To the Editor: We read with particular interest your comments in Obesity regarding the coronavirus disease 2019 (COVID‐19) epidemic (1) and a related manuscript by Simonnet et al. (2). Resolution of the specific relationship between obesity and COVID‐19, two existing public health epidemics, is critically needed to potentially prevent health systems worldwide from being overburdened. Few studies describing COVID‐19 with rates of obesity exist, and most are based on heterogenous populations (Table 1) (2, 3, 4, 5, 6, 7, 8, 9). In cohort studies of COVID‐19, obesity rates are generally reported as no higher than population‐based estimates; in contrast, subgroups of patients with critical illness (e.g., intensive care unit [ICU] patients) report higher prevalence rates of obesity.
Table 1.
Obesity and COVID‐19
| Source | Nation | Obesity prevalence (%) | Age (y) | Notes | |
|---|---|---|---|---|---|
| General population | Patients with COVID‐19 | ||||
| McMichael et al. ( 3 ) | USA | 42.4 | 22.2 | 72 (range: 21‐100) | Inpatients (n = 101), health care personnel (n = 50), visitors (n = 16) |
| Richardson et al. ( 4 ) | USA | 42.4 | 41.7 | 63 (IQR: 52‐75) | n = 4,170 hospitalized patients with and without critical illness |
| Centers for Disease Control and Prevention ( 8 ) | USA | 42.4 | 53.2 | >18 | n = 415 hospitalized patients with and without critical illness |
| European Centre for Disease Prevention and Control ( 9 ) a | Europe | 20 (male), 23 (female) | 73.4 | >18 | ICU patients with critical illness |
| Lighter J et al. ( 5 ) b | USA | 42.4 | 37 | >18 | n = 3,615 patients with and without critical illness |
| 46.8 | >18 | n = 431 ICU patients with critical illness | |||
| 41.1 | >18 | n = 547 acute care patients | |||
| Goyal et al. ( 6 ) | USA | 42.4 | 35.8 | 62 (49‐74) | n = 393, patients with critical illness on IMV and patients without critical illness |
| 43.4 | 65 | n = 130 ICU patients with critical illness | |||
| 31.9 | 62 | n = 263 acute care patients | |||
| Istituto Superiore Sanità ( 13 ) | Italy | 9.8 | 71.4 | 18‐40 | n = 49 young patient deaths as of April 16, 2020 |
| 11.8 | >18 | n = 19,996 c patient deaths as of April 16, 2020 | |||
| Simonnet et al. ( 2 ) d | France | 15 | 75.8 e | 60 (IQR 51‐70) | n = 124 ICU patients with critical illness |
| Qingxian et al. ( 7 ) f | China | 17.8 | 10.7 (BMI ≥ 28) | 48 (IQR 39‐54) | n = 383 patients with and without critical illness |
Data reported for Italy, Spain, Sweden, Switzerland, and the Netherlands.
Risk of acute or ICU admission for patients with obesity: ≥60 years old (odds ratios, 0.9 and 1.5; P = nonsignificant); <60 years old (odds ratios, 1.8 and 3.6; P < 0.001)
12.6% of all cases in Italy.
Risk of IMV for patients with BMI > 35: odds ratio, 7.36 (P = 0.021).
Versus 25.8% for ICU patients without COVID‐19.
Risk of progression to severe pneumonia for patients with obesity: odds ratio, 3.4 (P = 0.006).
COVID‐19, coronavirus disease 2019; ICU, intensive care unit; IMV, invasive mechanical ventilation; IQR, interquartile range.
In Italy, no official data have been released to evaluate the prevalence of obesity in COVID‐19 patients. A recent Italian report (10) failed to mention obesity as a comorbidity in admitted ICU patients with COVID‐19, despite the higher rates of obesity in severe disease (including ICU admission) in non‐Italian studies (Table 1). Although correlation does not imply a causal relationship, as other factors may indeed play a role in the heterogeneity of the sampled population, the incidence of COVID‐19 in each Italian region is surprisingly inversely related to the regional prevalence of obesity (r = −0.76; P < 0.001) (Figure 1). Yet Italian data demonstrated high obesity rates (~71%) only among younger patients (<40 years) dying of COVID‐19 in this small subgroup of 49 patients. Such data suggest that in Italy, obesity may have a greater impact at a younger age, which is consistent with data from ICU cohorts without COVID‐19. In fact, it also was reported (5) that the risk of ICU admission for patients with obesity is higher at younger ages (<60 years old). We cautiously speculate that the higher obesity rates (>75%) in ICU‐based patients with COVID‐19 as reported by Simonnet et al. (2) may depend on the relatively young age of their cohort (median age of 60 years). These authors also observed an increased risk of mechanical ventilation in patients with class II obesity. Rates of critical illness in patients with COVID‐19 and obesity are higher than those reported for ICU patients with obesity (~20%) (11). Although lower mortality rates have been reported in patients with BMI ≥ 25 kg/m2 in ICU settings (11, 12), additional data are lacking in ICU‐based COVID‐19 with obesity. Despite many limitations, data reported in Table 1 distinguish among obesity, diabetes, and hypertension, which further supports the importance of obesity in this illness.
Figure 1.
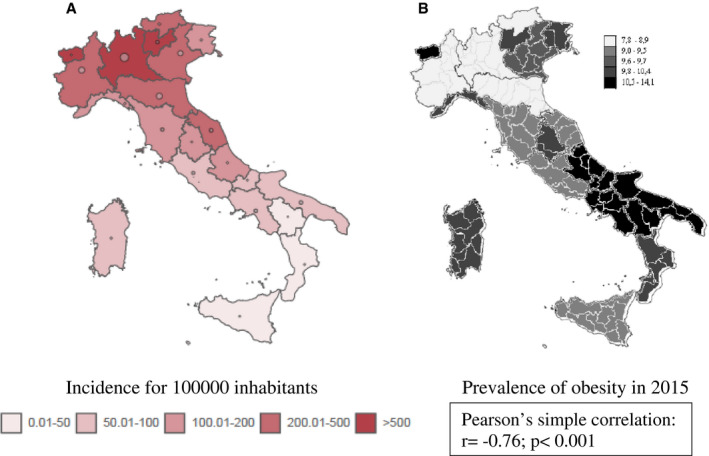
(A) Incidence of coronavirus 2019 disease (COVID‐19) in Italy as of April 16, 2020, and (B) prevalence of overweight and obesity. Data are from the Istituto Superiore di Sanità, Rome, Italy (13), and Istat (14). [Color figure can be viewed at wileyonlinelibrary.com]
In conclusion, obesity strongly impacts the severity of COVID‐19, yet it behooves clinicians and researchers to recognize the heterogenous nature of the existing cohort data. This study furthers our understanding of the obesity/COVID‐19 relationship. There are important, unresolved questions related to the impact of body composition (fat/fat‐free muscle), relevant coexisting comorbid conditions, severity of disease, and predictors of important outcomes such as hospitalization and mortality in this population.
Disclosure
The authors declared no conflict of interest.
References
- 1. Ryan DH, Ravussin E. COVID 19 and the patient with obesity ‐ the editors speak out. Obesity (Sliver Spring) 2020;28:847. doi:10.1002/oby.22808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020;28:1195‐1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McMichael TM, Currie DW, Clark S, et al. Epidemiology of COVID‐19 in a long‐term care facility in King County, Washington. N Engl J Med 2020;382:2005‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA 2020;323:2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 years is a risk factor for COVID‐19 hospital admission. Clin Infect Dis 2020:ciaa415. doi:10.1093/cid/ciaa415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID‐19 in New York City. N Engl J Med 2020;382:2372‐2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Qingxian C, Fengjuan C, Fang L, et al. Obesity and COVID‐19 severity in a designated hospital in Shenzhen, China. Diabetes Care 2020;43:1392‐1398. [DOI] [PubMed] [Google Scholar]
- 8. Coronavirus disease 2019 (COVID‐19): cases, data, and surveillance. Centers for Disease Control and Prevention. Accessed April 28, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/cases‐updates/index.html
- 9. European Center for Disease Prevention and Control . Rapid risk assessment: coronavirus disease 2019 (COVID‐19) in the EU/EEA and the UK – eighth update. Accessed April 28, 2020. https://www.ecdc.europa.eu/sites/default/files/documents/covid‐19‐rapid‐risk‐assessment‐coronavirus‐disease‐2019‐eighth‐update‐8‐april‐2020.pdf
- 10. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020;323:1574‐1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schetz M, De Jong A, Deane AM, et al. Obesity in the critically ill: a narrative review. Intensive Care Med 2019;45:757‐769. [DOI] [PubMed] [Google Scholar]
- 12. Akinnusi ME, Pineda LA, El Silh AA. Effect of obesity on intensive care morbidity and mortality: a meta‐analysis. Crit Care Med 2008;36:151‐158. [DOI] [PubMed] [Google Scholar]
- 13. Task force COVID‐19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità. Epidemia COVID‐19, Aggiornamento nazionale: 9 aprile 2020. Accessed April 16, 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino‐sorveglianza‐integrata‐COVID‐19_9‐aprile‐2020.pdf?fbclid=IwAR0T2dkwkLO56Xsl9yu2SR0jITRDvspzPyw0w3SodIaGeH4IJQdUsA0G15k [Google Scholar]
- 14. Rapporto osserva salute 2016. Accessed April 16, 2020. https://www.osservatoriosullasalute.it/osservasalute/rapporto‐osservasalute‐2016 [Google Scholar]


