Abstract
Background and Objectives
The proportion of racial/ethnic minority older adults in nursing homes (NHs) has increased dramatically and will surpass the proportion of white adults by 2030.Yet, little is known about minority groups’ experiences related to the quality of life (QOL). QOL is a person-centered measure, capturing multiple aspects of well-being. NH quality has been commonly measured using clinical care indicators, but there is growing recognition for the need to include QOL. This study examines the role of individual race/ethnicity, facility racial/ethnic composition, and the interaction of both for NH resident QOL.
Research Design and Methods
We used a unique state-level data set that includes self-reported QOL surveys with a random sample of long-stay Minnesota NH residents, using a multidimensional measure of QOL. These surveys were linked to resident clinical data from the Minimum Dataset 3.0 and facility-level characteristics. Minnesota is one of the two states in the nation that collects validated QOL measures, linked to data on resident and detailed facility characteristics. We used mixed-effects models, with random intercepts to model summary QOL score and individual domains.
Results
We identified significant racial disparities in NH resident QOL. Minority residents report significantly lower QOL scores than white residents, and NHs with higher proportion minority residents have significantly lower QOL scores. Minority residents have significantly lower adjusted QOL than white residents, whether they are in low- or high-minority facilities, indicating a remaining gap in individual care needs.
Discussion and Implications
The findings highlight system-level racial disparities in NH residents QOL, with residents who live in high-proportion minority NHs facing the greatest threats to their QOL. Efforts need to focus on reducing racial/ethnic disparities in QOL, including potential public reporting (similar to quality of care) and resources and attention to provision of culturally sensitive care in NHs to address residents’ unique needs.
Keywords: Long-term care, Racial/ethnic disparities, Diversity, Policy, Person-centered care
Translational Significance.
Nursing home residents from minority racial/ethnic backgrounds experience lower quality of life compared with white residents whether they are in low- or high-minority facilities. This disparity remains, even when controlling for other factors. Findings have implications for hospital discharge planners and family members when selecting NHs for residents of color and indigenous residents and for policy initiatives, such as public reporting and investment in high-proportion minority facilities.
The proportion of racial/ethnic minority older adults residing in nursing homes (NH) has increased dramatically in the past decade and will surpass that of white adults by 2030 (1). NHs account for 17% of Medicaid spending (2) but remain more racially segregated than other health care settings (3). Racial/ethnic disparities in various clinical quality indicators are persistent (4), with racial/ethnic minority NH residents having worse quality of care compared with white residents (5–7). Minority residents experience higher use of physical restraints (8), lower rates of flu vaccination (9), greater risk of end-of-life hospitalization (10), and are less likely to receive specialized dementia care (4,11). Other studies identified racial disparities in use of antipsychotic medications (12), diagnosis and treatment of depression (13), and differences in rates of pressure sores (12–14).
While important, all this research has focused on gaps in adequate clinical care processes and health outcomes (15–17). However, little research has focused on NH quality of life (QOL). QOL is a multidimensional construct that refers to an individual’s self-reported psychological and social well-being and captures nonmedical aspects of life in the facility (18). Life in NHs is regimented, which can impair privacy, dignity, and the ability to form meaningful relationships with other residents and staff. Furthermore, QOL includes aspects of the residents’ mood and their satisfaction with the food and services (19–21). Because overall well-being and life satisfaction can be as important to residents as the quality of care they receive, there have been numerous calls for the inclusion of QOL measures along with clinical quality indicators as a more comprehensive view of overall long-term care quality (22).
Yet, we know little about how QOL differs by residents’ race/ethnicity and the role of facility characteristics for racial and ethnic differences in QOL. Few studies have examined how NH residents from racial/ethnic minority groups differ in their QOL compared with their white counterparts. Existing studies have used NH deficiencies (7), which are state inspector reports regarding violations of federal guidelines. This work finds nearly no improvement in deficiency outcomes for high-proportion minority facilities. However, deficiencies are poor proxies for QOL as they are not self-reported by residents and reflect regulatory concerns. As a few qualitative studies point out, there are significant differences in NH QOL by racial/ethnic minority status, with minority residents reporting lower satisfaction with food and activities (23–25).
Most notably, when QOL is examined quantitatively, much of the racial disparity in QOL can be attributed to facility characteristics (26). These findings on QOL align with past studies on quality of care which have argued that the NH industry is effectively operated in a two-tiered system where some NHs have fewer resources and thus deliver subpar care (27,28). It is particularly concerning that minority residents often receive care in these lower tiered NHs (4,29,30).
New Contribution
The key focus of this study is the interaction of two components: resident race/ethnicity and facility minority composition and their association with resident QOL. This study adds to the limited literature on racial/ethnic disparities in NH QOL by using resident QOL interviews from a representative sample of residents in Minnesota, linked to the Minimum Dataset, and facility characteristics, to examine the roles of the resident’s race/ethnicity, the proportion of minority residents at the facility level, and the interaction between the two. By examining the role of the resident’s minority status and its interaction with facility minority composition, we can identify both the within-facility and between-facility disparities. The within-facility disparity arises from differences in treatment due to a resident’s minority status within a facility and potential differences in attention paid by the staff to minority residents. These, in part, could stem from inadequate attention to cultural sensitivity, racial bias, or discrimination.
In contrast, between-facility disparities arise because minority residents may reside in facilities that are different from white residents. For example, minority residents may cluster in higher proportion minority facilities, perhaps because they want to be in places that house people who are culturally alike and have similar experiences (17). Being in a facility with more people with similar backgrounds can lead to stronger social relationships, more shared experiences that stem from interacting with the health care system (31), and the NH being more willing to accommodate the needs of a minority group if there are more of them in the facility. However, if these high-minority facilities are also poorly resourced by having more Medicaid funding, the result is fewer resources to invest in quality efforts, including QOL.
Research Design and Methods
Data
This study uses 2015 QOL data from Minnesota, a state that collects validated QOL information that can be merged with the Minimum Dataset (MDS). In the data collection process, long-stay residents (which the Minnesota QOL data define as stays over 30 days) are randomly selected for in-person interviews conducted by an independent survey firm, resulting in an average of 32.3 respondents per NH (range 12–76) (32). We linked each QOL survey respondent to their MDS assessment that fell closest to their QOL survey date to obtain resident-level data. Furthermore, we used Certification and Survey Enhanced Provider Reporting and Minnesota cost report data to provide facility-level characteristics.
After excluding one facility on a Native American reservation with 100% Native American residents due to this NH being different from other NHs in the state, our analytical sample contains 10,455 non-Hispanic white residents and 671 racial/ethnic minority residents (6.0% of sample) in 355 NHs. Among the minority residents, 415 are non-Hispanic black residents, 101 are Native American residents, and 155 respondents who were Asian American, Hispanic of any race, or any other race or ethnicity.
Key Explanatory Variables
Individual race/ethnicity
The race/ethnicity of the respondent is an indicator variable for self-reported race/ethnicity and whether a resident is a member of a racial/ethnic minority group (aggregated due to small sample size). In full analyses, we report the results for black, Native American, and all other minority residents (aggregated) separately.
Racial/ethnic minority composition of the facility
We constructed an indicator variable for whether the facility is a high-proportion minority facility, based on data from the MDS. Because the threshold for what is considered high-minority composition varies across states, we defined an NH as high-minority if it was above the 90th percentile for proportion of minority residents in the state of Minnesota. For Minnesota, the 90th percentile facility had a minority composition of more than 14%. Making facility the unit of analysis, the low-minority NHs have 2.36% minority residents. The high-minority facilities have 27.22% minority residents on average. Of 355 NHs, 118 had no minority residents. We conducted a number of sensitivity analyses to test for different thresholds to define high-minority facilities, in addition to treating the percent of minority residents as a continuous variable with linear and quadratic terms. None of these sensitivity analyses substantively changed our findings.
QOL Measures
To measure QOL, we use an established, validated QOL instrument that has 31 items that cover six domains, such as social engagement, attention from staff, and meal enjoyment (33). We calculate scores for each domain by adding individual items and standardizing the summed items to percentage points (i.e., 0 to 100) with higher values indicating better QOL. We also calculate a summary score which is the average of standardized scores on the six domains. Table 1 provides a brief description of each domain. In calculating these scores, an average of 2.62 out of 31 items are reported as missing (i.e., respondent did not know, that the question does not matter, or refuses to answer). We used multiple imputation by chained equations for each question utilized in calculating the QOL measures and for the small number of covariates that had missing data. We did not impute race/ethnicity of the resident. Any resident with missing race/ethnicity was excluded from the analysis (less than 5% of the sample). Our sensitivity analyses generated similar results whether we used imputed or nonimputed data.
Table 1.
Definition of Quality of Life Domains and Mean Quality of Life Scores by Race/Ethnicity (N = 11,126)
| Domain | Number of Items | Definition | White Residents | Minority Residents |
|---|---|---|---|---|
| Summary score | 31 | Unweighted mean of domains below | 79.517 | 73.203*** |
| Environmental adaptations | 4 | Does resident’s environment maximize their independence? | 84.469 | 81.852* |
| Attention | 6 | Adequacy of personal care, are staff respectful and gentle, would resident recommend facility? | 92.160 | 84.662*** |
| Food enjoyment | 3 | Does resident enjoy food at facility? | 81.610 | 69.439*** |
| Engagement | 9 | Does resident have meaningful activities, meaningful relationships with other residents and staff? | 78.973 | 70.730*** |
| Negative mood | 6 | Negative affect | 65.269 | 62.549** |
| Positive mood | 3 | Positive affect | 75.667 | 71.248*** |
Note: Stars represent t-test for significance relative to white residents.
*p < 0.05, **p < 0.01, ***p < 0.001.
Control Variables
In multivariate analyses, we adjust the QOL scores for potential differences in resident and facility characteristics using regression analysis, drawing covariates from the existing literature. Resident-level covariates include age, gender, length of stay, activities of daily living score (range 0–28), and a count of six chronic conditions: congestive heart failure, diabetes, hip fracture, paralysis, pressure ulcers, and stroke. These six conditions were used in the previous literature (33). We separately created flags for serious mental illness (SMI), behavioral symptoms, dementia diagnosis, and moderate or severe cognitive impairment. Cognitive status was determined by responses to the Brief Interview for Mental Status, or if the resident is unable to respond, the nurse-assessed Cognitive Performance Scale (34).
At the facility-level, we include the proportion of residents under age 65, geographic location (Twin Cities metropolitan area, other metropolitan area, micropolitan area, or rural), proportion of Medicare and Medicaid patient-days, ownership (nonprofit, for-profit, government), affiliation with a hospital or with a NH chain, number of beds, occupancy ratio, proportion of private rooms, and acuity index. To account for staffing differences, we include the retention rate for all staff, and calculated staff hours per resident day for registered nurses, licensed practical nurses, certified nursing assistants, activities staff, and social workers and mental health workers combined. Lastly, we included the Minnesota Nursing Home Report Card score for facility quality of care, a 5-star rating score constructed from 21 indicators relevant for long-stay residents (35).
Analysis
We first present unadjusted mean QOL scores for white and minority residents stratified by the racial/ethnic composition of the facility. Next, we fit hierarchical linear models that include resident- and facility-level covariates along with a random intercept for each facility to predict the mean QOL score. We calculate predicted QOL scores for four groups—white and minority residents in both low- and high-minority facilities—at the mean values of the other resident and facility-level covariates. To determine the effect of minority status and facility minority composition, we report the difference for each group relative to a reference group of white residents in a low-minority facility.
We enter minority status and facility composition into the model in two ways: (A) allowing the respondent’s minority status and being in a high-minority facility to enter the model independently (Independent Effects) and (B) allowing minority status and facility composition to vary with each other by including an interaction term (Interacted Effects). The Independent Effects approach assumes that the effect of minority status on QOL is the same in low- and high-minority facilities, and the effect of being in a high-minority facility is the same regardless of the minority status of the respondent. Yet, this may not be the case, and the Interacted Effects approach allows the effect of minority status on QOL scores to vary with facility composition. By comparing the results from these two approaches, we are able to determine whether and how much of the disparity is likely driven by minority status, facility composition, or a combination of both.
Results
Descriptive Statistics
The unadjusted mean QOL scores are reported in Table 1 with stars reporting whether mean QOLs for minority residents are statistically different from white residents. Minority residents have QOL scores that are statistically lower than white residents for the summary score (73.2 vs 79.5) and each of the six domains. The largest disparities are in food enjoyment (69.4 vs 81.6), engagement (70.7 vs 79.0), and attention (84.6 vs 92.2). While each racial/ethnic group has statistically lower summary scores when compared with white residents, which domains are found to be statistically different for minority residents varies by racial/ethnic group. For example, black residents have significantly lower scores on all domains but lack of negative mood, Native American residents have significantly lower scores on all domains except environment and positive mood, and all other minority residents have significantly lower scores on all domains except environment and lack of negative mood (data not shown).
Differences in the characteristics of residents and the facilities where they reside could explain some of these disparities. Table 2 reports descriptive statistics of white and minority residents stratified by residing in a low- or high-minority facility. There are two general patterns that emerge. First, minority residents tend to be considerably younger, to have SMI and behavioral symptoms, and to live in for-profit NHs that are larger, more reliant on Medicaid, and generally have lower staffing levels. Second, high-minority facilities tend to be different from low-minority facilities, with low minority-facilities caring for residents with greater functional and cognitive impairment.
Table 2.
Sample Descriptive Statistics by Individual Race/Ethnicity and Facility Racial Composition
| Explanatory variables | Low-Minority Facility (N = 320 Facilities) | High-Minority Facility (N = 355 Facilities) | |||
|---|---|---|---|---|---|
| White | Minority | White | Minority | ||
| Resident characteristics | |||||
| Demographics | |||||
| Age | 84.084 | 73.944*** | 72.887*** | 65.759*** | |
| Female | 0.695 | 0.585*** | 0.547*** | 0.496*** | |
| Married | 0.221 | 0.154* | 0.112*** | 0.086*** | |
| Clinical and functional | |||||
| Length of stay (years) | 2.533 | 2.528 | 3.579*** | 3.650*** | |
| ADL score (0–28) | 14.985 | 14.209* | 11.337*** | 11.027*** | |
| Chronic conditions (0–5) | 1.729 | 1.980* | 1.670* | 1.924*** | |
| Anxiety or depression Dx | 0.572 | 0.512* | 0.583 | 0.514* | |
| Severe mental illness Dx | 0.112 | 0.160* | 0.350*** | 0.378*** | |
| Cognitive impairment or dementia Dx | 0.542 | 0.530 | 0.435*** | 0.425*** | |
| Behavioral symptoms | 0.184 | 0.223** | 0.324*** | 0.362*** | |
| Facility characteristics | |||||
| Structural characteristics | |||||
| Metropolitan statistical area (vs micropolitan or rural) | 0.541 | 0.778*** | 0.882*** | 0.942*** | |
| For-profit ownership (vs nonprofit or government) | 0.262 | 0.422*** | 0.558*** | 0.671*** | |
| Chain affiliation | 0.539 | 0.611* | 0.548 | 0.501 | |
| Hospital affiliation | 0.14 | 0.042*** | 0.043*** | 0.027*** | |
| Number of beds | 86.507 | 129.523*** | 114.512*** | 122.679*** | |
| Proportion private rooms | 0.538 | 0.438*** | 0.355*** | 0.276*** | |
| Case and payer-mix | |||||
| Proportion of Medicaid patient-days | 0.524 | 0.572*** | 0.698*** | 0.709*** | |
| Proportion of Medicare patient-days | 0.093 | 0.100* | 0.061*** | 0.056*** | |
| Staffing | |||||
| Registered nurse and licensed practical nurse HPRD | 1.228 | 1.316*** | 1.289*** | 1.291*** | |
| Certified nursing assistant HPRD | 2.201 | 2.141* | 1.810*** | 1.631*** | |
| Mental health and social worker HPRD | 0.118 | 0.130*** | 0.189*** | 0.251*** | |
| Activities staff HPRD | 0.261 | 0.222*** | 0.177*** | 0.165*** | |
| Staff retention | 0.672 | 0.652* | 0.682* | 0.683 | |
| Quality indicators | |||||
| Minnesota Quality of Care Star Rating | 3.052 | 2.948 | 2.978* | 2.874*** | |
| Sample sizes | 9553 | 306 | 902 | 365 | |
Notes: Stars represent the statistical significance levels for t- or chi-square tests for differences relative to white residents in low-proportion racial/ethnic-minority facilities. ADL = activities of daily living; Dx = Diagnosis; HPRD = hours per resident-day.
*p < .05, **p < .01, ***p < .001.
Predicted QOL Scores by Minority Status and Facility Composition
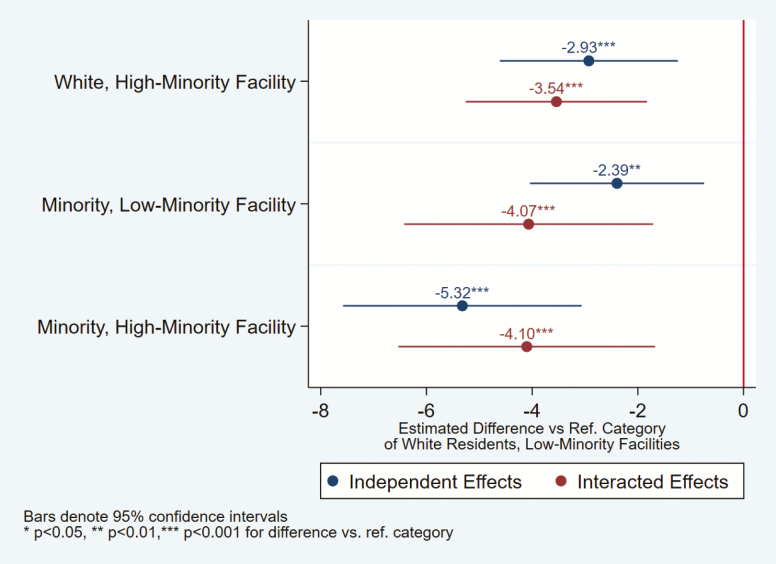
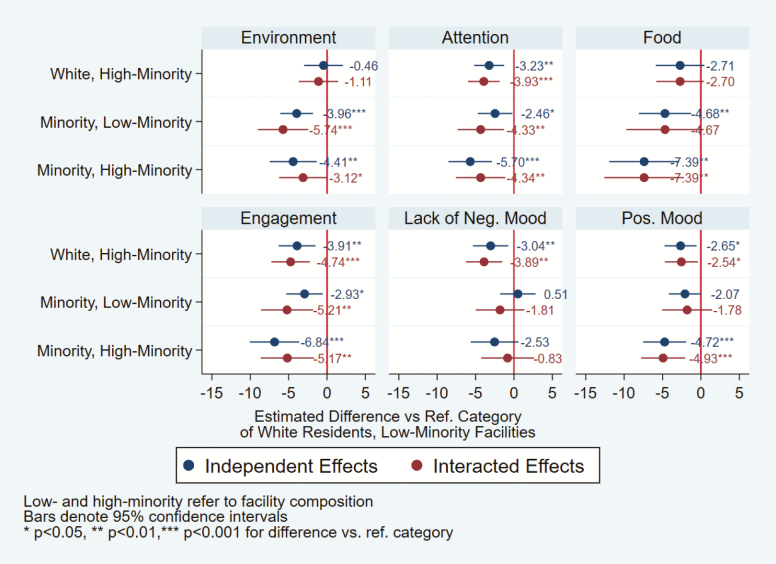
Differences in predicted QOL scores by minority status and facility composition relative to the reference group of a white resident in a low-minority facility are reported in Figure 1 for the summary score and Figure 2 for the six QOL domains. Table 3 reports the individual regression coefficients for individual race, high-minority facility, and their interaction. Full regression results are available upon request. In both figures, differences in predicted QOL score are reported that allow the resident’s race/ethnicity and facility composition to enter the model independently (Independent Effects) or through an interaction (Interacted Effects). The dots represent the average difference in predicted QOL score with the size of the effect listed above each dot along with the level of statistical significance. The horizontal lines show the 95% confidence interval.
Figure 1.
Differences in predicted overall quality of life scores by race/ethnicity and facility racial composition from independent versus interacted models. Note: Estimates are from full models, controlling for all covariates. Source: Authors’ analysis of data from Quality of Life Surveys, linked to Minimum Dataset and Facility Cost Report Data for Minnesota.
Figure 2.
Differences in predicted quality of life domain scores by race/ethnicity and facility racial composition from independent versus interacted models. Note: Estimates are from full models, controlling for all covariates. Source: Authors’ analysis of data from Quality of Life Surveys, linked to Minimum Dataset and Facility Cost Report Data for Minnesota.
Table 3.
Effect of Individual Race/Ethnicity and Facility Racial Composition Independent Effects Versus Interacted Effects Models (N = 11,126)
| Key Explanatory Variables | Independent Effects | Interacted Effects | ||
|---|---|---|---|---|
| b | SE | b | SE | |
| Race/Ethnicity | Summary score | |||
| Minority | −2.394** | 0.842 | −4.066*** | 1.202 |
| High-minority facility | −2.927*** | 0.860 | −3.541*** | 0.875 |
| Minority × High-minority facility | 3.505* | 1.553 | ||
| Environment | ||||
| Minority | −3.957*** | 1.085 | −5.735*** | 1.679 |
| High-minority facility | −0.458 | 1.295 | −1.113 | 1.310 |
| Minority × High-minority facility | 3.725 | 2.012 | ||
| Attention | ||||
| Minority | −2.464* | 1.154 | −4.334** | 1.540 |
| High-minority facility | −3.235** | 1.000 | −3.930*** | 1.054 |
| Minority × High-minority facility | 3.926 | 2.191 | ||
| Food | ||||
| Minority | −4.681** | 1.741 | −4.672 | 2.573 |
| High-minority facility | −2.708 | 1.619 | −2.704 | 1.582 |
| Minority × High-minority facility | −0.016 | 3.397 | ||
| Engagement | ||||
| Minority | −2.929* | 1.216 | −5.211** | 1.736 |
| High-minority facility | −3.907** | 1.229 | −4.742*** | 1.279 |
| Minority × High-minority facility | 4.781* | 2.293 | ||
| Lack of negative mood | ||||
| Minority | 0.510 | 1.178 | −1.814 | 1.619 |
| High-minority facility | −3.036** | 1.176 | −3.891** | 1.210 |
| Minority × High-minority facility | 4.873* | 2.278 | ||
| Positive mood | ||||
| Minority | −2.073 | 1.081 | −1.784 | 1.661 |
| High-minority facility | −2.648* | 1.067 | −2.544* | 1.103 |
| Minority × High-minority facility | −0.600 | 2.023 | ||
Note: Models control for age, sex, marital status, length of stay, diagnoses of anxiety, depression, and serious mental illness, behavioral symptoms, cognitive impairment, dementia, facility ownership, chain status, and hospital affiliation, number of beds, occupancy, percent of private rooms, metropolitan status, staffing, and quality of care star rating. × = Interaction term.
*p < .05, **p < .01, ***p < .001.
Compared with white residents in low-minority facilities, all other groups report lower QOL summary scores that are statistically significant at conventional levels (Figure 1). Allowing the effect of respondent’s minority status and facility composition to be independent, white residents in high-minority facilities have a predicted 2.9% point lower QOL score, whereas minority residents in low-minority facilities are 2.4% points lower and minority residents in high-minority facilities are 5.3% points lower. These results are consistent with minority residents reporting lower QOL scores and all residents regardless of minority status reporting lower QOL scores in high-minority facilities. However, the Interacted Effects model finds that white residents in high-minority facilities have a 3.5% point lower score, whereas minority residents in low- or high-minority facilities have a 4.1% point lower score. This implies that white residents have lower QOL scores in high-minority facilities, and minority residents have lower QOL scores, though score is similar whether the minority resident is in a low- or high-minority facility, indicating that the effect of the minority status and facility composition are not independent.
Among the six domains (Figure 2), white residents in high-minority facilities had significantly lower scores than their counterparts in low-minority facilities in four of the six domains. Minority residents also have lower QOL scores than the reference group. Among minorities in low-minority facilities, QOL scores are statistically lower in three and four domains in the Independent and Interacted Effects models, respectively. Minority residents in high-minority facilities have statistically lower QOL scores in five domains. Comparing the Independent and Interacted Effects models, the domains of staff attention, engagement, and lack of negative mood have similar effects for minority residents regardless of facility composition, whereas the domains of food enjoyment and positive mood tend to have independent effects for minority status and facility composition.
One limitation of the results reported in Figures 1 and 2 is all minorities are treated as one homogeneous group. To determine whether the results vary by racial/ethnic group, we calculated predicted QOL scores for black, Native American, and other minority groups separately (data not shown). For the summary score, relative to the reference group all minority groups have lower QOL scores, with the largest effect among Native Americans. Consistent with earlier reported results, the predicted summary score is similar for each minority group regardless of the facility composition in the Interacted Effects model. For the six domains, the smaller sample sizes caused many of the effects to become statistically insignificant, though patterns tended to follow the unadjusted means reported in Table 1. Furthermore, we conducted sensitivity analyses to test for different thresholds to define high-minority facilities (Supplementary Table 1). We also estimated the models using observations that were not imputed (Supplementary Table 2). The main findings are unchanged.
Discussion and Implications
Understanding racial/ethnic disparities in NH QOL is more complex than simply examining the average quality provided to residents by racial/ethnic minority status. As our summary statistics show, racial/ethnic minority NH residents are significantly different than their white counterparts. Minority residents tend to be younger and have higher reported prevalence of mental illness and behavioral problems. Furthermore, minority residents are more likely to reside in high-proportion minority NHs. These high-minority facilities are often larger, for-profit, have a higher reliance on Medicaid, and have lower staffing levels. Many of these factors, especially payer-mix and lower staffing levels, are associated with poor clinical quality (36). Yet, even after controlling for these differences, similar to studies that examine clinical measure of quality of care, we find significant racial/ethnic disparities in QOL among NHs residents.
Beyond just identifying a disparity, we also explore the interaction between minority status and facility minority composition. Compared with white residents in low-minority facilities, minority NH residents have lower QOL scores regardless of if they reside in a low- or high-minority facility. More importantly for overall QOL, as measured by a summary score, and for many QOL domains, minority residents in low- and high-minority facilities have similar QOL scores. To this end, minority residents report lower QOL regardless of the minority composition of the facility. However, some caution is warranted as some domains vary by facility composition. For example, racial/ethnic minorities in high-minority NHs express lower QOL in the food enjoyment and positive mood domains when compared with minorities in low-minority facilities.
These findings may be due to NHs with higher concentrations of racial/ethnic minorities having structural characteristics that are associated with lower QOL, including lower staffing and for-profit ownership, and higher reliance on Medicaid. Without greater funding for these facilities to invest in quality improvement efforts, progress toward improving resident QOL will be slow. Until policymakers focus on high-proportion minority facilities, a key finding of this article is that facility resources and capabilities to meet the residents’ needs should be the primary driver of where to suggest residents seek care, instead of focusing on a facility’s racial and ethnic composition.
While the results for minority residents suggest that there is a little protective effect for QOL by facility composition, this is not true for white residents. White residents in high-minority facilities have different characteristics than white residents in low-minority facilities. However, even after controlling for these differences, white residents consistently report lower QOL scores in high-minority facilities. Therefore, the minority composition of a facility seems to be more salient for white residents than minority residents.
While we have performed a number of robustness checks, our analysis still has limitations, such as being limited to Minnesota. However, we believe that our estimates are likely generalizable to other states and are more conservative, because Minnesota equalizes Medicaid and private NH per diem rates by statute, which could ameliorate disparities in facility financial resources between NHs that rely heavily on Medicaid and NHs that do not. Another consideration is that Minnesota is a Midwestern state with a relatively racially homogeneous older adult population and Minnesota’s NH population tends to be among the most segregated in the United States (4). A number of Native American respondents live in rural areas, but other minority residents are otherwise concentrated in NHs in the Twin Cities Metropolitan Area. We performed a number of sensitivity analyses to address these concerns. No analyses substantively changed our findings and significant racial/ethnic differences remained. While conducting this analysis for other states is warranted, and some states have used validated QOL instruments, such as Ohio (37), to the best of our knowledge, Minnesota is the only state that regularly uses a validated QOL instrument that can be merged with MDS data. This link to MDS data is essential to account for resident-level factors that may have a significant influence on QOL scores.
Conclusion
Even though high QOL is important to NHs residents, most initiatives to improve NH quality have focused on clinical aspects of care (38,39). Similar to these clinical aspects of care, there are racial/ethnic disparities in QOL, and understanding these disparities is key to improving the care racial/ethnic minority residents receive in NHs. Though minority residents have lower QOL scores than white residents in low-minority facilities, minority residents generally have similar scores in low- and high-minority facilities. In contrast, white residents report lower QOL scores in high-minority facilities (vs low-minority), even when other factors are held constant.
As efforts are developed to reduce disparities in all aspects of NH care, these findings have implications for discharge planners and selection of NHs for minority residents. Even though minority NH consumers may seek care at facilities that have similar racial/ethnic composition, when it comes to QOL, minority residents report somewhat higher satisfaction in NHs that have a greater proportion of white residents (in part, likely due to more resources). This is also relevant for using QOL information, including the potential public reporting of QOL measures. QOL scores could be incorporated as a quality metric and could be based on the facility’s racial/ethnic minority composition and resident race/ethnicity. Simply reporting average QOL scores may not provide the best information to the potential NH consumers as resident choices might vary by race/ethnicity. While reporting QOL scores by race/ethnicity is an option, race-specific measures may not be feasible in areas with small populations of minority residents. Therefore, more work is needed to understand which aspects of QOL are most important to those from diverse racial/ethnic groups and how race/ethnicity influences QOL scores, with the ultimate goal of developing a measure that best matches the needs of increasingly diverse population and providing care that meets the needs of all residents equitably.
Funding
This study was funded by the National Institute on Minority Health and Health Disparities (5R01MD010729 to T.P.S.).
Conflict of Interest
None reported.
Supplementary Material
References
- 1. Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Aff. 2011;30(7):1358–1365. doi: 10.1377/hlthaff.2011.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eiken S, Sredl K, Gold L, Kasten J, Burwell B, Saucier P.. Medicaid Expenditures for Long-Term Care Services and Supports in FFY 2012. Ann Arbor, MI: Truven Health Analytics; 2014. [Google Scholar]
- 3. Konetzka RT, Werner RM. Disparities in long-term care: building equity into market-based reforms. Med Care Res Rev. 2009;66:491–521. doi: 10.1177/1077558709331813 [DOI] [PubMed] [Google Scholar]
- 4. Smith DB, Feng Z, Fennell ML, Zinn J, Mor V. Racial disparities in access to long-term care: the illusive pursuit of equity. J Health Polit Policy Law. 2008;33:861–881. doi: 10.1215/03616878-2008-022 [DOI] [PubMed] [Google Scholar]
- 5. Arling G, Kane RL, Mueller C, Bershadsky J, Degenholtz HB.. Nursing effort and quality of care for nursing home residents. Gerontologist. 2007;47:672–682. doi: 10.1093/geront/47.5.672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fennell ML, Miller SC, Mor V. Facility effects on racial differences in nursing home quality of care. Am J Med Qual. 2000;15:174–181. doi: 10.1177/106286060001500408 [DOI] [PubMed] [Google Scholar]
- 7. Li Y, Harrington C, Temkin-Greener H, et al. Deficiencies in care at nursing homes and racial/ethnic disparities across homes fell, 2006–11. Health Aff. 2015;34(7):1139–1146. doi: 10.1377/hlthaff.2015.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cassie KM, Cassie W. Racial disparities in the use of physical restraints in U.S. nursing homes. Health Soc Work. 2013;38:207–213. doi: 10.1093/hsw/hlt020 [DOI] [PubMed] [Google Scholar]
- 9. Cai S, Feng Z, Fennell ML, Mor V. Despite small improvement, black nursing home residents remain less likely than whites to receive flu vaccine. Health Aff. 2011;30:1939–1946. doi: 10.1377/hlthaff.2011.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mor V, Papandonatos G, Miller SC. End-of-life hospitalization for African American and non-Latino white nursing home residents: variation by race and a facility’s racial composition. J Palliat Med. 2005;8:58–68. doi: 10.1089/jpm.2005.8.58 [DOI] [PubMed] [Google Scholar]
- 11. Sengupta M, Decker SL, Harris-Kojetin L, Jones A. Racial differences in dementia care among nursing home residents. J Aging Health. 2012;24:711–731. doi: 10.1177/0898264311432311 [DOI] [PubMed] [Google Scholar]
- 12. Hudson TJ, Cody M, Armitage TL, Curtis MA, Sullivan G. Disparities in use of antipsychotic medications among nursing home residents in Arkansas. Psychiatr Serv. 2005;56:749–751. doi: 10.1176/appi.ps.56.6.749 [DOI] [PubMed] [Google Scholar]
- 13. Levin CA, Wei W, Akincigil A, Lucas JA, Bilder S, Crystal S. Prevalence and treatment of diagnosed depression among elderly nursing home residents in Ohio. J Am Med Dir Assoc. 2007;8:585–594. doi: 10.1016/j.jamda.2007.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baumgarten M, Margolis D, van Doorn C, et al. Black/white differences in pressure ulcer incidence in nursing home residents. J Am Geriatr Soc. 2004;52:1293–1298. doi: 10.1111/j.1532-5415.2004.52358.x [DOI] [PubMed] [Google Scholar]
- 15. Arling G, Kane RL, Lewis T, Mueller C. Future development of nursing home quality indicators. Gerontologist. 2005;45:147–156. doi: 10.1093/geront/45.2.147 [DOI] [PubMed] [Google Scholar]
- 16. Mor V. Improving the quality of long-term care with better information. Milbank Q. 2005;83:333–364. doi: 10.1111/j.1468-0009.2005.00405.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rahman M, Foster AD.. Racial segregation and quality of care disparity in US nursing homes. J Health Econ. 2015;39:1–16. doi: 10.1016/j.jhealeco.2014.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zubritsky C, Abbott KM, Hirschman KB, Bowles KH, Foust JB, Naylor MD. Health-related quality of life: expanding a conceptual framework to include older adults who receive long-term services and supports. Gerontologist. 2013;53:205–210. doi: 10.1093/geront/gns093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kane RA. Definition, measurement, and correlates of quality of life in nursing homes: toward a reasonable practice, research, and policy agenda. Gerontologist. 2003;43(Spec No. 2):28–36. doi: 10.1093/geront/43.suppl_2.28 [DOI] [PubMed] [Google Scholar]
- 20. Meeks S, Looney SW. Depressed nursing home residents’ activity participation and affect as a function of staff engagement. Behav Ther. 2011;42:22–29. doi: 10.1016/j.beth.2010.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shippee TP. Examining Racial Differences in Nursing Home Residents’ Quality of Life. St. Paul, MN: Minnesota Department of Human Services; 2016. [Google Scholar]
- 22. Brauner D, Werner RM, Shippee TP, Cursio J, Sharma H, Konetzka RT. Does nursing home compare reflect patient safety in nursing homes? Health Aff. 2018;37:1770–1778. doi: 10.1377/hlthaff.2018.0721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Engle VF, Fox-Hill E, Graney MJ. The experience of living–dying in a nursing home: self-reports of black and white older adults. J Am Geriatr Soc. 1998;46:1091–1096. doi: 10.1111/j.1532-5415.1998.tb06646.x [DOI] [PubMed] [Google Scholar]
- 24. Ryvicker M. Staff–resident interaction in the nursing home: an ethnographic study of socio-economic disparities and community contexts. J Aging Stud. 2011;25(3):295–304. doi: 10.1016/j.jaging.2010.11.001 [DOI] [Google Scholar]
- 25. Wu S, Barker JC. Hot tea and juk: the institutional meaning of food for Chinese elders in an American nursing home. J Gerontol Nurs. 2008;34:46–54. doi: 10.3928/00989134-20081101-11 [DOI] [PubMed] [Google Scholar]
- 26. Shippee TP, Henning-Smith C, Rhee TG, Held RN, Kane RL. Racial differences in Minnesota nursing home residents’ quality of life: the importance of looking beyond individual predictors. J Aging Health. 2016;28:199–224. doi: 10.1177/0898264315589576 [DOI] [PubMed] [Google Scholar]
- 27. Konetzka RT, Gray ZS. The role of socioeconomic status in nursing home quality ratings. Seniors Hous Care J. 2017;25(1):3–14. [Google Scholar]
- 28. Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82: 227–256. doi: 10.1111/j.0887-378X.2004.00309.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Howard DL, Sloane PD, Zimmerman S, et al. Distribution of African Americans in residential care/assisted living and nursing homes: more evidence of racial disparity? American Journal of Public Health. 2002;92:272–1277. doi: 10.2105/ajph.92.8.1272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sharma H, Perraillon MC, Werner RM, Grabowski DC, Konetzka RT. Medicaid and nursing home choice: why do duals end up in low-quality facilities? J Appl Gerontol. 2019. doi: 10.1177/0733464819838447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14 [DOI] [PubMed] [Google Scholar]
- 32. Vital Research. Implementation of the 2010 Consumer Satisfaction and Quality of Life Survey in Minnesota Nursing Homes and Satisfaction Survey of Family Members of Residents in Minnesota Nursing Homes: Final Report. Los Angeles, CA: Vital Research; 2010. [Google Scholar]
- 33. Shippee TP, Henning-Smith C, Kane RL, Lewis T. Resident- and facility-level predictors of quality of life in long-term care. Gerontologist. 2015;55:643–655. doi: 10.1093/geront/gnt148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thomas KS, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function Scale. Med Care. 2017;55:e68–e72. doi: 10.1097/MLR.0000000000000334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Minnesota Department of Human Services. Minnesota Nursing Home Report Card Technical User Guide. St. Paul, MN: Minnesota Department of Human Services; 2017. [Google Scholar]
- 36. Bowblis JR. Ownership conversion and closure in the nursing home industry. Health Econ. 2011;20:631–644. doi: 10.1002/hec.1618 [DOI] [PubMed] [Google Scholar]
- 37. Shippee TP, Ng W, Roberts AR, Bowblis JR. Family satisfaction with nursing home care: findings and implications from two state comparison. J Appl Gerontol. 2018. doi: 10.1093/geroni/igy023.1479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Harrington C, Wiener JM, Ross L, Musumeci M.. Key Issues in Long-Term Services and Supports Quality. San Francisco, CA: Kaiser Family Foundation; 2017. [Google Scholar]
- 39. Kane RA, Cutler LJ. Re-imagining long-term services and supports: towards livable environments, service capacity, and enhanced community integration, choice, and quality of life for seniors. Gerontologist. 2015;55:286–295. doi: 10.1093/geront/gnv016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.