Kunos G, et al. Nonpsychotropic cannabinoid receptors regulate microglial cell migration. J Neurosci. 2003;23(4):1398–1405. doi: 10.1523/JNEUROSCI.23-04-01398.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ramirez SH, Hasko J, Skuba A, Fan S, Dykstra H, McCormick R, et al. Activation of cannabinoid receptor 2 attenuates leukocyte-endothelial cell interactions and blood-brain barrier dysfunction under inflammatory conditions. J Neurosci. 2012;32(12):4004–4016. doi: 10.1523/JNEUROSCI.4628-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang HY, Gao M, Liu QR, Bi GH, Li X, Yang HJ, et al. Cannabinoid CB2 receptors modulate midbrain dopamine neuronal activity and dopamine-related behavior in mice. Proc Natl Acad Sci U S A. 2014;111(46):E5007–E5015. doi: 10.1073/pnas.1413210111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sorgard M, Di Marzo V, et al. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature. 1999;400(6743):452–457. doi: 10.1038/22761. [DOI] [PubMed] [Google Scholar]
- 73.Bouaboula M, Hilairet S, Marchand J, Fajas L, Le Fur G, Casellas P. Anandamide induced PPARgamma transcriptional activation and 3T3-L1 preadipocyte differentiation. Eur J Pharmacol. 2005;517(3):174–181. doi: 10.1016/j.ejphar.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 74.Taylor SJ, Chae HZ, Rhee SG, Exton JH. Activation of the beta 1 isozyme of phospholipase C by alpha subunits of the Gq class of G proteins. Nature. 1991;350(6318):516–518. doi: 10.1038/350516a0. [DOI] [PubMed] [Google Scholar]
- 75.Kano M, Ohno-Shosaku T, Hashimotodani Y, Uchigashima M, Watanabe M. Endocannabinoid-mediated control of synaptic transmission. Physiol Rev. 2009;89(1):309–380. doi: 10.1152/physrev.00019.2008. [DOI] [PubMed] [Google Scholar]
- 76.Robbe D, Kopf M, Remaury A, Bockaert J, Manzoni OJ. Endogenous cannabinoids mediate long-term synaptic depression in the nucleus accumbens. Proc Natl Acad Sci U S A. 2002;99(12):8384–8388. doi: 10.1073/pnas.122149199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gerdeman GL, Ronesi J, Lovinger DM. Postsynaptic endocannabinoid release is critical to long-term depression in the striatum. Nat Neurosci. 2002;5(5):446–451. doi: 10.1038/nn832. [DOI] [PubMed] [Google Scholar]
- 78.Tsetsenis T, Younts TJ, Chiu CQ, Kaeser PS, Castillo PE, Sudhof TC. Rab3B protein is required for long-term depression of hippocampal inhibitory synapses and for normal reversal learning. Proc Natl Acad Sci U S A. 2011;108(34):14300–14305. doi: 10.1073/pnas.1112237108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jiang B, Huang S, de Pasquale R, Millman D, Song L, Lee HK, et al. The maturation of GABAergic transmission in visual cortex requires endocannabinoid-mediated LTD of inhibitory inputs during a critical period. Neuron. 2010;66(2):248–259. doi: 10.1016/j.neuron.2010.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chevaleyre V, Heifets BD, Kaeser PS, Sudhof TC, Castillo PE. Endocannabinoid-mediated long-term plasticity requires cAMP/PKA signaling and RIM1alpha. Neuron. 2007;54(5):801–812. doi: 10.1016/j.neuron.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chevaleyre V, Castillo PE. Endocannabinoid-mediated metaplasticity in the hippocampus. Neuron. 2004;43(6):871–881. doi: 10.1016/j.neuron.2004.08.036. [DOI] [PubMed] [Google Scholar]
- 82.Marinelli S, Pacioni S, Cannich A, Marsicano G, Bacci A. Self-modulation of neocortical pyramidal neurons by endocannabinoids. Nat Neurosci. 2009;12(12):1488–1490. doi: 10.1038/nn.2430. [DOI] [PubMed] [Google Scholar]
- 83.Marinelli S, Pacioni S, Bisogno T, Di Marzo V, Prince DA, Huguenard JR, et al. The endocannabinoid 2-arachidonoylglycerol is responsible for the slow self-inhibition in neocortical interneurons. J Neurosci. 2008;28(50):13532–13541. doi: 10.1523/JNEUROSCI.0847-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bacci A, Huguenard JR, Prince DA. Long-lasting self-inhibition of neocortical interneurons mediated by endocannabinoids. Nature. 2004;431(7006):312–316. doi: 10.1038/nature02913. [DOI] [PubMed] [Google Scholar]
- 85.Dubreucq S, Durand A, Matias I, Benard G, Richard E, Soria-Gomez E, et al. Ventral tegmental area cannabinoid type-1 receptors control voluntary exercise performance. Biol Psychiatry. 2013;73(9):895–903. doi: 10.1016/j.biopsych.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 86.Albayram O, Passlick S, Bilkei-Gorzo A, Zimmer A, Steinhauser C. Physiological impact of CB1 receptor expression by hippocampal GABAergic interneurons. Pflugers Arch. 2016;468(4):727–737. doi: 10.1007/s00424-015-1782-5. [DOI] [PubMed] [Google Scholar]
- 87.Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, Mackie K, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310(5746):329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 88.Hillard CJ, Beatka M, Sarvaideo J. Endocannabinoid signaling and the hypothalamic-pituitary-adrenal axis. Compr Physiol. 2016;7(1):1–15. doi: 10.1002/cphy.c160005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hedrich J, Angamo EA, Conrad A, Lutz B, Luhmann HJ. Cell type specific impact of cannabinoid receptor signaling in somatosensory barrel map formation in mice. J Comp Neurol. 2019. 10.1002/cne.24733. [DOI] [PubMed]
- 90.Friend LN, Williamson RC, Merrill CB, Newton ST, Christensen MT, Petersen J, et al. Hippocampal stratum oriens somatostatin-positive cells undergo CB1-dependent long-term potentiation and express endocannabinoid biosynthetic enzymes. Molecules. 2019;24(7). 10.3390/molecules24071306. [DOI] [PMC free article] [PubMed]
- 91.Fernandez-Espejo E, Nunez-Dominguez L. Endocannabinoid-mediated synaptic plasticity and substance use disorders. Neurologia. 2019. 10.1016/j.nrl.2018.12.004. [DOI] [PubMed]
- 92.Dow-Edwards D, Silva L. Endocannabinoids in brain plasticity: cortical maturation, HPA axis function and behavior. Brain Res. 2017;1654(Pt B):157–164. doi: 10.1016/j.brainres.2016.08.037. [DOI] [PubMed] [Google Scholar]
- 93.Augustin SM, Lovinger DM. Functional relevance of endocannabinoid-dependent synaptic plasticity in the central nervous system. ACS Chem Neurosci. 2018;9(9):2146–2161. doi: 10.1021/acschemneuro.7b00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Guo S, Liu Y, Ma R, Li J, Su B. Neuroprotective effect of endogenous cannabinoids on ischemic brain injury induced by the excess microglia-mediated inflammation. Am J Transl Res. 2016;8(6):2631–2640. [PMC free article] [PubMed] [Google Scholar]
- 95.Szczesniak AM, Porter RF, Toguri JT, Borowska-Fielding J, Gebremeskel S, Siwakoti A, et al. Cannabinoid 2 receptor is a novel anti-inflammatory target in experimental proliferative vitreoretinopathy. Neuropharmacology. 2017;113(Pt B):627–638. doi: 10.1016/j.neuropharm.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 96.Zurier RB, Burstein SH. Cannabinoids, inflammation, and fibrosis. FASEB J. 2016;30(11):3682–3689. doi: 10.1096/fj.201600646R. [DOI] [PubMed] [Google Scholar]
- 97.Rajesh M, Mukhopadhyay P, Batkai S, Patel V, Saito K, Matsumoto S, et al. Cannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell death signaling pathways in diabetic cardiomyopathy. J Am Coll Cardiol. 2010;56(25):2115–25. doi: 10.1016/j.jacc.2010.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Benito C, Romero JP, Tolon RM, Clemente D, Docagne F, Hillard CJ, et al. Cannabinoid CB1 and CB2 receptors and fatty acid amide hydrolase are specific markers of plaque cell subtypes in human multiple sclerosis. J Neurosci. 2007;27(9):2396–2402. doi: 10.1523/JNEUROSCI.4814-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ramirez BG, Blazquez C, Gomez del Pulgar T, Guzman M, de Ceballos ML. Prevention of Alzheimer’s disease pathology by cannabinoids: neuroprotection mediated by blockade of microglial activation. J Neurosci. 2005;25(8):1904–1913. doi: 10.1523/JNEUROSCI.4540-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mbvundula EC, Bunning RA, Rainsford KD. Arthritis and cannabinoids: HU-210 and Win-55,212-2 prevent IL-1alpha-induced matrix degradation in bovine articular chondrocytes in-vitro. J Pharm Pharmacol. 2006;58(3):351–358. doi: 10.1211/jpp.58.3.0009. [DOI] [PubMed] [Google Scholar]
- 101.Tomar S, Zumbrun EE, Nagarkatti M, Nagarkatti PS. Protective role of cannabinoid receptor 2 activation in galactosamine/lipopolysaccharide-induced acute liver failure through regulation of macrophage polarization and microRNAs. J Pharmacol Exp Ther. 2015;353(2):369–379. doi: 10.1124/jpet.114.220368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu Y, Fassbender K. Deficiency of TLR4 ameliorates hypoperfusion-induced brain pathology. Theranostics. 2018;8(22):6355–6356. doi: 10.7150/thno.30953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lee W, Park JY, Chun YM. Operative treatment of 2-part surgical neck fracture of the humerus: intramedullary nail versus locking compression plate with technical consideration. J Orthop Trauma. 2017;31(9):e270–e2e4. doi: 10.1097/BOT.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 104.Kim MS, Bang JH, Lee J, Kim HW, Sung SH, Han JS, et al. Salvia miltiorrhiza extract protects white matter and the hippocampus from damage induced by chronic cerebral hypoperfusion in rats. BMC Complement Altern Med. 2015;15:415. doi: 10.1186/s12906-015-0943-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee KM, Bang J, Kim BY, Lee IS, Han JS, Hwang BY, et al. Fructus mume alleviates chronic cerebral hypoperfusion-induced white matter and hippocampal damage via inhibition of inflammation and downregulation of TLR4 and p38 MAPK signaling. BMC Complement Altern Med. 2015;15:125. doi: 10.1186/s12906-015-0652-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Srivastava T, Diba P, Dean JM, Banine F, Shaver D, Hagen M, et al. A TLR/AKT/FoxO3 immune tolerance-like pathway disrupts the repair capacity of oligodendrocyte progenitors. J Clin Invest. 2018;128(5):2025–2041. doi: 10.1172/JCI94158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Habib A, Chokr D, Wan J, Hegde P, Mabire M, Siebert M, et al. Inhibition of monoacylglycerol lipase, an anti-inflammatory and antifibrogenic strategy in the liver. Gut. 2018. 10.1136/gutjnl-2018-316137. [DOI] [PubMed]
- 108.Xiang W, Shi R, Kang X, Zhang X, Chen P, Zhang L, et al. Monoacylglycerol lipase regulates cannabinoid receptor 2-dependent macrophage activation and cancer progression. Nat Commun. 2018;9(1):2574. doi: 10.1038/s41467-018-04999-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tobin RP, Mukherjee S, Kain JM, Rogers SK, Henderson SK, Motal HL, et al. Traumatic brain injury causes selective, CD74-dependent peripheral lymphocyte activation that exacerbates neurodegeneration. Acta Neuropathol Commun. 2014;2(1):143. doi: 10.1186/s40478-014-0143-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hua R, Mao SS, Zhang YM, Chen FX, Zhou ZH, Liu JQ. Effects of pituitary adenylate cyclase activating polypeptide on CD4(+)/CD8(+) T cell levels after traumatic brain injury in a rat model. World J Emerg Med. 2012;3(4):294–298. doi: 10.5847/wjem.j.issn.1920-8642.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Amick JE, Yandora KA, Bell MJ, Wisniewski SR, Adelson PD, Carcillo JA, et al. The Th1 versus Th2 cytokine profile in cerebrospinal fluid after severe traumatic brain injury in infants and children. Pediatr Crit Care Med. 2001;2(3):260–264. doi: 10.1097/00130478-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 112.Ojo JO, Greenberg MB, Leary P, Mouzon B, Bachmeier C, Mullan M, et al. Neurobehavioral, neuropathological and biochemical profiles in a novel mouse model of co-morbid post-traumatic stress disorder and mild traumatic brain injury. Front Behav Neurosci. 2014;8:213. doi: 10.3389/fnbeh.2014.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Braun M, Vaibhav K, Saad N, Fatima S, Brann DW, Vender JR, et al. Activation of myeloid TLR4 mediates t lymphocyte polarization after traumatic brain injury. J Immunol. 2017;198(9):3615–26. 10.4049/jimmunol.1601948. [DOI] [PMC free article] [PubMed]
- 114.Braun M, Vaibhav K, Saad NM, Fatima S, Vender JR, Baban B, et al. White matter damage after traumatic brain injury: a role for damage associated molecular patterns. Biochim Biophys Acta Mol basis Dis. 2017;1863(10 Pt B):2614–2626. doi: 10.1016/j.bbadis.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Alberti TB, Barbosa WL, Vieira JL, Raposo NR, Dutra RC. (-)-Beta-caryophyllene, a CB2 receptor-selective phytocannabinoid, suppresses motor paralysis and neuroinflammation in a murine model of multiple sclerosis. Int J Mol Sci. 2017;18(4). 10.3390/ijms18040691. [DOI] [PMC free article] [PubMed]
- 116.Annunziata P, Cioni C, Mugnaini C, Corelli F. Potent immunomodulatory activity of a highly selective cannabinoid CB2 agonist on immune cells from healthy subjects and patients with multiple sclerosis. J Neuroimmunol. 2017;303:66–74. doi: 10.1016/j.jneuroim.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 117.Fraguas-Sánchez AI, Torres-Suárez AI. Medical use of cannabinoids. Drugs. 2018;78(16):1665–1703. doi: 10.1007/s40265-018-0996-1. [DOI] [PubMed] [Google Scholar]
- 118.Schurman LD, Lichtman AH. Endocannabinoids: a promising impact for traumatic brain injury. Front Pharmacol. 2017;8:69. doi: 10.3389/fphar.2017.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bullock R, Zauner A, Woodward JJ, Myseros J, Choi SC, Ward JD, et al. Factors affecting excitatory amino acid release following severe human head injury. J Neurosurg. 1998;89(4):507–518. doi: 10.3171/jns.1998.89.4.0507. [DOI] [PubMed] [Google Scholar]
- 120.Zhao J, Moore AN, Clifton GL, Dash PK. Sulforaphane enhances aquaporin-4 expression and decreases cerebral edema following traumatic brain injury. J Neurosci Res. 2005;82(4):499–506. doi: 10.1002/jnr.20649. [DOI] [PubMed] [Google Scholar]
- 121.Meyer MJ, Megyesi J, Meythaler J, Murie-Fernandez M, Aubut JA, Foley N, et al. Acute management of acquired brain injury part II: an evidence-based review of pharmacological interventions. Brain Inj. 2010;24(5):706–721. doi: 10.3109/02699051003692126. [DOI] [PubMed] [Google Scholar]
- 122.Donat CK, Fischer F, Walter B, Deuther-Conrad W, Brodhun M, Bauer R, et al. Early increase of cannabinoid receptor density after experimental traumatic brain injury in the newborn piglet. Acta Neurobiol Exp. 2014;74(2):197–210. doi: 10.55782/ane-2014-1985. [DOI] [PubMed] [Google Scholar]
- 123.Amenta PS, Jallo JI, Tuma RF, Elliott MB. A cannabinoid type 2 receptor agonist attenuates blood-brain barrier damage and neurodegeneration in a murine model of traumatic brain injury. J Neurosci Res. 2012;90(12):2293–2305. doi: 10.1002/jnr.23114. [DOI] [PubMed] [Google Scholar]
- 124.Shohami E, Cohen-Yeshurun A, Magid L, Algali M, Mechoulam R. Endocannabinoids and traumatic brain injury. Br J Pharmacol. 2011;163(7):1402–1410. doi: 10.1111/j.1476-5381.2011.01343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Xing G, Carlton J, Jiang X, Wen J, Jia M, Li H. Differential expression of brain cannabinoid receptors between repeatedly stressed males and females may play a role in age and gender-related difference in traumatic brain injury: implications from animal studies. Front Neurol. 2014;5:161. doi: 10.3389/fneur.2014.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mechoulam R, Shohami E. Endocannabinoids and traumatic brain injury. Mol Neurobiol. 2007;36(1):68–74. doi: 10.1007/s12035-007-8008-6. [DOI] [PubMed] [Google Scholar]
- 127.Panikashvili D, Shein NA, Mechoulam R, Trembovler V, Kohen R, Alexandrovich A, et al. The endocannabinoid 2-AG protects the blood-brain barrier after closed head injury and inhibits mRNA expression of proinflammatory cytokines. Neurobiol Dis. 2006;22(2):257–264. doi: 10.1016/j.nbd.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 128.Panikashvili D, Mechoulam R, Beni SM, Alexandrovich A, Shohami E. CB1 cannabinoid receptors are involved in neuroprotection via NF-kappa B inhibition. J Cereb Blood Flow Metab. 2005;25(4):477–484. doi: 10.1038/sj.jcbfm.9600047. [DOI] [PubMed] [Google Scholar]
- 129.Panikashvili D, Simeonidou C, Ben-Shabat S, Hanus L, Breuer A, Mechoulam R, et al. An endogenous cannabinoid (2-AG) is neuroprotective after brain injury. Nature. 2001;413(6855):527–531. doi: 10.1038/35097089. [DOI] [PubMed] [Google Scholar]
- 130.Mayeux J, Katz P, Edwards S, Middleton JW, Molina PE. Inhibition of endocannabinoid degradation improves outcomes from mild traumatic brain injury: a mechanistic role for synaptic hyperexcitability. J Neurotrauma. 2017;34(2):436–443. doi: 10.1089/neu.2016.4452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tchantchou F, Zhang Y. Selective inhibition of alpha/beta-hydrolase domain 6 attenuates neurodegeneration, alleviates blood brain barrier breakdown, and improves functional recovery in a mouse model of traumatic brain injury. J Neurotrauma. 2013;30(7):565–579. doi: 10.1089/neu.2012.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Selvaraj P, Wen J, Tanaka M, Zhang Y. Therapeutic effect of a novel fatty acid amide hydrolase inhibitor PF04457845 in the repetitive closed head injury mouse model. J Neurotrauma. 2019;36(10):1655–1669. doi: 10.1089/neu.2018.6226. [DOI] [PubMed] [Google Scholar]
- 133.Katz PS, Sulzer JK, Impastato RA, Teng SX, Rogers EK, Molina PE. Endocannabinoid degradation inhibition improves neurobehavioral function, blood-brain barrier integrity, and neuroinflammation following mild traumatic brain injury. J Neurotrauma. 2015;32(5):297–306. doi: 10.1089/neu.2014.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tchantchou F, Tucker LB, Fu AH, Bluett RJ, McCabe JT, Patel S, et al. The fatty acid amide hydrolase inhibitor PF-3845 promotes neuronal survival, attenuates inflammation and improves functional recovery in mice with traumatic brain injury. Neuropharmacology. 2014;85:427–439. doi: 10.1016/j.neuropharm.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chen R, Zhang J, Wu Y, Wang D, Feng G, Tang YP, et al. Monoacylglycerol lipase is a therapeutic target for Alzheimer’s disease. Cell Rep. 2012;2(5):1329–1339. doi: 10.1016/j.celrep.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Johnson VE, Stewart W, Smith DH. Traumatic brain injury and amyloid-β pathology: a link to Alzheimer’s disease? Nat Rev Neurosci. 2010;11(5):361–370. doi: 10.1038/nrn2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Goldstein LE, Fisher AM, Tagge CA, Zhang X-L, Velisek L, Sullivan JA, et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Sci Transl Med. 2012;4(134):134ra60-ra60. doi: 10.1126/scitranslmed.3003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Smith DH, Chen XH, Nonaka M, Trojanowski JQ, Lee VM, Saatman KE, et al. Accumulation of amyloid beta and tau and the formation of neurofilament inclusions following diffuse brain injury in the pig. J Neuropathol Exp Neurol. 1999;58(9):982–992. doi: 10.1097/00005072-199909000-00008. [DOI] [PubMed] [Google Scholar]
- 139.Amenta PS, Jallo JI, Tuma RF, Elliott MB. A cannabinoid type 2 receptor agonist attenuates blood-brain barrier damage and neurodegeneration in a murine model of traumatic brain injury. J Neurosci Res. 2012;90(12):2293–2305. doi: 10.1002/jnr.23114. [DOI] [PubMed] [Google Scholar]
- 140.Schmitt U, Tanimoto N, Seeliger M, Schaeffel F, Leube RE. Detection of behavioral alterations and learning deficits in mice lacking synaptophysin. Neuroscience. 2009;162(2):234–243. doi: 10.1016/j.neuroscience.2009.04.046. [DOI] [PubMed] [Google Scholar]
- 141.Hind WH, Tufarelli C, Neophytou M, Anderson SI, England TJ, O'Sullivan SE. Endocannabinoids modulate human blood-brain barrier permeability in vitro. Br J Pharmacol. 2015;172(12):3015–3027. doi: 10.1111/bph.13106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hu D-E, Easton AS, Fraser PA. TRPV1 activation results in disruption of the blood-brain barrier in the rat. Br J Pharmacol. 2005;146(4):576–584. doi: 10.1038/sj.bjp.0706350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pertwee RG, Ross RA. Cannabinoid receptors and their ligands. Prostaglandins Leukot Essent Fat Acids. 2002;66(2–3):101–121. doi: 10.1054/plef.2001.0341. [DOI] [PubMed] [Google Scholar]
- 144.Guley NM, Del Mar NA, Ragsdale T, Li C, Perry AM, Moore BM, et al. Amelioration of visual deficits and visual system pathology after mild TBI with the cannabinoid type-2 receptor inverse agonist SMM-189. Exp Eye Res. 2019;182:109–124. doi: 10.1016/j.exer.2019.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Honig MG, Del Mar NA, Henderson DL, Ragsdale TD, Doty JB, Driver JH, et al. Amelioration of visual deficits and visual system pathology after mild TBI via the cannabinoid type-2 receptor inverse agonism of raloxifene. Exp Neurol. 2019;322:113063. doi: 10.1016/j.expneurol.2019.113063. [DOI] [PubMed] [Google Scholar]
- 146.Lopez-Rodriguez AB, Mela V, Acaz-Fonseca E, Garcia-Segura LM, Viveros M-P. CB2 cannabinoid receptor is involved in the anti-inflammatory effects of leptin in a model of traumatic brain injury. Exp Neurol. 2016;279:274–282. doi: 10.1016/j.expneurol.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 147.Lopez-Rodriguez AB, Siopi E, Finn DP, Marchand-Leroux C, Garcia-Segura LM, Jafarian-Tehrani M, et al. CB1 and CB2 cannabinoid receptor antagonists prevent minocycline-induced neuroprotection following traumatic brain injury in mice. Cereb Cortex. 2015;25(1):35–45. doi: 10.1093/cercor/bht202. [DOI] [PubMed] [Google Scholar]
- 148.López Rodríguez AB, Mateos Vicente B, Romero-Zerbo SY, Rodriguez-Rodriguez N, Bellini MJ, Rodriguez de Fonseca F, et al. Estradiol decreases cortical reactive astrogliosis after brain injury by a mechanism involving cannabinoid receptors. Cereb Cortex. 2011;21(9):2046–2055. doi: 10.1093/cercor/bhq277. [DOI] [PubMed] [Google Scholar]
- 149.Walker R, Cole JE, Logan TK, Corrigan JD. Screening substance abuse treatment clients for traumatic brain injury: prevalence and characteristics. J Head Trauma Rehabil. 2007;22(6):360–367. doi: 10.1097/01.HTR.0000300231.90619.50. [DOI] [PubMed] [Google Scholar]
- 150.O'Phelan K, McArthur DL, Chang CW, Green D, Hovda DA. The impact of substance abuse on mortality in patients with severe traumatic brain injury. J Trauma. 2008;65(3):674–677. doi: 10.1097/TA.0b013e31817db0a5. [DOI] [PubMed] [Google Scholar]
- 151.Hawley LA, Ketchum JM, Morey C, Collins K, Charlifue S. Cannabis use in individuals with spinal cord injury or moderate to severe traumatic brain injury in Colorado. Arch Phys Med Rehabil. 2018;99(8):1584–1590. doi: 10.1016/j.apmr.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 152.Nguyen BM, Kim D, Bricker S, Bongard F, Neville A, Putnam B, et al. Effect of marijuana use on outcomes in traumatic brain injury. Am Surg. 2014;80(10):979–983. [PubMed] [Google Scholar]
- 153.Lawrence DW, Foster E, Comper P, Langer L, Hutchison MG, Chandra T, et al. Cannabis, alcohol and cigarette use during the acute post-concussion period. Brain Inj. 2020;34(1):42–51. doi: 10.1080/02699052.2019.1679885. [DOI] [PubMed] [Google Scholar]
- 154.Grenier K, Ponnambalam F, Lee D, Lauwers R, Bhalerao S. Cannabis in the treatment of traumatic brain injury: a primer for clinicians. Can J Neurol Sci. 2019:1–7. 10.1017/cjn.2019.298. [DOI] [PubMed]
- 155.Rabner J, Gottlieb S, Lazdowsky L, LeBel A. Psychosis following traumatic brain injury and cannabis use in late adolescence. Am J Addict. 2016;25(2):91–93. doi: 10.1111/ajad.12338. [DOI] [PubMed] [Google Scholar]
- 156.Polivka J, Jr, Polivka J, Pesta M, Rohan V, Celedova L, Mahajani S, et al. Risks associated with the stroke predisposition at young age: facts and hypotheses in light of individualized predictive and preventive approach. EPMA J. 2019;10(1):81–99. doi: 10.1007/s13167-019-00162-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.England TJ, Hind WH, Rasid NA, O'Sullivan SE. Cannabinoids in experimental stroke: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2015;35(3):348–358. doi: 10.1038/jcbfm.2014.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Suzuki N, Suzuki M, Murakami K, Hamajo K, Tsukamoto T, Shimojo M. Cerebroprotective effects of TAK-937, a cannabinoid receptor agonist, on ischemic brain damage in middle cerebral artery occluded rats and non-human primates. Brain Res. 2012;1430:93–100. doi: 10.1016/j.brainres.2011.10.044. [DOI] [PubMed] [Google Scholar]
- 159.Leker RR, Gai N, Mechoulam R, Ovadia H. Drug-induced hypothermia reduces ischemic damage: effects of the cannabinoid HU-210. Stroke. 2003;34(8):2000–2006. doi: 10.1161/01.STR.0000079817.68944.1E. [DOI] [PubMed] [Google Scholar]
- 160.Bravo-Ferrer I, Cuartero MI, Zarruk JG, Pradillo JM, Hurtado O, Romera VG, et al. Cannabinoid type-2 receptor drives neurogenesis and improves functional outcome after stroke. Stroke. 2017;48(1):204–212. doi: 10.1161/STROKEAHA.116.014793. [DOI] [PubMed] [Google Scholar]
- 161.Wang Q, Peng Y, Chen S, Gou X, Hu B, Du J, et al. Pretreatment with electroacupuncture induces rapid tolerance to focal cerebral ischemia through regulation of endocannabinoid system. Stroke. 2009;40(6):2157–2164. doi: 10.1161/STROKEAHA.108.541490. [DOI] [PubMed] [Google Scholar]
- 162.Ceprián M, Jiménez-Sánchez L, Vargas C, Barata L, Hind W, Martínez-Orgado J. Cannabidiol reduces brain damage and improves functional recovery in a neonatal rat model of arterial ischemic stroke. Neuropharmacology. 2017;116:151–159. doi: 10.1016/j.neuropharm.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 163.Hind WH, England TJ, O’Sullivan SE. Cannabidiol protects an in vitro model of the blood-brain barrier from oxygen-glucose deprivation via PPARγ and 5-HT1A receptors. Br J Pharmacol. 2016;173(5):815–825. doi: 10.1111/bph.13368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rajesh M, Mukhopadhyay P, Bátkai S, Haskó G, Liaudet L, Drel VR, et al. Cannabidiol attenuates high glucose-induced endothelial cell inflammatory response and barrier disruption. Am J Physiol Heart Circ Physiol. 2007;293(1):H610–H6H9. doi: 10.1152/ajpheart.00236.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mishima K, Hayakawa K, Abe K, Ikeda T, Egashira N, Iwasaki K, et al. Cannabidiol prevents cerebral infarction via a serotonergic 5-hydroxytryptamine1A receptor-dependent mechanism. Stroke. 2005;36(5):1077–1082. doi: 10.1161/01.STR.0000163083.59201.34. [DOI] [PubMed] [Google Scholar]
- 166.Alvarez FJ, Lafuente H, Rey-Santano MC, Mielgo VE, Gastiasoro E, Rueda M, et al. Neuroprotective effects of the nonpsychoactive cannabinoid cannabidiol in hypoxic-ischemic newborn piglets. Pediatr Res. 2008;64(6):653–658. doi: 10.1203/PDR.0b013e318186e5dd. [DOI] [PubMed] [Google Scholar]
- 167.Sultan SR, Millar SA, England TJ, O’Sullivan SE. A systematic review and meta-analysis of the haemodynamic effects of cannabidiol. Front Pharmacol. 2017;8:81. doi: 10.3389/fphar.2017.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Jadoon KA, Tan GD, O'Sullivan SE. A single dose of cannabidiol reduces blood pressure in healthy volunteers in a randomized crossover study. JCI Insight. 2017;2(12):e93760. doi: 10.1172/jci.insight.93760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hayakawa K, Irie K, Sano K, Watanabe T, Higuchi S, Enoki M, et al. Therapeutic time window of cannabidiol treatment on delayed ischemic damage via high-mobility group box1-inhibiting mechanism. Biol Pharm Bull. 2009;32(9):1538–1544. doi: 10.1248/bpb.32.1538. [DOI] [PubMed] [Google Scholar]
- 170.Hayakawa K, Mishima K, Fujiwara M. Therapeutic potential of non-psychotropic cannabidiol in ischemic stroke. Pharmaceuticals (Basel, Switzerland) 2010;3(7):2197–2212. doi: 10.3390/ph3072197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Parmentier-Batteur S, Jin K, Mao XO, Xie L, Greenberg DA. Increased severity of stroke in CB1 cannabinoid receptor knock-out mice. J Neurosci. 2002;22(22):9771–9775. doi: 10.1523/JNEUROSCI.22-22-09771.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hayakawa K, Mishima K, Nozako M, Hazekawa M, Ogata A, Fujioka M, et al. Delta9-tetrahydrocannabinol (delta9-THC) prevents cerebral infarction via hypothalamic-independent hypothermia. Life Sci. 2007;80(16):1466–1471. doi: 10.1016/j.lfs.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 173.Choi S-H, Mou Y, Silva AC. Cannabis and cannabinoid biology in stroke. Stroke. 2019;50(9):2640–2645. doi: 10.1161/STROKEAHA.118.023587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wolff V, Jouanjus E. Strokes are possible complications of cannabinoids use. Epilepsy Behav. 2017;70(Pt B):355–363. doi: 10.1016/j.yebeh.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 175.Shearer JA, Coker SJ, Carswell HVO. Detrimental effects of 2-arachidonoylglycerol on whole blood platelet aggregation and on cerebral blood flow after a focal ischemic insult in rats. Am J Physiol Heart Circ Physiol. 2018;314(5):H967–HH77. doi: 10.1152/ajpheart.00299.2017. [DOI] [PubMed] [Google Scholar]
- 176.Keown OP, Winterburn TJ, Wainwright CL, Macrury SM, Neilson I, Barrett F, et al. 2-Arachidonyl glycerol activates platelets via conversion to arachidonic acid and not by direct activation of cannabinoid receptors. Br J Clin Pharmacol. 2010;70(2):180–188. doi: 10.1111/j.1365-2125.2010.03697.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Brantl SA, Khandoga AL, Siess W. Mechanism of platelet activation induced by endocannabinoids in blood and plasma. Platelets. 2014;25(3):151–161. doi: 10.3109/09537104.2013.803530. [DOI] [PubMed] [Google Scholar]
- 178.Polivka J, Polivka J, Jr, Rohan V. Predictive and individualized management of stroke-success story in Czech Republic. EPMA J. 2018;9(4):393–401. doi: 10.1007/s13167-018-0150-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Roos RA. Huntington’s disease: a clinical review. Orphanet J Rare Dis. 2010;5:40. doi: 10.1186/1750-1172-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Pazos MR, Sagredo O, Fernandez-Ruiz J. The endocannabinoid system in Huntington’s disease. Curr Pharm Des. 2008;14(23):2317–2325. doi: 10.2174/138161208785740108. [DOI] [PubMed] [Google Scholar]
- 181.Pacher P, Kunos G. Modulating the endocannabinoid system in human health and disease—successes and failures. FEBS J. 2013;280(9):1918–1943. doi: 10.1111/febs.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Micale V, Mazzola C, Drago F. Endocannabinoids and neurodegenerative diseases. Pharmacol Res. 2007;56(5):382–392. doi: 10.1016/j.phrs.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 183.Maccarrone M, Battista N, Centonze D. The endocannabinoid pathway in Huntington's disease: a comparison with other neurodegenerative diseases. Prog Neurobiol. 2007;81(5–6):349–379. doi: 10.1016/j.pneurobio.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 184.Lastres-Becker I, Bizat N, Boyer F, Hantraye P, Brouillet E, Fernandez-Ruiz J. Effects of cannabinoids in the rat model of Huntington’s disease generated by an intrastriatal injection of malonate. Neuroreport. 2003;14(6):813–816. doi: 10.1097/00001756-200305060-00007. [DOI] [PubMed] [Google Scholar]
- 185.Kreitzer AC, Malenka RC. Endocannabinoid-mediated rescue of striatal LTD and motor deficits in Parkinson’s disease models. Nature. 2007;445(7128):643–647. doi: 10.1038/nature05506. [DOI] [PubMed] [Google Scholar]
- 186.Dowie MJ, Bradshaw HB, Howard ML, Nicholson LF, Faull RL, Hannan AJ, et al. Altered CB1 receptor and endocannabinoid levels precede motor symptom onset in a transgenic mouse model of Huntington’s disease. Neuroscience. 2009;163(1):456–465. doi: 10.1016/j.neuroscience.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 187.Bisogno T, Di Marzo V. The role of the endocannabinoid system in Alzheimer’s disease: facts and hypotheses. Curr Pharm Des. 2008;14(23):2299–3305. doi: 10.2174/138161208785740027. [DOI] [PubMed] [Google Scholar]
- 188.Di Marzo V, Bifulco M, De Petrocellis L. The endocannabinoid system and its therapeutic exploitation. Nat Rev Drug Discov. 2004;3(9):771–784. doi: 10.1038/nrd1495. [DOI] [PubMed] [Google Scholar]
- 189.Palazuelos J, Aguado T, Pazos MR, Julien B, Carrasco C, Resel E, et al. Microglial CB2 cannabinoid receptors are neuroprotective in Huntington’s disease excitotoxicity. Brain. 2009;132(Pt 11):3152–3164. doi: 10.1093/brain/awp239. [DOI] [PubMed] [Google Scholar]
- 190.Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C, et al. Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice. Cell. 1996;87(3):493–506. doi: 10.1016/s0092-8674(00)81369-0. [DOI] [PubMed] [Google Scholar]
- 191.Sapp E, Kegel KB, Aronin N, Hashikawa T, Uchiyama Y, Tohyama K, et al. Early and progressive accumulation of reactive microglia in the Huntington disease brain. J Neuropathol Exp Neurol. 2001;60(2):161–172. doi: 10.1093/jnen/60.2.161. [DOI] [PubMed] [Google Scholar]
- 192.Sagredo O, Pazos MR, Valdeolivas S, Fernandez-Ruiz J. Cannabinoids: novel medicines for the treatment of Huntington’s disease. Recent Pat CNS Drug Discov. 2012;7(1):41–48. doi: 10.2174/157488912798842278. [DOI] [PubMed] [Google Scholar]
- 193.Valdeolivas S, Navarrete C, Cantarero I, Bellido ML, Muñoz E, Sagredo O. Neuroprotective properties of cannabigerol in Huntington’s disease: studies in R6/2 mice and 3-nitropropionate-lesioned mice. Neurotherapeutics. 2015;12(1):185–199. doi: 10.1007/s13311-014-0304-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Díaz-Alonso J, Paraíso-Luna J, Navarrete C, Del Río C, Cantarero I, Palomares B, et al. VCE-003.2, a novel cannabigerol derivative, enhances neuronal progenitor cell survival and alleviates symptomatology in murine models of Huntington’s disease. Sci Rep. 2016;6:29789. doi: 10.1038/srep29789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Saft C, von Hein SM, Lücke T, Thiels C, Peball M, Djamshidian A, et al. Cannabinoids for treatment of dystonia in Huntington’s disease. J Huntingtons Dis. 2018;7(2):167–173. doi: 10.3233/JHD-170283. [DOI] [PubMed] [Google Scholar]
- 196.Zarei S, Carr K, Reiley L, Diaz K, Guerra O, Altamirano PF, et al. A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int. 2015;6:171. doi: 10.4103/2152-7806.169561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Flavell L. Approved treatments. ALS News Today 2020. https://alsnewstoday.com/approved-treatments/. Accessed January 9 2020.
- 198.FDA-approved drugs. The ALS Association. 2020. http://www.alsa.org/als-care/fda-approved-drugs.html. Accessed January 9 2020.
- 199.Hardiman O, van den Berg LH, Kiernan MC. Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat Rev Neurol. 2011;7(11):639–649. doi: 10.1038/nrneurol.2011.153. [DOI] [PubMed] [Google Scholar]
- 200.Matamala JM, Dharmadasa T, Kiernan MC. Prognostic factors in C9orf72 amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2017;88(4):281. doi: 10.1136/jnnp-2016-314685. [DOI] [PubMed] [Google Scholar]
- 201.Miller RG, Mitchell JD, Lyon M, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst Rev. 2007;(1):CD001447-CD. 10.1002/14651858.CD001447.pub2. [DOI] [PubMed]
- 202.Raman C, McAllister SD, Rizvi G, Patel SG, Moore DH, Abood ME. Amyotrophic lateral sclerosis: delayed disease progression in mice by treatment with a cannabinoid. Amyotroph Lateral Scler Other Motor Neuron Disord. 2004;5(1):33–39. doi: 10.1080/14660820310016813. [DOI] [PubMed] [Google Scholar]
- 203.Moreno-Martet M, Espejo-Porras F, Fernández-Ruiz J, de Lago E. Changes in endocannabinoid receptors and enzymes in the spinal cord of SOD1(G93A) transgenic mice and evaluation of a Sativex(®)-like combination of phytocannabinoids: interest for future therapies in amyotrophic lateral sclerosis. CNS Neurosci Ther. 2014;20(9):809–815. doi: 10.1111/cns.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Weydt P, Hong S, Witting A, Möller T, Stella N, Kliot M. Cannabinol delays symptom onset in SOD1 (G93A) transgenic mice without affecting survival. Amyotroph Lateral Scler Other Motor Neuron Disord. 2005;6(3):182–184. doi: 10.1080/14660820510030149. [DOI] [PubMed] [Google Scholar]
- 205.Bilsland LG, Dick JRT, Pryce G, Petrosino S, Di Marzo V, Baker D, et al. Increasing cannabinoid levels by pharmacological and genetic manipulation delay disease progression in SOD1 mice. FASEB J. 2006;20(7):1003–1005. doi: 10.1096/fj.05-4743fje. [DOI] [PubMed] [Google Scholar]
- 206.Yiangou Y, Facer P, Durrenberger P, Chessell IP, Naylor A, Bountra C, et al. COX-2, CB2 and P2X7-immunoreactivities are increased in activated microglial cells/macrophages of multiple sclerosis and amyotrophic lateral sclerosis spinal cord. BMC Neurol. 2006;6:12. doi: 10.1186/1471-2377-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Shoemaker JL, Seely KA, Reed RL, Crow JP, Prather PL. The CB2 cannabinoid agonist AM-1241 prolongs survival in a transgenic mouse model of amyotrophic lateral sclerosis when initiated at symptom onset. J Neurochem. 2007;101(1):87–98. doi: 10.1111/j.1471-4159.2006.04346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Walter L, Stella N. Cannabinoids and neuroinflammation. Br J Pharmacol. 2004;141(5):775–785. doi: 10.1038/sj.bjp.0705667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Amtmann D, Weydt P, Johnson KL, Jensen MP, Carter GT. Survey of cannabis use in patients with amyotrophic lateral sclerosis. Am J Hosp Palliat Care. 2004;21(2):95–104. doi: 10.1177/104990910402100206. [DOI] [PubMed] [Google Scholar]
- 210.Carter GT, Rosen BS. Marijuana in the management of amyotrophic lateral sclerosis. Am J Hosp Palliat Care. 2001;18(4):264–270. doi: 10.1177/104990910101800411. [DOI] [PubMed] [Google Scholar]
- 211.Urbi B, Broadley S, Bedlack R, Russo E, Sabet A. Study protocol for a randomised, double-blind, placebo-controlled study evaluating the Efficacy of cannabis-based Medicine Extract in slowing the disease pRogression of Amyotrophic Lateral sclerosis or motor neurone Disease: the EMERALD trial. BMJ Open. 2019;9(11):e029449-e. doi: 10.1136/bmjopen-2019-029449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Baul HS, Manikandan C, Sen D. Cannabinoid receptor as a potential therapeutic target for Parkinson’s disease. Brain Res Bull. 2019;146:244–252. doi: 10.1016/j.brainresbull.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 213.Ceccarini J, Casteels C, Ahmad R, Crabbé M, Van de Vliet L, Vanhaute H, et al. Regional changes in the type 1 cannabinoid receptor are associated with cognitive dysfunction in Parkinson’s disease. Eur J Nucl Med Mol Imaging. 2019;46(11):2348–2357. doi: 10.1007/s00259-019-04445-x. [DOI] [PubMed] [Google Scholar]
- 214.Meireles J, Massano J. Cognitive impairment and dementia in parkinson’s disease: clinical features, diagnosis, and management. Front Neurol. 2012;3(88). 10.3389/fneur.2012.00088. [DOI] [PMC free article] [PubMed]
- 215.Tang Y, Ge J, Liu F, Wu P, Guo S, Liu Z, et al. Cerebral metabolic differences associated with cognitive impairment in Parkinson’s disease. PLoS One. 2016;11(4):e0152716. doi: 10.1371/journal.pone.0152716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Broeders M, Velseboer DC, de Bie R, Speelman JD, Muslimovic D, Post B, et al. Cognitive change in newly-diagnosed patients with Parkinson’s disease: a 5-year follow-up study. J Int Neuropsychol Soc. 2013;19(6):695–708. doi: 10.1017/S1355617713000295. [DOI] [PubMed] [Google Scholar]
- 217.MuslimoviĆ D, Post B, Speelman JD, De Haan RJ, Schmand BEN. Cognitive decline in Parkinson’s disease: a prospective longitudinal study. J Int Neuropsychol Soc. 2009;15(3):426–437. doi: 10.1017/S1355617709090614. [DOI] [PubMed] [Google Scholar]
- 218.Han Q-W, Yuan Y-H, Chen N-H. The therapeutic role of cannabinoid receptors and its agonists or antagonists in Parkinson’s disease. Prog Neuropsychopharmacol Biol Psychiatry. 2020;96:109745. 10.1016/j.pnpbp.2019.109745. [DOI] [PubMed]
- 219.van der Stelt M, Fox SH, Hill M, Crossman AR, Petrosino S, Di Marzo V, et al. A role for endocannabinoids in the generation of parkinsonism and levodopa-induced dyskinesia in MPTP-lesioned non-human primate models of Parkinson’s disease. FASEB J. 2005;19(9):1140–1142. doi: 10.1096/fj.04-3010fje. [DOI] [PubMed] [Google Scholar]
- 220.Segovia G, Mora F, Crossman AR, Brotchie JM. Effects of CB1 cannabinoid receptor modulating compounds on the hyperkinesia induced by high-dose levodopa in the reserpine-treated rat model of Parkinson’s disease. Mov Disord. 2003;18(2):138–149. doi: 10.1002/mds.10312. [DOI] [PubMed] [Google Scholar]
- 221.Scotter EL, Abood ME, Glass M. The endocannabinoid system as a target for the treatment of neurodegenerative disease. Br J Pharmacol. 2010;160(3):480–498. doi: 10.1111/j.1476-5381.2010.00735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Pisani V, Madeo G, Tassone A, Sciamanna G, Maccarrone M, Stanzione P, et al. Homeostatic changes of the endocannabinoid system in Parkinson’s disease. Mov Disord. 2011;26(2):216–222. doi: 10.1002/mds.23457. [DOI] [PubMed] [Google Scholar]
- 223.Pisani A, Fezza F, Galati S, Battista N, Napolitano S, Finazzi-Agro A, et al. High endogenous cannabinoid levels in the cerebrospinal fluid of untreated Parkinson’s disease patients. Ann Neurol. 2005;57(5):777–779. doi: 10.1002/ana.20462. [DOI] [PubMed] [Google Scholar]
- 224.Di Filippo M, Picconi B, Tozzi A, Ghiglieri V, Rossi A, Calabresi P. The endocannabinoid system in Parkinson’s disease. Curr Pharm Des. 2008;14(23):2337–2347. doi: 10.2174/138161208785740072. [DOI] [PubMed] [Google Scholar]
- 225.Centonze D, Finazzi-Agro A, Bernardi G, Maccarrone M. The endocannabinoid system in targeting inflammatory neurodegenerative diseases. Trends Pharmacol Sci. 2007;28(4):180–187. doi: 10.1016/j.tips.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 226.Brotchie JM. CB1 cannabinoid receptor signalling in Parkinson’s disease. Curr Opin Pharmacol. 2003;3(1):54–61. doi: 10.1016/s1471-4892(02)00011-5. [DOI] [PubMed] [Google Scholar]
- 227.Ferrer B, Asbrock N, Kathuria S, Piomelli D, Giuffrida A. Effects of levodopa on endocannabinoid levels in rat basal ganglia: implications for the treatment of levodopa-induced dyskinesias. Eur J Neurosci. 2003;18(6):1607–1614. doi: 10.1046/j.1460-9568.2003.02896.x. [DOI] [PubMed] [Google Scholar]
- 228.Gubellini P, Picconi B, Bari M, Battista N, Calabresi P, Centonze D, et al. Experimental parkinsonism alters endocannabinoid degradation: implications for striatal glutamatergic transmission. J Neurosci. 2002;22(16):6900–6907. doi: 10.1523/JNEUROSCI.22-16-06900.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Hermann H, Marsicano G, Lutz B. Coexpression of the cannabinoid receptor type 1 with dopamine and serotonin receptors in distinct neuronal subpopulations of the adult mouse forebrain. Neuroscience. 2002;109(3):451–460. doi: 10.1016/s0306-4522(01)00509-7. [DOI] [PubMed] [Google Scholar]
- 230.Navarrete F, García-Gutiérrez MS, Aracil-Fernández A, Lanciego JL, Manzanares J. Cannabinoid CB1 and CB2 receptors, and monoacylglycerol lipase gene expression alterations in the basal ganglia of patients with Parkinson’s disease. Neurotherapeutics. 2018;15(2):459–469. doi: 10.1007/s13311-018-0603-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Grunblatt E, Zander N, Bartl J, Jie L, Monoranu CM, Arzberger T, et al. Comparison analysis of gene expression patterns between sporadic Alzheimer’s and Parkinson’s disease. J Alzheimers Dis. 2007;12(4):291–311. doi: 10.3233/jad-2007-12402. [DOI] [PubMed] [Google Scholar]
- 232.Sierra S, Luquin N, Rico AJ, Gómez-Bautista V, Roda E, Dopeso-Reyes IG, et al. Detection of cannabinoid receptors CB1 and CB2 within basal ganglia output neurons in macaques: changes following experimental parkinsonism. Brain Struct Funct. 2015;220(5):2721–2738. doi: 10.1007/s00429-014-0823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Navarro G, Borroto-Escuela D, Angelats E, Etayo Í, Reyes-Resina I, Pulido-Salgado M, et al. Receptor-heteromer mediated regulation of endocannabinoid signaling in activated microglia. Role of CB1 and CB2 receptors and relevance for Alzheimer’s disease and levodopa-induced dyskinesia. Brain Behav Immun. 2018;67:139–151. doi: 10.1016/j.bbi.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 234.Pisani V, Moschella V, Bari M, Fezza F, Galati S, Bernardi G, et al. Dynamic changes of anandamide in the cerebrospinal fluid of Parkinson’s disease patients. Mov Disord. 2010;25(7):920–924. doi: 10.1002/mds.23014. [DOI] [PubMed] [Google Scholar]
- 235.Maccarrone M, Gubellini P, Bari M, Picconi B, Battista N, Centonze D, et al. Levodopa treatment reverses endocannabinoid system abnormalities in experimental parkinsonism. J Neurochem. 2003;85(4):1018–1025. doi: 10.1046/j.1471-4159.2003.01759.x. [DOI] [PubMed] [Google Scholar]
- 236.Celorrio M, Fernández-Suárez D, Rojo-Bustamante E, Echeverry-Alzate V, Ramírez MJ, Hillard CJ, et al. Fatty acid amide hydrolase inhibition for the symptomatic relief of Parkinson’s disease. Brain Behav Immun. 2016;57:94–105. doi: 10.1016/j.bbi.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 237.Viveros-Paredes JM, Gonzalez-Castañeda RE, Escalante-Castañeda A, Tejeda-Martínez AR, Castañeda-Achutiguí F, Flores-Soto ME. Efecto del inhibidor de amida hidrolasa de ácidos grasos en el daño neuronal dopaminérgico inducido por MPTP. Neurología. 2019;34(3):143–152. doi: 10.1016/j.nrl.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 238.Martinez AA, Morgese MG, Pisanu A, Macheda T, Paquette MA, Seillier A, et al. Activation of PPAR gamma receptors reduces levodopa-induced dyskinesias in 6-OHDA-lesioned rats. Neurobiol Dis. 2015;74:295–304. doi: 10.1016/j.nbd.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Solinas M, Justinova Z, Goldberg SR, Tanda G. Anandamide administration alone and after inhibition of fatty acid amide hydrolase (FAAH) increases dopamine levels in the nucleus accumbens shell in rats. J Neurochem. 2006;98(2):408–419. doi: 10.1111/j.1471-4159.2006.03880.x. [DOI] [PubMed] [Google Scholar]
- 240.Fernández-Suárez D, Celorrio M, Riezu-Boj JI, Ugarte A, Pacheco R, González H, et al. The monoacylglycerol lipase inhibitor JZL184 is neuroprotective and alters glial cell phenotype in the chronic MPTP mouse model. Neurobiol Aging. 2014;35(11):2603–2616. doi: 10.1016/j.neurobiolaging.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 241.van Vliet SAM, Vanwersch RAP, Jongsma MJ, Olivier B, Philippens IHCHM. Therapeutic effects of Δ9-THC and modafinil in a marmoset Parkinson model. Eur Neuropsychopharmacol. 2008;18(5):383–389. doi: 10.1016/j.euroneuro.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 242.Fernandez-Espejo E, Caraballo I, de Fonseca FR, El Banoua F, Ferrer B, Flores JA, et al. Cannabinoid CB1 antagonists possess antiparkinsonian efficacy only in rats with very severe nigral lesion in experimental parkinsonism. Neurobiol Dis. 2005;18(3):591–601. doi: 10.1016/j.nbd.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 243.Fernandez-Espejo E, Caraballo I, Rodriguez de Fonseca F, Ferrer B, Banoua FE, Flores JA, et al. Experimental parkinsonism alters anandamide precursor synthesis, and functional deficits are improved by AM404: a modulator of endocannabinoid function. Neuropsychopharmacology. 2004;29(6):1134–1142. doi: 10.1038/sj.npp.1300407. [DOI] [PubMed] [Google Scholar]
- 244.González S, Scorticati C, García-Arencibia M, de Miguel R, Ramos JA, Fernández-Ruiz J. Effects of rimonabant, a selective cannabinoid CB1 receptor antagonist, in a rat model of Parkinson’s disease. Brain Res. 2006;1073–1074:209–219. doi: 10.1016/j.brainres.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 245.Van Laere K, Casteels C, Lunskens S, Goffin K, Grachev ID, Bormans G, et al. Regional changes in type 1 cannabinoid receptor availability in Parkinson’s disease in vivo. Neurobiol Aging. 2012;33(3):620.e1-.e8. doi: 10.1016/j.neurobiolaging.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 246.Lastres-Becker I, Molina-Holgado F, Ramos JA, Mechoulam R, Fernández-Ruiz J. Cannabinoids provide neuroprotection against 6-hydroxydopamine toxicity in vivo and in vitro: relevance to Parkinson’s disease. Neurobiol Dis. 2005;19(1–2):96–107. doi: 10.1016/j.nbd.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 247.Cerri S, Levandis G, Ambrosi G, Montepeloso E, Antoninetti GF, Franco R, et al. Neuroprotective potential of adenosine A2A and cannabinoid CB1 receptor antagonists in an animal model of Parkinson disease. J Neuropathol Exp Neurol. 2014;73(5):414–424. doi: 10.1097/NEN.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 248.Price DA, Martinez AA, Seillier A, Koek W, Acosta Y, Fernandez E, et al. WIN55,212-2, a cannabinoid receptor agonist, protects against nigrostriatal cell loss in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease. Eur J Neurosci. 2009;29(11):2177–2186. doi: 10.1111/j.1460-9568.2009.06764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Chung YC, Bok E, Huh SH, Park J-Y, Yoon S-H, Kim SR, et al. Cannabinoid receptor type 1 protects nigrostriatal dopaminergic neurons against MPTP neurotoxicity by inhibiting microglial activation. J Immunol. 2011;187(12):6508–6517. doi: 10.4049/jimmunol.1102435. [DOI] [PubMed] [Google Scholar]
- 250.Lastres-Becker I, Cebeira M, de Ceballos ML, Zeng B-Y, Jenner P, Ramos JA, et al. Increased cannabinoid CB1 receptor binding and activation of GTP-binding proteins in the basal ganglia of patients with Parkinson’s syndrome and of MPTP-treated marmosets. Eur J Neurosci. 2001;14(11):1827–1832. doi: 10.1046/j.0953-816x.2001.01812.x. [DOI] [PubMed] [Google Scholar]
- 251.Martínez-Pinilla E, Aguinaga D, Navarro G, Rico AJ, Oyarzábal J, Sánchez-Arias JA, et al. Targeting CB(1) and GPR55 endocannabinoid receptors as a potential neuroprotective approach for Parkinson’s disease. Mol Neurobiol. 2019;56(8):5900–5910. doi: 10.1007/s12035-019-1495-4. [DOI] [PubMed] [Google Scholar]
- 252.Zeissler M-L, Eastwood J, McCorry K, Hanemann CO, Zajicek JP, Carroll CB. Delta-9-tetrahydrocannabinol protects against MPP+ toxicity in SH-SY5Y cells by restoring proteins involved in mitochondrial biogenesis. Oncotarget. 2016;7(29):46603–46614. doi: 10.18632/oncotarget.10314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Fishbein-Kaminietsky M, Gafni M, Sarne Y. Ultralow doses of cannabinoid drugs protect the mouse brain from inflammation-induced cognitive damage. J Neurosci Res. 2014;92(12):1669–1677. doi: 10.1002/jnr.23452. [DOI] [PubMed] [Google Scholar]
- 254.McPartland JM, Duncan M, Di Marzo V, Pertwee RG. Are cannabidiol and Δ9-tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br J Pharmacol. 2015;172(3):737–753. doi: 10.1111/bph.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.García C, Palomo-Garo C, García-Arencibia M, Ramos J, Pertwee R, Fernández-Ruiz J. Symptom-relieving and neuroprotective effects of the phytocannabinoid Δ9-THCV in animal models of Parkinson’s disease. Br J Pharmacol. 2011;163(7):1495–1506. doi: 10.1111/j.1476-5381.2011.01278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Ojha S, Javed H, Azimullah S, Haque ME. β-Caryophyllene, a phytocannabinoid attenuates oxidative stress, neuroinflammation, glial activation, and salvages dopaminergic neurons in a rat model of Parkinson disease. Mol Cell Biochem. 2016;418(1):59–70. doi: 10.1007/s11010-016-2733-y. [DOI] [PubMed] [Google Scholar]
- 257.Garcia C, Gomez-Canas M, Burgaz S, Palomares B, Gomez-Galvez Y, Palomo-Garo C, et al. Benefits of VCE-003.2, a cannabigerol quinone derivative, against inflammation-driven neuronal deterioration in experimental Parkinson’s disease: possible involvement of different binding sites at the PPARgamma receptor. J Neuroinflammation. 2018;15(1):19. doi: 10.1186/s12974-018-1060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Burgaz S, Garcia C, Gomez-Canas M, Munoz E, Fernandez-Ruiz J. Development of an oral treatment with the PPAR-gamma-acting cannabinoid VCE-003.2 against the inflammation-driven neuronal deterioration in experimental Parkinson’s disease. Molecules. 2019;24(15). 10.3390/molecules24152702. [DOI] [PMC free article] [PubMed]
- 259.Santos NAG, Martins NM, Sisti FM, Fernandes LS, Ferreira RS, Queiroz RHC, et al. The neuroprotection of cannabidiol against MPP+-induced toxicity in PC12 cells involves trkA receptors, upregulation of axonal and synaptic proteins, neuritogenesis, and might be relevant to Parkinson’s disease. Toxicol In Vitro. 2015;30(1, Part B):231–40. 10.1016/j.tiv.2015.11.004. [DOI] [PubMed]
- 260.Martín-Moreno AM, Reigada D, Ramírez BG, Mechoulam R, Innamorato N, Cuadrado A, et al. Cannabidiol and other cannabinoids reduce microglial activation in vitro and in vivo: relevance to Alzheimer’s disease. Mol Pharmacol. 2011;79(6):964–973. doi: 10.1124/mol.111.071290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Janefjord E, Mååg JLV, Harvey BS, Smid SD. Cannabinoid effects on β amyloid fibril and aggregate formation, neuronal and microglial-activated neurotoxicity in vitro. Cell Mol Neurobiol. 2014;34(1):31–42. doi: 10.1007/s10571-013-9984-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Binda KH, Real CC, Ferreira AFF, Britto LR, Chacur M. Antinociceptive effects of treadmill exercise in a rat model of Parkinson’s disease: the role of cannabinoid and opioid receptors. Brain Res. 2019:146521. 10.1016/j.brainres.2019.146521. [DOI] [PubMed]
- 263.Crivelaro do Nascimento G, Ferrari DP, Guimaraes FS, Del Bel EA, Bortolanza M, Ferreira-Junior NC. Cannabidiol increases the nociceptive threshold in a preclinical model of Parkinson’s disease. Neuropharmacology. 2020;163:107808. doi: 10.1016/j.neuropharm.2019.107808. [DOI] [PubMed] [Google Scholar]
- 264.Bisogno T, Hanuš L, De Petrocellis L, Tchilibon S, Ponde DE, Brandi I, et al. Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol. 2001;134(4):845–852. doi: 10.1038/sj.bjp.0704327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Zuardi A, Crippa J, Hallak J, Pinto J, Chagas M, Rodrigues G, et al. Cannabidiol for the treatment of psychosis in Parkinson’s disease. J Psychopharmacol. 2009;23(8):979–983. doi: 10.1177/0269881108096519. [DOI] [PubMed] [Google Scholar]
- 266.Chagas MHN, Zuardi AW, Tumas V, Pena-Pereira MA, Sobreira ET, Bergamaschi MM, et al. Effects of cannabidiol in the treatment of patients with Parkinson’s disease: an exploratory double-blind trial. J Psychopharmacol. 2014;28(11):1088–1098. doi: 10.1177/0269881114550355. [DOI] [PubMed] [Google Scholar]
- 267.Chagas MHN, Eckeli AL, Zuardi AW, Pena-Pereira MA, Sobreira-Neto MA, Sobreira ET, et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson’s disease patients: a case series. J Clin Pharm Ther. 2014;39(5):564–566. doi: 10.1111/jcpt.12179. [DOI] [PubMed] [Google Scholar]
- 268.Lotan I, Treves TA, Roditi Y, Djaldetti R. Cannabis (medical marijuana) treatment for motor and non-motor symptoms of Parkinson disease: an open-label observational study. Clin Neuropharmacol. 2014;37(2):41–44. doi: 10.1097/WNF.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 269.Kindred JH, Li K, Ketelhut NB, Proessl F, Fling BW, Honce JM, et al. Cannabis use in people with Parkinson’s disease and multiple sclerosis: a web-based investigation. Complement Ther Med. 2017;33:99–104. doi: 10.1016/j.ctim.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 270.Peball M, Werkmann M, Ellmerer P, Stolz R, Valent D, Knaus H-G, et al. Nabilone for non-motor symptoms of Parkinson’s disease: a randomized placebo-controlled, double-blind, parallel-group, enriched enrolment randomized withdrawal study (the NMS-Nab Study) J Neural Transm (Vienna) 2019;126(8):1061–1072. doi: 10.1007/s00702-019-02021-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Pertwee RG. Cannabinoids and multiple sclerosis. Pharmacol Ther. 2002;95(2):165–174. doi: 10.1016/s0163-7258(02)00255-3. [DOI] [PubMed] [Google Scholar]
- 272.Compston A, Coles A. Multiple sclerosis. Lancet (London, England) 2008;372(9648):1502–1517. doi: 10.1016/S0140-6736(08)61620-7. [DOI] [PubMed] [Google Scholar]
- 273.Nielsen S, Germanos R, Weier M, Pollard J, Degenhardt L, Hall W, et al. The use of cannabis and cannabinoids in treating symptoms of multiple sclerosis: a systematic review of reviews. Curr Neurol Neurosci Rep. 2018;18(2):8. doi: 10.1007/s11910-018-0814-x. [DOI] [PubMed] [Google Scholar]
- 274.Gaby A. Multiple sclerosis. Global Adv Health Med. 2013;2(1):50–56. doi: 10.7453/gahmj.2013.2.1.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Nicholas R, Rashid W. Multiple sclerosis. BMJ Clin Evid. 2012;2012:1202. [PMC free article] [PubMed]
- 276.Nicholas R, Rashid W. Multiple sclerosis. Am Fam Physician. 2013;87(10):712–714. [PubMed] [Google Scholar]
- 277.Uzunkopru C, Beckmann Y. Flammer syndrome in multiple sclerosis: diagnostics, prediction, and personalization of treatments. EPMA J. 2019;10(4):437–444. doi: 10.1007/s13167-019-00179-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Goncharenko V, Bubnov R, Polivka J, Jr, Zubor P, Biringer K, Bielik T, et al. Vaginal dryness: individualised patient profiles, risks and mitigating measures. EPMA J. 2019;10(1):73–79. doi: 10.1007/s13167-019-00164-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Golubnitschaja O, Flammer J. Individualised patient profile: clinical utility of Flammer syndrome phenotype and general lessons for predictive, preventive and personalised medicine. EPMA J. 2018;9(1):15–20. doi: 10.1007/s13167-018-0127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Cabranes A, Venderova K, de Lago E, Fezza F, Sanchez A, Mestre L, et al. Decreased endocannabinoid levels in the brain and beneficial effects of agents activating cannabinoid and/or vanilloid receptors in a rat model of multiple sclerosis. Neurobiol Dis. 2005;20(2):207–217. doi: 10.1016/j.nbd.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 281.Baker D, Pryce G, Croxford JL, Brown P, Pertwee RG, Makriyannis A, et al. Endocannabinoids control spasticity in a multiple sclerosis model. FASEB J. 2001;15(2):300–302. doi: 10.1096/fj.00-0399fje. [DOI] [PubMed] [Google Scholar]
- 282.Chiurchiù V, van der Stelt M, Centonze D, Maccarrone M. The endocannabinoid system and its therapeutic exploitation in multiple sclerosis: clues for other neuroinflammatory diseases. Prog Neurobiol. 2018;160:82–100. doi: 10.1016/j.pneurobio.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 283.Di Filippo M, Pini LA, Pelliccioli GP, Calabresi P, Sarchielli P. Abnormalities in the cerebrospinal fluid levels of endocannabinoids in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2008;79(11):1224–1229. doi: 10.1136/jnnp.2007.139071. [DOI] [PubMed] [Google Scholar]
- 284.Petro DJ, Ellenberger C., Jr Treatment of human spasticity with delta 9-tetrahydrocannabinol. J Clin Pharmacol. 1981;21(S1):413s–416s. doi: 10.1002/j.1552-4604.1981.tb02621.x. [DOI] [PubMed] [Google Scholar]
- 285.Ungerleider JT, Andrysiak T. Therapeutic issues of marijuana and THC (tetrahydrocannabinol) Int J Addict. 1985;20(5):691–699. doi: 10.3109/10826088509044289. [DOI] [PubMed] [Google Scholar]
- 286.Meinck HM, Schonle PW, Conrad B. Effect of cannabinoids on spasticity and ataxia in multiple sclerosis. J Neurol. 1989;236(2):120–122. doi: 10.1007/BF00314410. [DOI] [PubMed] [Google Scholar]
- 287.Clifford DB. Tetrahydrocannabinol for tremor in multiple sclerosis. Ann Neurol. 1983;13(6):669–671. doi: 10.1002/ana.410130616. [DOI] [PubMed] [Google Scholar]
- 288.Pryce G, Riddall DR, Selwood DL, Giovannoni G, Baker D. Neuroprotection in experimental autoimmune encephalomyelitis and progressive multiple sclerosis by cannabis-based cannabinoids. J Neuroimmune Pharmacol. 2015;10(2):281–292. doi: 10.1007/s11481-014-9575-8. [DOI] [PubMed] [Google Scholar]
- 289.Colizzi M, Bhattacharyya S. Does cannabis composition matter? Differential effects of delta-9-tetrahydrocannabinol and cannabidiol on human cognition. Curr Addict Rep. 2017;4(2):62–74. doi: 10.1007/s40429-017-0142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Rudroff T. Cannabis for neuropathic pain in multiple sclerosis-high expectations. Poor Data Front Pharmacol. 2019;10:1239. doi: 10.3389/fphar.2019.01239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Rudroff T, Honce JM. Cannabis and multiple sclerosis-the way forward. Front Neurol. 2017;8:299. doi: 10.3389/fneur.2017.00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Wilkinson JD, Whalley BJ, Baker D, Pryce G, Constanti A, Gibbons S, et al. Medicinal cannabis: is delta9-tetrahydrocannabinol necessary for all its effects? J Pharm Pharmacol. 2003;55(12):1687–1694. doi: 10.1211/0022357022304. [DOI] [PubMed] [Google Scholar]
- 293.Pryce G, Baker D. Control of spasticity in a multiple sclerosis model is mediated by CB1, not CB2, cannabinoid receptors. Br J Pharmacol. 2007;150(4):519–525. doi: 10.1038/sj.bjp.0707003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Perez J. Combined cannabinoid therapy via an oromucosal spray. Drugs Today (Barcelona, Spain : 1998) 2006;42(8):495–503. doi: 10.1358/dot.2006.42.8.1021517. [DOI] [PubMed] [Google Scholar]
- 295.Al-Ghezi ZZ, Miranda K, Nagarkatti M, Nagarkatti PS. Combination of cannabinoids, delta9-tetrahydrocannabinol and cannabidiol ameliorates experimental multiple sclerosis by suppressing neuroinflammation through regulation of miRNA-mediated signaling pathways. Front Immunol. 2019;10:1921. doi: 10.3389/fimmu.2019.01921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Meuth SG, Vila C, Dechant KL. Effect of Sativex on spasticity-associated symptoms in patients with multiple sclerosis. Expert Rev Neurother. 2015;15(8):909–918. doi: 10.1586/14737175.2015.1067607. [DOI] [PubMed] [Google Scholar]
- 297.Gado F, Digiacomo M, Macchia M, Bertini S, Manera C. Traditional uses of cannabinoids and new perspectives in the treatment of multiple sclerosis. Medicines (Basel, Switzerland). 2018;5(3). 10.3390/medicines5030091. [DOI] [PMC free article] [PubMed]
- 298.Svendsen KB, Jensen TS, Bach FW. Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised double blind placebo controlled crossover trial. BMJ (Clinical Research Ed) 2004;329(7460):253. doi: 10.1136/bmj.38149.566979.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Zajicek J, Fox P, Sanders H, Wright D, Vickery J, Nunn A, et al. Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet (London, England) 2003;362(9395):1517–1526. doi: 10.1016/S0140-6736(03)14738-1. [DOI] [PubMed] [Google Scholar]
- 300.Zajicek JP, Apostu VI. Role of cannabinoids in multiple sclerosis. CNS Drugs. 2011;25(3):187–201. doi: 10.2165/11539000-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 301.Wissel J, Haydn T, Muller J, Brenneis C, Berger T, Poewe W, et al. Low dose treatment with the synthetic cannabinoid nabilone significantly reduces spasticity-related pain : a double-blind placebo-controlled cross-over trial. J Neurol. 2006;253(10):1337–1341. doi: 10.1007/s00415-006-0218-8. [DOI] [PubMed] [Google Scholar]
- 302.Gehr S, Kaiser T, Kreutz R, Ludwig WD, Paul F. Suggestions for improving the design of clinical trials in multiple sclerosis-results of a systematic analysis of completed phase III trials. EPMA J. 2019;10(4):425–436. doi: 10.1007/s13167-019-00192-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Benito C, Nunez E, Tolon RM, Carrier EJ, Rabano A, Hillard CJ, et al. Cannabinoid CB2 receptors and fatty acid amide hydrolase are selectively overexpressed in neuritic plaque-associated glia in Alzheimer’s disease brains. J Neurosci. 2003;23(35):11136–11141. doi: 10.1523/JNEUROSCI.23-35-11136.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Piro JR, Benjamin DI, Duerr JM, Pi Y, Gonzales C, Wood KM, et al. A dysregulated endocannabinoid-eicosanoid network supports pathogenesis in a mouse model of Alzheimer’s disease. Cell Rep. 2012;1(6):617–623. doi: 10.1016/j.celrep.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Pazos MR, Nunez E, Benito C, Tolon RM, Romero J. Role of the endocannabinoid system in Alzheimer’s disease: new perspectives. Life Sci. 2004;75(16):1907–1915. doi: 10.1016/j.lfs.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 306.Mulder J, Zilberter M, Pasquare SJ, Alpar A, Schulte G, Ferreira SG, et al. Molecular reorganization of endocannabinoid signalling in Alzheimer’s disease. Brain. 2011;134(Pt 4):1041–1060. doi: 10.1093/brain/awr046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Koppel J, Davies P. Targeting the endocannabinoid system in Alzheimer’s disease. J Alzheimers Dis. 2008;15(3):495–504. doi: 10.3233/jad-2008-15315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Karl T, Cheng D, Garner B, Arnold JC. The therapeutic potential of the endocannabinoid system for Alzheimer’s disease. Expert Opin Ther Targets. 2012;16(4):407–420. doi: 10.1517/14728222.2012.671812. [DOI] [PubMed] [Google Scholar]
- 309.Fernandez-Ruiz J, Romero J, Ramos JA. Endocannabinoids and neurodegenerative disorders: Parkinson’s disease, Huntington’s chorea, Alzheimer’s disease, and others. Handb Exp Pharmacol. 2015;231:233–259. doi: 10.1007/978-3-319-20825-1_8. [DOI] [PubMed] [Google Scholar]
- 310.Campbell VA, Gowran A. Alzheimer’s disease; taking the edge off with cannabinoids? Br J Pharmacol. 2007;152(5):655–662. doi: 10.1038/sj.bjp.0707446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Benito C, Nunez E, Pazos MR, Tolon RM, Romero J. The endocannabinoid system and Alzheimer’s disease. Mol Neurobiol. 2007;36(1):75–81. doi: 10.1007/s12035-007-8006-8. [DOI] [PubMed] [Google Scholar]
- 312.Bedse G, Romano A, Lavecchia AM, Cassano T, Gaetani S. The role of endocannabinoid signaling in the molecular mechanisms of neurodegeneration in Alzheimer’s disease. J Alzheimers Dis. 2015;43(4):1115–1136. doi: 10.3233/JAD-141635. [DOI] [PubMed] [Google Scholar]
- 313.Aso E, Ferrer I. CB2 cannabinoid receptor as potential target against Alzheimer’s disease. Front Neurosci. 2016;10:243. doi: 10.3389/fnins.2016.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Talarico G, Trebbastoni A, Bruno G, de Lena C. Modulation of the cannabinoid system: a new perspective for the treatment of the Alzheimer’s disease. Curr Neuropharmacol. 2019;17(2):176–183. doi: 10.2174/1570159X16666180702144644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Ahmad R, Postnov A, Bormans G, Versijpt J, Vandenbulcke M, Van Laere K. Decreased in vivo availability of the cannabinoid type 2 receptor in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2016;43(12):2219–2227. doi: 10.1007/s00259-016-3457-7. [DOI] [PubMed] [Google Scholar]
- 316.Rodríguez-Cueto C, Benito C, Fernández-Ruiz J, Romero J, Hernández-Gálvez M, Gómez-Ruiz M. Changes in CB(1) and CB(2) receptors in the post-mortem cerebellum of humans affected by spinocerebellar ataxias. Br J Pharmacol. 2014;171(6):1472–1489. doi: 10.1111/bph.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Manuel I, González de San Román E, Giralt MT, Ferrer I, Rodríguez-Puertas R. Type-1 cannabinoid receptor activity during Alzheimer’s disease progression. J Alzheimers Dis. 2014;42(3):761–766. doi: 10.3233/JAD-140492. [DOI] [PubMed] [Google Scholar]
- 318.Di Marzo V, Stella N, Zimmer A. Endocannabinoid signalling and the deteriorating brain. Nat Rev Neurosci. 2015;16(1):30–42. doi: 10.1038/nrn3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Takkinen JS, López-Picón FR, Kirjavainen AK, Pihlaja R, Snellman A, Ishizu T, et al. [(18)F]FMPEP-d(2) PET imaging shows age- and genotype-dependent impairments in the availability of cannabinoid receptor 1 in a mouse model of Alzheimer’s disease. Neurobiol Aging. 2018;69:199–208. doi: 10.1016/j.neurobiolaging.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 320.Ahmad R, Goffin K, Van den Stock J, De Winter F-L, Cleeren E, Bormans G, et al. In vivo type 1 cannabinoid receptor availability in Alzheimer’s disease. Eur Neuropsychopharmacol. 2014;24(2):242–250. doi: 10.1016/j.euroneuro.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 321.Maccarrone M, Totaro A, Leuti A, Giacovazzo G, Scipioni L, Mango D, et al. Early alteration of distribution and activity of hippocampal type-1 cannabinoid receptor in Alzheimer’s disease-like mice overexpressing the human mutant amyloid precursor protein. Pharmacol Res. 2018;130:366–373. doi: 10.1016/j.phrs.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 322.Köfalvi A, Lemos C, Martín-Moreno AM, Pinheiro BS, García-García L, Pozo MA, et al. Stimulation of brain glucose uptake by cannabinoid CB2 receptors and its therapeutic potential in Alzheimer’s disease. Neuropharmacology. 2016;110(Pt A):519–529. doi: 10.1016/j.neuropharm.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 323.Pascual AC, Martín-Moreno AM, Giusto NM, de Ceballos ML, Pasquaré SJ. Normal aging in rats and pathological aging in human Alzheimer’s disease decrease FAAH activity: modulation by cannabinoid agonists. Exp Gerontol. 2014;60:92–99. doi: 10.1016/j.exger.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 324.Zhang J, Chen C. Alleviation of neuropathology by inhibition of monoacylglycerol lipase in APP transgenic mice lacking CB2 receptors. Mol Neurobiol. 2018;55(6):4802–4810. doi: 10.1007/s12035-017-0689-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Cassano T, Calcagnini S, Pace L, De Marco F, Romano A, Gaetani S. Cannabinoid receptor 2 signaling in neurodegenerative disorders: from pathogenesis to a promising therapeutic target. Front Neurosci. 2017;11:–30. 10.3389/fnins.2017.00030. [DOI] [PMC free article] [PubMed]
- 326.Jayant S, Sharma BM, Bansal R, Sharma B. Pharmacological benefits of selective modulation of cannabinoid receptor type 2 (CB2) in experimental Alzheimer’s disease. Pharmacol Biochem Behav. 2016;140:39–50. doi: 10.1016/j.pbb.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 327.Cheng D, Low JK, Logge W, Garner B, Karl T. Chronic cannabidiol treatment improves social and object recognition in double transgenic APPswe/PS1∆E9 mice. Psychopharmacology. 2014;231(15):3009–3017. doi: 10.1007/s00213-014-3478-5. [DOI] [PubMed] [Google Scholar]
- 328.Vallée A, Lecarpentier Y, Guillevin R, Vallée J-N. Effects of cannabidiol interactions with Wnt/β-catenin pathway and PPARγ on oxidative stress and neuroinflammation in Alzheimer’s disease. Acta Biochim Biophys Sin Shanghai. 2017;49(10):853–866. doi: 10.1093/abbs/gmx073. [DOI] [PubMed] [Google Scholar]
- 329.Karl T, Garner B, Cheng D. The therapeutic potential of the phytocannabinoid cannabidiol for Alzheimer’s disease. Behav Pharmacol. 2017;28(2 and 3-Spec Issue):142–160. doi: 10.1097/FBP.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 330.Wang L, Liu B-J, Cao Y, Xu W-Q, Sun D-S, Li M-Z, et al. Deletion of type-2 cannabinoid receptor induces Alzheimer’s disease-like tau pathology and memory impairment through AMPK/GSK3β pathway. Mol Neurobiol. 2018;55(6):4731–4744. doi: 10.1007/s12035-017-0676-2. [DOI] [PubMed] [Google Scholar]
- 331.Aso E, Andrés-Benito P, Carmona M, Maldonado R, Ferrer I. Cannabinoid receptor 2 participates in amyloid-β processing in a mouse model of Alzheimer’s disease but plays a minor role in the therapeutic properties of a cannabis-based medicine. J Alzheimers Dis. 2016;51(2):489–500. doi: 10.3233/JAD-150913. [DOI] [PubMed] [Google Scholar]
- 332.Schmöle A-C, Lundt R, Toporowski G, Hansen JN, Beins E, Halle A, et al. Cannabinoid receptor 2-deficiency ameliorates disease symptoms in a mouse model with Alzheimer’s disease-like pathology. J Alzheimers Dis. 2018;64(2):379–392. doi: 10.3233/JAD-180230. [DOI] [PubMed] [Google Scholar]
- 333.Zanettini C, Panlilio L, Aliczki M, Goldberg S, Haller J, Yasar S. Effects of endocannabinoid system modulation on cognitive and emotional behavior. Front Behav Neurosci. 2011;5(57). 10.3389/fnbeh.2011.00057. [DOI] [PMC free article] [PubMed]
- 334.Nadia S, Robert B. The chronic effects of cannabis on memory in humans: a review. Curr Drug Abuse Rev. 2008;1(1):81–98. doi: 10.2174/1874473710801010081. [DOI] [PubMed] [Google Scholar]
- 335.Bolla KI, Brown K, Eldreth D, Tate K, Cadet JL. Dose-related neurocognitive effects of marijuana use. Neurology. 2002;59(9):1337–1343. doi: 10.1212/01.wnl.0000031422.66442.49. [DOI] [PubMed] [Google Scholar]
- 336.Lundqvist T. Cognitive consequences of cannabis use: comparison with abuse of stimulants and heroin with regard to attention, memory and executive functions. Pharmacol Biochem Behav. 2005;81(2):319–330. doi: 10.1016/j.pbb.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 337.Fletcher JM, Page JB, Francis DJ, Copeland K, Naus MJ, Davis CM, et al. Cognitive correlates of long-term cannabis use in Costa Rican men. Arch Gen Psychiatry. 1996;53(11):1051–1057. doi: 10.1001/archpsyc.1996.01830110089011. [DOI] [PubMed] [Google Scholar]
- 338.Iversen L, Chapman V. Cannabinoids: a real prospect for pain relief? Curr Opin Pharmacol. 2002;2(1):50–55. doi: 10.1016/s1471-4892(01)00120-5. [DOI] [PubMed] [Google Scholar]
- 339.Calabrese EJ, Rubio-Casillas A. Biphasic effects of THC in memory and cognition. Eur J Clin Investig. 2018;48(5):e12920-e. doi: 10.1111/eci.12920. [DOI] [PubMed] [Google Scholar]
- 340.Jiang W, Zhang Y, Xiao L, Van Cleemput J, Ji S-P, Bai G, et al. Cannabinoids promote embryonic and adult hippocampus neurogenesis and produce anxiolytic- and antidepressant-like effects. J Clin Invest. 2005;115(11):3104–3116. doi: 10.1172/JCI25509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Assaf F, Fishbein M, Gafni M, Keren O, Sarne Y. Pre- and post-conditioning treatment with an ultra-low dose of Δ9-tetrahydrocannabinol (THC) protects against pentylenetetrazole (PTZ)-induced cognitive damage. Behav Brain Res. 2011;220(1):194–201. doi: 10.1016/j.bbr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 342.Bilkei-Gorzo A, Albayram O, Draffehn A, Michel K, Piyanova A, Oppenheimer H, et al. A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nat Med. 2017;23(6):782–787. doi: 10.1038/nm.4311. [DOI] [PubMed] [Google Scholar]
- 343.Sarne Y, Toledano R, Rachmany L, Sasson E, Doron R. Reversal of age-related cognitive impairments in mice by an extremely low dose of tetrahydrocannabinol. Neurobiol Aging. 2018;61:177–186. doi: 10.1016/j.neurobiolaging.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 344.Shelef A, Barak Y, Berger U, Paleacu D, Tadger S, Plopsky I, et al. Safety and efficacy of medical cannabis oil for behavioral and psychological symptoms of dementia: an-open label, add-on, pilot study. J Alzheimers Dis. 2016;51(1):15–19. doi: 10.3233/JAD-150915. [DOI] [PubMed] [Google Scholar]
- 345.van den Elsen GAH, Ahmed AIA, Lammers M, Kramers C, Verkes RJ, van der Marck MA, et al. Efficacy and safety of medical cannabinoids in older subjects: a systematic review. Ageing Res Rev. 2014;14:56–64. doi: 10.1016/j.arr.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 346.Liu CS, Chau SA, Ruthirakuhan M, Lanctôt KL, Herrmann N. Cannabinoids for the treatment of agitation and aggression in Alzheimer’s disease. CNS Drugs. 2015;29(8):615–623. doi: 10.1007/s40263-015-0270-y. [DOI] [PubMed] [Google Scholar]
- 347.Panza F, Solfrizzi V, Seripa D, Imbimbo BP, Santamato A, Lozupone M, et al. Progresses in treating agitation: a major clinical challenge in Alzheimer’s disease. Expert Opin Pharmacother. 2015;16(17):2581–2588. doi: 10.1517/14656566.2015.1092520. [DOI] [PubMed] [Google Scholar]
- 348.Porsteinsson AP, Antonsdottir IM. An update on the advancements in the treatment of agitation in Alzheimer’s disease. Expert Opin Pharmacother. 2017;18(6):611–620. doi: 10.1080/14656566.2017.1307340. [DOI] [PubMed] [Google Scholar]
- 349.Ruthirakuhan M, Lanctôt KL, Vieira D, Herrmann N. Natural and synthetic cannabinoids for agitation and aggression in Alzheimer’s disease: a meta-analysis. J Clin Psychiatry. 2019;80(2):18r12617. doi: 10.4088/JCP.18r12617. [DOI] [PubMed] [Google Scholar]
- 350.Ruthirakuhan MT, Herrmann N, Gallagher D, Andreazza AC, Kiss A, Verhoeff NPLG, et al. Investigating the safety and efficacy of nabilone for the treatment of agitation in patients with moderate-to-severe Alzheimer’s disease: study protocol for a cross-over randomized controlled trial. Contemp Clin Trials Commun. 2019;15:100385. doi: 10.1016/j.conctc.2019.100385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Zamberletti E, Rubino T, Parolaro D. The endocannabinoid system and schizophrenia: integration of evidence. Curr Pharm Des. 2012;18(32):4980–4990. doi: 10.2174/138161212802884744. [DOI] [PubMed] [Google Scholar]
- 352.Vigano D, Guidali C, Petrosino S, Realini N, Rubino T, Di Marzo V, et al. Involvement of the endocannabinoid system in phencyclidine-induced cognitive deficits modelling schizophrenia. Int J Neuropsychopharmacol. 2009;12(5):599–614. doi: 10.1017/S1461145708009371. [DOI] [PubMed] [Google Scholar]
- 353.Ujike H, Morita Y. New perspectives in the studies on endocannabinoid and cannabis: cannabinoid receptors and schizophrenia. J Pharmacol Sci. 2004;96(4):376–381. doi: 10.1254/jphs.fmj04003x4. [DOI] [PubMed] [Google Scholar]
- 354.Schwarcz G, Karajgi B, McCarthy R. Synthetic delta-9-tetrahydrocannabinol (dronabinol) can improve the symptoms of schizophrenia. J Clin Psychopharmacol. 2009;29(3):255–258. doi: 10.1097/JCP.0b013e3181a6bc3b. [DOI] [PubMed] [Google Scholar]
- 355.Muguruza C, Lehtonen M, Aaltonen N, Morentin B, Meana JJ, Callado LF. Quantification of endocannabinoids in postmortem brain of schizophrenic subjects. Schizophr Res. 2013;148(1–3):145–150. doi: 10.1016/j.schres.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 356.Koethe D, Llenos IC, Dulay JR, Hoyer C, Torrey EF, Leweke FM, et al. Expression of CB1 cannabinoid receptor in the anterior cingulate cortex in schizophrenia, bipolar disorder, and major depression. J Neural Transm (Vienna) 2007;114(8):1055–1063. doi: 10.1007/s00702-007-0660-5. [DOI] [PubMed] [Google Scholar]
- 357.Fernandez-Espejo E, Viveros MP, Nunez L, Ellenbroek BA, Rodriguez de Fonseca F. Role of cannabis and endocannabinoids in the genesis of schizophrenia. Psychopharmacology. 2009;206(4):531–549. doi: 10.1007/s00213-009-1612-6. [DOI] [PubMed] [Google Scholar]
- 358.De Marchi N, De Petrocellis L, Orlando P, Daniele F, Fezza F, Di Marzo V. Endocannabinoid signalling in the blood of patients with schizophrenia. Lipids Health Dis. 2003;2:5. doi: 10.1186/1476-511X-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Cohen M, Solowij N, Carr V. Cannabis, cannabinoids and schizophrenia: integration of the evidence. Aust N Z J Psychiatry. 2008;42(5):357–368. doi: 10.1080/00048670801961156. [DOI] [PubMed] [Google Scholar]
- 360.Chavarría-Siles I, Contreras-Rojas J, Hare E, Walss-Bass C, Quezada P, Dassori A, et al. Cannabinoid receptor 1 gene (CNR1) and susceptibility to a quantitative phenotype for hebephrenic schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2008;147(3):279–284. doi: 10.1002/ajmg.b.30592. [DOI] [PubMed] [Google Scholar]
- 361.Martínez-Gras I, Hoenicka J, Ponce G, Rodríguez–Jiménez R, Jiménez-Arriero MA, Pérez-Hernandez E et al. (AAT)n repeat in the cannabinoid receptor gene, CNR1: association with schizophrenia in a Spanish population. Eur Arch Psychiatry Clin Neurosci 2006;256(7):437–441. doi:10.1007/s00406-006-0665-3. [DOI] [PubMed]
- 362.Suárez-Pinilla P, Roiz-Santiañez R, Ortiz-García de la Foz V, Guest PC, Ayesa-Arriola R, Córdova-Palomera A, et al. Brain structural and clinical changes after first episode psychosis: focus on cannabinoid receptor 1 polymorphisms. Psychiatry Res Neuroimaging 2015;233(2):112–119. doi:10.1016/j.pscychresns.2015.05.005. [DOI] [PubMed]
- 363.Ujike H, Takaki M, Nakata K, Tanaka Y, Takeda T, Kodama M, et al. CNR1, central cannabinoid receptor gene, associated with susceptibility to hebephrenic schizophrenia. Mol Psychiatry. 2002;7(5):515–518. doi: 10.1038/sj.mp.4001029. [DOI] [PubMed] [Google Scholar]
- 364.Ho B-C, Wassink TH, Ziebell S, Andreasen NC. Cannabinoid receptor 1 gene polymorphisms and marijuana misuse interactions on white matter and cognitive deficits in schizophrenia. Schizophr Res. 2011;128(1):66–75. doi: 10.1016/j.schres.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Ishiguro H, Horiuchi Y, Ishikawa M, Koga M, Imai K, Suzuki Y, et al. Brain cannabinoid CB2 receptor in schizophrenia. Biol Psychiatry. 2010;67(10):974–982. doi: 10.1016/j.biopsych.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 366.Muller-Vahl KR. Treatment of Tourette syndrome with cannabinoids. Behav Neurol. 2013;27(1):119–124. doi: 10.3233/BEN-120276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Ceccarini J, De Hert M, van Winkel R, Koethe D, Bormans G, Leweke M, et al. In vivo pet imaging of cerebral type 1 cannabinoid receptor availability in patients with schizophrenia. Schizophr Res. 2010;117(2):170. [Google Scholar]
- 368.Dalton VS, Long LE, Weickert CS, Zavitsanou K. Paranoid schizophrenia is characterized by increased CB1 receptor binding in the dorsolateral prefrontal cortex. Neuropsychopharmacology. 2011;36(8):1620–1630. doi: 10.1038/npp.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Dean B, Sundram S, Bradbury R, Scarr E, Copolov D. Studies on [3H]CP-55940 binding in the human central nervous system: regional specific changes in density of cannabinoid-1 receptors associated with schizophrenia and cannabis use. Neuroscience. 2001;103(1):9–15. doi: 10.1016/s0306-4522(00)00552-2. [DOI] [PubMed] [Google Scholar]
- 370.Eggan SM, Stoyak SR, Verrico CD, Lewis DA. Cannabinoid CB1 receptor immunoreactivity in the prefrontal cortex: comparison of schizophrenia and major depressive disorder. Neuropsychopharmacology. 2010;35(10):2060–2071. doi: 10.1038/npp.2010.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Urigüen L, García-Fuster MJ, Callado LF, Morentin B, La Harpe R, Casadó V, et al. Immunodensity and mRNA expression of A2A adenosine, D2 dopamine, and CB1 cannabinoid receptors in postmortem frontal cortex of subjects with schizophrenia: effect of antipsychotic treatment. Psychopharmacology. 2009;206(2):313–324. doi: 10.1007/s00213-009-1608-2. [DOI] [PubMed] [Google Scholar]
- 372.Wong DF, Kuwabara H, Horti AG, Raymont V, Brasic J, Guevara M, et al. Quantification of cerebral cannabinoid receptors subtype 1 (CB1) in healthy subjects and schizophrenia by the novel PET radioligand [11C]OMAR. NeuroImage. 2010;52(4):1505–1513. doi: 10.1016/j.neuroimage.2010.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Zavitsanou K, Garrick T, Huang XF. Selective antagonist [3H]SR141716A binding to cannabinoid CB1 receptors is increased in the anterior cingulate cortex in schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry. 2004;28(2):355–360. doi: 10.1016/j.pnpbp.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 374.Reuter AR, Bumb JM, Mueller JK, Rohleder C, Pahlisch F, Hanke F, et al. Association of anandamide with altered binocular depth inversion illusion in schizophrenia. World J Biol Psychiatry. 2017;18(6):483–488. doi: 10.1080/15622975.2016.1246750. [DOI] [PubMed] [Google Scholar]
- 375.Pushpa-Rajah JA, McLoughlin BC, Gillies D, Rathbone J, Variend H, Kalakouti E, et al. Cannabis and schizophrenia. Schizophr Bull. 2015;41(2):336–337. doi: 10.1093/schbul/sbu168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Potvin S, Stip E, Lipp O, Roy M-A, Demers M-F, Bouchard R-H, et al. Anhedonia and social adaptation predict substance abuse evolution in dual diagnosis schizophrenia. Am J Drug Alcohol Abuse. 2008;34(1):75–82. doi: 10.1080/00952990701764631. [DOI] [PubMed] [Google Scholar]
- 377.Almeida V, Peres FF, Levin R, Suiama MA, Calzavara MB, Zuardi AW, et al. Effects of cannabinoid and vanilloid drugs on positive and negative-like symptoms on an animal model of schizophrenia: the SHR strain. Schizophr Res. 2014;153(1):150–159. doi: 10.1016/j.schres.2014.01.039. [DOI] [PubMed] [Google Scholar]
- 378.Levin R, Peres FF, Almeida V, Calzavara MB, Zuardi AW, Hallak JEC, et al. Effects of cannabinoid drugs on the deficit of prepulse inhibition of startle in an animal model of schizophrenia: the SHR strain. Front Pharmacol. 2014;5:10. doi: 10.3389/fphar.2014.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Malone DT, Taylor DA. The effect of Δ9-tetrahydrocannabinol on sensorimotor gating in socially isolated rats. Behav Brain Res. 2006;166(1):101–109. doi: 10.1016/j.bbr.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 380.Schneider M, Koch M. The cannabinoid agonist WIN 55,212-2 reduces sensorimotor gating and recognition memory in rats. Behav Pharmacol. 2002;13(1):29–37. doi: 10.1097/00008877-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 381.Wegener N, Kuhnert S, Thüns A, Roese R, Koch M. Effects of acute systemic and intra-cerebral stimulation of cannabinoid receptors on sensorimotor gating, locomotion and spatial memory in rats. Psychopharmacology. 2008;198(3):375. doi: 10.1007/s00213-008-1148-1. [DOI] [PubMed] [Google Scholar]
- 382.Ballmaier M, Bortolato M, Rizzetti C, Zoli M, Gessa G, Heinz A, et al. Cannabinoid receptor antagonists counteract sensorimotor gating deficits in the phencyclidine model of psychosis. Neuropsychopharmacology. 2007;32(10):2098–2107. doi: 10.1038/sj.npp.1301344. [DOI] [PubMed] [Google Scholar]
- 383.Raquel L, Valeria A, Fernanda Fiel P, Mariana Bendlin C, Neide Derci da S, Mayra Akimi S, et al. Antipsychotic profile of cannabidiol and rimonabant in an animal model of emotional context processing in schizophrenia. Curr Pharm Des. 2012;18(32):4960–4965. doi: 10.2174/138161212802884735. [DOI] [PubMed] [Google Scholar]
- 384.Campos AC, Rocha NP, Nicoli JR, Vieira LQ, Teixeira MM, Teixeira AL. Absence of gut microbiota influences lipopolysaccharide-induced behavioral changes in mice. Behav Brain Res. 2016;312:186–194. doi: 10.1016/j.bbr.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 385.Peres FF, Diana MC, Suiama MA, Justi V, Almeida V, Bressan RA, et al. Peripubertal treatment with cannabidiol prevents the emergence of psychosis in an animal model of schizophrenia. Schizophr Res. 2016;172(1):220–221. doi: 10.1016/j.schres.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 386.Zuardi AW, Morais SL, Guimarães FS, Mechoulam R. Antipsychotic effect of cannabidiol. J Clin Psychiatry. 1995;56(10):485–486. [PubMed] [Google Scholar]
- 387.Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2(3):e94-e. doi: 10.1038/tp.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Philip McGuire FRC, Robson P, Cubala WJ, Vasile D, Morrison PD, Barron R, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatr. 2018;175(3):225–231. doi: 10.1176/appi.ajp.2017.17030325. [DOI] [PubMed] [Google Scholar]
- 389.Amare AT, Schubert KO, Baune BT. Pharmacogenomics in the treatment of mood disorders: strategies and opportunities for personalized psychiatry. EPMA J. 2017;8(3):211–227. doi: 10.1007/s13167-017-0112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Lutz B. On-demand activation of the endocannabinoid system in the control of neuronal excitability and epileptiform seizures. Biochem Pharmacol. 2004;68(9):1691–1698. doi: 10.1016/j.bcp.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 391.Szaflarski JP, Bebin EM. Cannabis, cannabidiol, and epilepsy—from receptors to clinical response. Epilepsy Behav. 2014;41:277–282. doi: 10.1016/j.yebeh.2014.08.135. [DOI] [PubMed] [Google Scholar]
- 392.Ludanyi A, Eross L, Czirjak S, Vajda J, Halasz P, Watanabe M, et al. Downregulation of the CB1 cannabinoid receptor and related molecular elements of the endocannabinoid system in epileptic human hippocampus. J Neurosci. 2008;28(12):2976–2990. doi: 10.1523/JNEUROSCI.4465-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Goffin K, Van Paesschen W, Van Laere K. In vivo activation of endocannabinoid system in temporal lobe epilepsy with hippocampal sclerosis. Brain. 2011;134(Pt 4):1033–1040. doi: 10.1093/brain/awq385. [DOI] [PubMed] [Google Scholar]
- 394.von Rüden EL, Bogdanovic RM, Wotjak CT, Potschka H. Inhibition of monoacylglycerol lipase mediates a cannabinoid 1-receptor dependent delay of kindling progression in mice. Neurobiol Dis. 2015;77:238–245. doi: 10.1016/j.nbd.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 395.Terrone G, Pauletti A, Salamone A, Rizzi M, Villa BR, Porcu L, et al. Inhibition of monoacylglycerol lipase terminates diazepam-resistant status epilepticus in mice and its effects are potentiated by a ketogenic diet. Epilepsia. 2018;59(1):79–91. doi: 10.1111/epi.13950. [DOI] [PubMed] [Google Scholar]
- 396.Naziroglu M, Taner AN, Balbay E, Cig B. Inhibitions of anandamide transport and FAAH synthesis decrease apoptosis and oxidative stress through inhibition of TRPV1 channel in an in vitro seizure model. Mol Cell Biochem. 2018. 10.1007/s11010-018-3439-0. [DOI] [PubMed]
- 397.Colangeli R, Pierucci M, Benigno A, Campiani G, Butini S, Di Giovanni G. The FAAH inhibitor URB597 suppresses hippocampal maximal dentate afterdischarges and restores seizure-induced impairment of short and long-term synaptic plasticity. Sci Rep. 2017;7(1):11152. doi: 10.1038/s41598-017-11606-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Rainville P. Brain mechanisms of pain affect and pain modulation. Curr Opin Neurobiol. 2002;12(2):195–204. doi: 10.1016/s0959-4388(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 399.Woodhams SG, Sagar DR, Burston JJ, Chapman V. The role of the endocannabinoid system in pain. Handb Exp Pharmacol. 2015;227:119–143. doi: 10.1007/978-3-662-46450-2_7. [DOI] [PubMed] [Google Scholar]
- 400.Mallet C, Daulhac L, Bonnefont J, Ledent C, Etienne M, Chapuy E, et al. Endocannabinoid and serotonergic systems are needed for acetaminophen-induced analgesia. Pain. 2008;139(1):190–200. doi: 10.1016/j.pain.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 401.Kinsey SG, Long JZ, O’Neal ST, Abdullah RA, Poklis JL, Boger DL, et al. Blockade of endocannabinoid-degrading enzymes attenuates neuropathic pain. J Pharmacol Exp Ther. 2009;330(3):902–910. doi: 10.1124/jpet.109.155465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Guindon J, Beaulieu P. The role of the endogenous cannabinoid system in peripheral analgesia. Curr Mol Pharmacol. 2009;2(1):134–139. doi: 10.2174/1874467210902010134. [DOI] [PubMed] [Google Scholar]
- 403.Clapper JR, Moreno-Sanz G, Russo R, Guijarro A, Vacondio F, Duranti A, et al. Anandamide suppresses pain initiation through a peripheral endocannabinoid mechanism. Nat Neurosci. 2010;13(10):1265–1270. doi: 10.1038/nn.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Hohmann AG, Farthing JN, Zvonok AM, Makriyannis A. Selective activation of cannabinoid CB2 receptors suppresses hyperalgesia evoked by intradermal capsaicin. J Pharmacol Exp Ther. 2004;308(2):446–453. doi: 10.1124/jpet.103.060079. [DOI] [PubMed] [Google Scholar]
- 405.Malan TP, Jr, Ibrahim MM, Deng H, Liu Q, Mata HP, Vanderah T, et al. CB2 cannabinoid receptor-mediated peripheral antinociception. Pain. 2001;93(3):239–245. doi: 10.1016/S0304-3959(01)00321-9. [DOI] [PubMed] [Google Scholar]
- 406.Ibrahim MM, Deng H, Zvonok A, Cockayne DA, Kwan J, Mata HP, et al. Activation of CB2 cannabinoid receptors by AM1241 inhibits experimental neuropathic pain: pain inhibition by receptors not present in the CNS. Proc Natl Acad Sci U S A. 2003;100(18):10529–10533. doi: 10.1073/pnas.1834309100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Calignano A, La Rana G, Piomelli D. Antinociceptive activity of the endogenous fatty acid amide, palmitylethanolamide. Eur J Pharmacol. 2001;419(2–3):191–198. doi: 10.1016/s0014-2999(01)00988-8. [DOI] [PubMed] [Google Scholar]
- 408.Pertwee RG. Cannabinoid receptors and pain. Prog Neurobiol. 2001;63(5):569–611. doi: 10.1016/s0301-0082(00)00031-9. [DOI] [PubMed] [Google Scholar]
- 409.Hohmann AG. Spinal and peripheral mechanisms of cannabinoid antinociception: behavioral, neurophysiological and neuroanatomical perspectives. Chem Phys Lipids. 2002;121(1–2):173–190. doi: 10.1016/s0009-3084(02)00154-8. [DOI] [PubMed] [Google Scholar]
- 410.Walker JM, Hohmann AG. Cannabinoid mechanisms of pain suppression. Handb Exp Pharmacol. 2005;168:509–554. doi: 10.1007/3-540-26573-2_17. [DOI] [PubMed] [Google Scholar]
- 411.Rahn EJ, Makriyannis A, Hohmann AG. Activation of cannabinoid CB1 and CB2 receptors suppresses neuropathic nociception evoked by the chemotherapeutic agent vincristine in rats. Br J Pharmacol. 2007;152(5):765–777. doi: 10.1038/sj.bjp.0707333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Beltramo M, Bernardini N, Bertorelli R, Campanella M, Nicolussi E, Fredduzzi S, et al. CB2 receptor-mediated antihyperalgesia: possible direct involvement of neural mechanisms. Eur J Neurosci. 2006;23(6):1530–1538. doi: 10.1111/j.1460-9568.2006.04684.x. [DOI] [PubMed] [Google Scholar]
- 413.Khan SP, Pickens TA, Berlau DJ. Perspectives on cannabis as a substitute for opioid analgesics. Pain Manag. 2019;9(2):191–203. doi: 10.2217/pmt-2018-0051. [DOI] [PubMed] [Google Scholar]
- 414.Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014;82(17):1556–1563. doi: 10.1212/WNL.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–2473. doi: 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 416.Kim PS, Fishman MA. Cannabis for pain and headaches: primer. Curr Pain Headache Rep. 2017;21(4):19. doi: 10.1007/s11916-017-0619-7. [DOI] [PubMed] [Google Scholar]
- 417.NIDA. Marijuana. 2019. https://www.drugabuse.gov/publications/research-reports/marijuana. Accessed 22 November 2019.
- 418.NIDA. Marijuana as medicine. National Institute of Drug Abuse. 2019. https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine. Accessed 22 Novemeber, 2019 2019.
- 419.Grant I. Medical use of cannabinoids. JAMA. 2015;314(16):1750–1751. doi: 10.1001/jama.2015.11429. [DOI] [PubMed] [Google Scholar]
- 420.Weizman L, Dayan L, Brill S, Nahman-Averbuch H, Hendler T, Jacob G, et al. Cannabis analgesia in chronic neuropathic pain is associated with altered brain connectivity. Neurology. 2018;91(14):e1285–e1e94. doi: 10.1212/WNL.0000000000006293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.de Robles P, Fiest KM, Frolkis AD, Pringsheim T, Atta C, St Germaine-Smith C, et al. The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro Oncol. 2015;17(6):776–83. 10.1093/neuonc/nou283. [DOI] [PMC free article] [PubMed]
- 422.Hanif F, Muzaffar K, Perveen K, Malhi SM, Simjee SU. Glioblastoma multiforme: a review of its epidemiology and pathogenesis through clinical presentation and treatment. Asian Pac J Cancer Prev. 2017;18(1):3–9. doi: 10.22034/APJCP.2017.18.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Aldape K, Brindle KM, Chesler L, Chopra R, Gajjar A, Gilbert MR, et al. Challenges to curing primary brain tumours. Nat Rev Clin Oncol. 2019;16(8):509–520. doi: 10.1038/s41571-019-0177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Global, regional, and national burden of brain and other CNS cancer, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18(4):376–93. doi:10.1016/s1474-4422(18)30468-x. [DOI] [PMC free article] [PubMed]
- 425.Anjum K, Shagufta BI, Abbas SQ, Patel S, Khan I, Shah SAA, et al. Current status and future therapeutic perspectives of glioblastoma multiforme (GBM) therapy: a review. Biomed Pharmacother. 2017;92:681–689. doi: 10.1016/j.biopha.2017.05.125. [DOI] [PubMed] [Google Scholar]
- 426.Bifulco M, Di Marzo V. Targeting the endocannabinoid system in cancer therapy: a call for further research. Nat Med. 2002;8(6):547–550. doi: 10.1038/nm0602-547. [DOI] [PubMed] [Google Scholar]
- 427.Pertwee RG. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther. 1997;74(2):129–180. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- 428.Di Marzo V. ‘Endocannabinoids’ and other fatty acid derivatives with cannabimimetic properties: biochemistry and possible physiopathological relevance. Biochim Biophys Acta. 1998;1392(2–3):153–175. doi: 10.1016/s0005-2760(98)00042-3. [DOI] [PubMed] [Google Scholar]
- 429.Munson A, Harris L, Friedman M, Dewey W, Carchman RA. Antineoplastic activity of cannabinoids. J Natl Cancer Inst. 1975;55(3):597–602. doi: 10.1093/jnci/55.3.597. [DOI] [PubMed] [Google Scholar]
- 430.Guzmán M, Sánchez C, Galve-Roper Control of the cell survival/death decision by cannabinoids. J Mol Med (Berl) 2001;78(11):613–625. doi: 10.1007/s001090000177. [DOI] [PubMed] [Google Scholar]
- 431.Massi P, Vaccani A, Ceruti S, Colombo A, Abbracchio MP, Parolaro D. Antitumor effects of cannabidiol, a nonpsychoactive cannabinoid, on human glioma cell lines. J Pharmacol Exp Ther. 2004;308(3):838–845. doi: 10.1124/jpet.103.061002. [DOI] [PubMed] [Google Scholar]
- 432.Singer E, Judkins J, Salomonis N, Matlaf L, Soteropoulos P, McAllister S, et al. Reactive oxygen species-mediated therapeutic response and resistance in glioblastoma. Cell Death Dis. 2015;6:e1601. doi: 10.1038/cddis.2014.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Hermanson DJ, Marnett LJ. Cannabinoids, endocannabinoids, and cancer. Cancer Metastasis Rev. 2011;30(3–4):599–612. doi: 10.1007/s10555-011-9318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Galanti G, Fisher T, Kventsel I, Shoham J, Gallily R, Mechoulam R, et al. Delta 9-tetrahydrocannabinol inhibits cell cycle progression by downregulation of E2F1 in human glioblastoma multiforme cells. Acta Oncologica (Stockholm, Sweden) 2008;47(6):1062–1070. doi: 10.1080/02841860701678787. [DOI] [PubMed] [Google Scholar]
- 435.Hernandez-Tiedra S, Fabrias G, Davila D, Salanueva IJ, Casas J, Montes LR, et al. Dihydroceramide accumulation mediates cytotoxic autophagy of cancer cells via autolysosome destabilization. Autophagy. 2016;12(11):2213–2229. doi: 10.1080/15548627.2016.1213927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Galve-Roperh I, Sanchez C, Cortes ML, Gomez del Pulgar T, Izquierdo M, Guzman M. Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat Med. 2000;6(3):313–319. doi: 10.1038/73171. [DOI] [PubMed] [Google Scholar]
- 437.Lopez-Valero I, Torres S, Salazar-Roa M, Garcia-Taboada E, Hernandez-Tiedra S, Guzman M, et al. Optimization of a preclinical therapy of cannabinoids in combination with temozolomide against glioma. Biochem Pharmacol. 2018;157:275–284. doi: 10.1016/j.bcp.2018.08.023. [DOI] [PubMed] [Google Scholar]
- 438.Ellert-Miklaszewska A, Ciechomska I, Kaminska B. Cannabinoid signaling in glioma cells. Adv Exp Med Biol. 2013;986:209–220. doi: 10.1007/978-94-007-4719-7_11. [DOI] [PubMed] [Google Scholar]
- 439.Ellert-Miklaszewska A, Grajkowska W, Gabrusiewicz K, Kaminska B, Konarska L. Distinctive pattern of cannabinoid receptor type II (CB2) expression in adult and pediatric brain tumors. Brain Res. 2007;1137(1):161–169. doi: 10.1016/j.brainres.2006.12.060. [DOI] [PubMed] [Google Scholar]
- 440.Cioni C, Tassi M, Marotta G, Mugnaini C, Corelli F, Annunziata P. A novel highly selective cannabinoid CB2 agonist reduces in vitro growth and TGF-beta release of human glial cell tumors. Cent Nerv Syst Agents Med Chem. 2019;19(3):206–214. doi: 10.2174/1871524919666190923154351. [DOI] [PubMed] [Google Scholar]
- 441.Blazquez C, Casanova ML, Planas A, Gomez Del Pulgar T, Villanueva C, Fernandez-Acenero MJ, et al. Inhibition of tumor angiogenesis by cannabinoids. FASEB J. 2003;17(3):529–531. doi: 10.1096/fj.02-0795fje. [DOI] [PubMed] [Google Scholar]
- 442.Nabissi M, Morelli MB, Santoni M, Santoni G. Triggering of the TRPV2 channel by cannabidiol sensitizes glioblastoma cells to cytotoxic chemotherapeutic agents. Carcinogenesis. 2013;34(1):48–57. doi: 10.1093/carcin/bgs328. [DOI] [PubMed] [Google Scholar]
- 443.Nabissi M, Morelli MB, Amantini C, Farfariello V, Ricci-Vitiani L, Caprodossi S, et al. TRPV2 channel negatively controls glioma cell proliferation and resistance to Fas-induced apoptosis in ERK-dependent manner. Carcinogenesis. 2010;31(5):794–803. doi: 10.1093/carcin/bgq019. [DOI] [PubMed] [Google Scholar]
- 444.Likar R, Nahler G. The use of cannabis in supportive care and treatment of brain tumor. Neurooncol Pract. 2017;4(3):151–60. 10.1093/nop/npw027. [DOI] [PMC free article] [PubMed]
- 445.Taha T, Meiri D, Talhamy S, Wollner M, Peer A, Bar-Sela G. Cannabis impacts tumor response rate to nivolumab in patients with advanced malignancies. Oncologist. 2019;24(4):549–554. doi: 10.1634/theoncologist.2018-0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Likar R, Koestenberger M, Stultschnig M, Nahler G. Concomitant treatment of malignant brain tumours with CBD—a case series and review of the literature. Anticancer Res. 2019;39(10):5797–5801. doi: 10.21873/anticanres.13783. [DOI] [PubMed] [Google Scholar]
- 447.Warren PP, Bebin EM, Nabors LB, Szaflarski JP. The use of cannabidiol for seizure management in patients with brain tumor-related epilepsy. Neurocase. 2017;23(5–6):287–291. doi: 10.1080/13554794.2017.1391294. [DOI] [PubMed] [Google Scholar]
- 448.Cristino L, Bisogno T, Di Marzo V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat Rev Neurol. 2020;16(1):9–29. doi: 10.1038/s41582-019-0284-z. [DOI] [PubMed] [Google Scholar]
- 449.Dumitru CA, Sandalcioglu IE, Karsak M. Cannabinoids in glioblastoma therapy: new applications for old drugs. Front Mol Neurosci. 2018;11:159. doi: 10.3389/fnmol.2018.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Janssens JP, Schuster K, Voss A. Preventive, predictive, and personalized medicine for effective and affordable cancer care. EPMA J. 2018;9(2):113–123. doi: 10.1007/s13167-018-0130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Lu M, Zhan X. The crucial role of multiomic approach in cancer research and clinically relevant outcomes. EPMA J. 2018;9(1):77–102. doi: 10.1007/s13167-018-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Moris D, Georgopoulos S, Felekouras E, Patsouris E, Theocharis S. The effect of endocannabinoid system in ischemia-reperfusion injury: a friend or a foe? Expert Opin Ther Targets. 2015;19(9):1261–1275. doi: 10.1517/14728222.2015.1043268. [DOI] [PubMed] [Google Scholar]
- 453.Breivogel CS, Selley DE, Childers SR. Cannabinoid receptor agonist efficacy for stimulating [35S]GTPgammaS binding to rat cerebellar membranes correlates with agonist-induced decreases in GDP affinity. J Biol Chem. 1998;273(27):16865–16873. doi: 10.1074/jbc.273.27.16865. [DOI] [PubMed] [Google Scholar]
- 454.Mackie K, Devane WA, Hille B. Anandamide, an endogenous cannabinoid, inhibits calcium currents as a partial agonist in N18 neuroblastoma cells. Mol Pharmacol. 1993;44(3):498–503. [PubMed] [Google Scholar]
- 455.Kellogg R, Mackie K, Straiker A. Cannabinoid CB1 receptor-dependent long-term depression in autaptic excitatory neurons. J Neurophysiol. 2009;102(2):1160–1171. doi: 10.1152/jn.00266.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Straiker A, Mackie K. Depolarization-induced suppression of excitation in murine autaptic hippocampal neurones. J Physiol. 2005;569(Pt 2):501–517. doi: 10.1113/jphysiol.2005.091918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Kenakin T. Efficacy at G-protein-coupled receptors. Nat Rev Drug Discov. 2002;1(2):103–110. doi: 10.1038/nrd722. [DOI] [PubMed] [Google Scholar]
- 458.Kelley BG, Thayer SA. Delta 9-tetrahydrocannabinol antagonizes endocannabinoid modulation of synaptic transmission between hippocampal neurons in culture. Neuropharmacology. 2004;46(5):709–715. doi: 10.1016/j.neuropharm.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 459.van Amsterdam J, Brunt T, van den Brink W. The adverse health effects of synthetic cannabinoids with emphasis on psychosis-like effects. J Psychopharmacol. 2015;29(3):254–263. doi: 10.1177/0269881114565142. [DOI] [PubMed] [Google Scholar]
- 460.Huestis MA, Boyd SJ, Heishman SJ, Preston KL, Bonnet D, Le Fur G, et al. Single and multiple doses of rimonabant antagonize acute effects of smoked cannabis in male cannabis users. Psychopharmacology. 2007;194(4):505–515. doi: 10.1007/s00213-007-0861-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Tsou K, Patrick SL, Walker JM. Physical withdrawal in rats tolerant to delta 9-tetrahydrocannabinol precipitated by a cannabinoid receptor antagonist. Eur J Pharmacol. 1995;280(3):R13–R15. doi: 10.1016/0014-2999(95)00360-w. [DOI] [PubMed] [Google Scholar]
- 462.Cecyre B, Thomas S, Ptito M, Casanova C, Bouchard JF. Evaluation of the specificity of antibodies raised against cannabinoid receptor type 2 in the mouse retina. Naunyn Schmiedeberg's Arch Pharmacol. 2014;387(2):175–184. doi: 10.1007/s00210-013-0930-8. [DOI] [PubMed] [Google Scholar]
- 463.Callen L, Moreno E, Barroso-Chinea P, Moreno-Delgado D, Cortes A, Mallol J, et al. Cannabinoid receptors CB1 and CB2 form functional heteromers in brain. J Biol Chem. 2012;287(25):20851–20865. doi: 10.1074/jbc.M111.335273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Cristino L, Bisogno T, Di Marzo V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat Rev Neurol. 2019. 10.1038/s41582-019-0284-z. [DOI] [PubMed]
- 465.Lopez G. Marijuana is legal for medical purposes in 33 states. 2019. https://www.vox.com/identities/2018/8/20/17938366/medical-marijuana-legalization-states-map. Accessed 22 November, 2019 2019.
- 466.Corroon J, Felice JF. The endocannabinoid system and its modulation by cannabidiol (CBD) Altern Ther Health Med. 2019;25(S2):6–14. [PubMed] [Google Scholar]
- 467.Simmerman E, Qin X, Yu JC, Baban B. Cannabinoids as a potential new and novel treatment for melanoma: a pilot study in a murine model. J Surg Res. 2019;235:210–215. doi: 10.1016/j.jss.2018.08.055. [DOI] [PubMed] [Google Scholar]
- 468.Baban B, Hoda N, Malik A, Khodadadi H, Simmerman E, Vaibhav K, et al. Impact of cannabidiol treatment on regulatory T-17 cells and neutrophil polarization in acute kidney injury. Am J Physiol Ren Physiol. 2018;315(4):F1149–F1F58. doi: 10.1152/ajprenal.00112.2018. [DOI] [PubMed] [Google Scholar]
- 469.Wang J, Wang Y, Tong M, Pan H, Li D. Medical cannabinoids for cancer cachexia: a systematic review and meta-analysis. Biomed Res Int. 2019;2019:2864384. doi: 10.1155/2019/2864384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Thompson AE. JAMA Patient Page. Medical marijuana. JAMA. 2015;313(24):2508. doi: 10.1001/jama.2015.6676. [DOI] [PubMed] [Google Scholar]
- 471.Schatman ME. Medical use of cannabinoids. JAMA. 2015;314(16):1751. doi: 10.1001/jama.2015.11435. [DOI] [PubMed] [Google Scholar]
- 472.Hill KP, Hurley-Welljams-Dorof WM. Low to moderate quality evidence demonstrates the potential benefits and adverse events of cannabinoids for certain medical indications. Evid Based Med. 2016;21(1):17. doi: 10.1136/ebmed-2015-110264. [DOI] [PubMed] [Google Scholar]
- 473.Golubnitschaja O, Costigliola V. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2012;3(1):14. doi: 10.1186/1878-5085-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Xi ZX, Peng XQ, Li X, Song R, Zhang HY, Liu QR, et al. Brain cannabinoid CB(2) receptors modulate cocaine's actions in mice. Nat Neurosci. 2011;14(9):1160–1166. doi: 10.1038/nn.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Pertwee RG. Emerging strategies for exploiting cannabinoid receptor agonists as medicines. Br J Pharmacol. 2009;156(3):397–411. doi: 10.1111/j.1476-5381.2008.00048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Kaplan L, Klein T, Wilson M, Graves J. Knowledge, practices, and attitudes of Washington State health care professionals regarding medical cannabis. Cannabis Cannabinoid Res. 2019. 10.1089/can.2019.0051. [DOI] [PMC free article] [PubMed]
- 477.Goldenberg M, Reid MW, IsHak WW, Danovitch I. The impact of cannabis and cannabinoids for medical conditions on health-related quality of life: a systematic review and meta-analysis. Drug Alcohol Depend. 2017;174:80–90. doi: 10.1016/j.drugalcdep.2016.12.030. [DOI] [PubMed] [Google Scholar]
- 478.Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Bouaboula M, Poinot-Chazel C, Marchand J, Canat X, Bourrie B, Rinaldi-Carmona M, et al. Signaling pathway associated with stimulation of CB2 peripheral cannabinoid receptor. Involvement of both mitogen-activated protein kinase and induction of Krox-24 expression. Eur J Biochem. 1996;237(3):704–711. doi: 10.1111/j.1432-1033.1996.0704p.x. [DOI] [PubMed] [Google Scholar]
- 480.Bouaboula M, Desnoyer N, Carayon P, Combes T, Casellas P. Gi protein modulation induced by a selective inverse agonist for the peripheral cannabinoid receptor CB2: implication for intracellular signalization cross-regulation. Mol Pharmacol. 1999;55(3):473–480. [PubMed] [Google Scholar]
- 481.Devane WA, Dysarz FA, 3rd, Johnson MR, Melvin LS, Howlett AC. Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol. 1988;34(5):605–613. [PubMed] [Google Scholar]
- 482.Bonner TI. Molecular biology of cannabinoid receptors. J. Neuroimmunol. 1996;69(1–2):15–7.
- 483.Reggio PH. Endocannabinoid binding to the cannabinoid receptors: what is known and what remains unknown. Curr Med Chem. 2010;17(14):1468–1486. doi: 10.2174/092986710790980005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Svizenska I, Dubovy P, Sulcova A. Cannabinoid receptors 1 and 2 (CB1 and CB2), their distribution, ligands and functional involvement in nervous system structures—a short review. Pharmacol Biochem Behav. 2008;90(4):501–511. doi: 10.1016/j.pbb.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 485.Onaivi ES, Ishiguro H, Gong J-P, Patel S, Perchuk A, Meozzi PA, et al. Discovery of the presence and functional expression of cannabinoid CB2 receptors in brain. Ann N Y Acad Sci. 2006;1074(1):514–536. doi: 10.1196/annals.1369.052. [DOI] [PubMed] [Google Scholar]
- 486.Gong JP, Onaivi ES, Ishiguro H, Liu QR, Tagliaferro PA, Brusco A, et al. Cannabinoid CB2 receptors: immunohistochemical localization in rat brain. Brain Res. 2006;1071(1):10–23. doi: 10.1016/j.brainres.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 487.Ishiguro H, Horiuchi Y, Ishikawa M, Koga M, Imai K, Suzuki Y, et al. Brain cannabinoid CB2 receptor in schizophrenia. Biol Psychiatry. 2010;67(10):974–982. doi: 10.1016/j.biopsych.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 488.Devane W, Hanus L, Breuer A, Pertwee R, Stevenson L, Griffin G, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science (New York, NY) 1992;258(5090):1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 489.Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, et al. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev. 2002;54(2):161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- 490.Pertwee RG. Pharmacology of cannabinoid receptor ligands. Curr Med Chem. 1999;6(8):635–664. [PubMed] [Google Scholar]
- 491.Ross RA, Gibson TM, Brockie HC, Leslie M, Pashmi G, Craib SJ, et al. Structure-activity relationship for the endogenous cannabinoid, anandamide, and certain of its analogues at vanilloid receptors in transfected cells and vas deferens. Br J Pharmacol. 2001;132(3):631–640. doi: 10.1038/sj.bjp.0703850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Sugiura T, Waku K. 2-Arachidonoylglycerol and the cannabinoid receptors. Chem Phys Lipids. 2000;108(1–2):89–106. doi: 10.1016/s0009-3084(00)00189-4. [DOI] [PubMed] [Google Scholar]
- 493.Childers SR, Breivogel CS. Cannabis and endogenous cannabinoid systems. Drug Alcohol Depend. 1998;51(1–2):173–187. doi: 10.1016/s0376-8716(98)00075-1. [DOI] [PubMed] [Google Scholar]
- 494.Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50(1):83–90. doi: 10.1016/0006-2952(95)00109-d. [DOI] [PubMed] [Google Scholar]
- 495.Sugiura T, Kodaka T, Nakane S, Miyashita T, Kondo S, Suhara Y, et al. Evidence that the cannabinoid CB1 receptor is a 2-arachidonoylglycerol receptor. Structure-activity relationship of 2-arachidonoylglycerol, ether-linked analogues, and related compounds. J Biol Chem. 1999;274(5):2794–2801. doi: 10.1074/jbc.274.5.2794. [DOI] [PubMed] [Google Scholar]
- 496.Sugiura T, Kondo S, Sukagawa A, Nakane S, Shinoda A, Itoh K, et al. 2-Arachidonoylgylcerol: a possible endogenous cannabinoid receptor ligand in brain. Biochem Biophys Res Commun. 1995;215(1):89–97. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- 497.Huffman JW, Liddle J, Yu S, Aung MM, Abood ME, Wiley JL, et al. 3-(1′,1′-Dimethylbutyl)-1-deoxy-delta8-THC and related compounds: synthesis of selective ligands for the CB2 receptor. Bioorg Med Chem. 1999;7(12):2905–2914. doi: 10.1016/s0968-0896(99)00219-9. [DOI] [PubMed] [Google Scholar]
- 498.Huffman JW, Bushell SM, Miller JR, Wiley JL, Martin BR. 1-Methoxy-, 1-deoxy-11-hydroxy- and 11-hydroxy-1-methoxy-Delta(8)-tetrahydrocannabinols: new selective ligands for the CB2 receptor. Bioorg Med Chem. 2002;10(12):4119–4129. doi: 10.1016/s0968-0896(02)00331-0. [DOI] [PubMed] [Google Scholar]
- 499.Felder CC, Joyce KE, Briley EM, Mansouri J, Mackie K, Blond O, et al. Comparison of the pharmacology and signal transduction of the human cannabinoid CB1 and CB2 receptors. Mol Pharmacol. 1995;48(3):443–450. [PubMed] [Google Scholar]
- 500.Oka S, Wakui J, Ikeda S, Yanagimoto S, Kishimoto S, Gokoh M, et al. Involvement of the cannabinoid CB2 receptor and its endogenous ligand 2-arachidonoylglycerol in oxazolone-induced contact dermatitis in mice. J Immunol (Baltimore, MD : 1950) 2006;177(12):8796–8805. doi: 10.4049/jimmunol.177.12.8796. [DOI] [PubMed] [Google Scholar]
- 501.Sugiura T, Kondo S, Kishimoto S, Miyashita T, Nakane S, Kodaka T, et al. Evidence that 2-arachidonoylglycerol but not N-palmitoylethanolamine or anandamide is the physiological ligand for the cannabinoid CB2 receptor. Comparison of the agonistic activities of various cannabinoid receptor ligands in HL-60 cells. J Biol Chem. 2000;275(1):605–612. doi: 10.1074/jbc.275.1.605. [DOI] [PubMed] [Google Scholar]
- 502.Maldonado R, Valverde O, Berrendero F. Involvement of the endocannabinoid system in drug addiction. Trends Neurosci. 2006;29(4):225–232. doi: 10.1016/j.tins.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 503.Pan X, Ikeda SR, Lewis DL. Rat brain cannabinoid receptor modulates N-type Ca2+ channels in a neuronal expression system. Mol Pharmacol. 1996;49(4):707–714. [PubMed] [Google Scholar]
- 504.Gelfand EV, Cannon CP. Rimonabant: a cannabinoid receptor type 1 blocker for management of multiple cardiometabolic risk factors. J Am Coll Cardiol. 2006;47(10):1919–1926. doi: 10.1016/j.jacc.2005.12.067. [DOI] [PubMed] [Google Scholar]
- 505.Cota D, Marsicano G, Tschop M, Grubler Y, Flachskamm C, Schubert M, et al. The endogenous cannabinoid system affects energy balance via central orexigenic drive and peripheral lipogenesis. J Clin Invest. 2003;112(3):423–431. doi: 10.1172/JCI17725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Pagotto U, Pasquali R. Fighting obesity and associated risk factors by antagonising cannabinoid type 1 receptors. Lancet (London, England) 2005;365(9468):1363–1364. doi: 10.1016/S0140-6736(05)66348-9. [DOI] [PubMed] [Google Scholar]
- 507.Toguri JT, Moxsom R, Szczesniak AM, Zhou J, Kelly ME, Lehmann C. Cannabinoid 2 receptor activation reduces leukocyte adhesion and improves capillary perfusion in the iridial microvasculature during systemic inflammation. Clin Hemorheol Microcirc. 2015;61(2):237–249. doi: 10.3233/CH-151996. [DOI] [PubMed] [Google Scholar]
- 508.Rom S, Zuluaga-Ramirez V, Dykstra H, Reichenbach NL, Pacher P, Persidsky Y. Selective activation of cannabinoid receptor 2 in leukocytes suppresses their engagement of the brain endothelium and protects the blood-brain barrier. Am J Pathol. 2013;183(5):1548–1558. doi: 10.1016/j.ajpath.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.Zhao Y, Yuan Z, Liu Y, Xue J, Tian Y, Liu W, et al. Activation of cannabinoid CB2 receptor ameliorates atherosclerosis associated with suppression of adhesion molecules. J Cardiovasc Pharmacol. 2010;55(3):292–298. doi: 10.1097/FJC.0b013e3181d2644d. [DOI] [PubMed] [Google Scholar]
- 510.Fujii M, Sherchan P, Soejima Y, Doycheva D, Zhao D, Zhang JH. Cannabinoid receptor type 2 agonist attenuates acute neurogenic pulmonary edema by preventing neutrophil migration after subarachnoid hemorrhage in rats. Acta Neurochir Suppl. 2016;121:135–139. doi: 10.1007/978-3-319-18497-5_24. [DOI] [PubMed] [Google Scholar]
- 511.Braun M, Khan ZT, Khan MB, Kumar M, Ward A, Achyut BR, et al. Selective activation of cannabinoid receptor-2 reduces neuroinflammation after traumatic brain injury via alternative macrophage polarization. Brain Behav Immun. 2018;68:224–237. doi: 10.1016/j.bbi.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Gentili M, Ronchetti S, Ricci E, Di Paola R, Gugliandolo E, Cuzzocrea S, et al. Selective CB2 inverse agonist JTE907 drives T cell differentiation towards a Treg cell phenotype and ameliorates inflammation in a mouse model of inflammatory bowel disease. Pharmacol Res. 2019;141:21–31. doi: 10.1016/j.phrs.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 513.Kong W, Li H, Tuma RF, Ganea D. Selective CB2 receptor activation ameliorates EAE by reducing Th17 differentiation and immune cell accumulation in the CNS. Cell Immunol. 2014;287(1):1–17. doi: 10.1016/j.cellimm.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 514.Hasko J, Fazakas C, Molnar J, Nyul-Toth A, Herman H, Hermenean A, et al. CB2 receptor activation inhibits melanoma cell transmigration through the blood-brain barrier. Int J Mol Sci. 2014;15(5):8063–8074. doi: 10.3390/ijms15058063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 515.Sanchez MG, Ruiz-Llorente L, Sanchez AM, Diaz-Laviada I. Activation of phosphoinositide 3-kinase/PKB pathway by CB(1) and CB(2) cannabinoid receptors expressed in prostate PC-3 cells. Involvement in Raf-1 stimulation and NGF induction. Cell Signal. 2003;15(9):851–859. doi: 10.1016/s0898-6568(03)00036-6. [DOI] [PubMed] [Google Scholar]
- 516.Guzman M, Galve-Roperh I, Sanchez C. Ceramide: a new second messenger of cannabinoid action. Trends Pharmacol Sci. 2001;22(1):19–22. doi: 10.1016/s0165-6147(00)01586-8. [DOI] [PubMed] [Google Scholar]