Abstract
Objectives:
Previous research has shown that balance and gait difficulties are predictors of falls. The aim of this study was to evaluate the predictive validity of two tools reporting on balance and gait among older community-living adults independent in personal activities of daily living (p-ADL).
Methods:
Prospective study design. Baseline assessment included the Timed Up and Go test (TUG) and the Short Physical Performance Battery (SPPB). Following baseline, falls were recorded monthly for one year by 202 participants (70.1% women) who were independent in p-ADL, and at least 75 years old (79.2±3.5). ROC-curves were made and AUC were calculated.
Results:
Forty-seven percent of the participants reported falls. AUCs calculated for TUG were 0.5 (95%CI: 0.5-0.6) for those with at least one fall, and 0.5 (95% CI: 0.5-0.6) for recurrent fallers. Corresponding figures for SPPB were 0.5 (95% CI: 0.5-0.6) and 0.5 (95% CI: 0.5-0.6).
Conclusion:
This study does not support a recommendation to use the Timed Up and Go test or the Short Physical Performance Battery as tools for the identification of fall-prone persons among older adults living in the community. These results reinforce the need for further research into appropriate tools for identifying independent but fall-prone older adults.
Keywords: Accidental falls, Aged, Functional ability, Geriatric assessment/methods, Postural balance
Introduction
Falls are the most common cause of injury in old age[1-3]. In addition to fractures and other fall-related injuries, falls may lead to loss of balance confidence and social restrictions[4]. The cause of falls is multifaceted, based on both personal, environmental, and activity-related factors. Problems with balance and gait are frequently documented risk factors for falls[5], but it is still unclear what measurements to use in different populations for the purpose of fall prediction. Consequently, the choice of tools is often guided by the ease of use for clinicians and older adults instead of by adequate measurement properties. Therefore, evaluating measurements tools, which can be of help in the decision to whom fall preventive measures should be recommended, still remains an important issue in fall prevention.
Well-functioning older adults living in the community are often overlooked regarding fall prevention, however, they are also prone to falls[6,7]. Multifactorial interventions have been shown to decrease risk factors associated with falls, reduce admission to hospital and nursing homes, and preserve and improve physical function in community living older adults[8]. However, in a meta-analysis, neither multifactorial nor multicomponent interventions presented strong evidence for improving fall-related outcomes[9]. Interestingly, other meta-analyses have shown that exercise interventions, as a single intervention, reduce fall rates by more than 20%, up to 39% among community-living older adults[10,11]. The use of assessment tools with good predictive validity could facilitate onset of interventions at an early stage.
The Timed Up and Go (TUG) test and the Short Physical Performance Battery (SPPB) are well established clinical tests of balance and functional performance in older adults. TUG is a timed movement sequence including rising, walking and turning as a measure of basic mobility[12], and the SPPB is a summary score of balance, walking speed and chair stand-test[13]. Both tests appear frequently in the literature, have been evaluated, and are easy to use. However, literature reviews and meta-analyses have not been able to draw strong conclusions regarding the predictive validity of TUG in community living older adults[14-16]. There are some indications that the test might be more suitable in less healthy and less well-functioning older adults[15]. There is an ongoing discussion regarding recommendations of what cut-off scores to use when differentiating a high- risk from a low-risk of falling in community-living older adults[15,16]. The SPPB has excellent psychometric properties for test-retest reliability and concurrent validity regarding ADL disability, mobility, muscle strength and quality of life as well as for predictive validity regarding ADL disability, walking difficulties and mortality in community-dwelling older adults[17]. But few studies have studied the SPPB’s predictive validity of falls[17,18]. So far, studies using a prospective research design indicate that the SPPB does not predict a future fall[19,20]. Despite measuring frequently mentioned mobility risk-factors for falls among older adults, the predictive abilities of these tools thus remain inconclusive.
The aim of this study was, therefore, to evaluate the predictive validity of the Timed Up and Go (TUG) test and the Short Physical Performance Battery (SPPB) among independent older adults (aged 75 years and over) living in the community.
Materials and methods
The study had a prospective study design including a baseline assessment and a 1-year follow-up of falls. The participants comprised a cohort of 202 individuals selected from a previous study[21]. They were recruited through senior citizens organisations, advertisement in the local press, and through primary care. Inclusion criteria in the present study were: age (75 years or older), community living, a score ≥24 on the Mini Mental State Examination test (MMSE)[22], a score of 7 or higher on the SPPB[13], a time below 15 seconds in the TUG-test[12], and a score of 19 or 20 on the Barthel Index of Activities of Daily Living (p-ADL)[23]. Twenty is the maximum possible score. In this study, a score of 19 or 20 was regarded as independent in p-ADL. The study was approved by the Regional Ethics Committee in Umea, (04-071M) and all participants provided informed written consent for participation.
The baseline assessments included the Timed Up and Go test and the Short Physical Performance Battery. In the TUG test, the participants were asked to stand up from a chair, walk and cross a 3 meter mark on the floor with normal pace, then turn, walk back to the chair and sit down[12]. The timing was performed from the moment the participants back left the back of the chair to their buttocks touched the seating again[24]. The participants were allowed to practice once before two timed trials were performed. The second timed trial was analysed in this study.
The Short Physical Performance Battery (SPPB)[13] is comprised of three parts: gait speed, standing balance and lower limb muscle strength. Each item is timed and transferred to a score from zero to four and can provide a total score of 12 points. Gait speed was timed as the participant walked three meters with normal pace; the faster of two attempts were registered. The standing balance was assessed in three positions: side-by-side, semi-tandem and tandem stance. The positions were to be maintained for 10 seconds if possible. Muscle strength in the lower limbs was evaluated through a timed sit-to-stand action, performed repeatedly five times, arms held over the chest.
Other assessments at baseline were performed for descriptive purposes. The MMSE[22] was used for screening of cognitive difficulties and the Barthel Index[23] for dependence in activities of daily living. Visual acuity was assessed by reading a chart of letters from a distance of three meters[25]. Frändin-Grimby activity scale[26] was used to assess self-reported level of physical activity. The scale ranges from 0-6 and includes household activities. A score of 4 means doing either moderate physical activity 1-2 hours per week (such as jogging, swimming, gymnastics, harder gardening, cooking at home), or light physical activity more than 4 hours per week (domestic work, light as well as heavy). Use of assistive devices, medical diagnoses, perceived health, and prescribed drugs were also collected.
All participants were followed up regarding falls from their baseline assessments for one year. They maintained a journal to record daily whether they had fallen which they sent to the research team on a monthly basis. A fall was defined as “an event in which the participant unintentionally came to rest on the floor or ground, regardless of the cause and regardless of the consequences of the fall”. The participants were phoned for a structured interview when a fall was reported or as a reminder when the journal had not been received at the expected time.
Analyses
For descriptive purposes we used Spearman’s Rank Order Correlation to assess relation between frequency of falls over one year and time performing TUG, and score of SPPB. To assess the predictive accuracy, Receiver Operating Characteristics (ROC) Curves where constructed for TUG and SPPB regarding participants with at least one fall compared to no fall, and with recurrent falls (at least two falls) compared to no or a single fall. Areas Under Curve (AUC) were also calculated. An AUC value of 0.5 or lower is considered no better than chance to predict outcome. A value of acceptable discrimination is between 0.7 and 0.8, and higher is seen as excellent or outstanding[27]. All analyses were performed in the Statistical Package for the Social Sciences (SPSS) version 25.0.
Results
Baseline characteristics of the participants are presented in [Table 1a-b]. Participants’ mean age was 79 years, 71% were women, and 1.5% received home help service. They had a TUG performance of mean 9.5±1.7, and scored an SPPB mean 10.7±1.4. 185 of the 202 participants achieved a full score of the Barthel Index. The remaining 17 participants did not achieve a full score because of either incontinence (n=15) or that they needed help when ascending and/or descending stairs (n=1) or bathing (n=1). The median activity level according to Frändin-Grimby activity scale was 4 among both men and women. Out of the 202 participants, 95 participants (47.0%) fell at least once and 50 (24.8%) fell recurrently.
Table 1.
Baseline descriptive characteristics of the 202 participants.
| Men (n=59) | Women (n=143) | All (n=202) | |
|---|---|---|---|
| Age, years, mean ± SD | 79.2±4.0 | 79.2±3.2 | 79.2±3.5 |
| Educational level, n (%) | |||
| <6 years | 17(28.8) | 43(30.1) | 60(29.7) |
| 7-9 years | 16(27.1) | 44(30.8) | 60(29.7) |
| ≥10 years | 25(42.4) | 55(38.5) | 80(39.6) |
| Home help service, n (%) | |||
| Yes | 1(1.7) | 2(1.4) | 3(1.5) |
| No | 58(98.3) | 141(98.6) | 199(98.5) |
| Physical activity level | |||
| Frändin-Grimby Scale, median (Q1-Q3) | 4.0(3-4) | 4.0(3.75-4.0) | 4.0(3-4) |
| Measures of function | |||
| Mini Mental State Examination (MMSE), mean ± SD | 27.7±1.7 | 27.8±1.8 | 27.8±1.8 |
| Visual acuity with glasses, n (%) | |||
| Excellent/ good | 43(72.9) | 103(72.0) | 146(72.3) |
| Fair/poor | 16(27.1) | 38(26.6) | 54(26.7) |
| Barthel Index, mean ± SD | 20.0±0.2 | 19.9±0.3 | 19.9±0.3 |
| Timed Up and Go (TUG), seconds | 9.3±1.6 | 9.5±1.8 | 9.5±1.7 |
| Short Physical Performance Battery (SPPB), score | 10.8±1.4 | 10.6±1.4 | 10.7±1.4 |
| History of falls in previous year, n (%) | |||
| No falls | 23(39.0) | 72(50.3) | 95(47.0) |
| One fall | 23(39.0) | 49(34.3) | 72(35.6) |
| ≥2 falls | 13(22.0) | 22(15.4) | 35(17.3) |
| Medical Diagnosis, n (%) | |||
| High blood pressure | 20(33.9) | 77(53.8) | 97(48.0) |
| Heart disease | 20(33.9) | 22(15.4) | 42(20.8) |
| Pulmonary disease | 4(6.8) | 14(9.8) | 18(8.9) |
| Stroke | 11(18.6) | 12(8.4) | 23(11.4) |
| Transient Ischemic Attack | 2(3.4) | 7(4.9) | 9(4.5) |
| Rheumatic disease | 3(5.1) | 9(6.3) | 12(5.9) |
| Number of prescribed medications, mean | 3.2±2.5 | 3.3±2.4 | 3.3±2.5 |
| Body Mass Index (BMI), mean ± SD | 25.5±2.8 | 26.7±4.0 | 26.3±3.7 |
| Self-rated health, n (%) | |||
| Excellent | 1(1.7) | 7(4.9) | 8(4.0) |
| Very good | 28(47.5) | 31(21.7) | 59(29.2) |
| Good | 24(40.7) | 80(55.9) | 104(51.5) |
| Fair | 6(10.2) | 24(16.8) | 30(14.9) |
| Poor | 0 | 1(0.7) | 1(0.5) |
No relationship could be found between number of falls per person (0-5 or more) during one year and TUG, or SPPB (r=0.055, p=0.44 and r=0.076, p=0.28, respectively), (Figure 1a and 1b).
Figure 1.
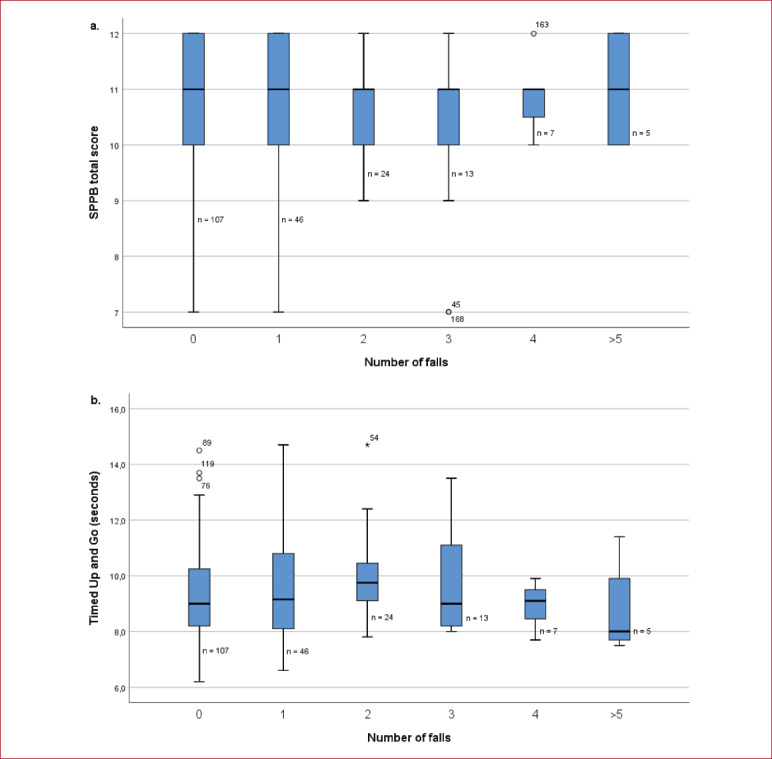
Boxplots representing the distribution of number of falls per person during one year according to test score in a. the Times Up and Go test and b. Short Physical Performance Battery.
Neither TUG nor SPPB were associated with future risk of falling, (Figures 2a-b and 3a-b). AUCs calculated for TUG were 0.5 (95% CI: 0.5-0.6) for those who fell at least once and 0.5 (95% CI: 0.5-0.6) for recurrent fallers. Corresponding figures for SPPB were 0.5 (95% CI: 0.5-0.6) and 0.5 (95% CI: 0.5-0.6), respectively. AUCs for men and women showed similar values.
Figure 2.
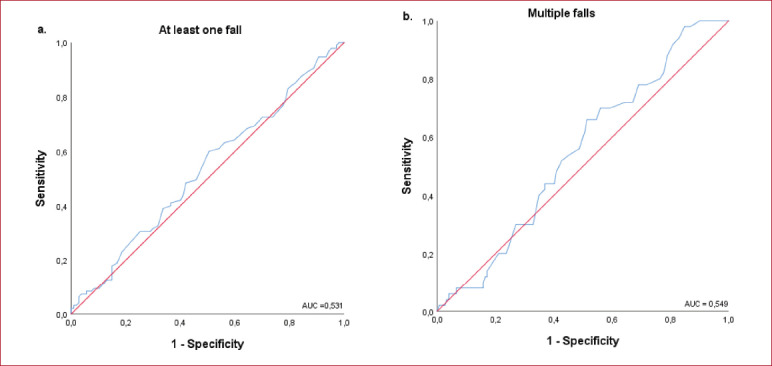
ROC-curves illustrating the predictive validity of the Timed Up and Go test for a. one or more falls compared to no falls and b. two or more falls compared to no or a single fall.
Figure 3.
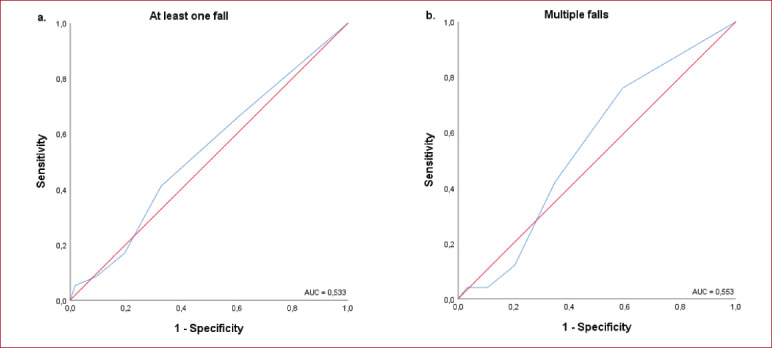
ROC-curves illustrating the predictive properties of Short Physical Performance Battery for a. one or more falls compared to no falls and b. two or more falls compared to no or a single fall.
Discussion
The participants in this study had a good mental and physical status. Nevertheless, almost half of them fell during the one-year follow-up period. Neither the Timed Up and Go test nor the Short Physical Performance Battery were able to predict falls in independent older adults living in the community. Our results are in accordance with some previous studies of independently living older adults[15,20,28].
Our results contradict previous suggestions that TUG below 13.5 seconds indicates a low risk of falling in community-living older adults[29]. On one hand, this contradiction might be due to our exclusion of frail older adults with poor function. On the other hand, and in line with our results, a meta-analysis of both retrospective and prospective studies in community-dwelling older adults found that the cut-off score of 13.5 did not predict falls[16]. Suggestions of cut-off time points for TUG to discriminate between fallers and non-fallers in community-living older adults range between 8.1 and 16 seconds, walking at preferred speed[16,30]. This large range of cut-offs points to the intricacy of making this distinction in such a heterogeneous group as community-living older adults constitutes. To our surprise, evaluations of SPPB in longitudinal prospective studies are scarce. A review on the prognostic validity of risk factors for falling[31] showed that the most consistent predictors of future falling were abnormalities of gait or balance. Given that the TUG and SPPB assess both balance and gait, the poor predictive validity was unexpected to us.
There are limitations to the generalisability of the results in this study. This study was a prospective follow-up of falls in which the falls were self-reported. There is always a challenge to know whether all falls were accurately reported. However, the participants were presented with a definition of a fall at the start of the study; they had fall-diaries with a printed definition of a fall and monthly reminders. The fall rate in this study was high which support that there was not an underreporting of falls.
The older adults included in this study might not be representative of the population of older community-living older adults as we excluded those who were lower functioning and not independent, all were aged 75 or over and only three received any home care service. However, as older adults live longer in their own homes, there is a need to clearly define which assessments tools that are appropriate to use in both less- and more well-functioning groups of older adults.
Conclusion
This study does not support a recommendation to use the Timed Up and Go test and the Short Physical Performance Battery as tools for the identification of fall-prone persons among older independent adults living in the community. These results reinforce the need for further research into appropriate tools for identifying fall-prone older adults in this group.
Acknowledgment
The authors would like to thank our colleagues who participated in the baseline assessments, for their valuable contribution to this study. The baseline assessments were performed at the Clinical Research Centre, Umeå University Hospital, Umeå, Sweden. This investigation was supported by grants from the Swedish Research Council, the Swedish Council for Working Life and Social Research, the Lions’ Research foundation for age related diseases, King Gustav V’s and Queen Victoria’s Freemansons’s Foundation, the Erik and Anne-Marie Detlof’s Foundation, Umeå University.
Footnotes
Edited by: Yannis Dionyssiotis.
References
- 1.Lord SR. Falls in older people :risk factors and strategies for prevention. 2nd ed. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 2.Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. 2002;8(4):280–3. doi: 10.1136/ip.8.4.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Ageing and Life Course (ALC) WHO Global Report on Falls Prevention in Older Age. Geneva: World Health Organization; 2007. [Google Scholar]
- 4.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42(1):17–23. doi: 10.1093/geront/42.1.17. [DOI] [PubMed] [Google Scholar]
- 5.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults:a review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Moreira MN, Bilton TL, Dias RC, Ferriolli E, Perracini MR. What are the Main Physical Functioning Factors Associated With Falls Among Older People With Different Perceived Fall Risk? Physiother Res Int. 2017;22(3) doi: 10.1002/pri.1664. [DOI] [PubMed] [Google Scholar]
- 7.Crenshaw JR, Bernhardt KA, Achenbach SJ, Atkinson EJ, Khosla S, Kaufman KR, et al. The circumstances, orientations, and impact locations of falls in community-dwelling older women. Arch Gerontol Geriat. 2017;73:240–7. doi: 10.1016/j.archger.2017.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J, et al. Complex interventions to improve physical function and maintain independent living in elderly people:a systematic review and meta-analysis. Lancet. 2008;371(9614):725–35. doi: 10.1016/S0140-6736(08)60342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7:CD012221. doi: 10.1002/14651858.CD012221.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. doi: 10.1002/14651858.CD012424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults:an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–8. doi: 10.1136/bjsports-2016-096547. [DOI] [PubMed] [Google Scholar]
- 12.Podsiadlo D, Richardson S. The timed “Up &Go”:a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 13.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function:association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 14.Rydwik E, Forsen L, Frandin K. Psychometric Properties of Timed Up and Go in Elderly People:A Systematic Review. Physical &Occupational Therapy in Geriatrics. 2011;29(2):102–25. [Google Scholar]
- 15.Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall:systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(2):202–8. doi: 10.1111/jgs.12106. [DOI] [PubMed] [Google Scholar]
- 16.Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults:a systematic review and meta-analysis. BMC Geriatr. 2014;14:14. doi: 10.1186/1471-2318-14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freiberger E, de Vreede P, Schoene D, Rydwik E, Mueller V, Frandin K, et al. Performance-based physical function in older community-dwelling persons:a systematic review of instruments. Age Ageing. 2012;41(6):712–21. doi: 10.1093/ageing/afs099. [DOI] [PubMed] [Google Scholar]
- 18.Ward RE, Leveille SG, Beauchamp MK, Travison T, Alexander N, Jette AM, et al. Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc. 2015;63(2):315–20. doi: 10.1111/jgs.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherrington C, Lord SR, Close JC, Barraclough E, Taylor M, OâRourke S, et al. Development of a tool for prediction of falls in rehabilitation settings (Predict_FIRST):a prospective cohort study. J Rehabil Med. 2010;42(5):482–8. doi: 10.2340/16501977-0550. [DOI] [PubMed] [Google Scholar]
- 20.Kwok BC, Clark RA, Pua YH. Novel use of the Wii Balance Board to prospectively predict falls in community-dwelling older adults. Clin Biomech (Bristol, Avon) 2015;30(5):481–4. doi: 10.1016/j.clinbiomech.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Nordin E, Moe-Nilssen R, Ramnemark A, Lundin-Olsson L. Changes in step-width during dual-task walking predicts falls. Gait Posture. 2010;32(1):92–7. doi: 10.1016/j.gaitpost.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Wade DT, Collin C. The Barthel ADL Index:a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64–7. doi: 10.3109/09638288809164105. [DOI] [PubMed] [Google Scholar]
- 24.Lundin-Olsson L, Nyberg L, Gustafson Y. Attention, frailty, and falls:the effect of a manual task on basic mobility. J Am Geriatr Soc. 1998;46(6):758–61. doi: 10.1111/j.1532-5415.1998.tb03813.x. [DOI] [PubMed] [Google Scholar]
- 25.Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46(3):M69–76. doi: 10.1093/geronj/46.3.m69. [DOI] [PubMed] [Google Scholar]
- 26.Frändin K GG. Assessment of physical activity, fitness and performance in 76-year-olds. Scand J Med Sci Sports. 1994;4:41–6. [Google Scholar]
- 27.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York, Chichester: Wiley; 2000. [Google Scholar]
- 28.Yamada M, Ichihashi N. Predicting the probability of falls in community-dwelling elderly individuals using the trail-walking test. Environ Health Prev Med. 2010;15(6):386–91. doi: 10.1007/s12199-010-0154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up &Go Test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 30.Kojima G, Masud T, Kendrick D, Morris R, Gawler S, Treml J, et al. Does the timed up and go test predict future falls among British community-dwelling older people?Prospective cohort study nested within a randomised controlled trial. BMC Geriatr. 2015;15:38. doi: 10.1186/s12877-015-0039-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]


