Abstract
Objectives
To compare the number of patients attending the Urology Emergency Department (ED) of the Centro Hospitalar Universitário do Porto (CHUP), as well as their demographic characteristics, the reasons for admission, the clinical severity under the Manchester triage system (MTS), and the need for emergency surgery or hospitalisation, during the coronavirus disease 2019 (COVID‐19) pandemic and the equivalent period in 2019.
Patients and methods
Data were collected from patients attending the Urology ED of the CHUP over 3 weeks, from 11 March to 1 April 2020, and from the same period in the previous year (from 11 March to 1 April 2019).
Results
During the pandemic, 46.4% fewer patients visited our urological ED (122 vs 263). There was no significant difference in the mean age or the number of old patients (aged ≥65 years) between the two periods. However, significantly fewer female patients sought emergency urological services during the COVID‐19 pandemic period (32.7% vs 14.8%, P < 0.05). No significant differences were noted between different clinical severity groups under the MTS. In 2019, significantly less patients required hospitalisation. The most common reasons for admission, during both periods, were haematuria, renal colic and urinary tract infections. The authors recognise that the study has several limitations, namely, those inherent to its retrospective nature.
Conclusion
COVID‐19 significantly influenced people’s urological care‐seeking behaviour. Understanding the present situation is helpful for predicting future urological needs. Based on the results of this study, we have reason to speculate that people’s requirements for urological services might grow explosively in the post‐COVID‐19 period. There should be further studies about the real state of long‐term urological services and the consequences that this pandemic may have in terms of morbimortality not directly related to the severe acute respiratory syndrome coronavirus 2.
Keywords: severe acute respiratory syndrome coronavirus 2 (SARS‐Cov‐2), emergency department, urology, pandemics, state of emergency
Introduction
Since its beginning in December 2019, the coronavirus disease 2019 (COVID‐19) outbreak has spread globally and was declared a pandemic by the World Health Organization on 11 March 2020 [1].
Following this pandemic, the state of emergency in Portugal was declared on 18 March and was renewed on 2 April 2020 [2]. The decrease in attendances to the Emergency Departments (EDs) of Portuguese hospitals was noticeable. The Portuguese media has reported several examples of tertiary hospitals that have registered a substantially lower number of visitors to EDs [3].
According to the Portuguese Health Report of 2018 [4], Portuguese hospitals received 6 318 359 emergency episodes, of which only 8% required hospitalisation.
A critical challenge is to determine if this reduction is applicable to patients with genitourinary symptoms or complications and to understand if patients with urological life‐threatening clinical situations are postponing their urgent evaluation with severe consequences in the near future.
The aim of the present study was to compare the number of patients who attended the Urology ED of a Portuguese Tertiary Hospital, the Centro Hospitalar Universitário do Porto (CHUP), as well as their demographic characteristics and the main causes of presentation to the ED, during the COVID‐19 pandemic and the equivalent period in the previous year.
Patients and Methods
This is an observational, retrospective and single‐centre study. Data were collected from patients attending the Urology ED of the CHUP over 3 weeks, from 11 March 2020 to 1 April 2020, and from the same period in the previous year (from 11 March to 1 April 2019). The Urology ED of the CHUP runs daily from 08:00 to 20:00 h.
The triage at this hospital is done according to the Manchester Triage System (MTS), which divides patients into five degrees of urgency, from those requiring immediate observation (red bracelet) to patients considered non‐urgent (blue bracelet). The white bracelet corresponds to cases referred to the ED for administrative or clinical reasons [5].
The patient’s demographic characteristics, the reasons for admission, the clinical severity under the MTS, and the need for emergency surgery or hospitalisation were collected. No patient aged <18 years was included.
The data were evaluated using the Statistical Package for the Social Sciences (SPSS®), version 23 (SPSS Inc., IBM Corp., Armonk, NY, USA) through descriptive and analytical statistics. A P < 0.05 was considered statistically significant.
Results
During the COVID‐19 pandemic, on the aforementioned dates, 46.4% fewer patients visited our Urology ED compared with the same period the year before (122 vs 263). There was no significant difference in the mean age (56.93 years in 2020 vs 53.83 years in 2019) or the number of old patients (aged ≥65 years) between the two periods.
However, significantly fewer female patients sought emergency urological services during the COVID‐19 pandemic period (32.7% vs 14.8%, P < 0.05).
Regarding the clinical severity grade under the MTS, comparing the 2019 period with the same period in 2020, 16.3% vs 6.6% of patients corresponded to the orange bracelet, 67.7% vs 77% to the yellow bracelet, 11.8% vs 6.6% to the green bracelet, 1.1% vs 2.5% to the blue bracelet, and 3.0% vs 7.4% to the white bracelet, respectively (P < 0.05). However, no significant differences were noted between urgent or very urgent cases (yellow or orange bracelet) vs non‐urgent cases (green, blue or white) between the groups.
During the period analysed in 2019, the percentage of patients who required emergency surgery and hospitalisation was 6.8% and 11.0%, respectively. During the corresponding period in 2020, 9.0% required emergency surgery (P > 0.05) and 18.9% needed hospitalisation (P < 0.05; Fig. 1).
Fig. 1.
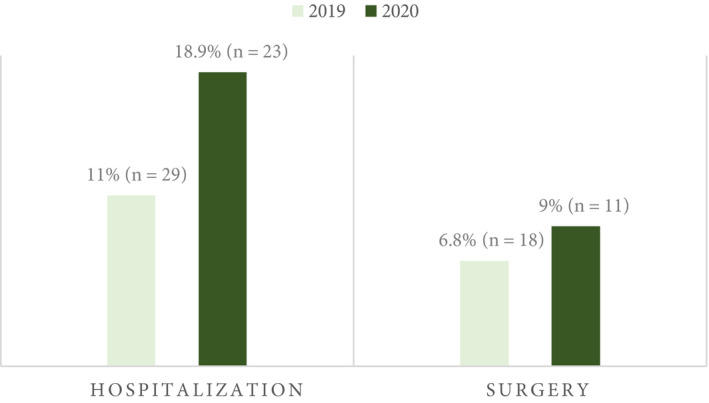
Requirement for hospitalisation and emergency surgery during both periods.
The main causes for presentation to the ED during the two periods studied are shown in Table 1.
Table 1.
Main causes of presentation to the Urology ED.
| Causes of presentation to the Urology ED | During the COVID‐19 pandemic, n (%) | Same period in 2019, n (%) |
|---|---|---|
| Haematuria | 19 (15.6) | 35 (13.3) |
| Renal colic | 19 (15.6) | 59 (22.4) |
| Acute urinary retention | 14 (11.5) | 21 (8.0) |
| UTIs | 29 (23.8) | 69 (26.2) |
| Acute pyelonephritis | 9 (7.4) | 22 (8.3) |
| Acute epididymo‐orchitis | 6 (4.9) | 11 (4.2) |
| Acute prostatitis | 4 (3.3) | 7 (2.7) |
| Urethritis | 2 (1.6) | 5 (1.9) |
| Acute cystitis | 3 (2.5) | 16 (6.1) |
| Obstructive acute pyelonephritis | 5 (4.1) | 8 (3.0) |
| Post‐renal acute renal injury | 4 (3.3) | 3 (1.1) |
| Testicular pain (of unknown cause) | 6 (4.9) | 6 (2.3) |
| Testicular torsion | 2 (1.6) | 2 (0.8) |
| Balanoposthitis | 4 (3.3) | 3 (1.1) |
| Perineal or scrotal abscess | 1 (0.8) | 1 (0.4) |
| LUTS | 1 (0.8) | 8 (3.0) |
| Flank pain (of unknown cause) | 3 (2.5) | 28 (10.6) |
| Trauma | 3 (2.5) | 5 (1.9) |
| Renal | – | 1 (0.4) |
| Bladder | 1 (0.8) | – |
| Penile | 2 (1.6) | 2 (0.8) |
| Testicular | – | 2 (0.8) |
| Postoperative wound complication | 3 (2.5) | 2 (0.8) |
| Urological cancer | 2 (1.6) | 3 (1.1) |
| End‐stage cancer symptoms | – | 3 (1.1) |
| Cancer diagnosis/staging | 2 (1.6) | – |
| Complications related to urinary diversions | 12 (9.8) | 15 (5.7) |
| Cutaneous urostomy | 4 (3.3) | 1 (0.4) |
| Nephrostomy tubes | – | 3 (1.1) |
| Suprapubic cystostomy | 2 (1.6) | 1 (0.4) |
| Urethral catheter | 6 (4.9) | 7 (2.7) |
| JJ stent | – | 3 (1.1) |
| Dyspareunia | – | 2 (0.8) |
| Haematospermia | – | 1 (0.4) |
| Total | 122 (100) | 263 (100) |
The most common reasons for referral to the ED, during both periods, were haematuria, renal colic and UTIs, with frequencies varying between 13.3% and 26.2%.
The admission rate for UTI was similar. Acute cystitis was a less common referral during the COVID‐19 pandemic (2.5% vs 6.1%, P > 0.05). Non‐specific flank pain (not related to renal colic), usually mild and without severity criteria, also had a lower incidence during the COVID‐19 pandemic (2.5% vs 10.6%, P > 0.05).
The causes for attending the ED were frequently associated with the need for urgent surgical intervention, such as acute obstructive pyelonephritis, obstructive acute renal injury, and testicular torsion, which corresponded, respectively, to 4.1%, 3.3% and 1.6% of the causes during the COVID‐19 pandemic, and 3.0%, 1.1% and 0.8% in the previous year.
Discussion
The primary hypothesis of the present study was that the COVID‐19 pandemic would cause a decrease in the demand for healthcare at the ED.
We found that the reasons that may account for such a reduction included: the moral conscience of not overloading services concentrated in response to the pandemic, the limitation of dislocation and social isolation, and avoiding exposure to the risk of contamination.
As expected, there was a 53.6% decrease in the number of attendees to the Urology ED at our hospital during the COVID‐19 pandemic. Our present results strongly support that COVID‐19 significantly influenced people’s urological care‐seeking behaviour.
These facts were corroborated by a study developed by The National School of Public Health of the University of Lisbon, which showed that emergency episodes for all causes in March 2020 fell by 45% compared to the same period in the previous year [6].
The Portuguese NHS considers reduction or exclusion from the payment of moderating fees to certain groups of people, taking into account the economic, social and health conditions of each one, allowing many Portuguese citizens to attend, relatively easily, an ED of a tertiary hospital [4]. Portugal also has the highest hospital emergency use in the Organisation for Economic Co‐operation and Development (OECD) area [6]. However, it appears that this ease of access did not influence the aforementioned restriction of the use of the ED for more serious situations.
Therefore, in our present sample, we were found a reduction in urgent causes to attend the ED considered less serious, such as non‐complicated UTI or non‐specific flank pain. On the other hand, the percentage of cases requiring emergency surgery and hospitalisation showed a higher percentage during the pandemic.
Regarding the MTS, no significant differences were noted between urgent vs non‐urgent cases in both groups, which, in the opinion of the authors, may be related to the fact that this triage often does not reflect the severity of the urological clinical situation.
During the pandemic, less female patients sought emergency urological services (14.8%, P < 0.05), which might be attributed to females being more apprehensive about viral transmission or that male patients normally have more urological urgent reasons to attend the ED.
Meanwhile, in 2020, more patients (7.4% vs 3%) were observed for administrative or clinical reasons (white bracelet), which might be attributed to the fact that the urological ED is convenient for care accessibility for patients who had their regular consultations, ambulatory treatments or procedures postponed due to the pandemic.
The authors recognise that the study has several limitations, namely, those inherent to its retrospective nature. As it is a recent and ongoing situation, a relatively short period has been analysed and may not be representative.
Regarding the causes for ED attendance, these were collected based on the records made by the doctors and not according to a pre‐established and validated coding, which could interfere with the quality of the data presented.
However, despite the fact that the study is single‐centred, the authors believe that it may be representative of the national reality. The CHUP is a tertiary hospital, covering a large geographical area [7].
Although most of the publics’ attention is focussed on the direct consequences of COVID‐19, possible health consequences resulting from people’s fears of it should not be overlooked. Understanding the present situation is helpful in terms of predicting future urological needs. Based on the results of the present study, we have reasons to speculate that people’s requirements for urological services might grow explosively in the post‐COVID‐19 period.
There is a continuity trail of this study, which the authors assume as unfinished.
Bearing in mind that it is not yet possible to determine the timeframe for the resumption of normality in the Portuguese NHS, it is important to analyse, subsequently and carefully, the consequences that this pandemic may have in terms of morbidity and mortality not directly related to the severe acute respiratory syndrome coronavirus 2 (SARS‐Cov‐2) virus.
Funding
None.
Conflicts of Interest
None.
Abbreviations
- CHUP
Centro Hospitalar Universitário do Porto
- COVID‐19
coronavirus disease 2019
- ED
Emergency Department
- MTS
Manchester Triage System
Acknowledgements
None.
References
- 1. World Health Organization . Virtual press conference on COVID‐19 – 11 March 2020. Available at: https://www.who.int/docs/default‐source/coronaviruse/transcripts/who‐audio‐emergencies‐coronavirus‐press‐conference‐full‐and‐final‐11mar2020.pdf?sfvrsn=cb432bb3_2. Accessed March 2020
- 2. Diário da RepúblicaElectronico. Decreto n.º 2‐B/2020. Available at: https://dre.pt/web/guest/home/‐/dre/131068124/details/maximized. Accessed April 2020
- 3. Executive Digest . Covid‐19. Afluência às urgências baixoumais de 50%. Available at: https://executivedigest.sapo.pt/covid‐19‐afluencia‐as‐urgencias‐baixou‐mais‐de‐50/. Accessed March 2020
- 4. Ministério da Saúde . Retrato da Saúde, 2018. Available at: https://www.sns.gov.pt/wp‐content/uploads/2018/04/RETRATO‐DA‐SAUDE_2018_compressed.pdf. Accessed March 2020
- 5. Zachariasse JM, Seiger N, Rood PP et al. Validity of the Manchester triage system in emergency care: a prospective observational study. PLoS One 2017; 12: e0170811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Santana R, Rocha J, Sousa J, Soares P. A procura dos A procura de serviços de urgência/emergência hospitalar: tendências durante o primeiro mês de resposta à COVID‐19. EscolaNacional de SaúdePública, Universidade NOVA de Lisboa 2020. [Epub ahead of print]. Available at: https://www.ensp.unl.pt/wp‐content/uploads/2017/06/tendencia‐de‐resposta‐dos‐servicos‐de‐urg‐emerg‐covid‐19.pdf. Accessed May 2020
- 7. Centro HospitalarUniversitário Do Porto. Relatório & Contas 2018. Available at: https://www.chporto.pt/pdf/princ_bom_gov/chp_RC_2018Final.pdf. Accessed April 2020


